Enhancing the Robustness of Smartphone Photoplethysmography: A Signal Quality Index Approach
Abstract
:1. Introduction
2. Materials and Methods
2.1. Signal Pre-Processing
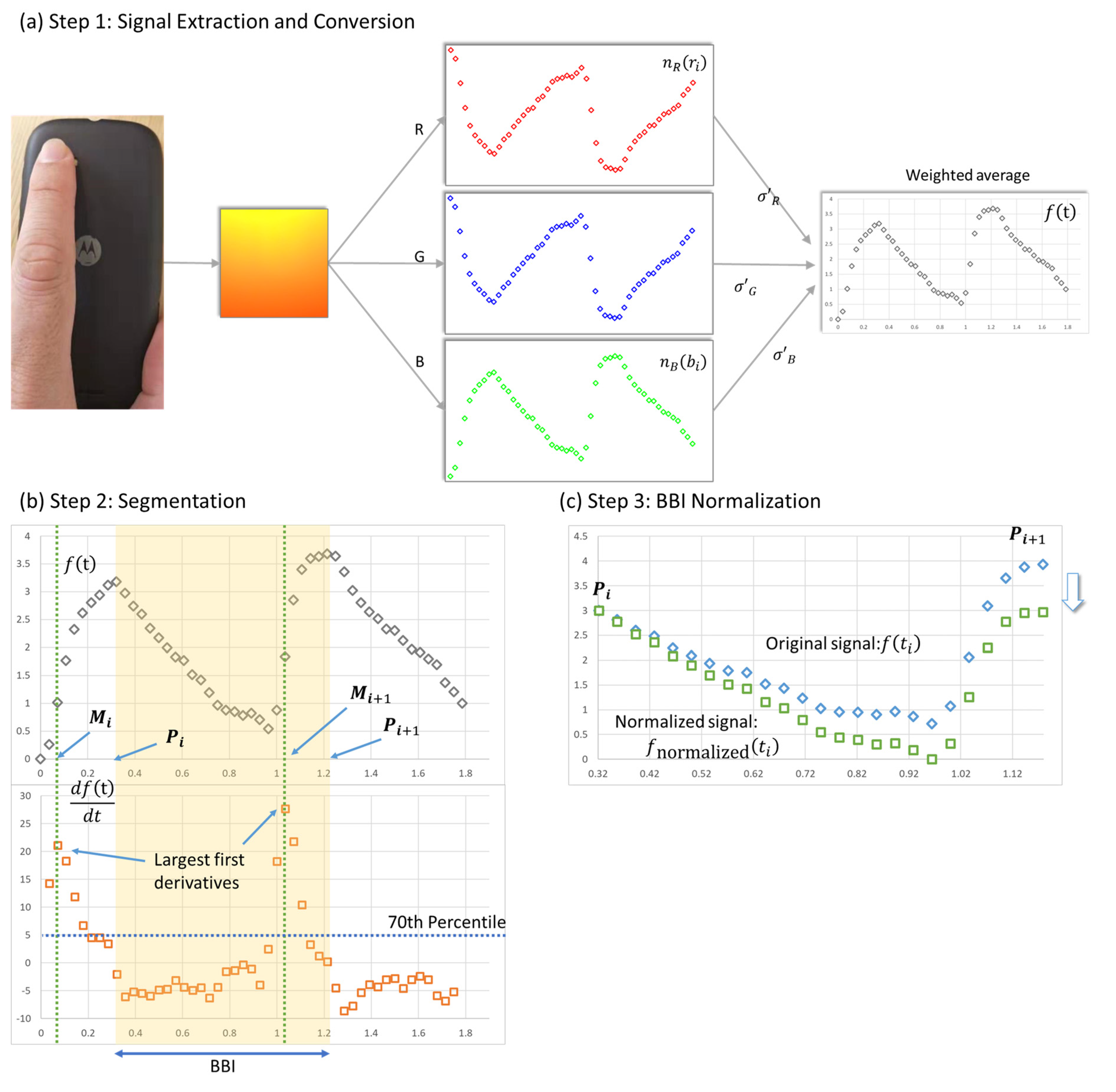
2.1.1. Signal Extraction and Conversion
2.1.2. Beat-to-Beat Interval (BBI) Segmentation
2.1.3. BBI Normalization
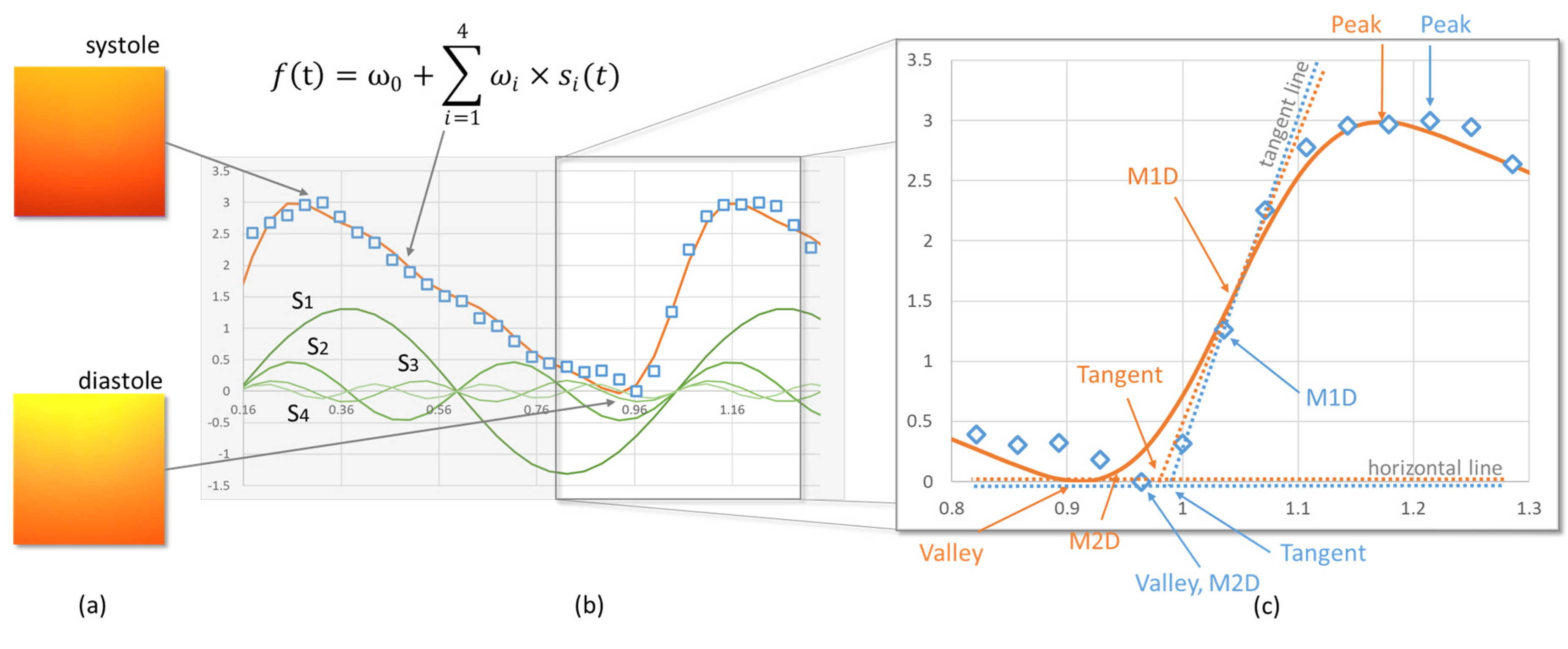
2.2. Sinusoidal Function-Based Photoplethysmography (PPG) Quality Index
2.3. HRV Measures
2.4. FPDT
2.5. Agreement Analysis
2.6. Participants and Data Collection
3. Results
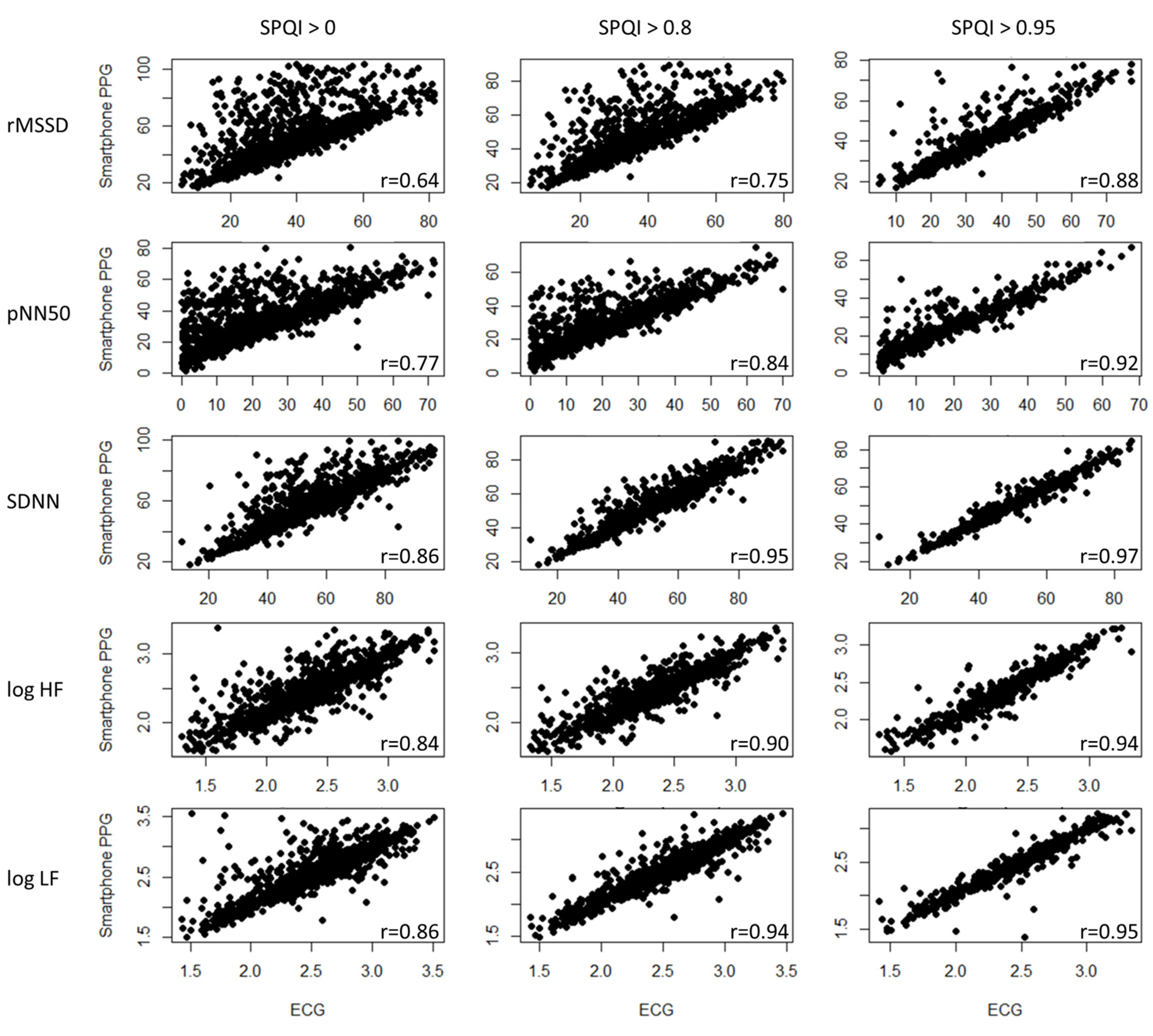
3.1. Correlation Coefficient Analysis
3.2. Bland–Altman Ratio Analysis
4. Discussion
4.1. Principal Findings
4.2. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Shaffer, F.; McCraty, R.; Zerr, C.L. A healthy heart is not a metronome: An integrative review of the heart’s anatomy and heart rate variability. Front. Psychol. 2014, 5, 1040. [Google Scholar] [CrossRef] [Green Version]
- Gordan, R.; Gwathmey, J.K.; Xie, L.-H. Autonomic and endocrine control of cardiovascular function. World J. Cardiol. 2015, 7, 204. [Google Scholar] [CrossRef] [PubMed]
- Berntson, G.G.; Cacioppo, J.T.; Quigley, K.S. Respiratory sinus arrhythmia: Autonomic origins, physiological mechanisms, and psychophysiological implications. Psychophysiology 1993, 30, 183–196. [Google Scholar] [CrossRef] [PubMed]
- Umetani, K.; Singer, D.H.; McCraty, R.; Atkinson, M. Twenty-four hour time domain heart rate variability and heart rate: Relations to age and gender over nine decades. J. Am. Coll. Cardiol. 1998, 31, 593–601. [Google Scholar] [CrossRef]
- Antelmi, I.; De Paula, R.S.; Shinzato, A.R.; Peres, C.A.; Mansur, A.J.; Grupi, C.J. Influence of age, gender, body mass index, and functional capacity on heart rate variability in a cohort of subjects without heart disease. Am. J. Cardiol. 2004, 93, 381–385. [Google Scholar] [CrossRef] [PubMed]
- Sandercock, G.R.; Bromley, P.D.; Brodie, D.A. Effects of exercise on heart rate variability: Inferences from meta-analysis. Med. Sci. Sports Exerc. 2005, 37, 433–439. [Google Scholar] [CrossRef]
- Hovland, A.; Pallesen, S.; Hammar, Å.; Hansen, A.L.; Thayer, J.F.; Sivertsen, B.; Tarvainen, M.P.; Nordhus, I.H. Subjective sleep quality in relation to inhibition and heart rate variability in patients with panic disorder. J. Affect. Disord. 2013, 150, 152–155. [Google Scholar] [CrossRef]
- Glos, M.; Fietze, I.; Blau, A.; Baumann, G.; Penzel, T. Cardiac autonomic modulation and sleepiness: Physiological consequences of sleep deprivation due to 40h of prolonged wakefulness. Physiol. Behav. 2014, 125, 45–53. [Google Scholar] [CrossRef]
- Rodríguez-Colón, S.M.; Li, X.; Shaffer, M.L.; He, F.; Bixler, E.O.; Vgontzas, A.N.; Cai, J.; Liao, D. Insulin resistance and circadian rhythm of cardiac autonomic modulation. Cardiovasc. Diabetol. 2010, 9, 85. [Google Scholar] [CrossRef] [Green Version]
- Stein, P.K.; Barzilay, J.I.; Chaves, P.H.; Traber, J.; Domitrovich, P.P.; Heckbert, S.R.; Gottdiener, J.S. Higher levels of inflammation factors and greater insulin resistance are independently associated with higher heart rate and lower heart rate variability in normoglycemic older individuals: The Cardiovascular Health Study. J. Am. Geriatr. Soc. 2008, 56, 315–321. [Google Scholar] [CrossRef]
- Nolan, R.P.; Jong, P.; Barry-Bianchi, S.M.; Tanaka, T.H.; Floras, J.S. Effects of drug, biobehavioral and exercise therapies on heart rate variability in coronary artery disease: A systematic review. Eur. J. Cardiovasc. Prev. Rehabil. 2008, 15, 386–396. [Google Scholar] [CrossRef] [PubMed]
- Koenig, J.; Williams, D.P.; Kemp, A.H.; Thayer, J.F. Vagally mediated heart rate variability in headache patients—a systematic review and meta-analysis. Cephalalgia 2016, 36, 265–278. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brotman, D.J.; Bash, L.D.; Qayyum, R.; Crews, D.; Whitsel, E.A.; Astor, B.C.; Coresh, J. Heart rate variability predicts ESRD and CKD-related hospitalization. J. Am. Soc. Nephrol. 2010, 21, 1560–1570. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hansen, A.L.; Johnsen, B.H.; Thayer, J.F. Vagal influence on working memory and attention. Int. J. Psychophysiol. 2003, 48, 263–274. [Google Scholar] [CrossRef]
- Thayer, J.F.; Hansen, A.L.; Sausrose, E.; Johnsen, B.H. Heart Rate Variability, Prefrontal Neural Function, and Cognitive Performance: The Neurovisceral Integration Perspective on Self-regulation, Adaptation, and Health. Ann. Behav. Med. 2009, 37, 141–153. [Google Scholar] [CrossRef]
- Hjortskov, N.; Rissén, D.; Blangsted, A.K.; Fallentin, N.; Lundberg, U.; Søgaard, K. The effect of mental stress on heart rate variability and blood pressure during computer work. Eur. J. Appl. Physiol. 2004, 92, 84–89. [Google Scholar] [CrossRef]
- Fenton-O’Creevy, M.; Lins, J.T.; Vohra, S.; Richards, D.W.; Davies, G.; Schaaff, K. Emotion regulation and trader expertise: Heart rate variability on the trading floor. J. Neurosci. Psychol. Econ. 2012, 5, 227. [Google Scholar] [CrossRef] [Green Version]
- Eisenberg, N.; Fabes, R.A.; Murphy, B.; Maszk, P.; Karbon, M.S. and M. The Role of Emotionality and Regulation in Children’s Social Functioning: A Longitudinal Study. Child Dev. 1995, 66, 1360–1384. [Google Scholar] [CrossRef]
- Porges, S.W. The polyvagal perspective. Biol. Psychol. 2007, 74, 116–143. [Google Scholar] [CrossRef]
- Geisler, F.C.; Vennewald, N.; Kubiak, T.; Weber, H. The impact of heart rate variability on subjective well-being is mediated by emotion regulation. Personal. Individ. Differ. 2010, 49, 723–728. [Google Scholar] [CrossRef]
- Plews, D.J.; Scott, B.; Altini, M.; Wood, M.; Kilding, A.E.; Laursen, P.B. Comparison of heart-rate-variability recording with smartphone photoplethysmography, Polar H7 chest strap, and electrocardiography. Int. J. Sports Physiol. Perform. 2017, 12, 1324–1328. [Google Scholar] [CrossRef] [PubMed]
- Li, K.H.C.; White, F.A.; Tipoe, T.; Liu, T.; Wong, M.C.; Jesuthasan, A.; Baranchuk, A.; Tse, G.; Yan, B.P. The Current State of Mobile Phone Apps for Monitoring Heart Rate, Heart Rate Variability, and Atrial Fibrillation: Narrative Review. JMIR MHealth UHealth 2019, 7, e11606. [Google Scholar] [CrossRef] [PubMed]
- Elgendi, M. On the analysis of fingertip photoplethysmogram signals. Curr. Cardiol. Rev. 2012, 8, 14–25. [Google Scholar] [CrossRef] [PubMed]
- Jonathan, E.; Leahy, M.J. Cellular phone-based photoplethysmographic imaging. J. Biophotonics 2011, 4, 293–296. [Google Scholar] [CrossRef]
- Pelegris, P.; Banitsas, K.; Orbach, T.; Marias, K. A novel method to detect heart beat rate using a mobile phone. In Proceedings of the 2010 Annual International Conference of the IEEE Engineering in Medicine and Biology, Buenos Aires, Argentina, 31 August–4 September 2010; pp. 5488–5491. [Google Scholar]
- Garcia-Agundez, A.; Dutz, T.; Goebel, S. Adapting smartphone-based photoplethysmography to suboptimal scenarios. Physiol. Meas. 2017, 38, 219–232. [Google Scholar] [CrossRef]
- Nam, Y.; Nam, Y.-C. Photoplethysmography signal analysis for optimal region-of-interest determination in video imaging on a built-in smartphone under different conditions. Sensors 2017, 17, 2385. [Google Scholar] [CrossRef] [Green Version]
- Ferrer-Mileo, V.; Guede-Fernandez, F.; Fernández-Chimeno, M.; Ramos-Castro, J.; García-González, M.A. Accuracy of heart rate variability estimation by photoplethysmography using an smartphone: Processing optimization and fiducial point selection. In Proceedings of the 2015 37th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Milan, Italy, 25–29 August 2015; pp. 5700–5703. [Google Scholar]
- Shin, H.S.; Lee, C.; Lee, M. Adaptive threshold method for the peak detection of photoplethysmographic waveform. Comput. Biol. Med. 2009, 39, 1145–1152. [Google Scholar]
- Dao, D.; Salehizadeh, S.M.; Noh, Y.; Chong, J.W.; Cho, C.H.; McManus, D.; Darling, C.E.; Mendelson, Y.; Chon, K.H. A robust motion artifact detection algorithm for accurate detection of heart rates from photoplethysmographic signals using time–frequency spectral features. IEEE J. Biomed. Health Inform. 2016, 21, 1242–1253. [Google Scholar] [CrossRef]
- Morelli, D.; Bartoloni, L.; Colombo, M.; Plans, D.; Clifton, D.A. Profiling the propagation of error from PPG to HRV features in a wearable physiological-monitoring device. Healthc. Technol. Lett. 2018, 5, 59–64. [Google Scholar] [CrossRef] [Green Version]
- Chong, J.W.; Cho, C.H.; Tabei, F.; Le-Anh, D.; Esa, N.; Mcmanus, D.D.; Chon, K.H. Motion and noise artifact-resilient atrial fibrillation detection using a smartphone. IEEE J. Emerg. Sel. Top. Circuits Syst. 2018, 8, 230–239. [Google Scholar] [CrossRef]
- Baek, H.J.; Shin, J.; Jin, G.; Cho, J. Reliability of the Parabola Approximation Method in Heart Rate Variability Analysis Using Low-Sampling-Rate Photoplethysmography. J. Med. Syst. 2017, 41, 189. [Google Scholar] [CrossRef] [PubMed]
- Peng, F.; Zhang, Z.; Gou, X.; Liu, H.; Wang, W. Motion artifact removal from photoplethysmographic signals by combining temporally constrained independent component analysis and adaptive filter. Biomed. Eng. Online 2014, 13, 50. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Siddiqui, S.A.; Zhang, Y.; Feng, Z.; Kos, A. A pulse rate estimation algorithm using PPG and smartphone camera. J. Med. Syst. 2016, 40, 126. [Google Scholar] [CrossRef]
- Sun, X.; Yang, P.; Li, Y.; Gao, Z.; Zhang, Y.-T. Robust heart beat detection from photoplethysmography interlaced with motion artifacts based on empirical mode decomposition. In Proceedings of the Proceedings of 2012 IEEE-EMBS International Conference on Biomedical and Health Informatics, Hong Kong, China, 5–7 January 2012; pp. 775–778. [Google Scholar]
- De Ridder, B.; Van Rompaey, B.; Kampen, J.K.; Haine, S.; Dilles, T. Smartphone apps using photoplethysmography for heart rate monitoring: Meta-analysis. JMIR Cardio 2018, 2, e2. [Google Scholar] [CrossRef] [PubMed]
- Bánhalmi, A.; Borbás, J.; Fidrich, M.; Bilicki, V.; Gingl, Z.; Rudas, L. Analysis of a pulse rate variability measurement using a smartphone camera. J. Healthc. Eng. 2018. [Google Scholar] [CrossRef]
- Huang, R.-Y.; Dung, L.-R. Measurement of heart rate variability using off-the-shelf smart phones. Biomed. Eng. OnLine 2016, 15, 11. [Google Scholar] [CrossRef] [Green Version]
- Peng, R.-C.; Zhou, X.-L.; Lin, W.-H.; Zhang, Y.-T. Extraction of heart rate variability from smartphone photoplethysmograms. Comput. Math. Methods Med. 2015. [Google Scholar] [CrossRef]
- Liu, I.; Ni, S.; Peng, K. Happiness at Your Fingertips: Assessing Mental Health with Smartphone Photoplethysmogram-Based Heart Rate Variability Analysis. Telemed. E-Health 2020. [Google Scholar] [CrossRef]
- Choi, A.; Shin, H. Photoplethysmography sampling frequency: Pilot assessment of how low can we go to analyze pulse rate variability with reliability? Physiol. Meas. 2017, 38, 586–600. [Google Scholar] [CrossRef]
- Laborde, S.; Mosley, E.; Thayer, J.F. Thayer Heart Rate Variability and Cardiac Vagal Tone in Psychophysiological Research – Recommendations for Experiment Planning, Data Analysis, and Data Reporting. Front. Psychol. 2017, 8. [Google Scholar] [CrossRef] [Green Version]
- Kok, B.E.; Coffey, K.A.; Cohn, M.A.; Catalino, L.I.; Vacharkulksemsuk, T.; Algoe, S.B.; Brantley, M.; Fredrickson, B.L. How positive emotions build physical health: Perceived positive social connections account for the upward spiral between positive emotions and vagal tone. Psychol. Sci. 2013, 24, 1123–1132. [Google Scholar] [CrossRef] [PubMed]
- Jiang, W.J.; Wittek, P.; Zhao, L.; Gao, S.C. Adaptive thresholding with inverted triangular area for real-time detection of the heart rate from photoplethysmogram traces on a smartphone. In Proceedings of the 2014 36th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Chicago, IL, USA, 26–30 August 2014; pp. 3212–3215. [Google Scholar]
- Paradkar, N.; Chowdhury, S.R. Cardiac arrhythmia detection using photoplethysmography. In Proceedings of the 2017 39th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Seogwipo, Korea, 11–15 July 2017; pp. 113–116. [Google Scholar]
- Millasseau, S.C.; Kelly, R.P.; Ritter, J.M.; Chowienczyk, P.J. The vascular impact of aging andvasoactive drugs: Comparison of two digital volume pulse measurements. Am. J. Hypertens. 2003, 16, 467–472. [Google Scholar] [CrossRef] [Green Version]
- Martínez, C.A.G.; Quintana, A.O.; Vila, X.A.; Touriño, M.J.L.; Rodríguez-Liñares, L.; Presedo, J.M.R.; Penín, A.J.M. Heart rate variability analysis with the R package RHRV; Springer: Berlin/Heidelberg, Germany, 2017; ISBN 3-319-65355-5. [Google Scholar]
- Millasseau, S.C.; Ritter, J.M.; Takazawa, K.; Chowienczyk, P.J. Contour analysis of the photoplethysmographic pulse measured at the finger. J. Hypertens. 2006, 24, 1449–1456. [Google Scholar] [CrossRef] [PubMed]
- Yousef, Q.; Reaz, M.B.I.; Ali, M.A.M. The analysis of PPG morphology: Investigating the effects of aging on arterial compliance. Meas. Sci. Rev. 2012, 12, 266–271. [Google Scholar] [CrossRef] [Green Version]
- Sukor, J.A.; Redmond, S.J.; Lovell, N.H. Signal quality measures for pulse oximetry through waveform morphology analysis. Physiol. Meas. 2011, 32, 369. [Google Scholar] [CrossRef] [PubMed]
- Couceiro, R.; Carvalho, P.; Paiva, R.P.; Henriques, J.; Quintal, I.; Antunes, M.; Muehlsteff, J.; Eickholt, C.; Brinkmeyer, C.; Kelm, M. Assessment of cardiovascular function from multi-Gaussian fitting of a finger photoplethysmogram. Physiol. Meas. 2015, 36, 1801–1825. [Google Scholar] [CrossRef]
- Goswami, D.; Chaudhuri, K.; Mukherjee, J. A new two-pulse synthesis model for digital volume pulse signal analysis. Cardiovasc. Eng. 2010, 10, 109–117. [Google Scholar] [CrossRef]
- Rubins, U. Finger and ear photoplethysmogram waveform analysis by fitting with Gaussians. Med. Biol. Eng. Comput. 2008, 46, 1271–1276. [Google Scholar] [CrossRef]
- Wang, Y.-Y.L.; Hsu, T.-L.; Jan, M.-Y.; Wang, W.-K. Theory and applications of the harmonic analysis of arterial pressure pulse waves. J. Med. Biol. Eng. 2010, 30, 125–131. [Google Scholar] [CrossRef]
- Shaffer, F.; Ginsberg, J.P. An overview of heart rate variability metrics and norms. Front. Public Health 2017, 5, 258. [Google Scholar] [CrossRef] [Green Version]
- Chalmers, J.A.; Heathers, J.A.J.; Abbott, M.J.; Kemp, A.H.; Quintana, D.S. Worry is associated with robust reductions in heart rate variability: A transdiagnostic study of anxiety psychopathology. Bmc Psychol. 2016, 4, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chiu, Y.C.; Arand, P.W.; Shroff, S.G.; Feldman, T.; Carroll, J.D. Determination of pulse wave velocities with computerized algorithms. Am. Heart J. 1991, 121, 1460–1470. [Google Scholar] [CrossRef]
- Jeyhani, V.; Mahdiani, S.; Peltokangas, M.; Vehkaoja, A. Comparison of HRV parameters derived from photoplethysmography and electrocardiography signals. In Proceedings of the 2015 37th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Milan, Italy, 25–29 August 2015; pp. 5952–5955. [Google Scholar]
- Leikan, G.M.; Rossi, E.; Sanz, M.; Rodríguez, D.D.; Mántaras, M.C.; Nicolet, J.; Zapata, D.; Lapyckyj, I.; Siri, L.N.; Perrone, M.S. Evaluation of agreement between temporal series obtained from electrocardiogram and pulse wave. J. Phys. Conf. Ser. 2016, 705, 012038. [Google Scholar] [CrossRef] [Green Version]
- Lin, W.-H.; Wu, D.; Li, C.; Zhang, H.; Zhang, Y.-T. Comparison of heart rate variability from PPG with that from ECG. In Proceedings of the International Conference on Health Informatics, Vilamoura, Portugal, 7–9 November 2014; pp. 213–215. [Google Scholar]
- Posada-Quintero, H.F.; Delisle-Rodríguez, D.; Cuadra-Sanz, M.B.; de la Vara-Prieto, R.F. Evaluation of pulse rate variability obtained by the pulse onsets of the photoplethysmographic signal. Physiol. Meas. 2013, 34, 179–187. [Google Scholar] [CrossRef] [PubMed]
- Schäck, T.; Harb, Y.S.; Muma, M.; Zoubir, A.M. Computationally efficient algorithm for photoplethysmography-based atrial fibrillation detection using smartphones. In Proceedings of the 2017 39th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Seogwipo, Korea, 11–15 July 2017; pp. 104–108. [Google Scholar]
- Peralta, E.; Lazaro, J.; Bailon, R.; Marozas, V.; Gil, E. Peralta Optimal fiducial points for pulse rate variability analysis from forehead and finger photoplethysmographic signals. Physiol. Meas. 2009, 40, 025007. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bland, J.M.; Altman, D. Statistical methods for assessing agreement between two methods of clinical measurement. The lancet 1986, 327, 307–310. [Google Scholar] [CrossRef]
- Schäfer, A.; Vagedes, J. How accurate is pulse rate variability as an estimate of heart rate variability?: A review on studies comparing photoplethysmographic technology with an electrocardiogram. Int. J. Cardiol. 2013, 166, 15–29. [Google Scholar] [CrossRef]
- Wierig, M.; Mandtler, L.P.; Rottmann, P.; Stroh, V.; Müller, U.; Büscher, W.; Plümer, L. Recording Heart Rate Variability of Dairy Cows to the Cloud—Why Smartphones Provide Smart Solutions. Sensor 2018, 18, 2541. [Google Scholar] [CrossRef] [Green Version]
- Westerink, J.; Ouwerkerk, M.; de Vries, G.-J.; de Waele, S.; van den Eerenbeemd, J.; van Boven, M. Emotion measurement platform for daily life situations. In Proceedings of the 2009 3rd International Conference on Affective Computing and Intelligent Interaction and Workshops, Amsterdam, The Netherlands, 10–12 September 2009; pp. 1–6. [Google Scholar]
- Burgess, H.J.; Penev, P.D.; Schneider, R.; Van Cauter, E. Estimating cardiac autonomic activity during sleep: Impedance cardiography, spectral analysis, and Poincare plots. Clin. Neurophysiol. 2004, 115, 19–28. [Google Scholar] [CrossRef]
- Ghodrati, A.; Marinello, S. Statistical analysis of RR interval irregularities for detection of atrial fibrillation. In Proceedings of the 2008 Computers in Cardiology, Bologna, Italy, 14–17 September 2008; pp. 1057–1060. [Google Scholar]
- Mahdiani, S.; Jeyhani, V.; Peltokangas, M.; Vehkaoja, A. Is 50 Hz high enough ECG sampling frequency for accurate HRV analysis? In Proceedings of the 2015 37th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Milan, Italy, 25–29 August 2015; pp. 5948–5951. [Google Scholar]
- Hejjel, L.; Roth, E. What is the adequate sampling interval of the ECG signal for heart rate variability analysis in the time domain? Physiol. Meas. 2004, 25, 1405. [Google Scholar] [CrossRef]
- Elgendi, M. Optimal signal quality index for photoplethysmogram signals. Bioengineering 2016, 3, 21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lu, G.; Yang, F. Limitations of oximetry to measure heart rate variability measures. Cardiovasc. Eng. 2009, 9, 119–125. [Google Scholar] [CrossRef] [PubMed]
- Cennini, G.; Arguel, J.; Akşit, K.; van Leest, A. Heart rate monitoring via remote photoplethysmography with motion artifacts reduction. Opt. Express 2010, 18, 4867–4875. [Google Scholar] [CrossRef] [PubMed]
- Ding, X.-R.; Zhang, Y.-T.; Liu, J.; Dai, W.-X.; Tsang, H.K. Continuous cuffless blood pressure estimation using pulse transit time and photoplethysmogram intensity ratio. IEEE Trans. Biomed. Eng. 2015, 63, 964–972. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.; Snoswell, C.L.; Harding, L.E.; Bambling, M.; Edirippulige, S.; Bai, X.; Smith, A.C. The Role of Telehealth in Reducing the Mental Health Burden from COVID-19. Telemed. Telemed. e-Health 2020. [Google Scholar] [CrossRef] [Green Version]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in china. Int. J. Environ. Res. Public. Health 2020, 17, 1729. [Google Scholar] [CrossRef] [Green Version]
- Lomaliza, J.P.; Park, H. A highly efficient and reliable heart rate monitoring system using smartphone cameras. Multimed. Tools Appl. 2016, 76, 1–21. [Google Scholar] [CrossRef]


| HRV Measures | Definition |
|---|---|
| Time-Domain | |
| SDNN | Standard deviation of the average normal-to-normal (NN) intervals |
| pNN50 | Percentage of successive NN intervals that differ by more than 50 ms |
| rMSSD | Root mean square of successive NN interval differences |
| Frequency-Domain | |
| HF | Absolute power of the high-frequency band (0.15–0.4 Hz) |
| LF | Absolute power of the low-frequency band (0.04–0.15 Hz) |
| VLF | Absolute power of the very-low frequency band (0.003–0.04 Hz) |
| ULF | Absolute power of the ultra-low frequency band (≤0.003 Hz) |
| log HF | Log-transformed HF |
| log LF | Log-transformed LF |
| log LF/HF | Log-transformed ratio of LF to HF |
| FPDT | Fiducial Point Definition |
|---|---|
| Peak | The maximum point in each BBI. |
| Valley | The minimum point in each BBI. |
| M1D | The maximum point of the first derivative in each BBI. |
| M2D | The maximum point of the second derivative in each BBI. |
| Tangent | The point where the tangent line from the M1D intersects the horizontal line from the Valley. The first derivatives of a discrete data set are determined by the difference function approximation. |
| Threshold | FPDT | rMSSD | pNN50 | SDNN | log HF | log LF | Avg. (FPDT) | Avg. (SPQI) |
|---|---|---|---|---|---|---|---|---|
| SPQI > 0 | Peak | 0.520 | 0.652 | 0.692 | 0.639 | 0.607 | 0.622 | 0.669 |
| Valley | 0.608 | 0.731 | 0.791 | 0.758 | 0.741 | 0.726 | ||
| M1D | 0.596 | 0.675 | 0.823 | 0.790 | 0.807 | 0.738 | ||
| M2D | 0.290 | 0.559 | 0.489 | 0.549 | 0.475 | 0.472 | ||
| Tangent | 0.615 | 0.752 | 0.864 | 0.843 | 0.858 | 0.786 | ||
| SPQI > 0.8 | Peak | 0.604 | 0.715 | 0.786 | 0.699 | 0.678 | 0.696 | 0.758 |
| Valley | 0.702 | 0.834 | 0.879 | 0.844 | 0.842 | 0.820 | ||
| M1D | 0.705 | 0.777 | 0.915 | 0.846 | 0.882 | 0.825 | ||
| M2D | 0.393 | 0.665 | 0.626 | 0.629 | 0.536 | 0.570 | ||
| Tangent | 0.756 | 0.848 | 0.947 | 0.900 | 0.936 | 0.877 | ||
| SPQI > 0.95 | Peak | 0.689 | 0.768 | 0.847 | 0.799 | 0.749 | 0.770 | 0.843 |
| Valley | 0.898 | 0.911 | 0.967 | 0.914 | 0.934 | 0.925 | ||
| M1D | 0.795 | 0.851 | 0.943 | 0.881 | 0.892 | 0.872 | ||
| M2D | 0.565 | 0.800 | 0.802 | 0.762 | 0.632 | 0.712 | ||
| Tangent | 0.879 | 0.923 | 0.974 | 0.939 | 0.954 | 0.934 | ||
| All correlation coefficients in the table have p < 0.05 | ||||||||
| Threshold | FPDT | rMSSD | pNN50 | SDNN | log HF | log LF | Avg. (FPDT) | Avg. (SPQI) |
|---|---|---|---|---|---|---|---|---|
| SPQI > 0 | Peak | 1283 | 1331 | 1276 | 1226 | 1257 | 1274.6 | 1263 |
| Valley | 1258 | 1329 | 1269 | 1245 | 1255 | 1271.2 | ||
| M1D | 1233 | 1330 | 1276 | 1250 | 1262 | 1270.2 | ||
| M2D | 1227 | 1321 | 1204 | 1189 | 1223 | 1232.8 | ||
| Tangent | 1250 | 1325 | 1274 | 1236 | 1246 | 1266.2 | ||
| SPQI > 0.8 | Peak | 1067 | 1087 | 1075 | 1049 | 1071 | 1069.8 | 1060 |
| Valley | 1062 | 1083 | 1073 | 1056 | 1066 | 1068.0 | ||
| M1D | 1052 | 1085 | 1067 | 1054 | 1068 | 1065.2 | ||
| M2D | 1006 | 1078 | 1012 | 1032 | 1057 | 1037.0 | ||
| Tangent | 1046 | 1081 | 1065 | 1053 | 1064 | 1061.8 | ||
| SPQI > 0.95 | Peak | 565 | 550 | 566 | 558 | 565 | 560.8 | 557 |
| Valley | 563 | 548 | 567 | 562 | 562 | 560.4 | ||
| M1D | 561 | 545 | 564 | 555 | 560 | 557.0 | ||
| M2D | 542 | 546 | 553 | 548 | 560 | 549.8 | ||
| Tangent | 562 | 548 | 564 | 557 | 563 | 558.8 |
| Threshold | FPDT | rMSSD | pNN50 | SDNN | Log HF | Log LF |
|---|---|---|---|---|---|---|
| SPQI > 0 | Peak | 0.694 | 0.888 | 0.443 | 0.232 | 0.268 |
| Valley | 0.552 | 0.813 | 0.344 | 0.199 * | 0.215 | |
| M1D | 0.539 | 0.833 | 0.312 | 0.186 * | 0.181 * | |
| M2D | 0.848 | 0.940 | 0.621 | 0.256 | 0.315 | |
| Tangent | 0.677 | 0.905 | 0.287 | 0.166 * | 0.156 * | |
| SPQI > 0.8 | Peak | 0.581 | 0.798 | 0.351 | 0.214 | 0.241 |
| Valley | 0.451 | 0.660 | 0.262 | 0.164 * | 0.165 * | |
| M1D | 0.433 | 0.701 | 0.220 | 0.164 * | 0.141 * | |
| M2D | 0.653 | 0.808 | 0.455 | 0.233 | 0.291 | |
| Tangent | 0.469 | 0.708 | 0.177 * | 0.134 * | 0.105 * | |
| SPQI > 0.95 | Peak | 0.514 | 0.737 | 0.283 | 0.180 * | 0.217 |
| Valley | 0.297 | 0.547 | 0.144 * | 0.129 * | 0.108 * | |
| M1D | 0.367 | 0.615 | 0.179 * | 0.150 * | 0.136 * | |
| M2D | 0.504 | 0.672 | 0.308 | 0.195 * | 0.257 | |
| Tangent | 0.325 | 0.529 | 0.123 * | 0.108 * | 0.092 * | |
| * acceptable or good agreement | ||||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, I.; Ni, S.; Peng, K. Enhancing the Robustness of Smartphone Photoplethysmography: A Signal Quality Index Approach. Sensors 2020, 20, 1923. https://doi.org/10.3390/s20071923
Liu I, Ni S, Peng K. Enhancing the Robustness of Smartphone Photoplethysmography: A Signal Quality Index Approach. Sensors. 2020; 20(7):1923. https://doi.org/10.3390/s20071923
Chicago/Turabian StyleLiu, Ivan, Shiguang Ni, and Kaiping Peng. 2020. "Enhancing the Robustness of Smartphone Photoplethysmography: A Signal Quality Index Approach" Sensors 20, no. 7: 1923. https://doi.org/10.3390/s20071923
APA StyleLiu, I., Ni, S., & Peng, K. (2020). Enhancing the Robustness of Smartphone Photoplethysmography: A Signal Quality Index Approach. Sensors, 20(7), 1923. https://doi.org/10.3390/s20071923






