Quantitative Analysis of EEG Power Spectrum and EMG Median Power Frequency Changes after Continuous Passive Motion Mirror Therapy System
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
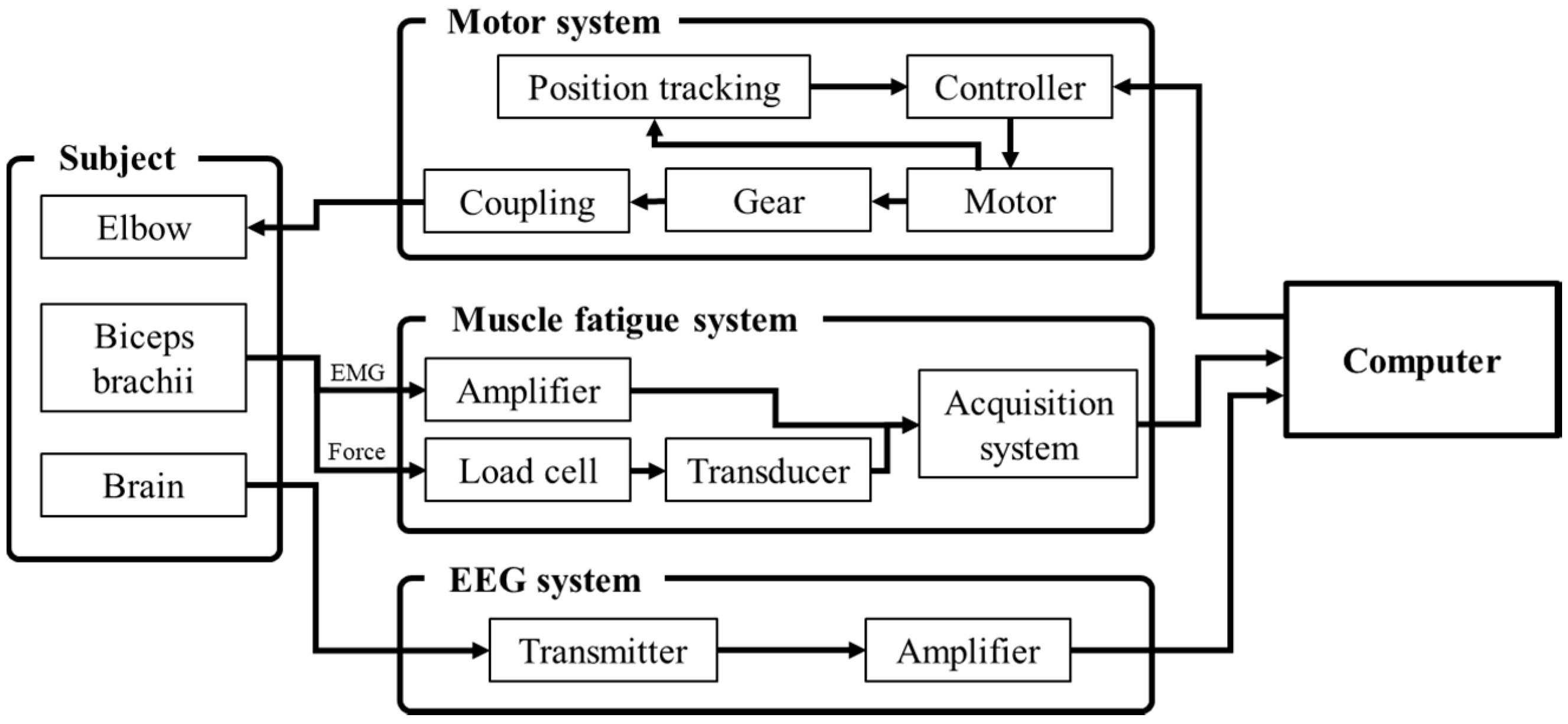
2.2. Apparatus and Materials
2.3. Customized CPM
2.4. Experimental Protocol
2.5. Signal Processing
2.5.1. EEG Signal Processing
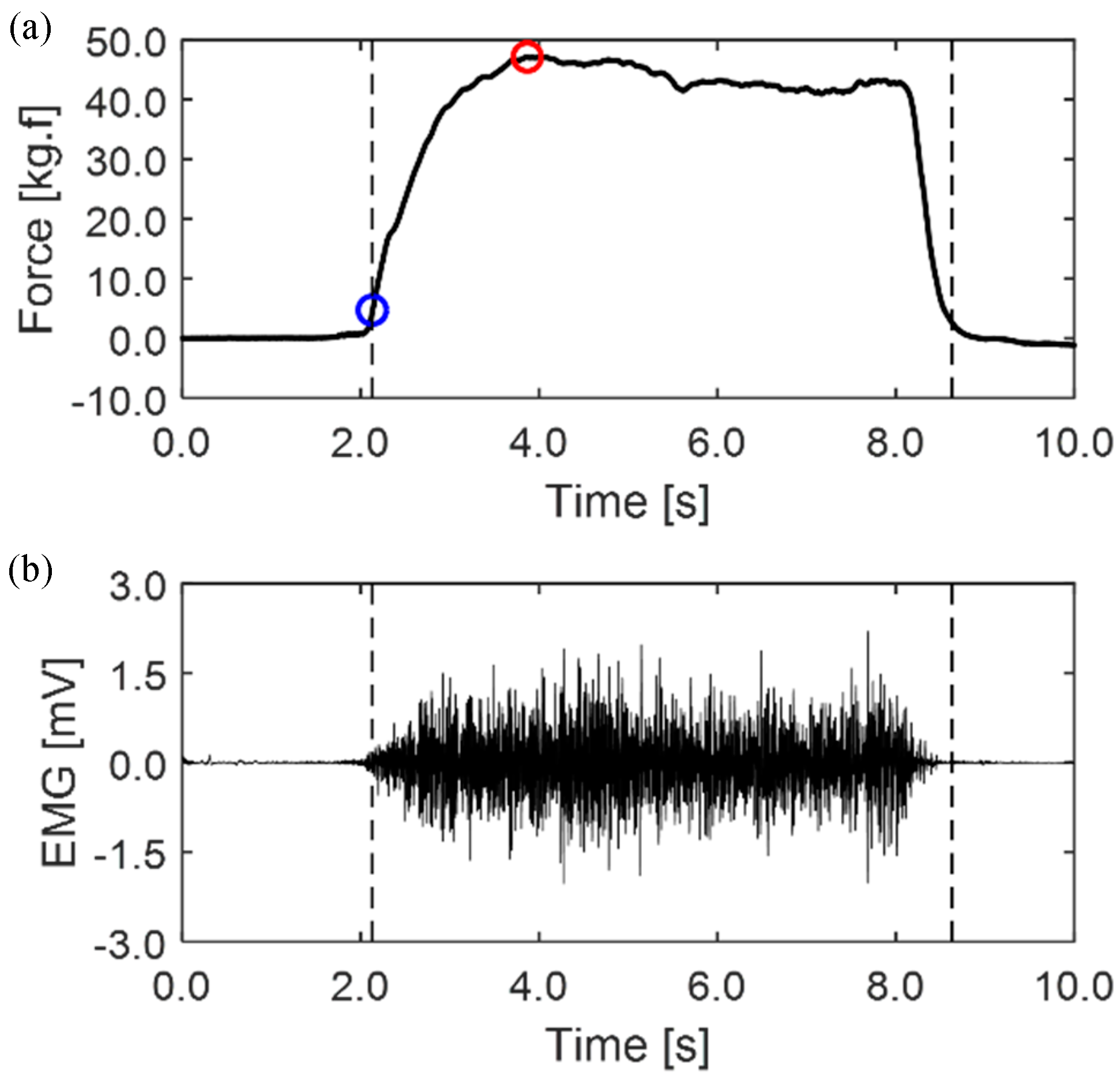
2.5.2. EMG Signal Processing
2.6. Data Analysis
3. Results and Discussion
3.1. Brain Activation Analysis: EEG
3.1.1. Relative PSD Analysis
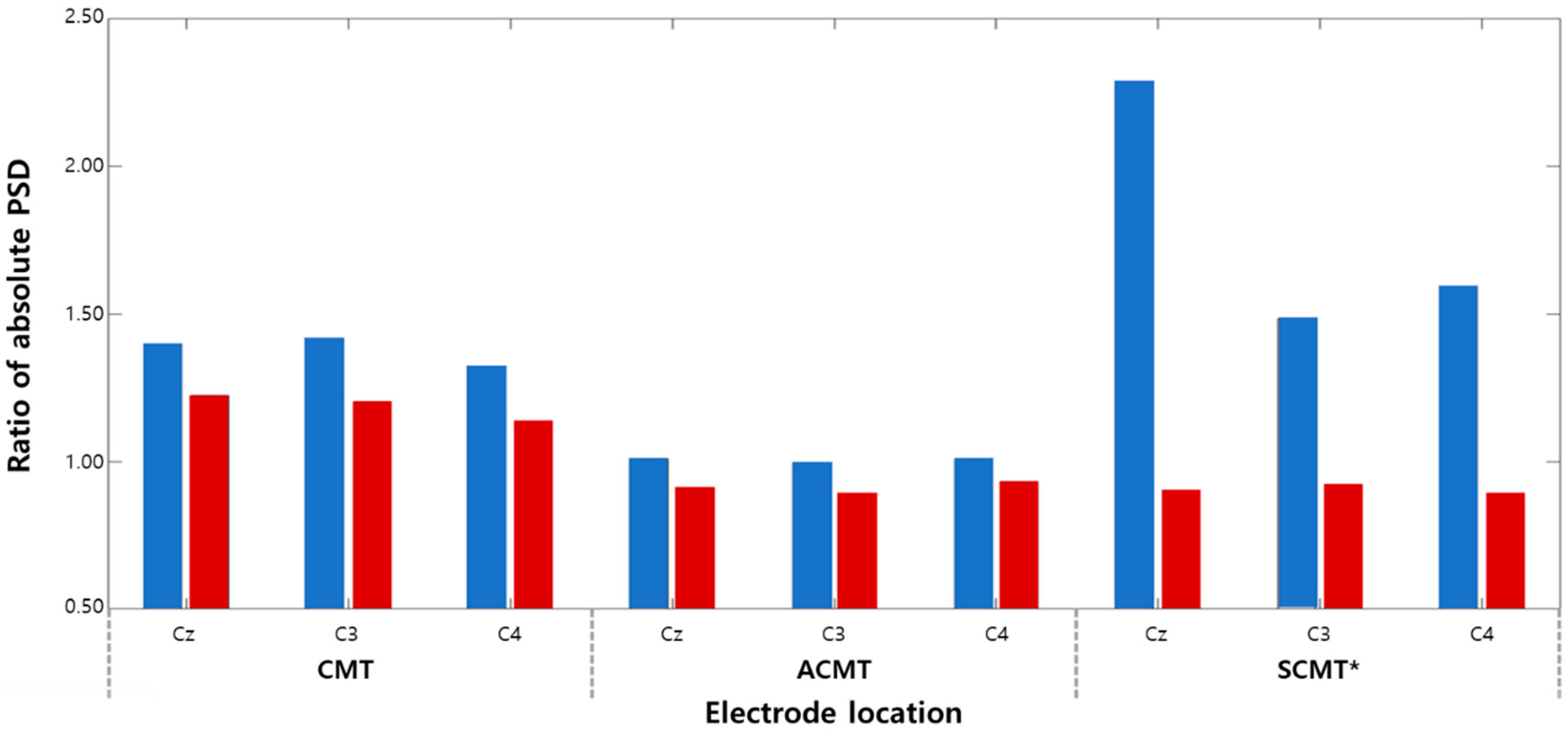
3.1.2. Absolute PSD Analysis
3.1.3. System Differences: CMT versus CPM-MT
3.2. Muscle Fatigue Analysis: EMG
3.3. Suggestions for High-Efficiency MT
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
Ethical Statements
References
- WHO. Available online: https://www.who.int/ (accessed on 1 November 2019).
- Magill, R.A.; Anderson, D.I. Motor Learning and Control: Concepts and Applications; McGraw-Hill: New York, NY, USA, 2007; Volume 11. [Google Scholar]
- Altschuler, E.L.; Wisdom, S.B.; Stone, L.; Foster, C.; Galasko, D.; Llewellyn, D.M.E.; Ramachandran, V.S. Rehabilitation of hemiparesis after stroke with a mirror. Lancet 1999, 353, 2035–2036. [Google Scholar] [CrossRef]
- Ramachandran, V.S.; Rogers-Ramachandran, D. Synaesthesia in phantom limbs induced with mirrors. Proc. Biol. Sci. 1996, 263, 377–386. [Google Scholar]
- Shimizu, T.; Hosaki, A.; Hino, T.; Sato, M.; Komori, T.; Hirai, S.; Rossini, P.M. Motor cortical disinhibition in the unaffected hemisphere after unilateral cortical stroke. Brain 2002, 125, 1896–1907. [Google Scholar] [CrossRef] [PubMed]
- Cauraugh, J.H.; Summers, J.J. Neural plasticity and bilateral movements: A rehabilitation approach for chronic stroke. Prog. Neurobiol. 2005, 75, 309–320. [Google Scholar] [CrossRef] [PubMed]
- Foran, J.R.; Steinman, S.; Barash, I.; Chambers, H.G.; Lieber, R.L. Structural and mechanical alterations in spastic skeletal muscle. Dev. Med. Child Neurol. 2005, 47, 713–717. [Google Scholar] [CrossRef]
- Liu, J.; Xu, D.; Ren, Y.; Zhang, L.-Q. Evaluations of neuromuscular dynamics of hyperactive reflexes poststroke. J. Rehabil. Res. Dev. 2011, 48, 577–586. [Google Scholar] [CrossRef]
- Shahbazi, M.; Atashzar, S.F.; Tavakoli, M.; Patel, R.V. Robotics-assisted mirror rehabilitation therapy: A therapist-in-the-loop assist-as-needed architecture. IEEE/ASME Trans. Mechatron. 2016, 21, 1954–1965. [Google Scholar] [CrossRef]
- Lessard, S.; Pansodtee, P.; Robbins, A.; Trombadore, J.M.; Kurniawan, S.; Teodorescu, M. A soft exosuit for flexible upper-extremity rehabilitation. IEEE Trans. Neural Syst. Rehabil. Eng. 2018, 26, 1604–1617. [Google Scholar] [CrossRef]
- Park, W.; Kwon, G.H.; Kim, D.-H.; Kim, Y.-H.; Kim, S.-P.; Kim, L. Assessment of cognitive engagement in stroke patients from single-trial EEG during motor rehabilitation. IEEE Trans. Neural Syst. Rehabil. Eng. 2014, 23, 351–362. [Google Scholar] [CrossRef]
- Bolognini, N.; Russo, C.; Edwards, D.J. The sensory side of post-stroke motor rehabilitation. Restor. Neurol. Neurosci. 2016, 34, 571–586. [Google Scholar] [CrossRef] [Green Version]
- Piovesan, D.; Morasso, P.; Giannoni, P.; Casadio, M. Arm stiffness during assisted movement after stroke: The influence of visual feedback and training. IEEE Trans. Neural Syst. Rehabil. Eng. 2012, 21, 454–465. [Google Scholar] [CrossRef] [PubMed]
- Yu, T.F.; Wilson, A.J. A passive movement method for parameter estimation of a musculo-skeletal arm model incorporating a modified hill muscle model. Comput. Methods Programs Biomed. 2014, 114, e46–e59. [Google Scholar] [CrossRef] [Green Version]
- Jeunet, C.; Glize, B.; Mcgonigal, A.; Batail, J.-M.; Micoulaud-Franchi, J.-A. Using EEG-based brain computer interface and neurofeedback targeting sensorimotor rhythms to improve motor skills: Theoretical background, applications and prospects. Neurophysiol. Clin. 2019, 49, 125–136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leamy, D.J.; Collins, R.; Ward, T.E. Combining fNIRS and EEG to improve motor cortex activity classification during an imagined movement-based task. In International Conference on Foundations of Augmented Cognition, 2011; Springer: Berlin/Heidelberg, Germany, 2011; pp. 177–185. [Google Scholar]
- Park, K.; Lee, D.J.; Heo, P.; Kim, J. Development of mirror image motion system with sEMG for shoulder rehabilitation of post-stroke hemiplegic patients. Int. J. Precis. Eng. Manuf. 2012, 13, 1473–1479. [Google Scholar] [CrossRef]
- Hermens, H.J.; Freriks, B.; Disselhorst-Klug, C.; Rau, G. Development of recommendations for SEMG sensors and sensor placement procedures. J. Electromyogr. Kinesiol. 2000, 10, 361–374. [Google Scholar] [CrossRef]
- Cifrek, M.; Medved, V.; Tonković, S.; Ostojić, S. Surface EMG based muscle fatigue evaluation in biomechanics. Clin. Biomech. 2009, 24, 327–340. [Google Scholar] [CrossRef]
- Kumar, D.K.; Arjunan, S.P.; Naik, G.R. Measuring increase in synchronization to identify muscle endurance limit. IEEE Trans. Neural Syst. Rehabil. Eng. 2011, 19, 578–587. [Google Scholar] [CrossRef]
- Zijdewind, I.; Butler, J.E.; Gandevia, S.C.; Taylor, J.L. The origin of activity in the biceps brachii muscle during voluntary contractions of the contralateral elbow flexor muscles. Exp. Brain Res. 2006, 175, 526–535. [Google Scholar] [CrossRef]
- Xiao, R.; Shida-Tokeshi, J.; Vanderbilt, D.L.; Smith, B.A. Electroencephalography power and coherence changes with age and motor skill development across the first half year of life. PLoS ONE 2018, 13, e0190276. [Google Scholar] [CrossRef] [Green Version]
- Zaepffel, M.; Trachel, R.; Kilavik, B.E.; Brochier, T. Modulations of EEG beta power during planning and execution of grasping movements. PLoS ONE 2013, 8, e60060. [Google Scholar] [CrossRef] [Green Version]
- Muthukumaraswamy, S.D.; Johnson, B.W.; McNair, N.A. Mu rhythm modulation during observation of an object-directed grasp. Cogn. Brain Res. 2004, 19, 195–201. [Google Scholar] [CrossRef] [PubMed]
- Ulloa, E.R.; Pineda, J.A. Recognition of point-light biological motion: Mu rhythms and mirror neuron activity. Behav. Brain Res. 2007, 183, 188–194. [Google Scholar] [CrossRef]
- Läppchen, C.H.; Ringer, T.; Blessin, J.; Seidel, G.; Grieshammer, S.; Lange, R.; Hamzei, F. Optical illusion alters M1 excitability after mirror therapy: A TMS study. J. Neurophysiol. 2012, 108, 2857–2861. [Google Scholar] [CrossRef] [PubMed]
- Delorme, A.; Makeig, S. EEGLAB: An open source toolbox for analysis of single-trial EEG dynamics including independent component analysis. J. Neurosci. Methods 2004, 134, 9–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oberman, L.M.; Hubbard, E.M.; McCleery, J.P.; Altschuler, E.L.; Ramachandran, V.S.; Pineda, J.A. EEG evidence for mirror neuron dysfunction in autism spectrum disorders. Cogn. Brain Res. 2005, 24, 190–198. [Google Scholar] [CrossRef] [PubMed]
- Arad, E.; Bartsch, R.P.; Kantelhardt, J.W.; Plotnik, M. Performance-based approach for movement artifact removal from electroencephalographic data recorded during locomotion. PLoS ONE 2018, 13, e0197153. [Google Scholar] [CrossRef]
- Nathan, K.; Contreras-Vidal, J.L. Negligible motion artifacts in scalp electroencephalography (EEG) during treadmill walking. Front. Hum. Neurosci. 2016, 9, 708. [Google Scholar] [CrossRef] [Green Version]
- Bulea, T.C.; Kim, J.; Damiano, D.L.; Stanley, C.J.; Park, H.-S. Prefrontal, posterior parietal and sensorimotor network activity underlying speed control during walking. Front. Hum. Neurosci. 2015, 9, 247. [Google Scholar] [CrossRef] [Green Version]
- Luu, T.P.; Nakagome, S.; He, Y.; Contreras-Vidal, J.L. Real-time EEG-based brain-computer interface to a virtual avatar enhances cortical involvement in human treadmill walking. Sci. Rep. 2017, 7, 8895. [Google Scholar] [CrossRef]
- Oliveira, A.S.; Schlink, B.R.; Hairston, W.D.; König, P.; Ferris, D.P. A channel rejection method for attenuating motion-related artifacts in EEG recordings during walking. Front. Neurosci. 2017, 11, 225. [Google Scholar] [CrossRef]
- Ouahabi, A.; Depollier, C.; Simon, L.; Koume, D. Spectrum estimation from randomly sampled velocity data [LDV]. IEEE Trans. Instrum. Meas. 1998, 47, 1005–1012. [Google Scholar] [CrossRef]
- Peyton, A.J. Circuit for Monitoring the Median Frequency of the Spectrum of the Surface EMG Signal. IEEE Trans. Biomed. Eng. 1987, 34, 391–394. [Google Scholar] [CrossRef] [PubMed]
- Merletti, R.; Biey, D.; Biey, M.; Prato, G.; Orusa, A. On-Line Monitoring of the Median Frequency of the Surface EMG Power Spectrum. IEEE Trans. Biomed. Eng. 1985, 32, 1–7. [Google Scholar] [CrossRef]
- Gandolfi, M.; Formaggio, E.; Geroin, C.; Storti, S.F.; Boscolo Galazzo, I.; Bortolami, M.; Saltuari, L.; Picelli, A.; Waldner, A.; Manganotti, P. Quantification of upper limb motor recovery and EEG power changes after robot-assisted bilateral arm training in chronic stroke patients: A prospective pilot study. Neural Plast. 2018, 2018, 8105480. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arnstein, D.; Cui, F.; Keysers, C.; Maurits, N.M.; Gazzola, V. μ-suppression during action observation and execution correlates with BOLD in dorsal premotor, inferior parietal, and SI cortices. J. Neurosci. 2011, 31, 14243–14249. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bronzino, J.D. Biomedical Engineering Handbook; CRC Press: Boca Raton, FL, USA, 1999; Volume 2. [Google Scholar]
- Kang, S.Y.; Im, C.-H.; Shim, M.; Nahab, F.B.; Park, J.; Kim, D.-W.; Kakareka, J.; Miletta, N.; Hallett, M. Brain networks responsible for sense of agency: An EEG study. PLoS ONE 2015, 10, e0135261. [Google Scholar] [CrossRef]
- Aman, J.E.; Elangovan, N.; Yeh, I.; Konczak, J. The effectiveness of proprioceptive training for improving motor function: A systematic review. Front. Hum. Neurosci. 2015, 8, 1075. [Google Scholar] [CrossRef] [Green Version]
- Canedo, A. Primary motor cortex influences on the descending and ascending systems. Prog. Neurobiol. 1997, 51, 287–335. [Google Scholar] [CrossRef]
- Carel, C.; Loubinoux, I.; Boulanouar, K.; Manelfe, C.; Rascol, O.; Celsis, P.; Chollet, F. Metabolism, Neural substrate for the effects of passive training on sensorimotor cortical representation: A study with functional magnetic resonance imaging in healthy subjects. J. Celebr. Blood Flow 2000, 20, 478–484. [Google Scholar] [CrossRef] [Green Version]
- Jang, S.H.; Kim, Y.-H.; Chang, Y.; Han, B.S.; Byun, W.M.; Chang, C.H. The predictive value of cortical activation by passive movement for motor recovery in stroke patients. Restor. Neurol. Neurosci. 2004, 22, 59–63. [Google Scholar]
- Cauraugh, J.H.; Kim, S.-B.; Summers, J.J. Chronic stroke longitudinal motor improvements: Cumulative learning evidence found in the upper extremity. Cerebrovasc. Dis. 2008, 25, 115–121. [Google Scholar] [CrossRef] [PubMed]
- Stinear, C.M.; Barber, P.A.; Coxon, J.P.; Fleming, M.K.; Byblow, W.D. Priming the motor system enhances the effects of upper limb therapy in chronic stroke. Brain 2008, 131, 1381–1390. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stinear, J.W.; Byblow, W.D. Rhythmic bilateral movement training modulates corticomotor excitability and enhances upper limb motricity poststroke: A pilot study. J. Clin. Neurophysiol. 2004, 21, 124–131. [Google Scholar] [CrossRef] [PubMed]
- Cauraugh, J.H.; Lodha, N.; Naik, S.K.; Summers, J.J. Bilateral movement training and stroke motor recovery progress: A structured review and meta-analysis. Hum. Mov. Sci. 2010, 29, 853–870. [Google Scholar] [CrossRef] [Green Version]
- Perrett, D.; Mistlin, A.; Harries, M.; Chitty, A. Understanding the visual appearance and consequence of hand actions. In Vision and Action: The Control of Grasping; Intellect Ltd.: Bristol, UK, 1990; pp. 163–180. [Google Scholar]
- Buccino, G.; Binkofski, F.; Fink, G.R.; Fadiga, L.; Fogassi, L.; Gallese, V.; Seitz, R.J.; Zilles, K.; Rizzolatti, G.; Freund, H.J. Action observation activates premotor and parietal areas in a somatotopic manner: An fMRI study. Eur. J. Neurosci. 2001, 13, 400–404. [Google Scholar] [CrossRef]
- Parsons, L.M.; Fox, P.T.; Downs, J.H.; Glass, T.; Hirsch, T.B.; Martin, C.C.; Jerabek, P.A.; Lancaster, J.L. Use of implicit motor imagery for visual shape discrimination as revealed by PET. Nature 1995, 375, 54. [Google Scholar] [CrossRef]
- Enoka, R.M.; Duchateau, J. Muscle fatigue: What, why and how it influences muscle function. J. Physiol. 2008, 586, 11–23. [Google Scholar] [CrossRef]
- Gates, D.H.; Dingwell, J.B. The effects of neuromuscular fatigue on task performance during repetitive goal-directed movements. Exp. Brain Res. 2008, 187, 573–585. [Google Scholar] [CrossRef] [Green Version]
- Formaggio, E.; Storti, S.F.; Galazzo, I.B.; Gandolfi, M.; Geroin, C.; Smania, N.; Fiaschi, A.; Manganotti, P. Time–frequency modulation of ERD and EEG coherence in robot-assisted hand performance. Brain Topogr. 2015, 28, 352–363. [Google Scholar] [CrossRef]
- Formaggio, E.; Masiero, S.; Bosco, A.; Izzi, F.; Piccione, F.; Del Felice, A. Quantitative EEG evaluation during robot-assisted foot movement. IEEE Trans. Neural Syst. Rehabil. Eng. 2016, 25, 1633–1640. [Google Scholar] [CrossRef]
- Emerson, J.R.; Binks, J.A.; Scott, M.W.; Kenny, R.P.; Eaves, D.L. Combined action observation and motor imagery therapy: A novel method for post-stroke motor rehabilitation. AIMS Neurosci. 2018, 5, 236–252. [Google Scholar] [CrossRef]
- Kang, Y.J.; Ku, J.; Kim, H.J.; Park, H.K. Facilitation of corticospinal excitability according to motor imagery and mirror therapy in healthy subjects and stroke patients. Ann. Rehabil. Med. 2011, 35, 747. [Google Scholar] [CrossRef] [PubMed]
- Gatti, R.; Rocca, M.A.; Fumagalli, S.; Cattrysse, E.; Kerckhofs, E.; Falini, A.; Filippi, M. The effect of action observation/execution on mirror neuron system recruitment: An fMRI study in healthy individuals. Brain Imaging Behav. 2017, 11, 565–576. [Google Scholar] [CrossRef] [PubMed]



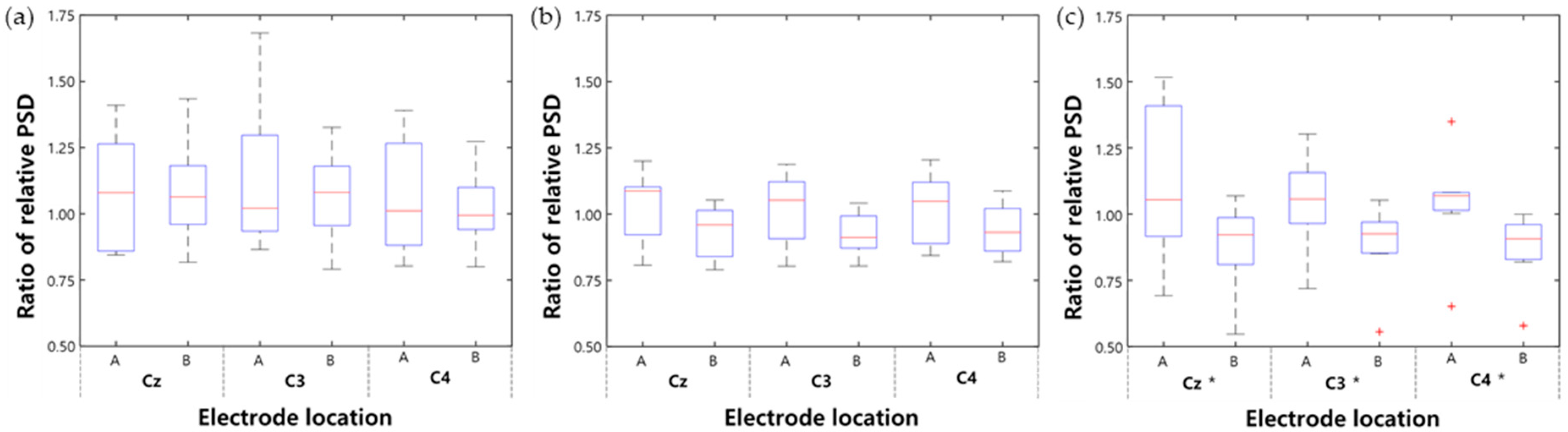

| Rehabilitation Protocol | CMT | ACMT | SCMT | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Electrode Location | Cz | C3 | C4 | Cz | C3 | C4 | Cz | C3 | C4 |
| Ratio of relative PSD after first session | 1.08 | 1.14 | 1.07 | 1.03 | 1.02 | 1.03 | 1.12 | 1.04 | 1.04 |
| Ratio of relative PSD after last session | 1.08 | 1.06 | 1.02 | 0.93 | 0.92 | 0.94 | 0.87 | 0.88 | 0.87 |
| Change after treatment (%) | 0.01 | −7.00 | −4.42 | −9.16 | −9.63 | −8.03 | −22.11 * | −15.31 * | −16.48 * |
| Change after first session (%) | 9.47 | 15.39 | 8.28 | 0.92 | 0.57 | 0.67 | 5.92 | −0.32 | −0.87 |
| Change after last session (%) | 5.86 | 5.48 | 0.40 | −8.66 | −8.97 | −8.02 | −16.08 * | −13.51 * | −15.93 * |
| Rehabilitation Protocol | CMT | ACMT | SCMT | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Electrode Location | Cz | C3 | C4 | Cz | C3 | C4 | Cz | C3 | C4 |
| Theta rhythm (%) | −5.78 | 1.58 | −2.25 | 3.33 | 3.91 | 5.90 | −21.23 | −17.87 | −18.11 |
| Mu rhythm (%) | −12.52 | −15.34 | −14.26 | −9.92 | −10.34 | −7.65 | −60.71 ** | −38.08 * | −44.28 * |
| Beta rhythm (%) | −1.15 | 4.85 | −3.81 | 7.40 | 2.79 | 1.25 | −15.13 | −1.73 | −9.89 |
| Gamma rhythm (%) | −1.91 | 2.26 | −6.30 | 3.64 | 11.00 | −3.40 | 5.50 | 20.19 | −9.83 |
| Rehabilitation Type | CMT | ACMT | SCMT | |||
|---|---|---|---|---|---|---|
| MPF | RMS | MPF | RMS | MPF | RMS | |
| First session (%) | −1.66 *** | 18.61 *** | 2.61 *** | −11.67 *** | 0.13 *** | −2.11 *** |
| Last session (%) | 0.11 *** | 6.80 *** | 0.56 *** | −7.88 *** | −1.19 *** | 6.36 *** |
| Abs. avg (%) | 0.89 *** | 12.71 *** | 1.59 *** | 9.78 *** | 0.66 *** | 4.24 *** |
| Electrode Location | Cz | C3 | C4 |
|---|---|---|---|
| CMT (%) | 33.76 | 27.52 | 26.24 |
| ACMT (%) | 17.46 | 17.49 | 16.58 |
| SCMT (%) | 22.40 | 12.79 | 10.75 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, T.; Lee, M.; Jeong, T.; Shin, Y.-I.; Park, S.-M. Quantitative Analysis of EEG Power Spectrum and EMG Median Power Frequency Changes after Continuous Passive Motion Mirror Therapy System. Sensors 2020, 20, 2354. https://doi.org/10.3390/s20082354
Park T, Lee M, Jeong T, Shin Y-I, Park S-M. Quantitative Analysis of EEG Power Spectrum and EMG Median Power Frequency Changes after Continuous Passive Motion Mirror Therapy System. Sensors. 2020; 20(8):2354. https://doi.org/10.3390/s20082354
Chicago/Turabian StylePark, Taewoong, Mina Lee, Taejong Jeong, Yong-Il Shin, and Sung-Min Park. 2020. "Quantitative Analysis of EEG Power Spectrum and EMG Median Power Frequency Changes after Continuous Passive Motion Mirror Therapy System" Sensors 20, no. 8: 2354. https://doi.org/10.3390/s20082354
APA StylePark, T., Lee, M., Jeong, T., Shin, Y.-I., & Park, S.-M. (2020). Quantitative Analysis of EEG Power Spectrum and EMG Median Power Frequency Changes after Continuous Passive Motion Mirror Therapy System. Sensors, 20(8), 2354. https://doi.org/10.3390/s20082354






