Smartphone App with an Accelerometer Enhances Patients’ Physical Activity Following Elective Orthopedic Surgery: A Pilot Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Population
2.3. Procedure
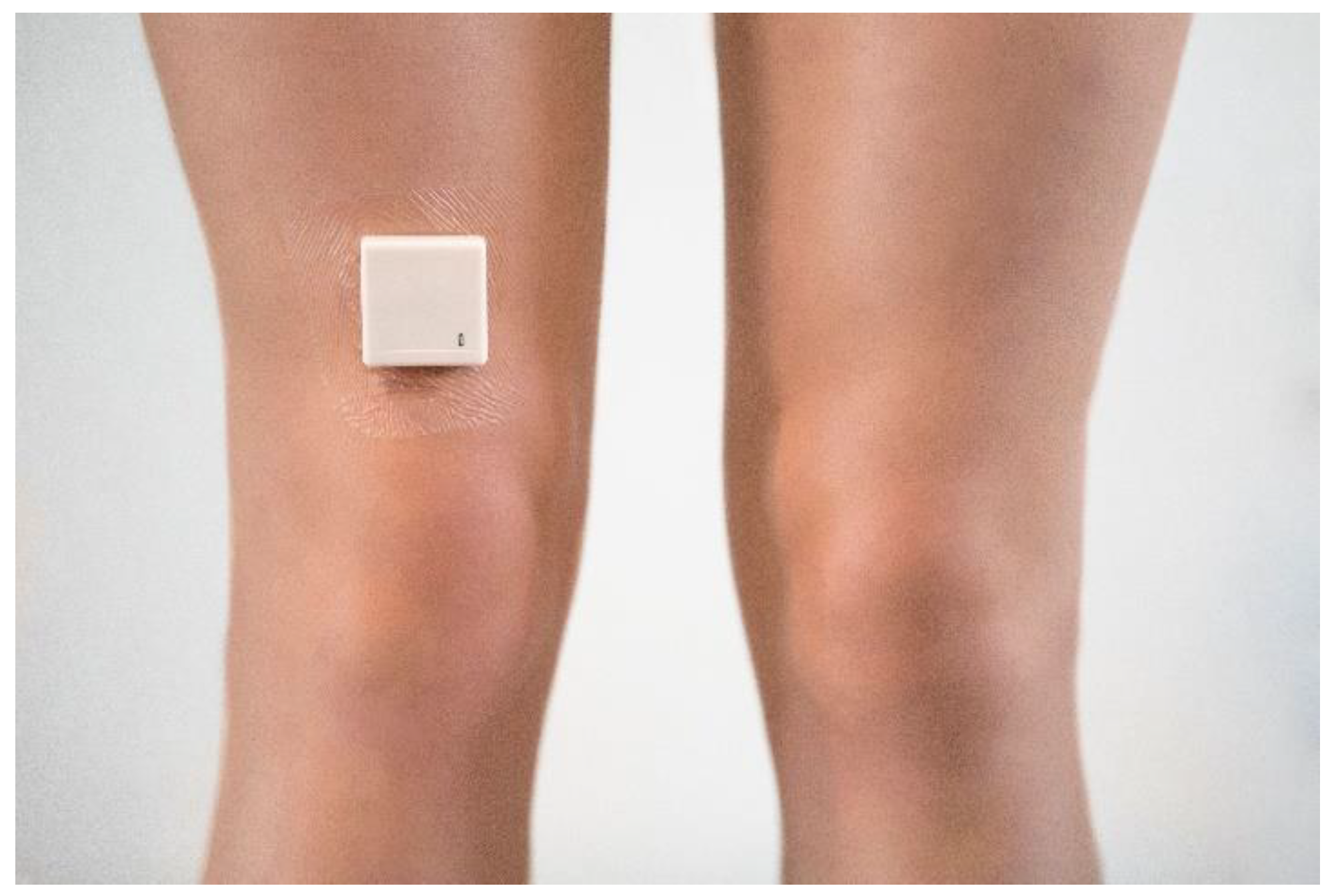
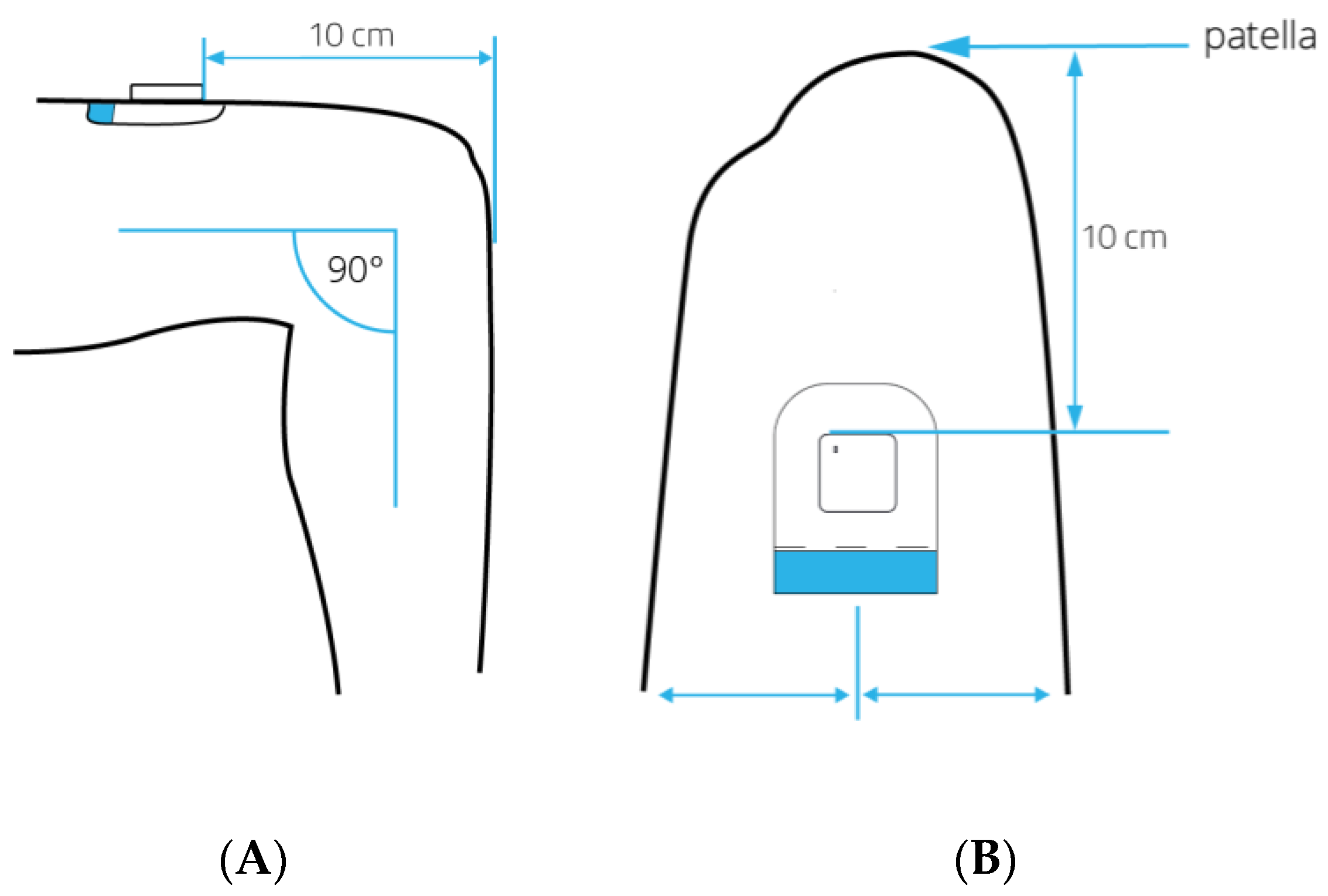
2.3.1. Device Description
2.3.2. Hospital Fit
2.4. Outcome Measures
2.4.1. Physical Activity
2.4.2. Functional Recovery
2.5. Sample Size Calculation
2.6. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Jansson, M.M.; Harjumaa, M.; Puhto, A.P.; Pikkarainen, M. Patients’ satisfaction and experiences during elective primary fast-track total hip and knee arthroplasty journey: A qualitative study. J. Clin. Nurs. 2019. [Google Scholar] [CrossRef] [PubMed]
- Berghmans, D.D.P.; Lenssen, A.F.; Emans, P.J.; de Bie, R.A. Functions, disabilities and perceived health in the first year after total knee arthroplasty; a prospective cohort study. BMC Musculoskelet. Disord. 2018, 19, 250. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, M.S.; Khan, M.A.; Nizam, I.; Haddad, F.S. Peri-operative interventions producing better functional outcomes and enhanced recovery following total hip and knee arthroplasty: An evidence-based review. BMC Med. 2013, 11, 37. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carr, A.J.; Robertsson, O.; Graves, S.; Price, A.J.; Arden, N.K.; Judge, A.; Beard, D.J. Knee replacement. Lancet 2012, 379, 1331–1340. [Google Scholar] [CrossRef]
- AJRR. 2019 Annual Report; American Academy of Orthopaedic Surgeons (AAOS): Rosemont, IL, USA, 2019. [Google Scholar]
- Soeters, R.; White, P.B.; Murray-Weir, M.; Koltsov, J.C.B.; Alexiades, M.M.; Ranawat, A.S. Preoperative physical therapy education reduces time to meet functional milestones after total joint arthroplasty. Clin. Orthop. Relat. Res. 2018, 476, 40–48. [Google Scholar] [CrossRef]
- Tanzer, D.; Smith, K.; Tanzer, M. Changing Patient expectations decreases length of stay in an enhanced recovery program for THA. Clin. Orthop. Relat. Res. 2018, 476, 372–378. [Google Scholar] [CrossRef]
- Didden, A.G.M.; Punt, I.M.; Feczko, P.Z.; Lenssen, A.F. Enhanced recovery in usual health care improves functional recovery after total knee arthroplasty. Int. J. Orthop. Trauma Nurs. 2019, 34, 9–15. [Google Scholar] [CrossRef]
- Engdal, M.; Foss, O.A.; Taraldsen, K.; Husby, V.S.; Winther, S.B. Daily Physical activity in total hip arthroplasty patients undergoing different surgical approaches: A Cohort study. Am. J. Phys. Med. Rehabil. 2017, 96, 473–478. [Google Scholar] [CrossRef]
- Den Hertog, A.; Gliesche, K.; Timm, J.; Muhlbauer, B.; Zebrowski, S. Pathway-controlled fast-track rehabilitation after total knee arthroplasty: A randomized prospective clinical study evaluating the recovery pattern, drug consumption, and length of stay. Arch. Orthop. Trauma. Surg. 2012, 132, 1153–1163. [Google Scholar] [CrossRef] [Green Version]
- Malviya, A.; Martin, K.; Harper, I.; Muller, S.D.; Emmerson, K.P.; Partington, P.F.; Reed, M.R. Enhanced recovery program for hip and knee replacement reduces death rate. Acta Orthop. 2011, 82, 577–581. [Google Scholar] [CrossRef] [Green Version]
- Brown, C.J.; Roth, D.L.; Allman, R.M. Validation of use of wireless monitors to measure levels of mobility during hospitalization. J. Rehabil. Res. Dev. 2008, 45, 551–558. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, M.M.; Bodilsen, A.C.; Petersen, J.; Beyer, N.; Andersen, O.; Lawson-Smith, L.; Kehlet, H.; Bandholm, T. Twenty-four-hour mobility during acute hospitalization in older medical patients. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2013, 68, 331–337. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Evensen, S.; Sletvold, O.; Lydersen, S.; Taraldsen, K. Physical activity among hospitalized older adults—An observational study. BMC Geriatr. 2017, 17, 110. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- So, C.; Pierluissi, E. Attitudes and expectations regarding exercise in the hospital of hospitalized older adults: A qualitative study. J. Am. Geriatr. Soc. 2012, 60, 713–718. [Google Scholar] [CrossRef]
- Hoogeboom, T.J.; Dronkers, J.J.; Hulzebos, E.H.; van Meeteren, N.L. Merits of exercise therapy before and after major surgery. Curr. Opin. Anaesthesiol. 2014, 27, 161–166. [Google Scholar] [CrossRef]
- Hoogeboom, T.J.; van Meeteren, N.L.; Schank, K.; Kim, R.H.; Miner, T.; Stevens-Lapsley, J.E. Risk factors for delayed inpatient functional recovery after total knee arthroplasty. Biomed. Res. Int. 2015, 2015, 167643. [Google Scholar] [CrossRef]
- Lenssen, A.F.; Crijns, Y.H.; Waltje, E.M.; van Steyn, M.J.; Geesink, R.J.; van den Brandt, P.A.; de Bie, R.A. Efficiency of immediate postoperative inpatient physical therapy following total knee arthroplasty: An RCT. BMC Musculoskelet. Disord. 2006, 7, 71. [Google Scholar] [CrossRef] [Green Version]
- Joosen, P.; Piette, D.; Buekers, J.; Taelman, J.; Berckmans, D.; De Boever, P. A smartphone-based solution to monitor daily physical activity in a care home. J. Telemed. Telecare 2019, 25, 611–622. [Google Scholar] [CrossRef]
- WHO. mHealth: New Horizons for Health Through Mobile Technologies; WHO: Geneva, Switzerland, 2011. [Google Scholar]
- Ureña, R.; Chiclana, F.; Gonzalez-Alvarez, A.; Herrera-Viedma, E.; Moral-Munoz, J.A. m-SFT: A novel mobile health system to assess the elderly physical condition. Sensors 2020, 20, 1462. [Google Scholar] [CrossRef] [Green Version]
- Block, V.A.; Pitsch, E.; Tahir, P.; Cree, B.A.; Allen, D.D.; Gelfand, J.M. Remote Physical activity monitoring in neurological disease: A systematic review. PLoS ONE 2016, 11, e0154335. [Google Scholar] [CrossRef]
- Thijs, I.; Fresiello, L.; Oosterlinck, W.; Sinnaeve, P.; Rega, F. Assessment of physical activity by wearable technology during rehabilitation after cardiac surgery: Explorative Prospective monocentric observational cohort study. JMIR mHealth uHealth 2019, 7, e9865. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vandelanotte, C.; Muller, A.M.; Short, C.E.; Hingle, M.; Nathan, N.; Williams, S.L.; Lopez, M.L.; Parekh, S.; Maher, C.A. Past, present, and future of eHealth and mHealth research to improve physical activity and dietary behaviors. J. Nutr. Educ. Behav. 2016, 48, 219–228. [Google Scholar] [CrossRef]
- Coughlin, S.S.; Whitehead, M.; Sheats, J.Q.; Mastromonico, J.; Smith, S. A review of smartphone applications for promoting physical activity. Jacobs J. Community Med. 2016, 2, 1–14. [Google Scholar]
- van der Weegen, S.; Verwey, R.; Spreeuwenberg, M.; Tange, H.; van der Weijden, T.; de Witte, L. It’s life! Mobile and web-based monitoring and feedback tool embedded in primary care increases physical activity: A cluster randomized controlled trial. J. Med. Internet Res. 2015, 17, e184. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feldman, D.I.; Theodore Robison, W.; Pacor, J.M.; Caddell, L.C.; Feldman, E.B.; Deitz, R.L.; Feldman, T.; Martin, S.S.; Nasir, K.; Blaha, M.J. Harnessing mHealth technologies to increase physical activity and prevent cardiovascular disease. Clin. Cardiol. 2018, 41, 985–991. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ramkumar, P.N.; Haeberle, H.S.; Ramanathan, D.; Cantrell, W.A.; Navarro, S.M.; Mont, M.A.; Bloomfield, M.; Patterson, B.M. Remote Patient monitoring using mobile health for total knee arthroplasty: Validation of a wearable and machine learning-based surveillance platform. J. Arthroplast. 2019, 34, 2253–2259. [Google Scholar] [CrossRef]
- Ramkumar, P.N.; Haeberle, H.S.; Bloomfield, M.R.; Schaffer, J.L.; Kamath, A.F.; Patterson, B.M.; Krebs, V.E. Artificial Intelligence and arthroplasty at a single institution: Real-world applications of machine learning to big data, value-based care, mobile health, and remote patient monitoring. J. Arthroplast. 2019, 34, 2204–2209. [Google Scholar] [CrossRef]
- Correia, F.D.; Nogueira, A.; Magalhães, I.; Guimarães, J.; Moreira, M.; Barradas, I.; Molinos, M.; Teixeira, L.; Tulha, J.; Seabra, R.; et al. Medium-Term outcomes of digital versus conventional home-based rehabilitation after total knee arthroplasty: Prospective, parallel-group feasibility study. JMIR Rehabil. Assist. Technol. 2019, 6, e13111. [Google Scholar] [CrossRef]
- Dorje, T.; Zhao, G.; Scheer, A.; Tsokey, L.; Wang, J.; Chen, Y.; Tso, K.; Tan, B.K.; Ge, J.; Maiorana, A. SMARTphone and social media-based Cardiac Rehabilitation and Secondary Prevention (SMART-CR/SP) for patients with coronary heart disease in China: A randomised controlled trial protocol. BMJ Open 2018, 8, e021908. [Google Scholar] [CrossRef] [Green Version]
- Chen, K.Y.; Janz, K.F.; Zhu, W.; Brychta, R.J. Redefining the roles of sensors in objective physical activity monitoring. Med. Sci. Sports Exerc. 2012, 44, 13–23. [Google Scholar] [CrossRef] [Green Version]
- Evenson, K.R.; Goto, M.M.; Furberg, R.D. Systematic review of the validity and reliability of consumer-wearable activity trackers. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 159. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bijnens, W.A.; Aarts, J.; Stevens, A.; Ummels, D.; Meijer, K. Optimization and validation of an adjustable activity classification algorithm for assessment of physical behavior in elderly. Sensors 2019, 19, 5344. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Berendsen, B.A.; Hendriks, M.R.; Meijer, K.; Plasqui, G.; Schaper, N.C.; Savelberg, H.H. Which activity monitor to use? Validity, reproducibility and user friendliness of three activity monitors. BMC Public Health 2014, 14, 749. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Annegarn, J.; Spruit, M.A.; Uszko-Lencer, N.H.; Vanbelle, S.; Savelberg, H.H.; Schols, A.M.; Wouters, E.F.; Meijer, K. Objective physical activity assessment in patients with chronic organ failure: A validation study of a new single-unit activity monitor. Arch. Phys. Med. Rehabil. 2011, 92, 1852–1857. [Google Scholar] [CrossRef] [PubMed]
- Manas, A.; Del Pozo-Cruz, B.; Garcia-Garcia, F.J.; Guadalupe-Grau, A.; Ara, I. Role of objectively measured sedentary behaviour in physical performance, frailty and mortality among older adults: A short systematic review. Eur. J. Sport Sci. 2017, 17, 940–953. [Google Scholar] [CrossRef] [PubMed]
- Shields, R.K.; Enloe, L.J.; Evans, R.E.; Smith, K.B.; Steckel, S.D. Reliability, validity, and responsiveness of functional tests in patients with total joint replacement. Phys. Ther. 1995, 75, 169–176. [Google Scholar] [CrossRef] [PubMed]
- Bercken, V.e.V.d. Lineaire Regressieanalyse, 1st ed.; Noordhoff Uitgevers bv: Groningen/Houten, The Netherlands, 2010. [Google Scholar]
- Twisk, J.W.R. Inleiding in de Toegepaste Biostatistiek, 2nd ed.; Elsevier Gezondheidszorg: Maarssen, The Netherlands, 2010. [Google Scholar]
- Fisher, S.R.; Goodwin, J.S.; Protas, E.J.; Kuo, Y.F.; Graham, J.E.; Ottenbacher, K.J.; Ostir, G.V. Ambulatory activity of older adults hospitalized with acute medical illness. J. Am. Geriatr. Soc. 2011, 59, 91–95. [Google Scholar] [CrossRef] [Green Version]
- Ostir, G.V.; Berges, I.M.; Kuo, Y.F.; Goodwin, J.S.; Fisher, S.R.; Guralnik, J.M. Mobility activity and its value as a prognostic indicator of survival in hospitalized older adults. J. Am. Geriatr. Soc. 2013, 61, 551–557. [Google Scholar] [CrossRef] [Green Version]
- Brown, C.J.; Williams, B.R.; Woodby, L.L.; Davis, L.L.; Allman, R.M. Barriers to mobility during hospitalization from the perspectives of older patients and their nurses and physicians. J. Hosp. Med. 2007, 2, 305–313. [Google Scholar] [CrossRef] [Green Version]
- Koenders, N.; van Oorsouw, R.; Seeger, J.P.H.; Nijhuis-van der Sanden, M.W.G.; van de Glind, I.; Hoogeboom, T.J. “I’m not going to walk, just for the sake of walking…”: A qualitative, phenomenological study on physical activity during hospital stay. Disabil. Rehabil. 2018, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Small, S.R.; Bullock, G.S.; Khalid, S.; Barker, K.; Trivella, M.; Price, A.J. Current clinical utilisation of wearable motion sensors for the assessment of outcome following knee arthroplasty: A scoping review. BMJ Open 2019, 9, e033832. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brønd, J.C.; Arvidsson, D. Sampling frequency affects the processing of Actigraph raw acceleration data to activity counts. J. Appl. Physiol. 2016, 120, 362–369. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Godfrey, A.; Hetherington, V.; Shum, H.; Bonato, P.; Lovell, N.H.; Stuart, S. From A to Z: Wearable technology explained. Maturitas 2018, 113, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Clark, C.C.T.; Nobre, G.C.; Fernandes, J.F.T.; Moran, J.; Drury, B.; Mannini, A.; Gronek, P.; Podstawski, R. Physical activity characterization: Does one site fit all? Physiol. Meas. 2018, 39, 09TR02. [Google Scholar] [CrossRef] [PubMed]
- Matthews, C.E.; Hagströmer, M.; Pober, D.M.; Bowles, H.R. Best practices for using physical activity monitors in population-based research. Med. Sci. Sports Exerc. 2012, 44, 68–76. [Google Scholar] [CrossRef] [Green Version]
- Schotanus, M.G.M.; Bemelmans, Y.F.L.; Grimm, B.; Heyligers, I.C.; Kort, N.P. Physical activity after outpatient surgery and enhanced recovery for total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 3366–3371. [Google Scholar] [CrossRef]
- Fenten, M.G.E.; Bakker, S.M.K.; Scheffer, G.J.; Wymenga, A.B.; Stienstra, R.; Heesterbeek, P.J.C. Femoral nerve catheter vs. local infiltration for analgesia in fast track total knee arthroplasty: Short-term and long-term outcomes. Br. J. Anaesth. 2018, 121, 850–858. [Google Scholar] [CrossRef] [Green Version]
- Luna, I.E.; Kehlet, H.; Wede, H.R.; Hoevsgaard, S.J.; Aasvang, E.K. Objectively measured early physical activity after total hip or knee arthroplasty. J. Clin. Monit. Comput. 2019, 33, 509–522. [Google Scholar] [CrossRef]
- Krenk, L.; Jennum, P.; Kehlet, H. Activity, sleep and cognition after fast-track hip or knee arthroplasty. J. Arthroplast. 2013, 28, 1265–1269. [Google Scholar] [CrossRef]
- Tsuji, S.; Tomita, T.; Fujii, M.; Laskin, R.S.; Yoshikawa, H.; Sugamoto, K. Is minimally invasive surgery-total knee arthroplasty truly less invasive than standard total knee arthroplasty? A quantitative evaluation. J. Arthroplast. 2010, 25, 970–976. [Google Scholar] [CrossRef]
- Hayashi, K.; Kako, M.; Suzuki, K.; Takagi, Y.; Terai, C.; Yasuda, S.; Kadono, I.; Seki, T.; Hiraiwa, H.; Ushida, T.; et al. Impact of variation in physical activity after total joint replacement. J. Pain Res. 2018, 11, 2399–2406. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Twiggs, J.; Salmon, L.; Kolos, E.; Bogue, E.; Miles, B.; Roe, J. Measurement of physical activity in the pre- and early post-operative period after total knee arthroplasty for Osteoarthritis using a Fitbit Flex device. Med. Eng. Phys. 2018, 51, 31–40. [Google Scholar] [CrossRef]
- Bassett, D.R.; John, D. Use of pedometers and accelerometers in clinical populations: Validity and reliability issues. Phys. Ther. Rev. 2010, 15, 135–142. [Google Scholar] [CrossRef]
- Peel, N.M.; Kuys, S.S.; Klein, K. Gait speed as a measure in geriatric assessment in clinical settings: A systematic review. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2013, 68, 39–46. [Google Scholar] [CrossRef] [PubMed]
- Floegel, T.A.; Florez-Pregonero, A.; Hekler, E.B.; Buman, M.P. Validation of consumer-based hip and wrist activity monitors in older adults with varied ambulatory abilities. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2017, 72, 229–236. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beevi, F.H.; Miranda, J.; Pedersen, C.F.; Wagner, S. An evaluation of commercial pedometers for monitoring slow walking speed populations. Telemed. J. E Health 2016, 22, 441–449. [Google Scholar] [CrossRef]
- Martin, J.B.; Krč, K.M.; Mitchell, E.A.; Eng, J.J.; Noble, J.W. Pedometer accuracy in slow walking older adults. Int. J. Ther. Rehabil. 2012, 19, 387–393. [Google Scholar] [CrossRef] [Green Version]
- Cyarto, E.V.; Myers, A.; Tudor-Locke, C. Pedometer accuracy in nursing home and community-dwelling older adults. Med. Sci. Sports Exerc. 2004, 36, 205–209. [Google Scholar] [CrossRef]
- Argent, R.; Slevin, P.; Bevilacqua, A.; Neligan, M.; Daly, A.; Caulfield, B. Clinician perceptions of a prototype wearable exercise biofeedback system for orthopaedic rehabilitation: A qualitative exploration. BMJ Open 2018, 8, e026326. [Google Scholar] [CrossRef] [Green Version]
- Argent, R.; Slevin, P.; Bevilacqua, A.; Neligan, M.; Daly, A.; Caulfield, B. Wearable sensor-based exercise biofeedback for orthopaedic rehabilitation: A mixed methods user evaluation of a prototype system. Sensors 2019, 19, 432. [Google Scholar] [CrossRef] [Green Version]
- Kayaalp, M.E.; Agres, A.N.; Reichmann, J.; Bashkuev, M.; Duda, G.N.; Becker, R. Validation of a novel device for the knee monitoring of orthopaedic patients. Sensors 2019, 19, 5193. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brennan, L.; Dorronzoro Zubiete, E.; Caulfield, B. Feedback design in targeted exercise digital biofeedback systems for home rehabilitation: A scoping review. Sensors 2019, 20, 181. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bell, K.M.; Onyeukwu, C.; McClincy, M.P.; Allen, M.; Bechard, L.; Mukherjee, A.; Hartman, R.A.; Smith, C.; Lynch, A.D.; Irrgang, J.J. Verification of a portable motion tracking system for remote management of physical rehabilitation of the knee. Sensors 2019, 19, 21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chiang, C.Y.; Chen, K.H.; Liu, K.C.; Hsu, S.J.; Chan, C.T. Data Collection and analysis using wearable sensors for monitoring knee range of motion after total knee arthroplasty. Sensors 2017, 17, 418. [Google Scholar] [CrossRef] [PubMed]
- Msayib, Y.; Gaydecki, P.; Callaghan, M.; Dale, N.; Ismail, S. An Intelligent remote monitoring system for total knee arthroplasty patients. J. Med. Syst. 2017, 41, 90. [Google Scholar] [CrossRef] [PubMed]
- O’Reilly, M.; Caulfield, B.; Ward, T.; Johnston, W.; Doherty, C. Wearable Inertial Sensor Systems for Lower Limb Exercise Detection and Evaluation: A Systematic Review. Sports Medicine (Auckland N. Z.) 2018, 48, 1221–1246. [Google Scholar] [CrossRef] [Green Version]
- Peake, J.M.; Kerr, G.; Sullivan, J.P. A critical review of consumer wearables, mobile applications, and equipment for providing biofeedback, monitoring stress, and sleep in physically active populations. Front. Physiol. 2018, 9, 743. [Google Scholar] [CrossRef]





| Control Group (n = 64) | Intervention Group (n = 33) | |
|---|---|---|
| Age, years (median, IQR) | 66.60 (10.62) | 65.10 (13.72) |
| Sex (n, %) | ||
| Female | 24 (38) | 18 (55) |
| Male | 40 (63) | 15 (45) |
| BMI, kg/m2 (median, IQR) | 27.73 (4.72) | 27.47 (4.70) |
| Type of surgery (n, %): | ||
| Total knee arthroplasty | 49 (77) | 15 (45) |
| Total hip arthroplasty | 15 (23) | 18 (55) |
| ASA-class (n, %): | ||
| ASA 1–2 | 53 (83) | 26 (79) |
| ASA 3 | 11 (17) | 7 (21) |
| Walking aid (n, %): | ||
| Two crutches | 53 (83) | 31 (94) |
| One crutch | 1 (2) | - |
| Walking frame | 5 (8) | 1 (3) |
| Walker | 5 (8) | 1 (3) |
| LOS, days (median, IQR) | 3.00 (1) | 3.00 (0) |
| B | Std. Error | p-Value | 95% Confidence Interval for B | ||
|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||
| Constant | 70.89 | 5.98 | 0.000 | 59.00 | 82.80 |
| Hospital Fit use | 32.10 | 11.43 | 0.006 | 9.35 | 54.84 |
| B | Std. Error | p-Value | 95% Confidence Interval for B | ||
|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||
| Constant | 124.25 | 31.80 | 0.000 | 60.98 | 187.52 |
| Hospital Fit use | 28.43 | 11.50 | 0.016 | 5.55 | 51.32 |
| Age | −0.81 | 0.48 | 0.092 | −1.76 | 0.13 |
| B | Std. Error | p-Value | Odds Ratio | 95% Confidence Interval for Odds Ratio | ||
|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | |||||
| Constant | −0.31 | 0.26 | 0.243 | 0.735 | - | - |
| Hospital Fit use | 1.00 | 0.49 | 0.039 | 2.720 | 1.050 | 7.049 |
| B | Std. Error | p-Value | Odds Ratio | 95% Confidence Interval for Odds Ratio | ||
|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | |||||
| Constant | −0.91 | 0.58 | 0.112 | 0.401 | - | - |
| Hospital Fit use | 1.13 | 0.51 | 0.026 | 3.080 | 1.14 | 8.31 |
| ASA-class | 0.71 | 0.59 | 0.228 | 2.03 | 0.64 | 6.39 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
van Dijk-Huisman, H.C.; Weemaes, A.T.R.; Boymans, T.A.E.J.; Lenssen, A.F.; de Bie, R.A. Smartphone App with an Accelerometer Enhances Patients’ Physical Activity Following Elective Orthopedic Surgery: A Pilot Study. Sensors 2020, 20, 4317. https://doi.org/10.3390/s20154317
van Dijk-Huisman HC, Weemaes ATR, Boymans TAEJ, Lenssen AF, de Bie RA. Smartphone App with an Accelerometer Enhances Patients’ Physical Activity Following Elective Orthopedic Surgery: A Pilot Study. Sensors. 2020; 20(15):4317. https://doi.org/10.3390/s20154317
Chicago/Turabian Stylevan Dijk-Huisman, Hanneke C., Anouk T.R. Weemaes, Tim A.E.J. Boymans, Antoine F. Lenssen, and Rob A. de Bie. 2020. "Smartphone App with an Accelerometer Enhances Patients’ Physical Activity Following Elective Orthopedic Surgery: A Pilot Study" Sensors 20, no. 15: 4317. https://doi.org/10.3390/s20154317
APA Stylevan Dijk-Huisman, H. C., Weemaes, A. T. R., Boymans, T. A. E. J., Lenssen, A. F., & de Bie, R. A. (2020). Smartphone App with an Accelerometer Enhances Patients’ Physical Activity Following Elective Orthopedic Surgery: A Pilot Study. Sensors, 20(15), 4317. https://doi.org/10.3390/s20154317





