Electrohysterogram for ANN-Based Prediction of Imminent Labor in Women with Threatened Preterm Labor Undergoing Tocolytic Therapy
Abstract
:1. Introduction
2. Materials and Methods
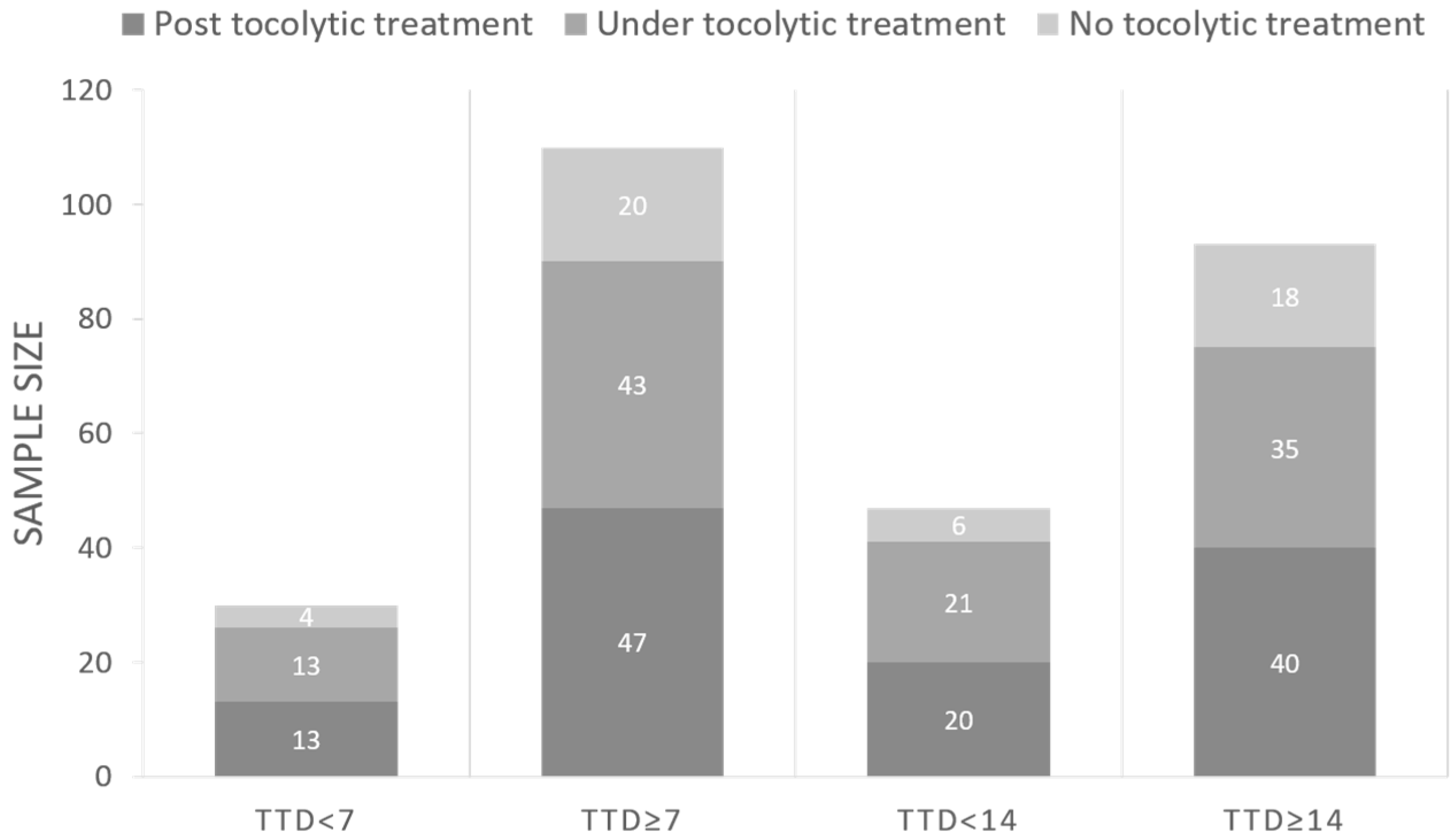
2.1. Database
2.2. EHG Characterization
2.3. Classifiers Design and Evaluation
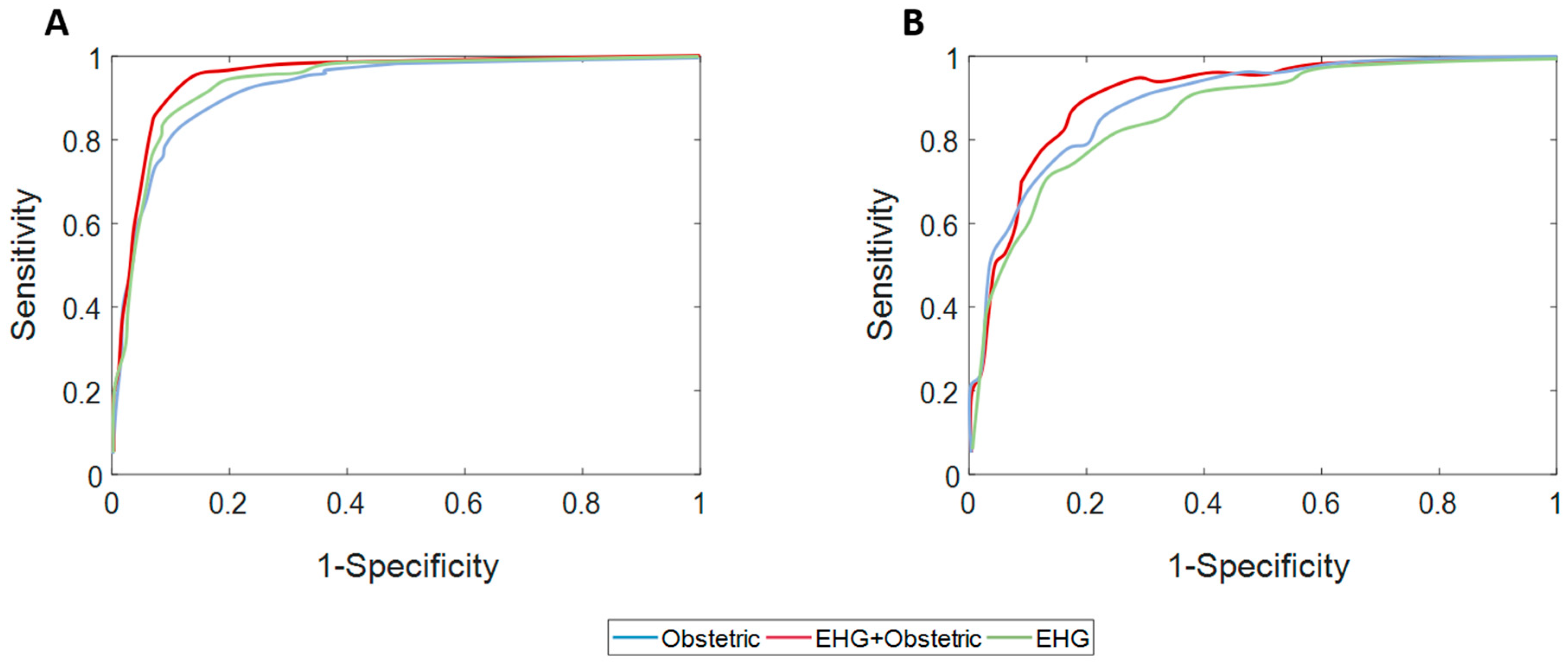
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Beck, S.; Wojdyla, D.; Say, L.; Pilar Bertran, A.; Meraldi, M.; Harris Requejo, J.; Rubens, C.; Menon, R.; Van Look, P. The worldwide incidence of preterm birth: A systematic review of maternal mortality and morbidity. Bull. World Health Organ. 2010, 88, 31–38. [Google Scholar] [CrossRef] [PubMed]
- Zeitlin, J.; Szamotulska, K.; Drewniak, N.; Mohangoo, A.D.; Chalmers, J.; Sakkeus, L.; Irgens, L.; Gatt, M.; Gissler, M.; Blondel, B. Preterm birth time trends in Europe: A study of 19 countries. BJOG 2013, 120, 1356–1365. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goldenberg, R.L.; Culhane, J.F.; Iams, J.D.; Romero, R. Epidemiology and causes of preterm birth. Lancet 2008, 371, 75–84. [Google Scholar] [CrossRef]
- Petrou, S. The economic consequences of preterm birth duringthe first 10 years of life. BJOG An Int. J. Obstet. Gynaecol. 2005, 112, 10–15. [Google Scholar] [CrossRef]
- Butler, A.S.; Behrman, R.E. (Eds.) Preterm Birth: Causes, Consequences, and Prevention; National academies press: Washington, DC, USA, 2007. [Google Scholar]
- Lucovnik, M.; Chambliss, L.R.; Garfield, R.E. Costs of unnecessary admissions and treatments for “threatened preterm labor”. Am. J. Obstet. Gynecol. 2013, 209, 213–217. [Google Scholar] [CrossRef]
- Haas, D.M.; Benjamin, T.; Sawyer, R.; Quinney, S.K. Short-term tocolytics for preterm delivery—Current perspectives. Int. J. Womens. Health 2014, 6, 343–349. [Google Scholar] [CrossRef] [Green Version]
- Garfield, R.E.; Maner, W.L. Biophysical methods of prediction and prevention of preterm labor: Uterine electromyography and cervical light-induced fluorescence—New obstetrical diagnostic techniques. In Preterm Birth; CRC Press: Boca Raton, FL, USA, 2006; pp. 131–144. [Google Scholar]
- Euliano, T.Y.; Nguyen, M.T.; Darmanjian, S.; McGorray, S.P.; Euliano, N.; Onkala, A.; Gregg, A.R. Monitoring uterine activity during labor: A comparison of 3 methods. Am. J. Obstet. Gynecol. 2013, 208, 66.e1–66.e6. [Google Scholar] [CrossRef] [Green Version]
- Devedeux, D.; Marque, C.; Mansour, S.; Germain, G.; Duchêne, J. Uterine electromyography: A critical review. Am. J. Obstet. Gynecol. 1993, 169, 1636–1653. [Google Scholar] [CrossRef]
- Chkeir, A.; Fleury, M.J.; Karlsson, B.; Hassan, M.; Marque, C. Patterns of electrical activity synchronization in the pregnant rat uterus. BioMedicine 2013, 3, 140–144. [Google Scholar] [CrossRef]
- Fele-Žorž, G.; Kavšek, G.; Novak-Antolič, Ž.; Jager, F. A comparison of various linear and non-linear signal processing techniques to separate uterine EMG records of term and pre-term delivery groups. Med. Biol. Eng. Comput. 2008, 46, 911–922. [Google Scholar] [CrossRef]
- Horoba, K.; Jezewski, J.; Matonia, A.; Wrobel, J.; Czabanski, R.; Jezewski, M. Early predicting a risk of preterm labour by analysis of antepartum electrohysterograhic signals. Biocybern. Biomed. Eng. 2016, 36, 574–583. [Google Scholar] [CrossRef]
- Vinken, M.P.G.C.; Rabotti, C.; Mischi, M.; Oei, S.G. Accuracy of Frequency-Related Parameters of the Electrohysterogram for Predicting Preterm Delivery. Obstet. Gynecol. Surv. 2009, 64, 529–541. [Google Scholar] [CrossRef] [PubMed]
- Vrhovec, J.; Macek-Lebar, A.; Rudel, D. Evaluating Uterine Electrohysterogram with Entropy. In Proceedings of the 11th Mediterranean Conference on Medical and Biomedical Engineering and Computing, Ljubljana, Slovenia, 26–30 June 2007; pp. 144–147. [Google Scholar] [CrossRef]
- Diab, A.; Hassan, M.; Marque, C.; Karlsson, B. Performance analysis of four nonlinearity analysis methods using a model with variable complexity and application to uterine EMG signals. Med. Eng. Phys. 2014, 36, 761–767. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lemancewicz, A.; Borowska, M.; Kuć, P.; Jasińska, E.; Laudański, P.; Laudański, T.; Oczeretko, E. Early diagnosis of threatened premature labor by electrohysterographic recordings—The use of digital signal processing. Biocybern. Biomed. Eng. 2016, 36, 302–307. [Google Scholar] [CrossRef]
- Hassan, M.; Terrien, J.; Marque, C.; Karlsson, B. Comparison between approximate entropy, correntropy and time reversibility: Application to uterine electromyogram signals. Med. Eng. Phys. 2011, 33, 980–986. [Google Scholar] [CrossRef]
- Fergus, P.; Idowu, I.; Hussain, A.; Dobbins, C. Advanced artificial neural network classification for detecting preterm births using EHG records. Neurocomputing 2016, 188, 42–49. [Google Scholar] [CrossRef] [Green Version]
- Acharya, U.R.; Sudarshan, V.K.; Qing, S.; Tan, Z.; Lim, M.; Ew, J.; Nayak, S.; Bhandary, S.V. Automated detection of premature delivery using empirical mode and wavelet packet decomposition techniques with uterine electromyogram signals. Comput. Biol. Med. 2017, 85, 33–42. [Google Scholar] [CrossRef]
- Fergus, P.; Cheung, P.; Hussain, A.; Al-Jumeily, D.; Dobbins, C.; Iram, S. Prediction of Preterm Deliveries from EHG Signals Using Machine Learning. PLoS ONE 2013, 8. [Google Scholar] [CrossRef]
- Ren, P.; Yao, S.; Li, J.; Valdes-Sosa, P.A.; Kendrick, K.M. Improved prediction of preterm delivery using empirical mode decomposition analysis of uterine electromyography signals. PLoS ONE 2015, 10. [Google Scholar] [CrossRef] [Green Version]
- Naeem, S.M.; Seddik, A.F.; Eldosoky, M.A. New technique based on uterine electromyography nonlinearity for preterm delivery detection. J. Eng. Technol. Res. 2014, 6, 107–114. [Google Scholar] [CrossRef]
- Degbedzui, D.K.; Yüksel, M.E. Accurate diagnosis of term–preterm births by spectral analysis of electrohysterography signals. Comput. Biol. Med. 2020, 119, 103677. [Google Scholar] [CrossRef] [PubMed]
- Borowska, M.; Brzozowska, E.; Kuć, P.; Oczeretko, E.; Mosdorf, R.; Laudański, P. Identification of preterm birth based on RQA analysis of electrohysterograms. Comput. Methods Programs Biomed. 2018, 153, 227–236. [Google Scholar] [CrossRef] [PubMed]
- Vinken, M.P.G.C.; Rabotti, C.; Mischi, M.; van Laar, J.O.E.H.; Oei, S.G. Nifedipine-induced changes in the electrohysterogram of preterm contractions: Feasibility in clinical practice. Obstet. Gynecol. Int. 2010, 2010, 325635. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mas-Cabo, J.; Prats-Boluda, G.; Perales, A.; Garcia-Casado, J.; Alberola-Rubio, J.; Ye-Lin, Y. Uterine electromyography for discrimination of labor imminence in women with threatened preterm labor under tocolytic treatment. Med. Biol. Eng. Comput. 2018, 57, 401–411. [Google Scholar] [CrossRef] [PubMed]
- Bradley, A.P. The use of the area under the ROC curve in the evaluation of machine learning algorithms. Pattern Recognit. 1997, 30, 1145–1159. [Google Scholar] [CrossRef] [Green Version]
- Weiss, S.M.; Kulikowski, C.A. Computer Systems that Learn: Classification and Prediction Methods from Statistics Nets, Machine Learning, and Expert Systems; Morgan Kaufmann Publishers Inc.: Burlington, MA, USA, 1991; ISBN 9781558600652. [Google Scholar]
- Alexandersson, A.; Steingrimsdottir, T.; Terrien, J.; Marque, C.; Karlsson, B. The Icelandic 16-electrode electrohysterogram database. Sci. Data 2015, 2, 150017. [Google Scholar] [CrossRef] [Green Version]
- Maner, W.L.; Garfield, R.E.; Maul, H.; Olson, G.; Saade, G. Predicting Term and Preterm Delivery With Transabdominal Uterine Electromyography. Obstet. Gynecol. 2003, 101, 1254–1260. [Google Scholar] [CrossRef]
- Maner, W.L.; Garfield, R.E. Identification of human term and preterm labor using artificial neural networks on uterine electromyography data. Ann. Biomed. Eng. 2007, 35, 465–473. [Google Scholar] [CrossRef]
- Mas-Cabo, J.; Prats-Boluda, G.; Garcia-Casado, J.; Alberola-Rubio, J.; Perales, A.; Ye-Lin, Y. Design and Assessment of a Robust and Generalizable ANN-Based Classifier for the Prediction of Premature Birth by means of Multichannel Electrohysterographic Records. J. Sens. 2019, 2019. [Google Scholar] [CrossRef]
- Terrien, J.; Marque, C.; Karlsson, B. Spectral characterization of human EHG frequency components based on the extraction and reconstruction of the ridges in the scalogram. In Proceedings of the 2007 29th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Lyon, France, 22–26 August 2007; pp. 1872–1875. [Google Scholar] [CrossRef]
- Rooijakkers, M.J.; Rabotti, C.; Oei, S.G.; Aarts, R.M.; Mischi, M. Low-complexity intrauterine pressure estimation using the Teager energy operator on electrohysterographic recordings. Physiol. Meas. 2014, 35, 1215–1228. [Google Scholar] [CrossRef]
- Ahmed, M.U.; Chanwimalueang, T.; Thayyil, S.; Mandic, D.P. A multi variate multiscale fuzzy entropy algorithm with application to uterine EMG complexity analysis. Entropy 2017, 19, 2. [Google Scholar] [CrossRef] [Green Version]
- Moslem, B.; Hassan, M.; Khalil, M.; Marque, C.; Diab, M.O. Monitoring the progress of pregnancy and detecting labor using uterine electromyography. In Proceedings of the 2009 International Symposium On Bioelectronics & Bioinformatics, Melbourne, Australia, 9–11 December 2009; pp. 160–163. [Google Scholar]
- Karmakar, C.K.; Khandoker, A.H.; Gubbi, J.; Palaniswami, M. Complex correlation measure: A novel descriptor for Poincaré plot. Biomed. Eng. Online 2009, 8, 17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roy, B.; Ghatak, S. Nonlinear Methods to Assess Changes in Heart Rate Variability in Type 2 Diabetic Patients. Arq. Bras. Cardiol. 2013. [Google Scholar] [CrossRef] [PubMed]
- Chawla, N.V.; Bowyer, K.W.; Hall, L.O.; Kegelmeyer, W.P. SMOTE: Synthetic Minority Over-Sampling Technique. Journal of Artificial Intelligence Research. J. Artif. Intell. Res. 2002, 16, 321–357. [Google Scholar] [CrossRef]
- Smrdel, A.; Jager, F. Separating sets of term and pre-term uterine EMG records. Physiol. Meas. 2015, 36, 341–355. [Google Scholar] [CrossRef]
- Naeem, S.M.; Ali, A.F.; Eldosoky, M.A. Comparison between using linear and non-linear features to classify uterine electromyography signals of term and preterm deliveries. In Proceedings of the 2013 30th National Radio Science Conference (NRSC), Cairo, Egypt, 16–18 April 2013; pp. 492–502. [Google Scholar] [CrossRef]
- Aditya, S.; Tibarewala, D.N. Comparing ANN, LDA, QDA, KNN and SVM algorithms in classifying relaxed and stressful mental state from two-channel prefrontal EEG data. Int. J. Artif. Intell. Soft Comput. 2012, 3, 143. [Google Scholar] [CrossRef]
- Li, Q.; Rajagopalan, C.; Clifford, G.D. A machine learning approach to multi-level ECG signal quality classification. Comput. Methods Programs Biomed. 2014, 117, 435–447. [Google Scholar] [CrossRef]
- Li, Z.; Zhang, Q.; Zhao, X. Performance analysis of K-nearest neighbor, support vector machine, and artificial neural network classifiers for driver drowsiness detection with different road geometries. Int. J. Distrib. Sens. Netw. 2017, 13. [Google Scholar] [CrossRef]
- Murthy, H.S.N.; Meenakshi, D.M. ANN, SVM and KNN Classifiers for Prognosis of Cardiac Ischemia—A Comparison. Bonfring Int. J. Res. Commun. Eng. 2015, 5, 7–11. [Google Scholar] [CrossRef]
- Suguna, N.; Thanushkodi, K. An Improved k-Nearest Neighbor Classification Using Genetic Algorithm. IJCSI Int. J. Comput. Sci. 2010, 7, 7–10. [Google Scholar]
- Ren, J. ANN vs. SVM: Which one performs better in classification of MCCs in mammogram imaging. Knowledge-Based Syst. 2012, 26, 144–153. [Google Scholar] [CrossRef] [Green Version]
- Zhang, G.; Patuwo, B.E.; Hu, M.Y. Forecasting with artificial neural networks: The state of the art. Int. J. Forecast. 1998, 14, 35–62. [Google Scholar] [CrossRef]
- Bottou, L. Neural Networks: Tricks of the Trade; Springer: Berlin, Heidelberg, 2012; Volume 7700, ISBN 978-3-642-35288-1. [Google Scholar]
- Caruana, R.; Lawrence, S.; Giles, L. Overfitting in Neural Nets: Backpropagation, Conjugate Gradient, and Early Stopping. Adv. Neural Inf. Process. Syst. 2000, 402–408. [Google Scholar] [CrossRef]
- Diab, A.; Hassan, M.; Boudaoud, S.; Marque, C.; Karlsson, B. Nonlinear estimation of coupling and directionality between signals: Application to uterine EMG propagation. In Proceedings of the 2013 35th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Osaka, Japan, 3–7 July 2013; pp. 4366–4369. [Google Scholar] [CrossRef] [Green Version]
- Most, O.; Langer, O.; Kerner, R.; Ben David, G.; Calderon, I. Can myometrial electrical activity identify patients in preterm labor? Am. J. Obstet. Gynecol. 2008, 199, 378. [Google Scholar] [CrossRef] [PubMed]
- Mas-Cabo, J.; Prats-Boluda, G.; Ye-Lin, Y.; Alberola-Rubio, J.; Perales, A.; Garcia-Casado, J. Characterization of the effects of Atosiban on uterine electromyograms recorded in women with threatened preterm labor. Biomed. Signal Process. Control 2019, 52, 198–205. [Google Scholar] [CrossRef]
- You, J.; Kim, Y.; Seok, W.; Lee, S.; Sim, D.; Park, K.S.; Park, C. Multivariate Time–Frequency Analysis of Electrohysterogram for Classification of Term and Preterm Labor. J. Electr. Eng. Technol. 2019, 14, 897–916. [Google Scholar] [CrossRef]
- Roos, C.; Schuit, E.; Scheepers, H.; Bloemenkamp, K.; Bolte, A.; Duvekot, H.; van Eyck, J.; Kok, J.; Kwee, A.; Merién, A.; et al. Predictive Factors for Delivery within 7 Days after Successful 48-Hour Treatment of Threatened Preterm Labor. Am. J. Perinatol. Rep. 2015, 5, e141–e149. [Google Scholar] [CrossRef] [Green Version]
- Liao, J.B.; Buhimschi, C.S.; Norwitz, E.R. Normal labor: Mechanism and duration. Obstet. Gynecol. Clin. North Am. 2005, 32, 145–164. [Google Scholar] [CrossRef]
- Ye-Lin, Y.; Garcia-Casado, J.; Prats-Boluda, G.; Alberola-Rubio, J.; Perales, A. Automatic identification of motion artifacts in EHG recording for robust analysis of uterine contractions. Comput. Math. Methods Med. 2014, 2014. [Google Scholar] [CrossRef] [Green Version]


| EHG Temporal Parameters | EHG Spectral Parameters | EHG Non-Linear Parameters | Obstetric Data |
|---|---|---|---|
| Peak-to-peak amplitude | DF1 DF2 H/L Ratio Deciles [D1-D9] Teager Energy | Binary Lempel-Ziv Multistate Lempel-Ziv (n = 6) Sample Entropy Spectral Entropy Fuzzy Entropy Time reversibility SD1 SD2 SD1/SD2 | Cervical length Gestational age at moment of recording Maternal age Gestations Parity Abortions |
| TTD < 7 | TTD ≥ 7 | p-Value | TTD < 14 | TTD ≥ 14 | p-Value | |
|---|---|---|---|---|---|---|
| Cervical length (mm) | 13.67 ± 8.32 | 21.34 ± 12.07 | 0.001 | 14.13 ± 8.67 | 22.59 ± 12.17 | 7 × 10−5 |
| Gestational age at recording (weeks) | 32.17 ± 2.09 | 30.50 ± 3.10 | 0.003 | 31.48 ± 2.34 | 30.53 ± 3.23 | 0.075 |
| Maternal age (years) | 31.80 ± 4.56 | 31.89 ± 6.17 | 0.628 | 31.73 ± 5.66 | 31.95 ± 5.97 | 0.937 |
| Gestation | 1.80 ± 1.27 | 1.85 ± 1.13 | 0.487 | 1.69 ± 1.11 | 1.91 ± 1.18 | 0.140 |
| Parity | 0.40 ± 0.67 | 0.45 ± 0.58 | 0.481 | 0.39 ± 0.58 | 0.52 ± 0.60 | 0.065 |
| Abortion | 0.27 ± 0.83 | 0.33 ± 0.69 | 0.196 | 0.31 ± 0.80 | 0.32 ± 0.68 | 0.386 |
| TTD < 7 | TTD ≥ 7 | p-Value | TTD < 14 | TTD ≥ 14 | p-Value | |
|---|---|---|---|---|---|---|
| Peak-to-peak amplitude (µV) | 144.0 ± 72.4 | 154.8 ± 206.5 | 0.482 | 136.4 ± 63.5 | 160.8 ± 224.5 | 0.977 |
| DF1 (Hz) | 0.269 ± 0.02 | 0.266 ± 0.019 | 0.650 | 0.268 ± 0.02 | 0.266 ± 0.019 | 0.520 |
| DF2 (Hz) | 0.399 ± 0.015 | 0.401 ± 0.024 | 0.966 | 0.397 ± 0.014 | 0.403 ± 0.025 | 0.374 |
| H/L Ratio | 0.410 ± 0.084 | 0.428 ± 0.073 | 0.237 | 0.42 ± 0.09 | 0.426 ± 0.068 | 0.344 |
| Decile 1 (Hz) | 0.223 ± 0.007 | 0.223 ± 0.006 | 0.976 | 0.224 ± 0.008 | 0.222 ± 0.005 | 0.460 |
| Decile 2 (Hz) | 0.243 ± 0.012 | 0.243 ± 0.011 | 0.579 | 0.245 ± 0.015 | 0.242 ± 0.009 | 0.797 |
| Decile 3 (Hz) | 0.262 ± 0.016 | 0.264 ± 0.014 | 0.509 | 0.265 ± 0.018 | 0.263 ± 0.012 | 0.642 |
| Decile 4 (Hz) | 0.284 ± 0.019 | 0.287 ± 0.017 | 0.369 | 0.287 ± 0.02 | 0.286 ± 0.016 | 0.974 |
| Decile 5 (Hz) | 0.308 ± 0.023 | 0.312 ± 0.019 | 0.383 | 0.311 ± 0.022 | 0.312 ± 0.018 | 0.781 |
| Decile 6 (Hz) | 0.336 ± 0.028 | 0.341 ± 0.022 | 0.271 | 0.338 ± 0.025 | 0.341 ± 0.022 | 0.445 |
| Decile 7 (Hz) | 0.371 ± 0.032 | 0.380 ± 0.026 | 0.109 | 0.374 ± 0.028 | 0.381 ± 0.027 | 0.177 |
| Decile 8 (Hz) | 0.427 ± 0.039 | 0.439 ± 0.033 | 0.077 | 0.431 ± 0.037 | 0.439 ± 0.034 | 0.161 |
| Decile 9 (Hz) | 0.525 ± 0.045 | 0.541 ± 0.038 | 0.103 | 0.530 ± 0.044 | 0.541 ± 0.038 | 0.221 |
| Teager energy (a.u.) | 8.6 ± 8.8 | 21.6 ± 19.9 | 0.183 | 9.1 ± 8.6 | 23.9 ± 19.8 | 0.440 |
| Binary Lempel-Ziv | 0.388 ± 0.066 | 0.437 ± 0.075 | 0.002 | 0.411 ± 0.075 | 0.435 ± 0.075 | 0.062 |
| Multistate Lempel-Ziv | 0.210 ± 0.058 | 0.241 ± 0.062 | 0.011 | 0.231 ± 0.062 | 0.236 ± 0.063 | 0.510 |
| Sample entropy | 2.173 ± 0.308 | 2.272 ± 0.243 | 0.143 | 2.261 ± 0.27 | 2.245 ± 0.257 | 0.158 |
| Spectral entropy | 0.874 ± 0.018 | 0.887 ± 0.022 | 0.003 | 0.881 ± 0.02 | 0.886 ± 0.022 | 0.078 |
| Fuzzy entropy | 0.264 ± 0.06 | 0.308 ± 0.064 | 0.002 | 0.287 ± 0.065 | 0.304 ± 0.066 | 0.152 |
| Time reversibility | 4.858 ± 3.182 | 3.554 ± 2.049 | 0.011 | 4.538 ± 2.649 | 3.467 ± 2.161 | 0.001 |
| SD1 | 2.86 ± 1.62 | 3.54 ± 3.18 | 0.126 | 3.038 ± 1.527 | 3.59 ± 3.434 | 0.385 |
| SD2 | 26.28 ± 13.03 | 27.02 ± 25.19 | 0.501 | 25.28 ± 11.57 | 27.68 ± 27.24 | 0.809 |
| SD1/SD2 | 0.116 ± 0.032 | 0.141 ± 0.045 | 0.003 | 0.129 ± 0.04 | 0.14 ± 0.045 | 0.119 |
| EHG | OBSTETRIC | EHG+OBSTETRIC | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Train | Validation | Test | Train | Validation | Test | Train | Validation | Test | |
| Accuracy | 88.2 ± 4.4 | 82.6 ± 5.8 | 76.8 ± 4.1 | 93.0 ± 4.9 | 90.9 ± 5.5 | 74.9 ± 5.2 | 89.9 ± 4.3 | 84.0 ± 4.9 | 80.2 ± 4.5 |
| AUC | 92.7 ± 3.7 | 90.0 ± 4.3 | 84.4 ± 4.8 | 94.9 ± 3.9 | 93.8 ± 4.1 | 79.6 ± 6.3 | 94.5 ± 3.1 | 91.8 ± 3.2 | 87.1 ± 4.3 |
| F1-Score | 88.3 ± 4.3 | 82.9 ± 6.0 | 77.1 ± 5.1 | 93.0 ± 4.9 | 91.1 ± 5.2 | 75.4 ± 5.4 | 89.9 ± 4.2 | 84.3 ± 5.0 | 80.3 ± 5.5 |
| Sensibility | 89.0 ± 5.2 | 84.8 ± 9.1 | 79.4 ± 9.7 | 94.1 ± 5.6 | 93.0 ± 6.1 | 77.7 ± 7.7 | 90.0 ± 4.8 | 86.5 ± 7.4 | 81.6 ± 9.4 |
| Specificity | 87.4 ± 5.9 | 80.4 ± 8.9 | 74.1 ± 8.3 | 91.8 ± 5.2 | 88.8 ± 7.6 | 72.1 ± 6.2 | 89.8 ± 6.5 | 81.5 ± 7.3 | 78.8 ± 5.8 |
| PPV | 87.8 ± 5.1 | 81.7 ± 7.0 | 75.9 ± 4.8 | 92.0 ± 4.9 | 89.6 ± 6.6 | 73.6 ± 4.9 | 90.1 ± 5.7 | 82.7 ± 5.5 | 79.6 ± 4.1 |
| NPV | 88.9 ± 4.8 | 84.8 ± 7.9 | 79.1 ± 6.4 | 94.1 ± 5.7 | 92.9 ± 6.0 | 76.7 ± 6.7 | 90.1 ± 4.6 | 86.2 ± 6.3 | 81.8 ± 7.0 |
| EHG | OBSTETRIC | EHG+OBSTETRIC | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Train | Validation | Test | Train | Validation | Test | Train | Validation | Test | |
| Accuracy | 81.2 ± 7.0 | 75.4 ± 7.1 | 65.6 ± 5.6 | 81.3 ± 11.5 | 75.8 ± 11.5 | 70.4 ± 8.2 | 83.6 ± 3.7 | 78.9 ± 3.7 | 71.1 ± 5.7 |
| AUC | 86.4 ± 7.8 | 83.6 ± 7.3 | 71.1 ± 7.4 | 83.8 ± 10.7 | 81.8 ± 11.1 | 75.5 ± 8.2 | 89.5 ± 3.2 | 86.6 ± 3.1 | 76.2 ± 5.8 |
| F1-Score | 81.7 ± 4.9 | 75.3 ± 5.6 | 65.9 ± 5.7 | 82.1 ± 10.5 | 75.8 ± 11.8 | 70.8 ± 8.3 | 83.5 ± 3.9 | 76.5 ± 4.3 | 70.8 ± 6.9 |
| Sensibility | 83.0 ± 6.6 | 74.8 ± 11.3 | 67.6 ± 13.2 | 85 ± 12.2 | 77.1 ± 16.1 | 72.6 ± 12.9 | 87.6 ± 6.0 | 77.5 ± 8.7 | 70.8 ± 12 |
| Specificity | 79.3 ± 16.1 | 76.0 ± 14.2 | 63.6 ± 12.6 | 77.7 ± 17.9 | 74.4 ± 18.8 | 68.2 ± 17.0 | 83.7 ± 5.3 | 78.7 ± 9.3 | 70.0 ± 10.9 |
| PPV | 81.3 ± 4.6 | 78.4 ± 10.0 | 66.5 ± 6.4 | 80.2 ± 11.1 | 76.4 ± 11.8 | 70.6 ± 8.9 | 83.8 ± 4.5 | 78.8 ± 6.6 | 68.8 ± 6.9 |
| NPV | 95.5 ± 4.5 | 90.8 ± 5.2 | 62.9 ± 6.9 | 90.0 ± 8.4 | 88.8 ± 10.0 | 65.5 ± 7.4 | 83.8 ± 5.1 | 76.7 ± 5.0 | 68.8 ± 7.7 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mas-Cabo, J.; Prats-Boluda, G.; Garcia-Casado, J.; Alberola-Rubio, J.; Monfort-Ortiz, R.; Martinez-Saez, C.; Perales, A.; Ye-Lin, Y. Electrohysterogram for ANN-Based Prediction of Imminent Labor in Women with Threatened Preterm Labor Undergoing Tocolytic Therapy. Sensors 2020, 20, 2681. https://doi.org/10.3390/s20092681
Mas-Cabo J, Prats-Boluda G, Garcia-Casado J, Alberola-Rubio J, Monfort-Ortiz R, Martinez-Saez C, Perales A, Ye-Lin Y. Electrohysterogram for ANN-Based Prediction of Imminent Labor in Women with Threatened Preterm Labor Undergoing Tocolytic Therapy. Sensors. 2020; 20(9):2681. https://doi.org/10.3390/s20092681
Chicago/Turabian StyleMas-Cabo, J., G. Prats-Boluda, J. Garcia-Casado, J. Alberola-Rubio, R. Monfort-Ortiz, C. Martinez-Saez, A. Perales, and Y. Ye-Lin. 2020. "Electrohysterogram for ANN-Based Prediction of Imminent Labor in Women with Threatened Preterm Labor Undergoing Tocolytic Therapy" Sensors 20, no. 9: 2681. https://doi.org/10.3390/s20092681
APA StyleMas-Cabo, J., Prats-Boluda, G., Garcia-Casado, J., Alberola-Rubio, J., Monfort-Ortiz, R., Martinez-Saez, C., Perales, A., & Ye-Lin, Y. (2020). Electrohysterogram for ANN-Based Prediction of Imminent Labor in Women with Threatened Preterm Labor Undergoing Tocolytic Therapy. Sensors, 20(9), 2681. https://doi.org/10.3390/s20092681







