Identifying Fatigue Indicators Using Gait Variability Measures: A Longitudinal Study on Elderly Brisk Walking
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Equipment and Experimental Procedures
2.3. Data Processing
- Extract the data of the baseline min, 30th min, and 60th min, and incomplete gait cycles are ignored.
- Calculate these 10 parameters of each gait cycle in these three time periods, then calculate the average value for each parameter.
- Normalize by dividing each participant’s baseline-min, 30th-min, and 60th-min data by their respective baseline-min data to get the proportion of change of each parameter relative to the baseline, thereby eliminating the difference in gait parameters between the experiments. The units of each parameter are 1 since each parameter uses a ratio.
2.4. Statistical Analysis
3. Results
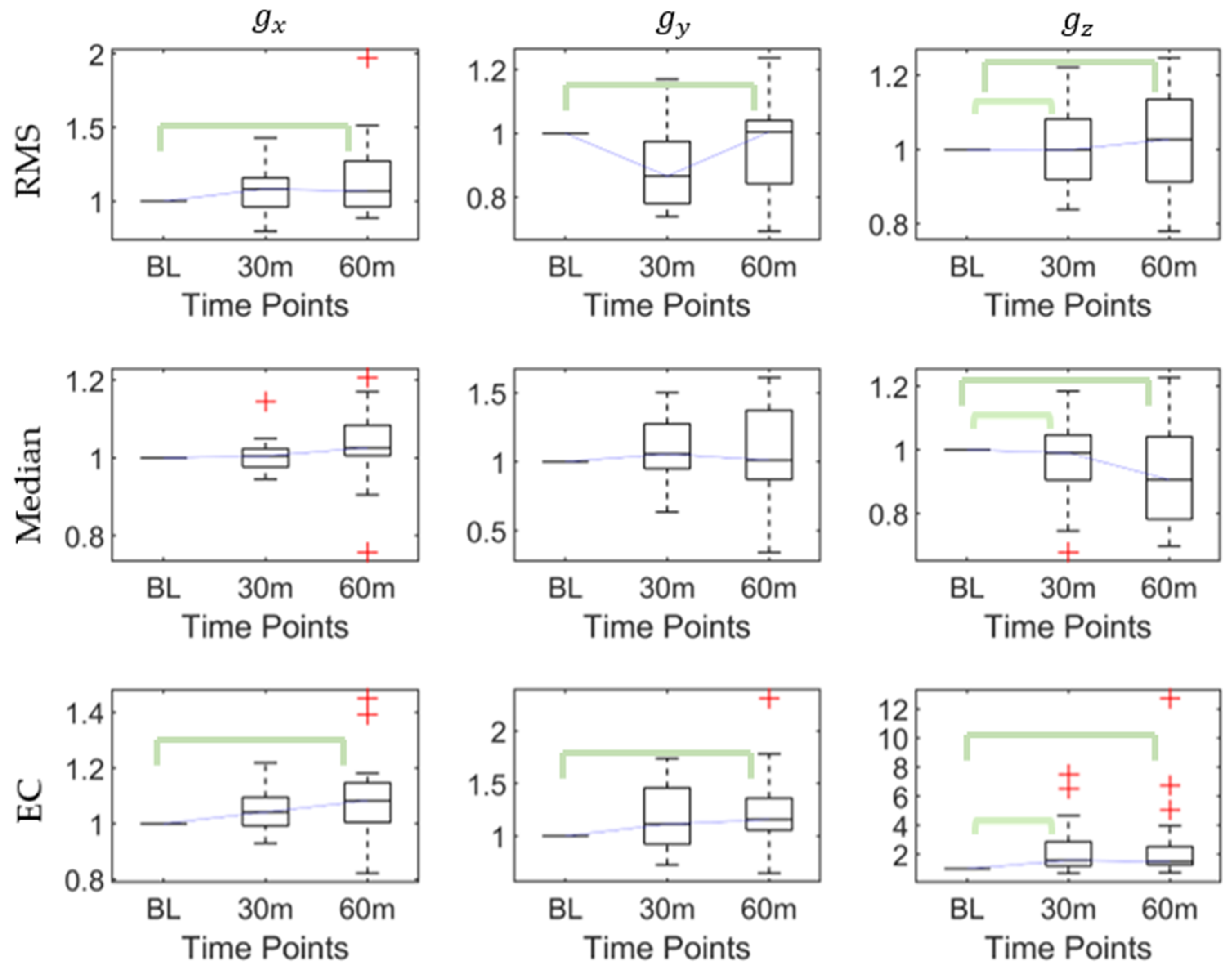
3.1. Influence of Walking Time (Fatigue) on Posterior Heel Acceleration
3.2. Influence of Walking Time (Fatigue) on Posterior Heel Angular Velocity
3.3. Influence of Walking Time (Fatigue) on Posterior Heel Orientation (Rotation Angle)
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Thomas, E.; Battaglia, G.; Patti, A.; Brusa, J.; Leonardi, V.; Palma, A.; Bellafiore, M. Physical activity programs for balance and fall prevention in elderly: A systematic review. Medicine 2019, 98, 16218. [Google Scholar] [CrossRef] [PubMed]
- Paterson, D.H.; Warburton, D.E. Physical activity and functional limitations in older adults: A systematic review related to Canada’s Physical Activity Guidelines. Int. J. Behav. Nutr. Phys. Act. 2010, 7, 1–22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Committee, P.A.G.A. Physical Activity Guidelines Advisory Committee Report, 2008; US Department of Health and Human Services: Washington, DC, USA, 2008; pp. A1–H14.
- Paterson, D.H.; Jones, G.R.; Rice, C.L. Ageing and physical activity: Evidence to develop exercise recommendations for older adults. Appl. Physiol. Nutr. Metab. 2007, 32, S69–S108. [Google Scholar] [CrossRef] [Green Version]
- Global Recommendations on Physical Activity for Health. Available online: https://www.who.int/dietphysicalactivity/global-PA-recs-2010.pdf (accessed on 6 December 2020).
- Chastin, S.; De Craemer, M.; De Cocker, K.; Powell, L.; Van Cauwenberg, J.; Dall, P.; Hamer, M.; Stamatakis, E. How does light-intensity physical activity associate with adult cardiometabolic health and mortality? Systematic review with meta-analysis of experimental and observational studies. Br. J. Sports Med. 2019, 53, 370–376. [Google Scholar] [CrossRef] [Green Version]
- Aranyavalai, T.; Jalayondeja, C.; Jalayondeja, W.; Pichaiyongwongdee, S.; Kaewkungwal, J.; Laskin, J.J. Association between walking 5000 step/day and fall incidence over six months in urban community-dwelling older people. BMC Geriatr. 2020, 20, 194. [Google Scholar] [CrossRef] [PubMed]
- Tudor-Locke, C.; Craig, C.L.; Aoyagi, Y.; Bell, R.C.; A Croteau, K.; De Bourdeaudhuij, I.; Ewald, B.; Gardner, A.; Hatano, Y.; Lutes, L.D.; et al. How many steps/day are enough? For older adults and special populations. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 80. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tirosh, O.; Sparrow, W. Age and walking speed effects on muscle recruitment in gait termination. Gait Posture 2005, 21, 279–288. [Google Scholar] [CrossRef]
- Nagano, H.; James, L.; Sparrow, W.; Begg, R.K. Effects of walking-induced fatigue on gait function and tripping risks in older adults. J. Neuroeng. Rehabil. 2014, 11, 155. [Google Scholar] [CrossRef] [Green Version]
- Bruijn, S.M.; Meijer, O.G.; Beek, P.J.; Van Dieën, J.H. Assessing the stability of human locomotion: A review of current measures. J. R. Soc. Interface 2013, 10, 20120999. [Google Scholar] [CrossRef]
- Elhadi, M.M.; Ma, C.Z.-H.; Wong, D.W.-C.; Wan, A.H.; Lee, W.C.-C. Comprehensive Gait Analysis of Healthy Older Adults Who Have Undergone Long-Distance Walking. J. Aging Phys. Act. 2017, 25, 367–377. [Google Scholar] [CrossRef]
- Wong, D.W.-C.; Lam, W.-K.; Lee, W.C.-C. Gait asymmetry and variability in older adults during long-distance walking: Implications for gait instability. Clin. Biomech. 2020, 72, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.-H.; Lin, C.-B.; Chen, Y.; Chen, W.; Huang, T.-S.; Hsu, C.-Y. An EMG Patch for the Real-Time Monitoring of Muscle-Fatigue Conditions During Exercise. Sensors 2019, 19, 3108. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moniri, A.; Terracina, D.; Rodriguez-Manzano, J.; Strutton, P.H.; Georgiou, P. Real-Time Forecasting of sEMG Features for Trunk Muscle Fatigue using Machine Learning. IEEE Trans. Biomed. Eng. 2020. [Google Scholar] [CrossRef] [PubMed]
- de Oliveira, C.F.; Soares, D.P.; Bertani, M.C.; Rodrigues, L.J.; Vila-boas, J.P. Effects of Fast-Walking on Muscle Activation in Young Adults and Elderly Persons. J. Novel Physiother. Rehabil. 2017, 1, 012–019. [Google Scholar]
- Buckley, C.; O’Reilly, M.; Whelan, D.; Farrell, A.V.; Clark, L.; Longo, V.; Gilchrist, M.; Caulfield, B. Binary classification of running fatigue using a single inertial measurement unit. In Proceedings of the 2017 IEEE 14th International Conference on Wearable and Implantable Body Sensor Networks (BSN), Eindhoven, The Netherlands, 9–12 May 2017; pp. 197–201. [Google Scholar]
- Zhang, J.; Lockhart, T.E.; Soangra, R. Classifying Lower Extremity Muscle Fatigue During Walking Using Machine Learning and Inertial Sensors. Ann. Biomed. Eng. 2014, 42, 600–612. [Google Scholar] [CrossRef] [Green Version]
- Hu, B.; Dixon, P.; Jacobs, J.; Dennerlein, J.; Schiffman, J. Machine learning algorithms based on signals from a single wearable inertial sensor can detect surface- and age-related differences in walking. J. Biomech. 2018, 71, 37–42. [Google Scholar] [CrossRef]
- Ma, C.Z.-H.; Wong, D.W.-C.; Lam, W.-K.; Wan, A.H.-P.; Lee, W.C.-C. Balance Improvement Effects of Biofeedback Systems with State-of-the-Art Wearable Sensors: A Systematic Review. Sensors 2016, 16, 434. [Google Scholar] [CrossRef] [Green Version]
- Seeley, M.K.; Umberger, B.R.; Shapiro, R. A test of the functional asymmetry hypothesis in walking. Gait Posture 2008, 28, 24–28. [Google Scholar] [CrossRef] [PubMed]
- Grami, A. Signals, Systems, and Spectral Analysis. In Introduction to Digital Communications; Springer: New York, NY, USA, 2007; pp. 41–150. [Google Scholar]
- Barry, D.T.; Hill, T.; Im, D. Muscle fatigue measured with evoked muscle vibrations. Muscle Nerve Off. J. Am. Assoc. Electrodiagn. Med. 1992, 15, 303–309. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bhat, P.; Gupta, A. A novel approach to detect localized muscle fatigue during isometric exercises. In Proceedings of the 2016 IEEE 13th International Conference on Wearable and Implantable Body Sensor Networks (BSN), San Francisco, CA, USA, 14–17 June 2016. [Google Scholar]
- Hausdorff, J.M.; Rios, D.A.; Edelberg, H.K. Gait variability and fall risk in community-living older adults: A 1-year prospective study. Arch. Phys. Med. Rehabil. 2001, 82, 1050–1056. [Google Scholar] [CrossRef] [PubMed]
- Thies, B.S.; Richardson, J.K.; Ashton-Miller, J.A. Effects of surface irregularity and lighting on step variability during gait: A study in healthy young and older women. Gait Posture 2005, 22, 26–31. [Google Scholar] [CrossRef] [PubMed]
- Hamacher, D.; Singh, N.; Van Dieën, J.; Heller, M.; Taylor, W.R. Kinematic measures for assessing gait stability in elderly individuals: A systematic review. J. R. Soc. Interface 2011, 8, 1682–1698. [Google Scholar] [CrossRef] [PubMed]
- Woledge, R.C.; Birtles, D.; Newham, D.J. The Variable Component of Lateral Body Sway During Walking in Young And Older Humans. J. Gerontol. Ser. A Boil. Sci. Med. Sci. 2005, 60, 1463–1468. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Owings, T.M.; Grabiner, M.D. Step width variability, but not step length variability or step time variability, discriminates gait of healthy young and older adults during treadmill locomotion. J. Biomech. 2004, 37, 935–938. [Google Scholar] [CrossRef]
- Owings, T.M.; Grabiner, M.D. Variability of step kinematics in young and older adults. Gait Posture 2004, 20, 26–29. [Google Scholar] [CrossRef]
- Maki, B.E. Gait Changes in Older Adults: Predictors of Falls or Indicators of Fear? J. Am. Geriatr. Soc. 1997, 45, 313–320. [Google Scholar] [CrossRef]
- Brach, J.S.; Talkowski, J.B.; VanSwearingen, J.; Newman, A.B.; Studenski, S.A. Too much or too little step width variability is associated with a fall history in older persons who walk at or near normal gait speed. J. Neuroeng. Rehabil. 2005, 2, 21. [Google Scholar] [CrossRef] [Green Version]
- Chizewski, M.G.; Chiu, L.Z.F. Contribution of calcaneal and leg segment rotations to ankle joint dorsiflexion in a weight-bearing task. Gait Posture 2012, 36, 85–89. [Google Scholar] [CrossRef]
- Modarresi, S.; Divine, A.; Grahn, J.A.; Overend, T.J.; Hunter, S.W. Gait parameters and characteristics associated with increased risk of falls in people with dementia: A systematic review. Int. Psychogeriatr. 2018, 31, 1287–1303. [Google Scholar] [CrossRef]
- Morris, M.E.; Vermeulen, M.; Van Oers, M.H. Changes in gait and fatigue from morning to afternoon in people with multiple sclerosis. J. Neurol. Neurosurg. Psychiatry 2002, 72, 361–365. [Google Scholar] [CrossRef] [Green Version]
- Tong, J.W.; Kong, P.W. Association Between Foot Type and Lower Extremity Injuries: Systematic Literature Review With Meta-analysis. J. Orthop. Sports Phys. Ther. 2013, 43, 700–714. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jafarnezhadgero, A.; Alavi-Mehr, S.M.; Granacher, U. Effects of anti-pronation shoes on lower limb kinematics and kinetics in female runners with pronated feet: The role of physical fatigue. PLoS ONE 2019, 14, e0216818. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, J.C.; Alexander, I.J.; Hayes, K.C. Nerve supply of the human knee and its functional importance. Am. J. Sports Med. 1982, 10, 329–335. [Google Scholar] [CrossRef]
- Baratta, R.; Solomonow, M.; Zhou, B.H.; Letson, D.; Chuinard, R.; D’ambrosia, R. Muscular coactivation: The role of the antagonist musculature in maintaining knee stability. Am. J. Sports Med. 1988, 16, 113–122. [Google Scholar] [CrossRef] [PubMed]
- Johnston, R., 3rd; Howard, M.E.; Cawley, P.W.; Losse, G.M. Effect of lower extremity muscular fatigue on motor control performance. Med. Sci. Sports Exerc. 1998, 30, 1703–1707. [Google Scholar] [CrossRef] [PubMed]
- Ma, C.Z.-H.; Wong, D.W.-C.; Wan, A.H.-P.; Lee, W.C.-C. Effects of orthopedic insoles on static balance of older adults wearing thick socks. Prosthet. Orthot. Int. 2018, 42, 357–362. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, C.-H.; Chen, S.-H.; Jiang, B.C.; Sun, T.-L. Estimating Postural Stability Using Improved Permutation Entropy via TUG Accelerometer Data for Community-Dwelling Elderly People. Entropy 2020, 22, 1097. [Google Scholar] [CrossRef]
- Finsterer, J.; Mahjoub, S.Z. Fatigue in Healthy and Diseased Individuals. Am. J. Hosp. Palliat. Med. 2014, 31, 562–575. [Google Scholar] [CrossRef]
- Chen, T.L.-W.; Wong, D.W.-C.; Wang, Y.; Tan, Q.; Lam, W.-K.; Zhang, M. Changes in segment coordination variability and the impacts of the lower limb across running mileages in half marathons: Implications for running injuries. J. Sport Health Sci. 2020. [Google Scholar] [CrossRef]
- Wong DW, C.; Lam, W.K.; Yeung, L.F.; Lee, W.C. Does long-distance walking improve or deteriorate walking stability of transtibial amputees? Clin. Biomech. 2015, 30, 867–873. [Google Scholar] [CrossRef]
- Huang, C.L.-C.; Hsu, S.-Y.; Lin, E. A comparison of classification methods for predicting Chronic Fatigue Syndrome based on genetic data. J. Transl. Med. 2009, 7, 81. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arab, A.M.; Salavati, M.; Ebrahimi, I.; Mousavi, M.E. Sensitivity, specificity and predictive value of the clinical trunk muscle endurance tests in low back pain. Clin. Rehabil. 2007, 21, 640–647. [Google Scholar] [CrossRef] [PubMed]
- Peng, Y.; Wong, D.W.-C.; Wang, Y.; Chen, T.L.-W.; Tan, Q.; Chen, Z.; Jin, Z.-M.; Zhang, M. Immediate Effects of Medially Posted Insoles on Lower Limb Joint Contact Forces in Adult Acquired Flatfoot: A Pilot Study. Int. J. Environ. Res. Public Health 2020, 17, 2226. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tan, Q.; Wang, Y.; Chen, T.L.-W.; Wong, D.W.-C.; Yan, F.; Li, Z.; Zhang, M. Exercise-Induced Hemodynamic Changes in Muscle Tissue: Implication of Muscle Fatigue. Appl. Sci. 2020, 10, 3512. [Google Scholar] [CrossRef]
- Coviello, G.; Avitabile, G. Multiple Synchronized Inertial Measurement Unit Sensor Boards Platform for Activity Monitoring. IEEE Sens. J. 2020, 20, 8771–8777. [Google Scholar] [CrossRef]
- Rucksana, S.; Babu, C.; Saranyabharathi, S. Efficient timing-sync protocol in wireless sensor network. In Proceedings of the 2015 International Conference on Innovations in Information, Embedded and Communication Systems (ICIIECS), Trivandrum, India, 16–19 December 2015. [Google Scholar]
- Ma, C.Z.-H.; Wan, A.H.-P.; Wong, D.W.-C.; Zheng, Y.-P.; Lee, W.C.-C. A Vibrotactile and Plantar Force Measurement-Based Biofeedback System: Paving the Way towards Wearable Balance-Improving Devices. Sensors 2015, 15, 31709–31722. [Google Scholar] [CrossRef] [Green Version]
- Lambert, E.; Gibson, A.S.C.; Noakes, T. Complex systems model of fatigue: Integrative homoeostatic control of peripheral physiological systems during exercise in humans. Br. J. Sports Med. 2005, 39, 52–62. [Google Scholar] [CrossRef] [Green Version]



| Parameters | Range | Stability | Transmission Frequency |
|---|---|---|---|
| Acceleration | ±16 g | 0.01 g | 50 Hz |
| Angle | X/Z: ±180° Y: ±90° | 0.05° | 50 Hz |
| Angular Velocity | ±2000°/s | 0.05°/s | 50 Hz |
| Features | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| MAD | 0.113 | 0.056 | 0.494 | 0.327 | 0.662 | 0.390 | 0.327 | 0.943 | 0.662 |
| Kurtosis | 0.838 | 0.120 | 0.113 | 0.838 | 0.113 | 0.193 | 0.113 | 0.230 | 0.014 * |
| Skewness | 0.790 | 0.494 | 0.028 * | 0.080 | 0.589 | 0.662 | 0.465 | 0.161 | 0.035 * |
| RMS | 0.080 | 0.028 * | 0.390 | 0.025 * | 0.589 | 0.327 | 0.028 * | 0.014 * | 0.002 * |
| Variance | 0.204 | 0.028 * | 0.662 | 0.056 | 0.790 | 0.193 | 0.113 | 0.943 | 0.943 |
| Maximum | 0.056 | 0.465 | 0.193 | 0.028 * | 0.790 | 0.080 | 0.001 * | 0.080 | 0.002 * |
| Minimum | 0.465 | 0.001 * | 0.193 | 0.494 | 0.113 | 0.790 | 0.494 | 0.790 | 0.005 * |
| Range | 0.023 * | 0.465 | 0.193 | 0.059 | 0.790 | 0.193 | 0.001 * | 0.080 | 0.005 * |
| Median | 0.001 * | 0.494 | 0.028 * | 0.589 | 0.790 | 0.390 | 0.662 | 0.327 | 0.005 * |
| EC | 0.193 | 0.028 * | 0.230 | 0.019 * | 0.790 | 0.291 | 0.028 * | 0.014 * | 0.000 * |
| Signals | Features | Baseline-30th | Baseline-60th | 30th–60th | |||
|---|---|---|---|---|---|---|---|
| p | Adjusted p | p | Adjusted p | p | Adjusted p | ||
| range | 0.17 | 0.51 | 0.006 | 0.018 * | 0.17 | 0.51 | |
| median | 0.17 | 0.51 | 0 | 0 * | 0.016 | 0.049 * | |
| RMS | 0.016 | 0.049 * | 1 | 1 | 0.026 | 0.077 | |
| variance | 0.016 | 0.049 * | 1 | 1 | 0.026 | 0.077 | |
| minimum | 0.303 | 0.91 | 0.01 | 0.03 * | 0 | 0.001 * | |
| EC | 0.016 | 0.049 * | 1 | 1 | 0.026 | 0.077 | |
| skewness | 1 | 1 | 0.016 | 0.049 * | 0.026 | 0.077 | |
| median | 1 | 1 | 0.026 | 0.077 | 0.016 | 0.049 * | |
| RMS | 1 | 1 | 0.01 | 0.03 * | 0.04 | 0.119 | |
| maximum | 1 | 1 | 0.016 | 0.049 * | 0.026 | 0.077 | |
| EC | 1 | 1 | 0.006 | 0.018 * | 0.059 | 0.178 | |
| RMS | 0.026 | 0.077 | 0.016 | 0.049 * | 1 | 1 | |
| maximum | 0.016 | 0.049 * | 0 | 0 * | 0.17 | 0.51 | |
| range | 0.016 | 0.049 * | 0 | 0 * | 0.17 | 0.51 | |
| EC | 0.026 | 0.077 | 0.016 | 0.049 * | 1 | 1 | |
| RMS | 0.23 | 0.69 | 0.004 | 0.011 * | 0.086 | 0.259 | |
| EC | 0.23 | 0.69 | 0.004 | 0.011 * | 0.086 | 0.259 | |
| kurtosis | 0.23 | 0.69 | 0.004 | 0.011 * | 0.086 | 0.259 | |
| skewness | 0.303 | 0.91 | 0.01 | 0.03 * | 0.123 | 0.368 | |
| RMS | 0.002 | 0.006 * | 0.002 | 0.006 * | 1 | 1 | |
| maximum | 0.004 | 0.011 * | 0.001 | 0.003 * | 1 | 1 | |
| minimum | 0.006 | 0.018 * | 0.004 | 0.011 * | 1 | 1 | |
| range | 0.004 | 0.011 * | 0.006 | 0.018 * | 1 | 1 | |
| median | 0.004 | 0.011 * | 0.006 | 0.018 * | 1 | 1 | |
| EC | 0 | 0.001 * | 0 | 0.001 * | 1 | 1 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, G.; Wong, I.K.-K.; Chen, T.L.-W.; Hong, T.T.-H.; Wong, D.W.-C.; Peng, Y.; Yan, F.; Wang, Y.; Tan, Q.; Zhang, M. Identifying Fatigue Indicators Using Gait Variability Measures: A Longitudinal Study on Elderly Brisk Walking. Sensors 2020, 20, 6983. https://doi.org/10.3390/s20236983
Zhang G, Wong IK-K, Chen TL-W, Hong TT-H, Wong DW-C, Peng Y, Yan F, Wang Y, Tan Q, Zhang M. Identifying Fatigue Indicators Using Gait Variability Measures: A Longitudinal Study on Elderly Brisk Walking. Sensors. 2020; 20(23):6983. https://doi.org/10.3390/s20236983
Chicago/Turabian StyleZhang, Guoxin, Ivy Kwan-Kei Wong, Tony Lin-Wei Chen, Tommy Tung-Ho Hong, Duo Wai-Chi Wong, Yinghu Peng, Fei Yan, Yan Wang, Qitao Tan, and Ming Zhang. 2020. "Identifying Fatigue Indicators Using Gait Variability Measures: A Longitudinal Study on Elderly Brisk Walking" Sensors 20, no. 23: 6983. https://doi.org/10.3390/s20236983
APA StyleZhang, G., Wong, I. K.-K., Chen, T. L.-W., Hong, T. T.-H., Wong, D. W.-C., Peng, Y., Yan, F., Wang, Y., Tan, Q., & Zhang, M. (2020). Identifying Fatigue Indicators Using Gait Variability Measures: A Longitudinal Study on Elderly Brisk Walking. Sensors, 20(23), 6983. https://doi.org/10.3390/s20236983






