Real-Time Person Identification in a Hospital Setting: A Systematic Review
Abstract
1. Introduction
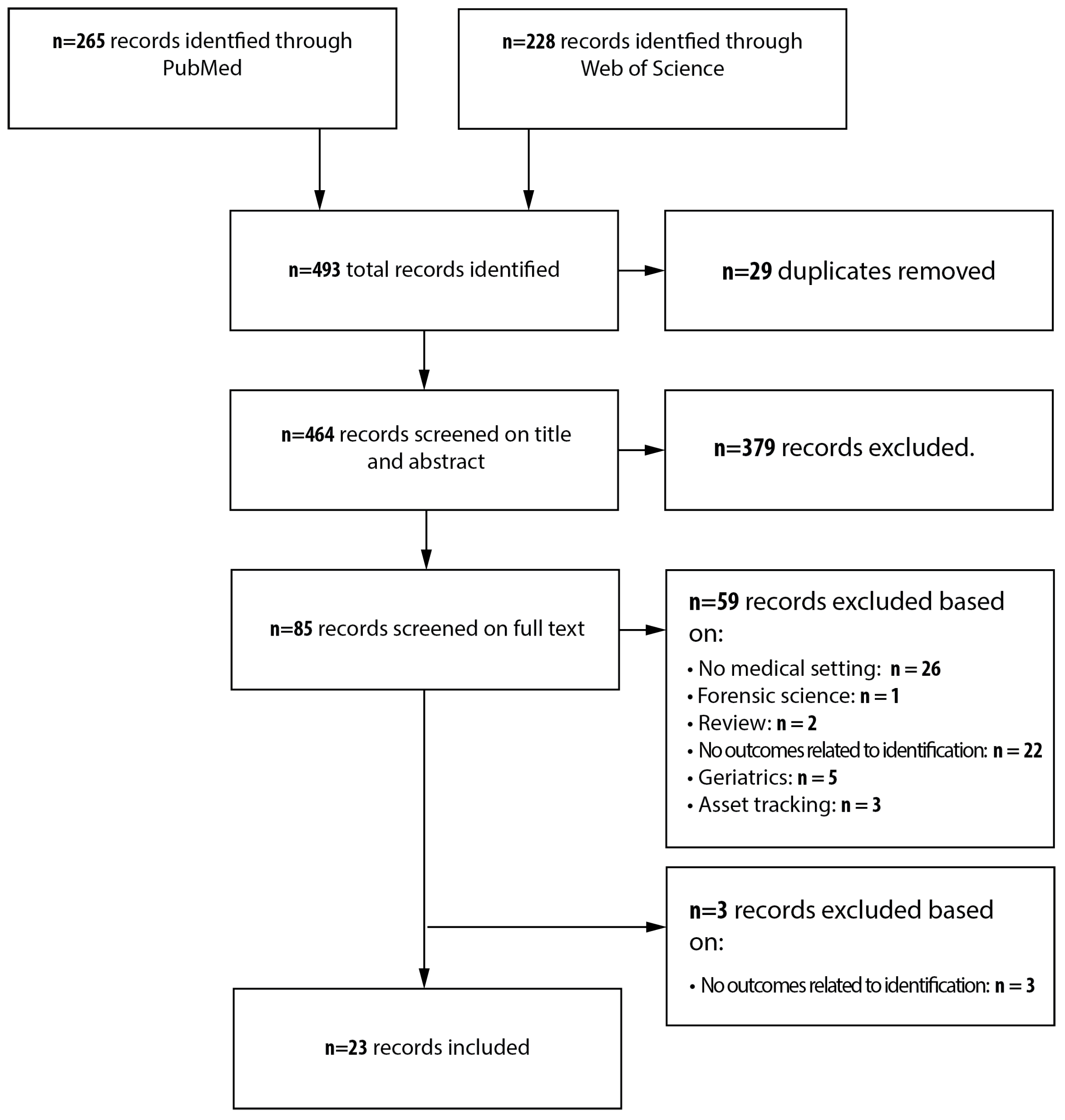
2. Method
3. Results
3.1. RFID
3.1.1. Active RFID
3.1.2. Passive RFID
3.1.3. Unspecified RFID
3.2. Biometric
3.2.1. Fingerprints
3.2.2. Facial Recognition
3.2.3. Iris Scan
3.3. Others
4. Discussion
4.1. Limitations of the Included Studies and Outcomes
4.2. Limitations of the Review Method
4.3. Contribution and Future Research
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| MDPI | Multidisciplinary Digital Publishing Institute |
| DOAJ | Directory of open access journals |
| TLA | Three letter acronym |
| LD | linear dichroism |
| RFID | Radio Frequency Identification Device |
| IR | Infrared |
| US | Ultrasound |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Anlaysis |
| RTLS | Real-Time Location Tracking System |
| CT | Computer Tomography |
| MRI | Magnetic Resonance Imaging |
| IT | Information Technology |
| UHF | Ultra High Frequency |
| HIV | Human Immunodeficiency Virus |
| ICU | Intensive Care Unit |
| WLAN | Wireless Local Area Network |
| UWB | Ultra-Wide Band |
| ID | Identification |
| NFC | Near-Field Communication |
Appendix A. Search String
Appendix A.1. PubMed
Appendix A.2. Web of Science
Appendix B. Quality/Bias Assessment
- Description of technique (0–2.5p)
- –
- Is there a general description of hardware components? (+1p)
- –
- Is the brand and type of technology described? (+0.5p)
- –
- Is the specific setting for which the technology will be used described? (+0.5p)
- –
- Is there a description of which software is used? (+0.5p)
- Description of implementation-/test setting of the research (0–3.5p)
- –
- Is it described which hardware and software components have been used during the test? (+0.5p)
- –
- Is it described which persons have been tested: personnel/ patients? (+0.5p)
- –
- Is it described how many people were used during the test? (+1p)
- –
- Are the people used during the test also the users for which the technology is made? (+0.5p)
- –
- Is the duration of the test/study described? (+0.5p)
- –
- Is it described which way results were obtained? (+0.5p)
- Stadium of technology used during the test (0.5–1.5p)
- –
- Is the technology, that was tested, a Proof of concept/Prototype? (0.5p)
- –
- Is the technology, that was tested, in a Pilot study / Pre-Final version? (1p)
- –
- Is the technology, that was tested, a Final version? (1.5p)
- Test setting (0.5–1.5p)
- –
- Is it tested as a simulation of a hospital/ care setting? Is it tested in other department or environment in care? (0.5p)
- –
- Is the test partly used in daily care practice or used parallel next to the old system? (1p)
- –
- Is the test already used in daily care practice? (1.5p)
- * 1–3.75
- ** 4–6.75
- *** 7–9
- A
- People used for testing are also the people who are actively involved in the development of the technology.
- B
- The observations of technology are done by the people actively involved in the development of technology.
- C
- There is an conflict of interest.
References
- El-Shafy, I.A.; Delgado, J.; Akerman, M.; Bullaro, F.; Christopherson, N.A.; Prince, J.M. Closed-Loop Communication Improves Task Completion in Pediatric Trauma Resuscitation. J. Surg. Educ. 2018, 75, 58–64. [Google Scholar] [CrossRef] [PubMed]
- Salas, E.; Wilson, K.A.; Murphy, C.E.; King, H.; Salisbury, M. Communicating, Coordinating, and Cooperating When Lives Depend on It: Tips for Teamwork. Jt. Comm. J. Qual. Patient Saf. 2008, 34, 333–341. [Google Scholar] [CrossRef]
- Bergs, E.A.; Rutten, F.L.; Tadros, T.; Krijnen, P.; Schipper, I.B. Communication during trauma resuscitation: Do we know what is happening? Injury 2005, 36, 905–911. [Google Scholar] [CrossRef]
- Raley, J.; Meenakshi, R.; Dent, D.; Willis, R.; Lawson, K.; Duzinski, S. The Role of Communication During Trauma Activations: Investigating the Need for Team and Leader Communication Training. J. Surg. Educ. 2017, 74, 173–179. [Google Scholar] [CrossRef]
- Sarcevic, A.; Marsic, I.; Burd, R.S. Teamwork Errors in Trauma Resuscitation. ACM Trans. Comput.-Hum. Interact. 2012, 19, 1–30. [Google Scholar] [CrossRef]
- Gillespie, B.M.; Gwinner, K.; Chaboyer, W.; Fairweather, N. Team communications in surgery—Creating a culture of safety. J. Interprof. Care 2013, 27, 387–393. [Google Scholar] [CrossRef]
- Yao, W.; Chu, C.H.; Li, Z. The Adoption and Implementation of RFID Technologies in Healthcare: A Literature Review. J. Med. Syst. 2011, 36, 3507–3525. [Google Scholar] [CrossRef]
- Martínez Pérez, M.; Dafonte, C.; Gómez, Á. Traceability in Patient Healthcare through the Integration of RFID Technology in an ICU in a Hospital. Sensors 2018, 18, 1627. [Google Scholar] [CrossRef]
- Stankiewicz, S.; Kar, R.; Hadoulis, A.; Sullivan, F.; Nugent, W.C.; Sample, J. Implementation of a Radio-frequency Identification System to Improve the Documentation and Compliance of Attending Physicians’ Arrival to Trauma Activations. Cureus 2018, 10, e3582. [Google Scholar] [CrossRef]
- Cheng, P.L.; Su, Y.C.; Hou, C.H.; Chang, P.L. Management of In-Field Patient Tracking and Triage by Using Near-Field Communication in Mass Casualty Incidents. Stud. Health Technol. Inf. 2017, 245, 1214. [Google Scholar]
- Landaluce, H.; Arjona, L.; Perallos, A.; Falcone, F.; Angulo, I.; Muralter, F. A Review of IoT Sensing Applications and Challenges Using RFID and Wireless Sensor Networks. Sensors 2020, 20, 2495. [Google Scholar] [CrossRef] [PubMed]
- Ladan, M.A.; Wharrad, H.; Windle, R. Towards understanding healthcare professionals’ adoption and use of technologies in clinical practice: Using Qmethodology and models of technology acceptance. J. Innov. Health Inf. 2018, 25, 965. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef] [PubMed]
- Bramer, W.M.; Giustini, D.; de Jonge, G.B.; Holland, L.; Bekhuis, T. De-duplication of database search results for systematic reviews in EndNote. J. Med. Libr. Assoc. 2016, 104, 240. [Google Scholar] [CrossRef]
- Anne, N.; Dunbar, M.D.; Abuna, F.; Simpson, P.; Macharia, P.; Betz, B.; Cherutich, P.; Bukusi, D.; Carey, F. Feasibility and acceptability of an iris biometric system for unique patient identification in routine HIV services in Kenya. Int. J. Med. Inf. 2020, 133, 104006. [Google Scholar] [CrossRef] [PubMed]
- Cao, Q.; Jones, D.R.; Sheng, H. Contained nomadic information environments: Technology, organization, and environment influences on adoption of hospital RFID patient tracking. Inf. Manag. 2014, 51, 225–239. [Google Scholar] [CrossRef]
- Chang, Y.T.; Syed-Abdul, S.; Tsai, C.Y.; Li, Y.C. A novel method for inferring RFID tag reader recordings into clinical events. Int. J. Med. Inf. 2011, 80, 872–880. [Google Scholar] [CrossRef]
- Chen, C.; Chang, Y. Smart Healthcare Environment: Design with RFID Technology and Performance Evaluation. J. Med. Biol. Eng. 2013, 33, 427–432. [Google Scholar] [CrossRef]
- Fisher, J.A.; Monahan, T. Evaluation of real-time location systems in their hospital contexts. Int. J. Med. Informatics 2012, 81, 705–712. [Google Scholar] [CrossRef]
- Frisby, J.; Smith, V.; Traub, S.; Patel, V.L. Contextual Computing: A Bluetooth based approach for tracking healthcare providers in the emergency room. J. Biomed. Inform. 2017, 65, 97–104. [Google Scholar] [CrossRef]
- Hsu, J.M.; Yu, Y.C.; Hou, T.W.; Teng, W.G.; Chiang, T.C.; Yang, M.C. A Multi-Constraint Scheme with Authorized Mechanism for the Patient Safety. J. Med. Syst. 2016, 40, 123. [Google Scholar] [CrossRef] [PubMed]
- Jeong, I.C.; Bychkov, D.; Hiser, S.; Kreif, J.D.; Klein, L.M.; Hoyer, E.H.; Searson, P.C. Using a Real-Time Location System for Assessment of Patient Ambulation in a Hospital Setting. Arch. Phys. Med. Rehabil. 2017, 98, 1366–1373. [Google Scholar] [CrossRef] [PubMed]
- Jeon, B.; Jeong, B.; Jee, S.; Huang, Y.; Kim, Y.; Park, G.H.; Kim, J.; Wufuer, M.; Jin, X.; Kim, S.W.; et al. A Facial Recognition Mobile App for Patient Safety and Biometric Identification: Design, Development, and Validation. JMIR Mhealth Uhealth 2019, 7, e11472. [Google Scholar] [CrossRef] [PubMed]
- Kranzfelder, M.; Zywitza, D.; Jell, T.; Schneider, A.; Gillen, S.; Friess, H.; Feussner, H. Real-time monitoring for detection of retained surgical sponges and team motion in the surgical operation room using radio-frequency-identification (RFID) technology: A preclinical evaluation. J. Surg. Res. 2012, 175, 191–198. [Google Scholar] [CrossRef]
- Lin, J.; Pai, J.Y.; Chen, C.C. Applied Patent RFID Systems for Building Reacting HEPA Air Ventilation System in Hospital Operation Rooms. J. Med. Syst. 2012, 36, 3399–3405. [Google Scholar] [CrossRef]
- Liu, C.C.; Chang, C.H.; Su, M.C.; Chu, H.T.; Hung, S.H.; Wong, J.M.; Wang, P.C. RFID-initiated workflow control to facilitate patient safety and utilization efficiency in operation theater. Comput. Methods Programs Biomed. 2011, 104, 435–442. [Google Scholar] [CrossRef]
- Odei-Lartey, E.O.; Boateng, D.; Danso, S.; Kwarteng, A.; Abokyi, L.; Amenga-Etego, S.; Gyaase, S.; Asante, K.P.; Owusu-Agyei, S. The application of a biometric identification technique for linking community and hospital data in rural Ghana. Glob. Health Action 2016, 9, 1–7. [Google Scholar] [CrossRef]
- Ohashi, K.; Ota, S.; Ohno-Machado, L.; Tanaka, H. Smart medical environment at the point of care: Auto-tracking clinical interventions at the bed side using RFID technology. Comput. Biol. Med. 2010, 40, 545–554. [Google Scholar] [CrossRef]
- Martínez Pérez, M.; Vázquez González, G.; Dafonte, C. Evaluation of a Tracking System for Patients and Mixed Intravenous Medication Based on RFID Technology. Sensors 2016, 16, 2031. [Google Scholar] [CrossRef]
- Perez, M.M.; Gonzalez, G.V.; Dafonte, C. Safety and Traceability in Patient Healthcare through the Integration of RFID Technology for Intravenous Mixtures in the Prescription-Validation-Elaboration- Dispensation-Administration Circuit to Day Hospital Patients. Sensors 2016, 16, 1188. [Google Scholar] [CrossRef]
- Pineles, L.L.; Morgan, D.J.; Limper, H.M.; Weber, S.G.; Thom, K.A.; Perencevich, E.N.; Harris, A.D.; Landon, E. Accuracy of a radiofrequency identification (RFID) badge system to monitor hand hygiene behavior during routine clinical activities. Am. J. Infect. Control 2014, 42, 144–147. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Polycarpou, A.C.; Dimitriou, A.; Bletsas, A.; Polycarpou, P.C.; Papaloizou, L.; Gregoriou, G.; Sahalos, J.N. On the Design, Installation, and Evaluation of a Radio-Frequency Identification System for Healthcare Applications. IEEE Antennas Propag. Mag. 2012, 54, 255–271. [Google Scholar] [CrossRef]
- Saito, Y.; Suzuki, R.; Torikai, K.; Hasegawa, T.; Sakamaki, T. Efficiency and safety of new radiofrequency identification system in a hospital. Stud. Health Technol. Inf. 2013, 192, 1032. [Google Scholar]
- Steffen, T.; Luechinger, R.; Wildermuth, S.; Kern, C.; Fretz, C.; Lange, J.; Hetzer, F.H. Safety and reliability of radio frequency identification devices in magnetic resonance imaging and computed tomography. Patient Saf. Surg. 2010, 4. [Google Scholar] [CrossRef]
- Ting, S.L.; Kwok, S.K.; Tsang, A.H.C.; Lee, W.B. Critical Elements and Lessons Learnt from the Implementation of an RFID-enabled Healthcare Management System in a Medical Organization. J. Med. Syst. 2011, 35, 657–669. [Google Scholar] [CrossRef]
- Wall, K.M.; Kilembe, W.; Inambao, M.; Chen, Y.N.; McHoongo, M.; Kimaru, L.; Hammond, Y.T.; Sharkey, T.; Malama, K.; Fulton, T.R.; et al. Implementation of an electronic fingerprint-linked data collection system: A feasibility and acceptability study among Zambian female sex workers. Glob. Health 2015, 11, 27. [Google Scholar] [CrossRef]
- White, E.B.; Meyer, A.J.; Ggita, J.M.; Babirye, D.; Mark, D.; Ayakaka, I.; Haberer, J.E.; Katamba, A.; Armstrong-Hough, M.; Davis, J.L. Feasibility, Acceptability, and Adoption of Digital Fingerprinting During Contact Investigation for Tuberculosis in Kampala, Uganda: A Parallel-Convergent Mixed-Methods Analysis. J. Med. Internet Res. 2018, 20, e11541. [Google Scholar] [CrossRef]
- Bueno-Delgado, M.V.; Vales-Alonso, J.; Angerer, C.; Rupp, M. A comparative study of RFID schedulers in dense reader environments. In Proceedings of the 2010 IEEE International Conference on Industrial Technology, Vina del Mar, Chile, 14–17 March 2010; pp. 1373–1378. [Google Scholar]
- Martinez Perez, M.; Cabrero-Canosa, M.; Vizoso Hermida, J.; Carrajo Garcia, L.; Llamas Gomez, D.; Vazquez Gonzalez, G.; Martin Herranz, I. Application of RFID technology in patient tracking and medication traceability in emergency care. J. Med. Syst. 2012, 36, 3983–3993. [Google Scholar] [CrossRef] [PubMed]
- Pateriya, R.; Sharma, S. The evolution of RFID security and privacy: A research survey. In Proceedings of the 2011 International Conference on Communication Systems and Network Technologies, Jammu, India, 3–5 June 2011; pp. 115–119. [Google Scholar]
- Vidhyapriya, R.; Lovelyn Rose, S. Personal Authentication Mechanism Based on Finger Knuckle Print. J. Med. Syst. 2019, 43, 232. [Google Scholar] [CrossRef]
- Etter, L.P.; Ragan, E.J.; Campion, R.; Martinez, D.; Gill, C.J. Ear biometrics for patient identification in global health: A field study to test the effectiveness of an image stabilization device in improving identification accuracy. BMC Med. Inf. Decis. Mak. 2019, 19, 114. [Google Scholar] [CrossRef]
| Authors | Year | Design | Sample Size | Sample Characteristics | Quality Assessment a | Bias b | Technique/System | Specifications | Application |
|---|---|---|---|---|---|---|---|---|---|
| Anne et al. [15] | 2020 | Longitudinal study | 8794 | Patients | *** | - | Iris scanner | Binocular iris recognition cameras (SMITech model BMT-20) | Patient identification for routine HIV program data for surveillance |
| Cao et al. [16] | 2014 | Case study | 13 | IT personnel | ** | B | Active RFID tags | Battery-powered fixed receivers; mobile, battery-powered RFID beacons placed on badges | Personnel RTLS |
| Chang et al. [17] | 2011 | Pilot study | n.a. | n.a. | ** | B | Active RFID tags | Four active RFID tags (125 kHz) and two tag readers | Identification of ICU staff to trace contact history of caregivers at the ICU with patients |
| Chen et al. [18] | 2013 | Pilot study | n.a. | n.a. | ** | B | Active RFID tags | Active RFID with far-field communication (UHF 865–928 MHZ) with compact readers | Patient identification for tracking during hospital stay |
| Fisher et al. [19] | 2012 | Qualitative study | 80 interviews and 23 hospitals | Interviews and hospitals | ** | B | RTLS | RFID, WiFi, Wireless Local Area Network (WLAN), Ultra-Wide Band (UWB), infrared (IR), Zig-Bee, Bluetooth, or ultrasound (US) | Patient identification/tracking or personnel tracking in a.o.surgery, delivering medicine, and general hospital setting |
| Frisby et al. [20] | 2016 | Cross-sectional study | n.a. | n.a. | *** | - | Active RFID tags | Active RFID tags on badges (Bluetooth low energy beacon) and Raspberry Pi in rooms | Personnel attendance to patients to compute door to doctor time at the emergency department |
| Hsu et al. [21] | 2016 | Cross-sectional study | 3 per test | 1 patient, 2 healthcare workers | * | A* | Active RFID tags | Active RFID tags with 3 active antennas | Location confirmation by RTLS to authorize X-ray use |
| Jeong et al. [22] | 2017 | Criterion validation study | 25 | 25 neuroscience patients | ** | B | Infrared (IR) transmitting badges | Infrared (IR) transmitting badges that are detected by ceiling sensors | Real-time location tracking for patients during 2 min walking test in the Neuroscience Acute Care/Brain Rescue Unit |
| Jeon et al. [23] | 2019 | Case study | 30 | Patients | *** | B | Face recognition | Self-developed app on smartphone with external database | Patient identification throughout hospital stay |
| Kranzfelder et al. [24] | 2012 | Preclinical evaluation | 6 | 3 surgeons, 3 engineers | ** | B, C* | Active RFID tags | Active RFID transponder badges (2.45 GHz) with three sector antennas and one RFID sector controller | Position monitoring team members in the operating room |
| Lin et al. [25] | 2012 | Case study | 20 | medical staff | ** | B | Active RFID tags | Active RFID tags (433 MHz) in a garment, one active antenna in the room | Personnel count for air filtration optimization in the operating room |
| Liu et al. [26] | 2011 | Pilot study | Test: n.a.; survey: 174 | n.a. 56 surgeons, 41 anesthesia and recovery room nurses, 26 operative room and instrument room nurses, 30 staff of the ED | *** | C* | Active RFID tags | Active RFID wristbands (2.4 GHz) with 80m transmission and RFID readers on the ceilings | Patient identification to control the workflow for surgical patients in the operation theater |
| Odei-Lartey et al. [27] | 2016 | Cross-sectional study | n.a. | n.a. | *** | B | Fingerprint recognition | Hamster plus IV, SecuGen Inc. | Identification and registration of entering patients in a rural African setting. |
| Ohashi et al. [28] | 2010 | Feasibility study | 5 | Nurses and people pretending to be patients | ** | A*, B | Active RFID tags | RFID Power Tag from Matrix Inc. (300 MHz), with a maximum communication distance of 3000 mm | A system using RFID for reducing misidentifications of patients in a smart hospital at the University in Tokyo |
| Pérez et al. [29] | Nov. 2016 | Cross-sectional study | n.a. | n.a. | *** | B | Active RFID tags | WiFi Active Aeroscout T2 | Patient identification throughout hospital for safer medication matching |
| Pérez et al. [30] | Aug. 2016 | Case study | n.a. | n.a. | *** | B | Active RFID tags | WiFi Active Aeroscout tags | Patient tracking through hospital for efficient medication supply and safer medication matching |
| Pineles et al. [31] | 2014 | Pilot study | n.a. | n.a. | ** | B, C | Active RFID tags | Active RFID badges | Presence detection in front of soap dispenser |
| Polycarpou et al. [32] | 2012 | Observational study | n.a. | Patients in the ward | ** | B | Active RFID tags | Class 1 Generation 2 USB stick-like UHF RFID badges and wristbands | Patient identification in a hospital environment |
| Saito et al. [33] | 2013 | Case study | 20 tests with 1–4 users | Lab personnel | * | A*, B, C* | RFID | RFID tags (953 MHz UHF) in a garment combined with one active antenna per room | Presence detection in the lab |
| Steffen et al. [34] | 2010 | Cross-sectional study | n.a. | volunteers | ** | A*, B, C | Passive RFID tags | Copper etched and aluminum etched RFID tags | Identification of patients after MRI or CT scanning |
| Ting et al. [35] | 2011 | Exploratory case study | Test: 10; survey: unknown | None | ** | A*, B | RFID | n.a. | Implementation of RFID with a patient identification system in a healthcare company |
| Wall et al. [36] | 2015 | Cross-sectional study | 120, 42 | Staff members, female sex workers | ** | B, C | Fingerprint recognition | n.a. | Identification of female sex workers for HIV treatment |
| White at al. [37] | 2018 | Parallel, convergent study | 919 | Patients | *** | B | Fingerprint reader | Optical fingerprint reader | Patient identification in a tuberculosis clinic |
| Type | Cost | Usability | Accuracy | Response Time | Hygiene | Privacy | User Safety |
|---|---|---|---|---|---|---|---|
| Active | €60–€70/tag AeroScout [30] | Patients should be reminded to take tags back to the hospital [30] | 1–4 m accuracy in patient localization [21,30] | Detection by surveillance sector antenna within 30 s [24] | Non-sterilizable with an autoclave; should be packaged in a single use bag [29] | Less vulnerable to attacks by using a unique patient ID that changes over time [16] | - |
| $2.7/sqft (€26.37/m2) beacon for RTLS [16] | Older patients can lose tags [29] | Calculated entering times into room accurate to 1 s [20] | Detection of position change between 30 and 60 s [24] | ||||
| $600 (€545.31)/433 MHz reader [25] | Management of low battery in tags (collection and change) [30] | Not accurate if not worn on visible places [29] | Locating process within 20 s [21] | ||||
| $20 (€18.18)/433 MHz tag [25] | Configuration first time use (battery test, number of channels, frequency of transmission) [30] | Wrist band only detected within 5 cm of the detector [32] | Reduction of 61% of medication dispensing time compared to a regular barcode based workflow [28] | ||||
| €0.001 plastic bag for hygiene [30] | Battery life 2 weeks–6 months [16,25] | RFID tags attached to personal ID cards detected within 80 cm of the detector [32] | |||||
| €0.3 lanyards [30] | WiFi infrastructure usually already present in hospitals [21] | Detection accuracy of 52.4% [31], 82.0% [17], 85.0% [16], 98.0% [25], 100% [24] | |||||
| €18,327.11 [30]–€50,000 [25] for RTLS software | Registration area (range) has to be clearly marked [28] | Accuracy may differ by 10% between 1 and 2 readers in the room [25] | |||||
| 91.3% agreed that the system was conducive to improving patient identification [26] | Large influence of tag position on accuracy (20% decrease) [31] | ||||||
| False positives due to proximity [16,20,25,26] | |||||||
| Failure to detect when in too large or crowded areas [18] | |||||||
| 1 hospital: able to locate tag, but no room-level accuracy [19] | |||||||
| Passive | - | Showed small artifacts of 2–4 mm on MRI image [34] | - | - | - | - | - Little to no interaction in MRI [34] |
| No memory loss or data alteration of RFID tags after MRI/CT scanning [34] | |||||||
| Unspecified | - | 12% of patients forget membership card with tag [35] | Location estimated accuracy 95% [33] | - | - | - | No interference with other medical devices in cardiac intervention lab [33] |
| Usability depends on staff training and change management [35] | Accuracy independent of tag position on patient [33] | No interference with other medical devices at a distance >30 cm apart [35] | |||||
| 2 hospitals: tag not found [19] | |||||||
| 4 hospitals: able to locate tag, but no room-level accuracy [19] | |||||||
| 1 hospital: room-level accuracy [19] |
| Type | Cost | Usability | Accuracy | Response Time | Hygiene | Privacy | User Safety |
|---|---|---|---|---|---|---|---|
| Facial recognition | - | - | Sensitivity 99.7% and specificity 99.99% [23] | Verification could take from 0.5 s up to 5 min depending on lightning conditions [23] | - | - | - |
| (Partially) covered faces could not be detected [23] | |||||||
| Fingerprint recognition | - | 26% failure of the technique in capturing fingerprints [37] | Sensitivity of 65.7% [27] to 95% [36] and 100% specificity [15,25] | Average reading time 30 s [27] | - | Full acceptance rate (100%) if correctly informed [27] | - |
| Unable to capture individuals ≤ 5y old [37] | Thumb and index finger more accurate than index finger alone [36] | 50% refusal for fingerprinting based on privacy issues [37] | |||||
| Sensitivity <15% when capturing individuals ≤ 12y old [27] | False fingerprint matching 0.1% [36] | ||||||
| Iris recognition | - | 5.3% failure of technique in generating iris template or unique ID [15] | Sensitivity 94.7% [15] | Average identification time 20 s [15] | - | Technique is not used in any civil or governmental processes [15] | - |
| False match rate 0.5% [15] | 1% refusal rate due to privacy concerns [15] | ||||||
| False rejection rate 4.8% [15] |
| Type | Cost | Usability | Accuracy | Response Time | Hygiene | Privacy | User Safety |
|---|---|---|---|---|---|---|---|
| Infrared (IR) | - | - | 4.4% non-detection rate for IR based RTLS [22] | - | - | - | - |
| Detection rate: 96% [22] | |||||||
| 1 hospital: room-level accuracy [19] | |||||||
| Ultrasound (US) | - | - | 2 hospitals: able to locate tag, but no room-level accuracy [19] | - | - | - | - |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Essink, H.M.; Knops, A.; Liqui Lung, A.M.A.; van der Meulen, C.N.; Wouters, N.L.; van der Molen, A.J.; Veldkamp, W.J.H.; Termaat, M.F. Real-Time Person Identification in a Hospital Setting: A Systematic Review. Sensors 2020, 20, 3937. https://doi.org/10.3390/s20143937
Essink HM, Knops A, Liqui Lung AMA, van der Meulen CN, Wouters NL, van der Molen AJ, Veldkamp WJH, Termaat MF. Real-Time Person Identification in a Hospital Setting: A Systematic Review. Sensors. 2020; 20(14):3937. https://doi.org/10.3390/s20143937
Chicago/Turabian StyleEssink, Heleen M., Armelle Knops, Amber M.A. Liqui Lung, C. Nienke van der Meulen, Nino L. Wouters, Aart J. van der Molen, Wouter J.H. Veldkamp, and M. Frank Termaat. 2020. "Real-Time Person Identification in a Hospital Setting: A Systematic Review" Sensors 20, no. 14: 3937. https://doi.org/10.3390/s20143937
APA StyleEssink, H. M., Knops, A., Liqui Lung, A. M. A., van der Meulen, C. N., Wouters, N. L., van der Molen, A. J., Veldkamp, W. J. H., & Termaat, M. F. (2020). Real-Time Person Identification in a Hospital Setting: A Systematic Review. Sensors, 20(14), 3937. https://doi.org/10.3390/s20143937





