Development of a CO2 Sensor for Extracorporeal Life Support Applications
Abstract
:1. Introduction
2. Materials and Methods
2.1. State-of-the-Art on CO2 Sensors
2.2. Design Requirements for CO2 Sensors Applied to ECLS Procedures
2.3. The Newly Developed CO2 Sensing Platform
- emission stage for the generation of the mid-IR beam;
- receiver stage for the detection, conditioning and amplification of the optical signal after CO2 absorption and;
- CPU for signal acquisition, processing, and communication with a host device.
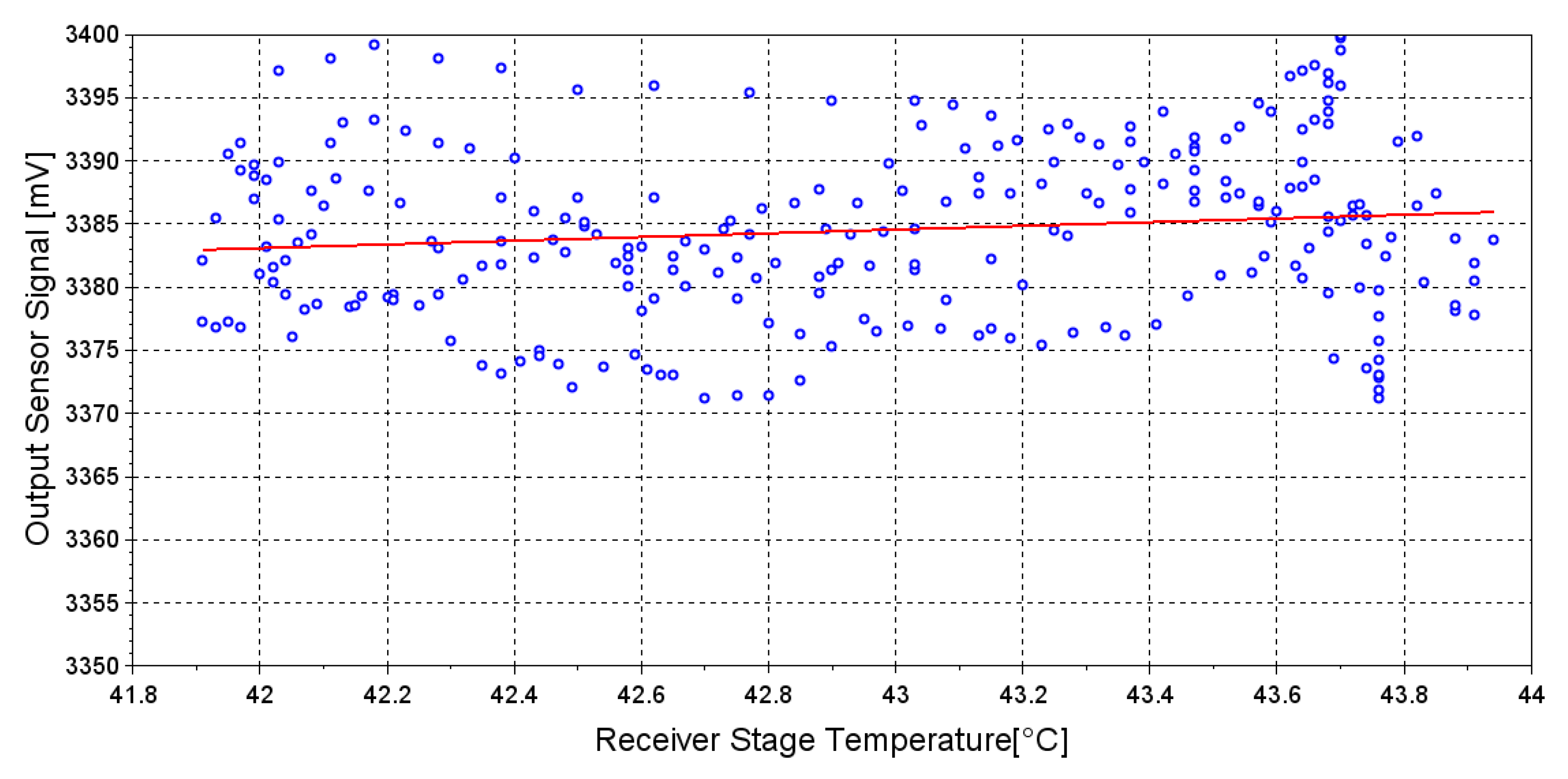
2.4. Preliminary Analysis of Temperature Effect on Receiver Stage
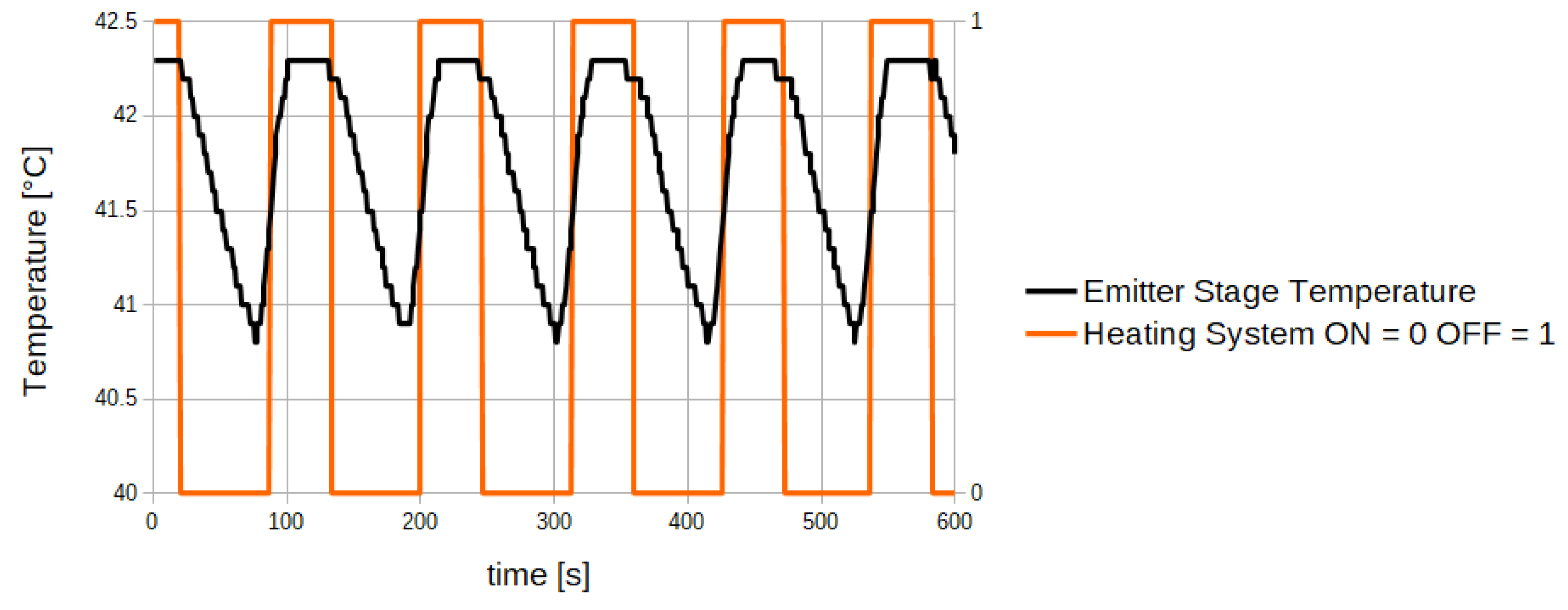
2.5. Preliminary Analysis of Temperature Effect on the Emitter Stage
2.6. Experimental Analysis
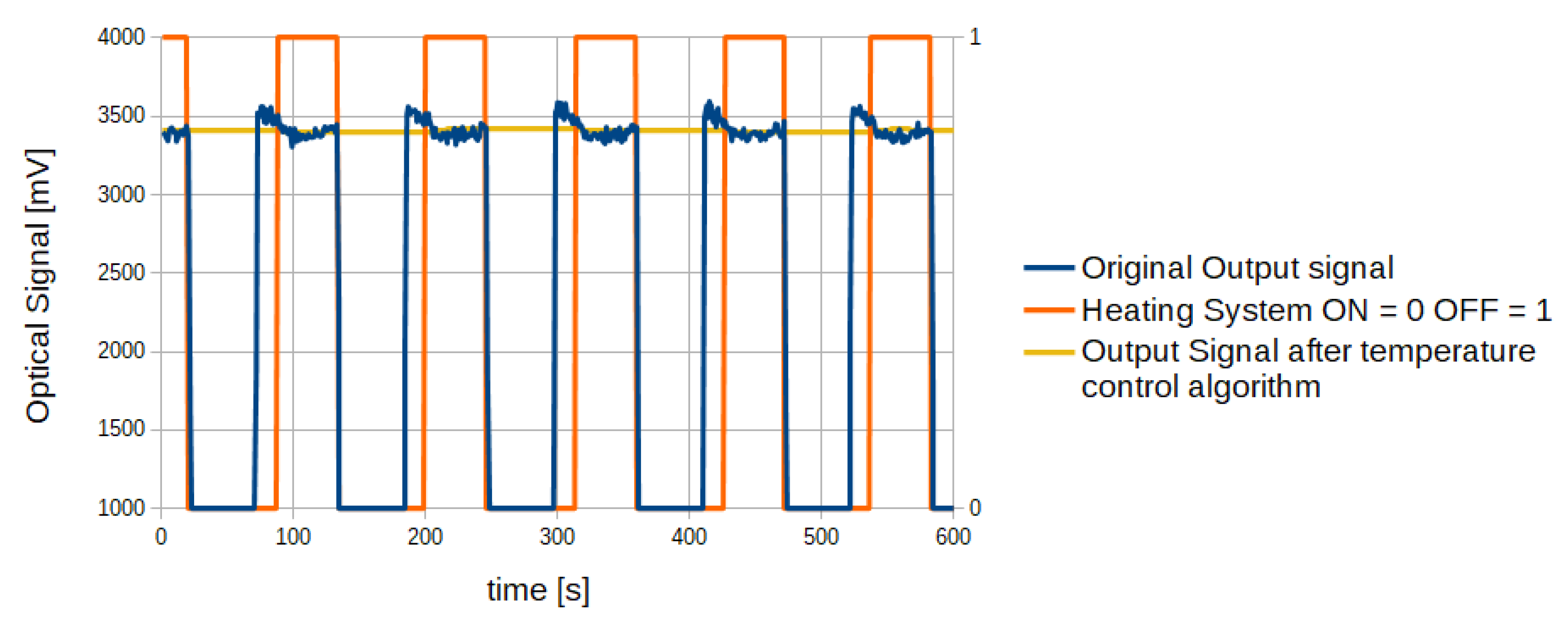
2.7. Temperature Control Algorithm
- an initial phase performed at start-up, necessary to allow the sensor to reach the steady state temperature, and
- a phase in which the heating module is alternatively turned on and off by the CPU.
3. Results
3.1. Sensor Validation in Experimental Laboratory Setting
3.2. In Vivo Sensor Validation
4. Discussion and Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Davis, D.P. Quantitative capnometry as a critical resuscitation tool. J. Trauma Nurs. 2005, 12, 40. [Google Scholar] [CrossRef] [PubMed]
- Cereceda-Sánchez, F.J.; Molina-Mula, J. Systematic Review of Capnography with Mask Ventilation during Cardiopulmonary Resuscitation Maneuvers. J. Clin. Med. 2019, 8, 358. [Google Scholar] [CrossRef] [Green Version]
- Eipe, N.; Doherty, D.R. A review of pediatric capnography. J. Clin. Monit. Comput. 2010, 24, 261–268. [Google Scholar] [CrossRef] [PubMed]
- Grmec, Š. Comparison of three different methods to confirm tracheal tube placement in emergency intubation. Intensive Care Med. 2002, 28, 701–704. [Google Scholar] [CrossRef] [PubMed]
- Kupnik, D.; Skok, P. Capnometry in the prehospital setting: Are we using its potential? Emergency Med. J. 2007, 24, 614–617. [Google Scholar] [CrossRef]
- Baraka, A.; El-Khatib, M.; Muallem, E.; Jamal, S.; Haroun-Bizri, S.; Aouad, M. Oxygenator exhaust capnography for prediction of arterial carbon dioxide tension during hypothermic cardiopulmonary bypass. J. Extra-Corporeal Technol. 2005, 37, 192. [Google Scholar]
- Montalti, A.; Belliato, M.; Gelsomino, S.; Nalon, S.; Matteucci, F.; Parise, O.; de Jong, M.; Makhoul, M.; Johnson, D.M.; Lorusso, R. Continuous monitoring of membrane lung carbon dioxide removal during ECMO: Experimental testing of a new volumetric capnometer. Perfusion 2019, 34, 538–543. [Google Scholar] [CrossRef] [PubMed]
- Duscio, E.; Cipulli, F.; Vasques, F.; Collino, F.; Rapetti, F.; Romitti, F.; Behnemann, T.; Niewenhuys, J.; Tonetti, T.; Pasticci, I.; et al. Extra-corporeal CO2 removal: The minimally invasive approach, theory, and practice. Crit. Care Med. 2019, 47, 33–40. [Google Scholar] [CrossRef] [PubMed]
- Epis, F.; Belliato, M. Oxygenator performance and artificial-native lung interaction. J. Thoracic Dis. 2018, 10, S596. [Google Scholar] [CrossRef] [PubMed]
- Potger, K.C.; McMillan, D.; Southwell, J.; Dando, H.; O Shaughnessy, K. Membrane oxygenator exhaust capnography for continuously estimating arterial carbon dioxide tension during cardiopulmonary bypass. J. Extra-Corporeal Technol. 2003, 35, 218–223. [Google Scholar]
- Bembea, M.M.; Lee, R.; Masten, D.; Kibler, K.K.; Lehmann, C.U.; Brady, K.M.; Easley, R.B. Magnitude of arterial carbon dioxide change at initiation of extracorporeal membrane oxygenation support is associated with survival. J. Extra-Corporeal Technol. 2013, 45, 26. [Google Scholar]
- Morales-Quinteros, L.; Del Sorbo, L.; Artigas, A. Extracorporeal carbon dioxide removal for acute hypercapnic respiratory failure. Ann. Intensive Care 2019, 9, 79. [Google Scholar] [CrossRef]
- Msimo EMMA Capnometer Datasheet. Available online: https://www.masimo.com/siteassets/us/documents/pdf/plm-10642a_product_information_emma_capnograph_us.pdf (accessed on 20 November 2019).
- Medtronic Microcap Capnometer Datasheet. Available online: https://www.medtronic.com/covidien/en-us/products/capnography/microcap-handheld-capnographs.html (accessed on 20 November 2019).
- Hodgkinson, J.; Tatam, R.P. Optical gas sensing: A review. Meas. Sci. Technol. 2012, 24, 012004. [Google Scholar] [CrossRef] [Green Version]
- Stuart, B. Infrared spectroscopy. Kirk-Othmer Encycl. Chem. Technol. 2000, 1–18. [Google Scholar] [CrossRef]
- Dinh, T.V.; Choi, I.Y.; Son, Y.S.; Kim, J.C. A review on non-dispersive infrared gas sensors: Improvement of sensor detection limit and interference correction. Sens. Actuators, B 2016, 231, 529–538. [Google Scholar] [CrossRef]
- Bezyazychnaya, T.; Bogdanovich, M.; Kabanov, V.; Kabanau, D.; Lebiadok, Y.; Parashchuk, V.; Ryabtsev, A.; Ryabtsev, G.; Shpak, P.; Shchemelev, M.; et al. Light emitting diode–photodiode optoelectronic pairs based on the InAs/InAsSb/InAsSbP heterostructure for the detection of carbon dioxide. Semiconductors 2015, 49, 980–983. [Google Scholar] [CrossRef]
- Gordon, I.E.; Rothman, L.S.; Hill, C.; Kochanov, R.V.; Tan, Y.; Bernath, P.F.; Birk, M.; Boudon, V.; Campargue, A.; Chance, K.; et al. The HITRAN2016 molecular spectroscopic database. J. Quant. Spectrosc. Radiat. Transfer 2017, 203, 3–69. [Google Scholar] [CrossRef]
- Degner, M.; Jürß, H.; Ewald, H. Fast and low power optical CO2-sensors for medical application: New sensor designs for main-and side-stream CO2-sensors are presented in comparison with state of the art capnometers. In Proceedings of the 2018 IEEE International Instrumentation and Measurement Technology Conference (I2MTC), Houston, TX, USA, 14–17 May 2018; pp. 1–5. [Google Scholar]
- Jaffe, M.B. Infrared measurement of carbon dioxide in the human breath:“breathe-through” devices from Tyndall to the present day. Anesthesia Analgesia 2008, 107, 890–904. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sotnikova, G.Y.; Gavrilov, G.A.; Aleksandrov, S.E.; Kapralov, A.A.; Karandashev, S.A.; Matveev, B.A.; Remennyy, M.A. Low Voltage CO2-Gas Sensor Based on III–V Mid-IR Immersion Lens Diode Optopairs: Where we Are and How Far we Can Go? IEEE Sens. J. 2009, 10, 225–234. [Google Scholar] [CrossRef]
- Walsh, B.K.; Crotwell, D.N.; Restrepo, R.D. Capnography/Capnometry during mechanical ventilation: 2011. Respir. Care 2011, 56, 503–509. [Google Scholar] [CrossRef] [PubMed]
- ISO—International Organization for Standardization. ISO 80601-2-55 Medical Electrical Equipment—Particular Requirements for the Basic Safety and Essential Performance of Respiratory Gas Monitors. Available online: https://infostore.saiglobal.com/preview/98695750340.pdf?sku=867463_saig_nsai_nsai_2063036 (accessed on 26 June 2020).
- Capnometer. Available online: https://patentimages.storage.googleapis.com/f9/f3/7a/67700280bd19d5/WO2016092308A1.pdf (accessed on 26 June 2020).
- Jaffe, M.B. Mainstream or sidestream capnography? Environment 2002, 4, 5. [Google Scholar]
- Aittomäki, J. Monitoring of CO2 exchange during cardiopulmonary bypass: The effect of oxygenator design on the applicability of capnometry. Perfusion 1993, 8, 337–344. [Google Scholar] [CrossRef] [PubMed]
- Høgetveit, J.O.; Kristiansen, F.; Pedersen, T.H. Development of an instrument to indirectly monitor arterial pCO2 during cardiopulmonary bypass. Perfusion 2006, 21, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.J.; Jang, S.P. Experimental and numerical analysis of heat transfer phenomena in a sensor tube of a mass flow controller. Int. J. Heat Mass Transfer 2001, 44, 1711–1724. [Google Scholar] [CrossRef]
- LED MicrosensorNT: LED and Photodiode Datasheet. Available online: http://lmsnt.com/ (accessed on 20 November 2019).
- Kristiansen, F.; Høgetveit, J.O.; Pedersen, T.H. Clinical evaluation of an instrument to measure carbon dioxide tension at the oxygenator gas outlet in cardiopulmonary bypass. Perfusion 2006, 21, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Aleksandrov, S.; Gavrilov, G.; Kapralov, A.; Matveev, B.; Sotnikova, G.Y.; Remennyi, M. Simulation of characteristics of optical gas sensors based on diode optopairs operating in the mid-IR spectral range. Tech. Phys. 2009, 54, 874–881. [Google Scholar] [CrossRef]
- Del Castillo, J.; López-Herce, J.; Matamoros, M.; Cañadas, S.; Rodriguez-Calvo, A.; Cechetti, C.; Rodriguez-Núñez, A.; Álvarez, A.C.; Iberoamerican Pediatric Cardiac Arrest Study Network RIBEPCI. Hyperoxia, hypocapnia and hypercapnia as outcome factors after cardiac arrest in children. Resuscitation 2012, 83, 1456–1461. [Google Scholar] [CrossRef]














| CO2 Concentration Set-Point [v/v %] | Developed CO2 Sensor | “Gold Standard” Sensor |
|---|---|---|
| 1.60% | 1.60% | 1.40% |
| 2.20% | 2.00% | 1.90% |
| 3.60% | 3.50% | 3.40% |
| 3.90% | 4.00% | 4.00% |
| 5.40% | 5.50% | 5.30% |
| 6.10% | 5.80% | 6.20% |
| 6.60% | 6.50% | 6.70% |
| 7.40% | 7.50% | 7.50% |
| Average Error ± SD | 0.13 ± 0.09% | 0.15 ± 0.07% |
| Gas Flow | Gas Flow | CO2 Concentration | CO2 Concentration | VCO2 | VCO2 |
|---|---|---|---|---|---|
| Developed Sensor | “Gold Standard” | Developed Sensor | “Gold Standard” | Developed Sensor | “Gold Standard” |
| [L/min] | Sensor [L/min] | [v/v %] | Sensor [v/v %] | [mL/min] | Sensor [mL/min] |
| 1.60 | 1.50 | 3.80% | 3.80% | 60.8 | 57.0 |
| 1.00 | 1.00 | 7.00% | 6.90% | 70.0 | 69.0 |
| 1.00 | 1.00 | 7.10% | 7.00% | 71.0 | 70.0 |
| 1.10 | 1.00 | 8.20% | 8.30% | 90.2 | 83.0 |
| 1.50 | 1.40 | 7.60% | 7.60% | 114.0 | 106.4 |
| 2.20 | 2.10 | 5.20% | 5.00% | 114.4 | 105.0 |
| 3.60 | 3.60 | 3.60% | 3.40% | 129.6 | 122.4 |
| 0.80 | 0.70 | 5.00% | 4.80% | 40.0 | 33.6 |
| 3.10 | 3.00 | 4.40% | 4.40% | 136.4 | 132.0 |
| 4.50 | 4.50 | 3.60% | 3.40% | 162.0 | 153.0 |
| Gas Flow Average Error ± SD [L/min] | CO2 Concentration Average Error ± SD [v/v%] | VCO2 Average Error ± SD [mL/min] | |||
| 0.06 ± 0.05 | 0.11 ± 0.09 | 5.7 ± 3 | |||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bellancini, M.; Cercenelli, L.; Severi, S.; Comai, G.; Marcelli, E. Development of a CO2 Sensor for Extracorporeal Life Support Applications. Sensors 2020, 20, 3613. https://doi.org/10.3390/s20133613
Bellancini M, Cercenelli L, Severi S, Comai G, Marcelli E. Development of a CO2 Sensor for Extracorporeal Life Support Applications. Sensors. 2020; 20(13):3613. https://doi.org/10.3390/s20133613
Chicago/Turabian StyleBellancini, Michele, Laura Cercenelli, Stefano Severi, Guido Comai, and Emanuela Marcelli. 2020. "Development of a CO2 Sensor for Extracorporeal Life Support Applications" Sensors 20, no. 13: 3613. https://doi.org/10.3390/s20133613
APA StyleBellancini, M., Cercenelli, L., Severi, S., Comai, G., & Marcelli, E. (2020). Development of a CO2 Sensor for Extracorporeal Life Support Applications. Sensors, 20(13), 3613. https://doi.org/10.3390/s20133613






