A Scoping Review of Integrated Blockchain-Cloud (BcC) Architecture for Healthcare: Applications, Challenges and Solutions
Abstract
:1. Introduction
- We present the limitations of a healthcare system that is based on either cloud or blockchain and highlight the importance of implementing an integrated BcC system for better patient care.
- We present a scoping review and devise a taxonomy of existing integrated BcC healthcare system architectures into two different types based on the nature of integration. We analyze the effectiveness and limitation of these architectures.
- We compare and analyze Blockchain as a Service (BaaS) platforms provided by different cloud service providers.
- We identify the research challenges prevailing in an integrated BcC healthcare system and possible solutions that are proposed for these issues.
2. Related Work
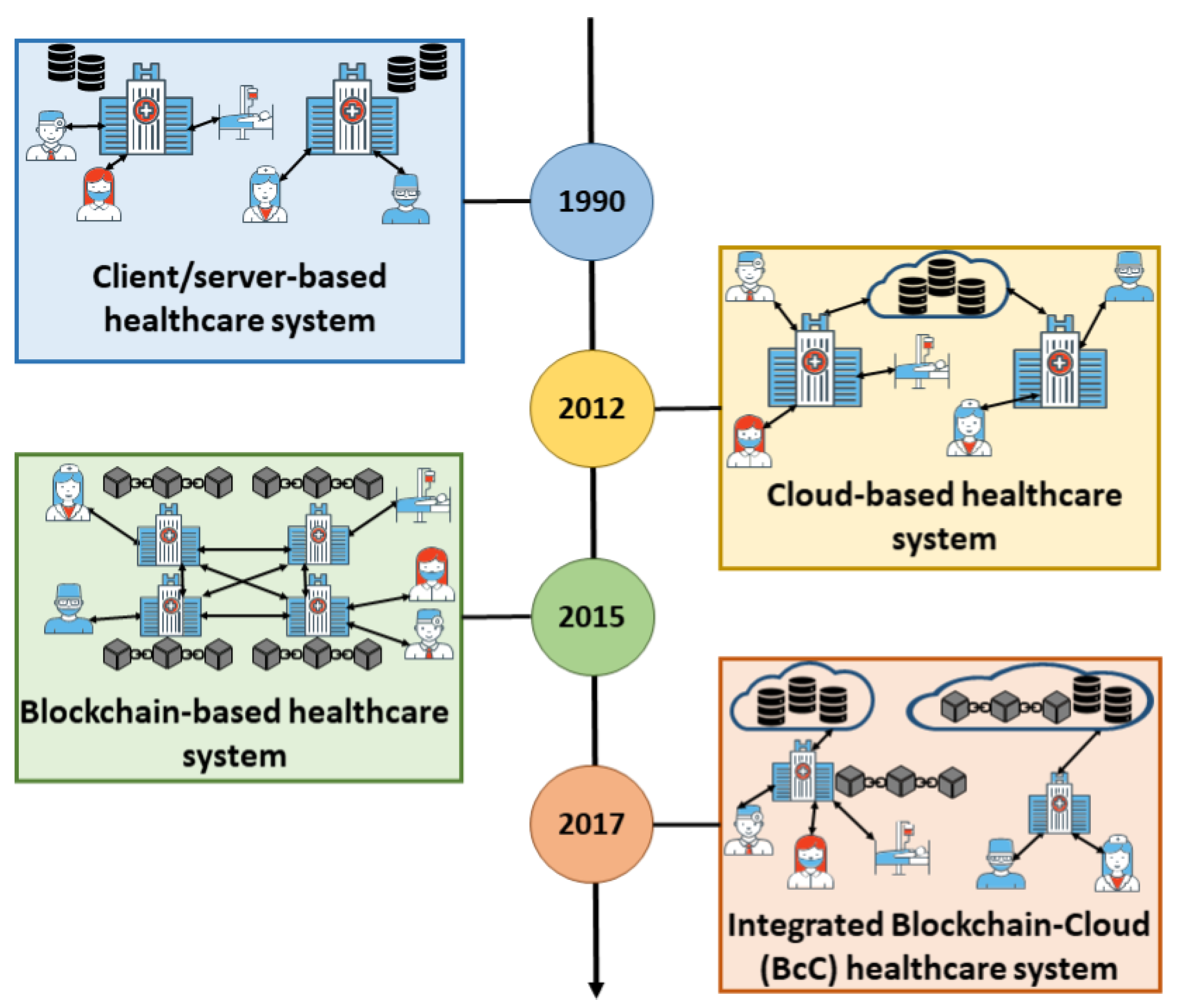
3. Background and Motivation
3.1. Background
3.1.1. Cloud Computing
- Public cloud: Allows public access to systems and services without any restrictions and is less secure.
- Private cloud: Allows members of the organization that manages the cloud to access the systems and services and is more secure than a public cloud. A private cloud when shared among multiple organizations is known as a community cloud.
- Hybrid cloud: Combination of a public and private cloud that enables greater flexibility. The critical and confidential activities can be managed using the private cloud while the general activities can be managed using the public cloud.
3.1.2. Blockchain
- Decentralization: Blockchain eliminates the intervention of a third-party entity for the processing of transactions and maintaining the ledger data. The transactions are validated and executed by the agreement of the majority of the participants that maintain the network.
- Immutability: The blockchain is a continuous chain of blocks where a block is connected to its preceding block by including the hash of the latter while hashing the former. A block is composed of a block header consisting of metadata and a block body consisting of valid transactions [21]. If a malicious entity attempts to tamper with the data of a block in past, the hash of the block will change leading to a different hash value than the one used to calculate the hash of the succeeding block. Consequently, the malicious entity needs to re-hash all the subsequent blocks in the chain up till the last block. This re-hashing is compute-intensive especially when there are several replicated copies of the ledger in the network. Thus, any data modification attempt is discouraged leading to immutability.
- Transparency: Each operation performed in the network to access the data stored in the ledger is considered as a transaction in the blockchain. Each node in the network that holds the copy of the ledger can track any unauthorized or malicious data access, making the blockchain secure and transparent.
- Traceability: The replicated ledger in the blockchain enables efficient tracing of any transaction by the nodes maintaining the ledger. This discourages any malevolent activity, making the network more secure, efficient, and transparent.
- Consensus: Each transaction in the blockchain is verified and processed by the agreement of most of the participants holding the ledger copy. This enables transactions between participants who do not know and trust each other.
- Provenance: The immutable blockchain ledger enables audit trail increasing the trust in the network. Any fraud in the network along with its source can be easily traced. This discourages malicious activities.
- Protection against natural disasters: In case of a natural disaster such as forest fires, hurricanes, and floods, a database and its regional replicas might be unavailable. In such a scenario, the globally replicated blockchain ledger can aid in fault tolerance.
- Real-time data access: Patient’s health records can be accessed in real-time from the local or the nearest copy of the ledger to avoid life-threatening situations.
- Accurate patient care: The cohesive view of a patient’s health records provided by the blockchain enables allied health professionals in better prognosis/diagnosis.
3.2. Motivation of Integrated BcC for Healthcare
4. Taxonomy and Strength/Weaknesses of Integrated BcC Healthcare System Architectures
4.1. Encapsulated Architecture
- Step 1:
- A transaction initiator (network participant) hashes the health record (transaction payload).
- Step 2:
- The digital signature of the payload is generated by encrypting the hashed transaction.
- Step 3:
- The transaction payload along with the digital signature is broadcasted to the blockchain nodes running in the cloud instances.
- Step 4:
- The transaction is validated, and the block is generated based on the consensus mechanism.
- Step 5:
- The block is updated to the ledger.
4.2. Non-Encapsulated Architecture
- Step 1:
- The health records data is encrypted by the transaction initiator (network participant) and broadcasted to the third-party cloud database.
- Step 2:
- The data is stored in the cloud database.
- Step 3:
- The meta-data of the health record such as the hash of the data, the address in the cloud where the data is stored, and the access control list containing the IDs of the authorized participants is sent to the blockchain by the integrator.
- Step 4:
- The meta-data is recorded in the blockchain as a transaction and the ledge is updated upon consensus.
5. Healthcare Applications
6. Integrated BcC Architecture: Research Challenges and Possible Solutions
6.1. Scalability
6.2. Energy Consumption
6.3. Interoperability
6.4. Real-Time Data Access
7. Discussion
- Security: In the encapsulated architecture the blockchain is encapsulated within the cloud and the underlying blockchain technology is implemented by the cloud service provider. Consequently, the healthcare stakeholders have to trust the cloud service provider for data security as the cloud service provider might tamper with the patients’ records by modifying the underlying blockchain implementation. In this case, an integrated BcC healthcare system is similar to a stand-alone cloud-based healthcare system. On the other hand, in the non-encapsulated architecture, the patients’ records are stored in the cloud database, whereas the blockchain is implemented outside the cloud with each stakeholder having a copy of the ledger. The ledger includes the health records metadata. The stakeholders can track any changes in the health records by the cloud service provider. Therefore, non-encapsulated architecture addresses the issue of data security in healthcare.
- Privacy: In the encapsulated architecture, the privacy threat still exists as the cloud service provider might use the patient’s record without the patient’s knowledge. The data query transaction in the blockchain can be removed from the ledger by the cloud service provider as the provider is the one who implements the blockchain and holds the copy of the ledger. On the other, in the non-encapsulated architecture, the privacy of the health records is preserved because the blockchain is implemented outside the cloud and each stakeholder owns a copy of the ledger. Any data query will be recorded in the blockchain ledger, thus making the healthcare system private. Consequently, non-encapsulated architecture addresses the issue of privacy in healthcare.
- Medical records destruction: In the encapsulated architecture, the health records are stored in the blockchain ledger and replicated across different network participants. The records stored in the ledger cannot be destructed because of the blockchain’s immutability characteristics. Any attempt to destruct the records will be logged in the ledger. On the other hand, in the non-encapsulated architecture, the health records are stored in the cloud database and not replicated in the ledger. Only the hash of these records and the query/update events are logged in the ledger. Consequently, the destruction of records is possible. The records stored in the cloud database can be destructed and the destruction event will be stored in the ledger.
- Total cost of ownership:Table 5 shows that healthcare organizations which implement a non-encapsulated architecture incur the extra cost of recruiting on-site blockchain developer compared to encapsulated architecture.
8. Conclusions
Author Contributions
Funding
Informed Consent Statement
Conflicts of Interest
References
- Ismail, L.; Materwala, H.; Karduck, A.P.; Adem, A. Requirements of Health Data Management Systems for Biomedical Care and Research: Scoping Review. J. Med. Internet Res. 2020, 22, e17508. [Google Scholar] [CrossRef]
- Rind, D.M.; Kohane, I.S.; Szolovits, P.; Safran, C.; Chueh, H.C.; Barnett, G.O. Maintaining the confidentiality of medical records shared over the Internet and the World Wide Web. Ann. Intern. Med. 1997, 127, 138–141. [Google Scholar] [CrossRef] [PubMed]
- Schoenberg, R.; Safran, C. Internet based repository of medical records that retains patient confidentiality. BMJ 2000, 321, 1199–1203. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Uckert, F.; Görz, M.; Ataian, M.; Prokosch, H.U. Akteonline-an electronic healthcare record as a medium for information and communication. Stud. Health Technol. Inform. 2002, 90, 293–297. [Google Scholar] [PubMed]
- Grant, R.W.; Wald, J.S.; Poon, E.G.; Schnipper, J.L.; Gandhi, T.K.; Volk, L.A.; Middleton, B. Design and implementation of a web-based patient portal linked to an ambulatory care electronic health record: Patient gateway for diabetes collaborative care. Diabetes Technol. Ther. 2006, 8, 576–586. [Google Scholar] [CrossRef] [Green Version]
- Gritzalis, D.; Lambrinoudakis, C. A security architecture for interconnecting health information systems. Int. J. Med. Inform. 2004, 73, 305–309. [Google Scholar] [CrossRef]
- Ismail, L.; Materwala, H. BlockHR: A Blockchain-based Framework for Health Records Management. In Proceedings of the 12th International Conference on Computer Modeling and Simulation, Brisbane, Australia, 23–25 June 2020; pp. 164–168. [Google Scholar]
- Ismail, L.; Materwala, H.; Khan, M.A. Performance Evaluation of a Patient-Centric Blockchain-based Healthcare Records Management Framework. In Proceedings of the 2020 2nd International Electronics Communication Conference, Singapore, 8–10 July 2020; pp. 39–50. [Google Scholar]
- Chang, P.; Bjornstad, K.; Rosen, C.; McNamara, M.; Mancini, R.; Goldstein, L.; Chylack, L.; Blakely, E. Effects of iron ions, protons and X rays on human lens cell differentiation. Radiat. Res. 2005, 164, 531–539. [Google Scholar] [CrossRef]
- Mell, P.; Grance, T. The NIST Definition of Cloud Computing. 2011. Available online: http://faculty.winthrop.edu/domanm/csci411/Handouts/NIST.pdf (accessed on 27 May 2021).
- Pfitzmann, A.; Köhntopp, M. Anonymity, unobservability, and pseudonymity—A proposal for terminology. In Designing Privacy Enhancing Technologies; Springer: Berlin/Heidelberg, Germany, 2001; pp. 1–9. [Google Scholar]
- Azaria, A.; Ekblaw, A.; Vieira, T.; Lippman, A. Medrec: Using blockchain for medical data access and permission management. In Proceedings of the 2016 2nd International Conference on Open and Big Data (OBD), Vienna, Austria, 22–24 August 2016; pp. 25–30. [Google Scholar]
- Dagher, G.G.; Mohler, J.; Milojkovic, M.; Marella, P.B. Ancile: Privacy-preserving framework for access control and interoperability of electronic health records using blockchain technology. Sustain. Cities Soc. 2018, 39, 283–297. [Google Scholar] [CrossRef]
- Li, H.; Zhu, L.; Shen, M.; Gao, F.; Tao, X.; Liu, S. Blockchain-based data preservation system for medical data. J. Med. Syst. 2018, 42, 141. [Google Scholar] [CrossRef]
- Fan, K.; Wang, S.; Ren, Y.; Li, H.; Yang, Y. Medblock: Efficient and secure medical data sharing via blockchain. J. Med. Syst. 2018, 42, 136. [Google Scholar] [CrossRef] [PubMed]
- Dey, T.; Jaiswal, S.; Sunderkrishnan, S.; Katre, N. HealthSense: A medical use case of Internet of Things and blockchain. In Proceedings of the 2017 International Conference on Intelligent Sustainable Systems (ICISS), Palladam, India, 7–8 December 2017; pp. 486–491. [Google Scholar]
- Jamil, F.; Hang, L.; Kim, K.; Kim, D. A novel medical blockchain model for drug supply chain integrity management in a smart hospital. Electronics 2019, 8, 505. [Google Scholar] [CrossRef] [Green Version]
- Jayaraman, R.; Salah, K.; King, N. Improving Opportunities in healthcare supply chain processes via the Internet of Things and Blockchain Technology. Int. J. Healthc. Inf. Syst. Inform. (IJHISI) 2019, 14, 49–65. [Google Scholar] [CrossRef] [Green Version]
- He, X.; Alqahtani, S.; Gamble, R. Toward privacy-assured health insurance claims. In Proceedings of the 2018 IEEE International Conference on Internet of Things (iThings) and IEEE Green Computing and Communications (GreenCom) and IEEE Cyber, Physical and Social Computing (CPSCom) and IEEE Smart Data (SmartData), Halifax, NS, Canada, 30 July–3 August 2018; pp. 1634–1641. [Google Scholar]
- Ismail, L.; Zeadally, S. Healthcare Insurance Frauds: Taxonomy and Blockchain-based Detection Framework (Block-HI). IEEE IT Prof. 2020. [Google Scholar] [CrossRef]
- Ismail, L.; Materwala, H. A review of blockchain architecture and consensus protocols: Use cases, challenges, and solutions. Symmetry 2019, 11, 1198. [Google Scholar] [CrossRef] [Green Version]
- Bordel, B.; Alcarria, R.; Martin, D.; Sanchez-Picot, A. Trust provision in the internet of things using transversal blockchain networks. Intell. Autom. Soft Comput. 2019, 25, 155–170. [Google Scholar] [CrossRef]
- Le Nguyen, B.; Lydia, E.L.; Elhoseny, M.; Pustokhina, I.; Pustokhin, D.A.; Selim, M.M.; Nguyen, G.N.; Shankar, K. Privacy preserving blockchain technique to achieve secure and reliable sharing of IoT data. Comput. Mater. Contin. 2020, 65, 87–107. [Google Scholar] [CrossRef]
- Ismail, L.; Materwala, H. Blockchain Paradigm for Healthcare: Performance Evaluation. Symmetry 2020, 12, 1200. [Google Scholar] [CrossRef]
- Hu, Y.; Bai, G. A systematic literature review of cloud computing in eHealth. arXiv 2014, arXiv:1412.2494. [Google Scholar] [CrossRef]
- Ali, O.; Shrestha, A.; Soar, J.; Wamba, S.F. Cloud computing-enabled healthcare opportunities, issues, and applications: A systematic review. Int. J. Inf. Manag. 2018, 43, 146–158. [Google Scholar] [CrossRef]
- Mehraeen, E.; Ghazisaeedi, M.; Farzi, J.; Mirshekari, S. Security challenges in healthcare cloud computing: A systematic review. Glob. J. Health Sci. 2016, 9, 157. [Google Scholar] [CrossRef]
- Ermakova, T.; Huenges, J.; Erek, K.; Zarnekow, R. Cloud Computing in Healthcare–A Literature Review on Current State of Research. 2013. Available online: https://aisel.aisnet.org/amcis2013/HealthInformation/GeneralPresentations/17/ (accessed on 27 May 2021).
- Hölbl, M.; Kompara, M.; Kamišalić, A.; Nemec Zlatolas, L. A systematic review of the use of blockchain in healthcare. Symmetry 2018, 10, 470. [Google Scholar] [CrossRef] [Green Version]
- Kuo, T.T.; Zavaleta Rojas, H.; Ohno-Machado, L. Comparison of blockchain platforms: A systematic review and healthcare examples. J. Am. Med Informatics Assoc. 2019, 26, 462–478. [Google Scholar] [CrossRef]
- Agbo, C.C.; Mahmoud, Q.H.; Eklund, J.M. Blockchain Technology in Healthcare: A Systematic Review. In Healthcare; Multidisciplinary Digital Publishing Institute: Basel, Switzerland, 2019; Volume 7, p. 56. [Google Scholar]
- Vazirani, A.A.; O’Donoghue, O.; Brindley, D.; Meinert, E. Implementing blockchains for efficient health care: Systematic review. J. Med. Internet Res. 2019, 21, e12439. [Google Scholar] [CrossRef] [Green Version]
- Hussien, H.M.; Yasin, S.M.; Udzir, S.; Zaidan, A.A.; Zaidan, B.B. A systematic review for enabling of develop a blockchain technology in healthcare application: Taxonomy, substantially analysis, motivations, challenges, recommendations and future direction. J. Med. Syst. 2019, 43, 320. [Google Scholar] [CrossRef]
- Bahga, A.; Madisetti, V.K. A cloud-based approach for interoperable electronic health records (EHRs). IEEE J. Biomed. Health Inform. 2013, 17, 894–906. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Cardeñosa, G.; de la Torre-Díez, I.; López-Coronado, M.; Rodrigues, J.J. Analysis of cloud-based solutions on EHRs systems in different scenarios. J. Med. Syst. 2012, 36, 3777–3782. [Google Scholar] [CrossRef]
- Zangara, G.; Corso, P.P.; Cangemi, F.; Millonzi, F.; Collova, F.; Scarlatella, A. A Cloud Based Architecture to Support Electronic Health Record; IOS Press: Amsterdam, The Netherlands, 2014; Volume 207, pp. 380–389. [Google Scholar]
- Patil, H.K.; Seshadri, R. Big data security and privacy issues in healthcare. In Proceedings of the 2014 IEEE International Congress on Big Data, Anchorage, AK, USA, 27 June–2 July 2014; pp. 762–765. [Google Scholar]
- Abbas, A.; Khan, S.U. e-Health cloud: Privacy concerns and mitigation strategies. In Medical Data Privacy Handbook; Springer: Basel, Switzerland, 2015; pp. 389–421. [Google Scholar]
- Nakamoto, S. Bitcoin: A Peer-To-Peer Electronic Cash System. 2008. Available online: https://bitcoin.org/bitcoin.pdf (accessed on 27 May 2021).
- Ismail, L.; Materwala, H.; Zeadally, S. Lightweight blockchain for healthcare. IEEE Access 2019, 7, 149935–149951. [Google Scholar] [CrossRef]
- Cao, S.; Zhang, G.; Liu, P.; Zhang, X.; Neri, F. Cloud-assisted secure eHealth systems for tamper-proofing EHR via blockchain. Inf. Sci. 2019, 485, 427–440. [Google Scholar] [CrossRef]
- Al Omar, A.; Bhuiyan, M.Z.A.; Basu, A.; Kiyomoto, S.; Rahman, M.S. Privacy-friendly platform for healthcare data in cloud based on blockchain environment. Future Gener. Comput. Syst. 2019, 95, 511–521. [Google Scholar] [CrossRef]
- Kurdi, H.; Alsalamah, S.; Alatawi, A.; Alfaraj, S.; Altoaimy, L.; Ahmed, S.H. Healthybroker: A trustworthy blockchain-based multi-cloud broker for patient-centered ehealth services. Electronics 2019, 8, 602. [Google Scholar] [CrossRef] [Green Version]
- Kubendiran, M.; Singh, S.; Sangaiah, A.K. Enhanced Security Framework for E-Health Systems using Blockchain. J. Inf. Process. Syst. 2019, 15. [Google Scholar]
- Nagasubramanian, G.; Sakthivel, R.K.; Patan, R.; Gandomi, A.H.; Sankayya, M.; Balusamy, B. Securing e-health records using keyless signature infrastructure blockchain technology in the cloud. Neural Comput. Appl. 2020, 32, 639–647. [Google Scholar] [CrossRef]
- Kaur, H.; Alam, M.A.; Jameel, R.; Mourya, A.K.; Chang, V. A proposed solution and future direction for blockchain-based heterogeneous medicare data in cloud environment. J. Med. Syst. 2018, 42, 156. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, J.; Park, S.; Kim, K.; Lee, D. CORUS: Blockchain-based trustworthy evaluation system for efficacy of healthcare remedies. In Proceedings of the 2018 IEEE International Conference on Cloud Computing Technology and Science (CloudCom), Nicosia, Cyprus, 10–13 December 2018; pp. 181–184. [Google Scholar]
- Benet, J. Ipfs-content addressed, versioned, p2p file system. arXiv 2014, arXiv:1407.3561. [Google Scholar]
- Du, Y.; Liu, J.; Guan, Z.; Feng, H. A medical information service platform based on distributed cloud and blockchain. In Proceedings of the 2018 IEEE International Conference on Smart Cloud (SmartCloud), New York, NY, USA, 21–23 September 2018; pp. 34–39. [Google Scholar]
- Thwin, T.T.; Vasupongayya, S. Blockchain based secret-data sharing model for personal health record system. In Proceedings of the 2018 5th International Conference on Advanced Informatics: Concept Theory and Applications (ICAICTA), Krabi, Thailand, 14–17 August 2018; pp. 196–201. [Google Scholar]
- Zheng, X.; Mukkamala, R.R.; Vatrapu, R.; Ordieres-Mere, J. Blockchain-based personal health data sharing system using cloud storage. In Proceedings of the 2018 IEEE 20th International Conference on e-Health Networking, Applications and Services (Healthcom), Ostrava, Czech Republic, 17–20 September 2018; pp. 1–6. [Google Scholar]
- Rouhani, S.; Butterworth, L.; Simmons, A.D.; Humphery, D.G.; Deters, R. MediChain TM: A secure decentralized medical data asset management system. In Proceedings of the 2018 IEEE International Conference on Internet of Things (iThings) and IEEE Green Computing and Communications (GreenCom) and IEEE Cyber, Physical and Social Computing (CPSCom) and IEEE Smart Data (SmartData), Halifax, NS, Canada, 30 July–3 August 2018; pp. 1533–1538. [Google Scholar]
- Wang, H.; Song, Y. Secure cloud-based EHR system using attribute-based cryptosystem and blockchain. J. Med. Syst. 2018, 42, 152. [Google Scholar] [CrossRef]
- Christo, M.S.; Sarathy, P.; Priyanka, C. An Efficient Data Security in Medical Report using Block Chain Technology. In Proceedings of the 2019 International Conference on Communication and Signal Processing (ICCSP), Chennai, India, 4–6 April 2019; pp. 606–610. [Google Scholar]
- Feng, T.; Jiao, Y.; Fang, J. Secure Sharing Model Based on Block Chain in Medical Cloud (Short Paper). In International Conference on Collaborative Computing: Networking, Applications and Worksharing; Springer: Cham, Switzerland, 2019; pp. 429–438. [Google Scholar]
- Xu, J.; Xue, K.; Li, S.; Tian, H.; Hong, J.; Hong, P.; Yu, N. Healthchain: A blockchain-based privacy preserving scheme for large-scale health data. IEEE Internet Things J. 2019, 6, 8770–8781. [Google Scholar] [CrossRef]
- Chen, L.; Lee, W.K.; Chang, C.C.; Choo, K.K.R.; Zhang, N. Blockchain based searchable encryption for electronic health record sharing. Future Gener. Comput. Syst. 2019, 95, 420–429. [Google Scholar] [CrossRef]
- Chen, Y.; Ding, S.; Xu, Z.; Zheng, H.; Yang, S. Blockchain-based medical records secure storage and medical service framework. J. Med. Syst. 2019, 43, 5. [Google Scholar] [CrossRef]
- Wang, S.; Zhang, D.; Zhang, Y. Blockchain-based personal health records sharing scheme with data integrity verifiable. IEEE Access 2019, 7, 102887–102901. [Google Scholar] [CrossRef]
- Wang, Y.; Zhang, A.; Zhang, P.; Wang, H. Cloud-assisted EHR sharing with security and privacy preservation via consortium blockchain. IEEE Access 2019, 7, 136704–136719. [Google Scholar] [CrossRef]
- Liu, J.; Li, X.; Ye, L.; Zhang, H.; Du, X.; Guizani, M. BPDS: A blockchain based privacy-preserving data sharing for electronic medical records. In Proceedings of the 2018 IEEE Global Communications Conference (GLOBECOM), Abu Dhabi, United Arab Emirates, 9–13 December 2018; pp. 1–6. [Google Scholar]
- Theodouli, A.; Arakliotis, S.; Moschou, K.; Votis, K.; Tzovaras, D. On the design of a Blockchain-based system to facilitate Healthcare Data Sharing. In Proceedings of the 2018 17th IEEE International Conference On Trust, Security And Privacy in Computing and Communications/12th IEEE International Conference On Big Data Science And Engineering (TrustCom/BigDataSE), New York, NY, USA, 1–3 August 2018; pp. 1374–1379. [Google Scholar]
- Badr, S.; Gomaa, I.; Abd-Elrahman, E. Multi-tier blockchain framework for IoT-EHRs systems. Procedia Comput. Sci. 2018, 141, 159–166. [Google Scholar] [CrossRef]
- Nguyen, D.C.; Nguyen, K.D.; Pathirana, P.N. A mobile cloud based iomt framework for automated health assessment and management. In Proceedings of the 2019 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Berlin, Germany, 23–27 July 2019; pp. 6517–6520. [Google Scholar]
- Guo, R.; Shi, H.; Zheng, D.; Jing, C.; Zhuang, C.; Wang, Z. Flexible and efficient blockchain-based ABE scheme with multi-authority for medical on demand in telemedicine system. IEEE Access 2019, 7, 88012–88025. [Google Scholar] [CrossRef]
- Nguyen, D.C.; Pathirana, P.N.; Ding, M.; Seneviratne, A. Blockchain for secure ehrs sharing of mobile cloud based e-health systems. IEEE Access 2019, 7, 66792–66806. [Google Scholar] [CrossRef]
- Liang, X.; Zhao, J.; Shetty, S.; Liu, J.; Li, D. Integrating blockchain for data sharing and collaboration in mobile healthcare applications. In Proceedings of the 2017 IEEE 28th annual international symposium on personal, indoor, and mobile radio communications (PIMRC), Montreal, QC, Canada, 8–13 October 2017; pp. 1–5. [Google Scholar]
- Iqbal, J.; Umar, A.I.; Amin, N.; Waheed, A. Efficient and secure attribute-based heterogeneous online/offline signcryption for body sensor networks based on blockchain. Int. J. Distrib. Sens. Netw. 2019, 15, 1550147719875654. [Google Scholar] [CrossRef]
- Dwivedi, A.D.; Srivastava, G.; Dhar, S.; Singh, R. A decentralized privacy-preserving healthcare blockchain for IoT. Sensors 2019, 19, 326. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Uddin, M.A.; Stranieri, A.; Gondal, I.; Balasubramanian, V. Continuous patient monitoring with a patient centric agent: A block architecture. IEEE Access 2018, 6, 32700–32726. [Google Scholar] [CrossRef]
- Xia, Q.; Sifah, E.B.; Asamoah, K.O.; Gao, J.; Du, X.; Guizani, M. MeDShare: Trust-less medical data sharing among cloud service providers via blockchain. IEEE Access 2017, 5, 14757–14767. [Google Scholar] [CrossRef]
- Steinfeld, R.; Bull, L.; Zheng, Y. Content extraction signatures. In International Conference on Information Security and Cryptology; Springer: Berlin/Heidelberg, Germany, 2001; pp. 285–304. [Google Scholar]
- Xia, Q.; Sifah, E.B.; Smahi, A.; Amofa, S.; Zhang, X. BBDS: Blockchain-based data sharing for electronic medical records in cloud environments. Information 2017, 8, 44. [Google Scholar] [CrossRef]
- Zhu, X.; Shi, J.; Lu, C. Cloud health resource sharing based on consensus-oriented blockchain technology: Case study on a breast tumor diagnosis service. J. Med. Internet Res. 2019, 21, e13767. [Google Scholar] [CrossRef]
- Celiz, R.C.; De La Cruz, Y.E.; Sanchez, D.M. Cloud model for purchase management in health sector of peru based on IoT and blockchain. In Proceedings of the 2018 IEEE 9th Annual Information Technology, Electronics and Mobile Communication Conference (IEMCON), Vancouver, BC, Canada, 1–3 November 2018; pp. 328–334. [Google Scholar]
- Zilliqa. Available online: https://docs.zilliqa.com/positionpaper.pdf. (accessed on 26 September 2020).
- Sharding. Available online: https://www.investopedia.com/terms/s/sharding.asp#:~:text=DEFINITION%20of%20Sharding,process%20more%20transactions%20per%20second (accessed on 26 September 2020).
- Ismail, L.; Materwala, H. Energy-aware vm placement and task scheduling in cloud-iot computing: Classification and performance evaluation. IEEE Internet Things J. 2018, 5, 5166–5176. [Google Scholar] [CrossRef]
- Ismail, L.; Abed, E.H. Linear Power Modeling for Cloud Data Centers: Taxonomy, Locally Corrected Linear Regression, Simulation Framework and Evaluation. IEEE Access 2019, 7, 175003–175019. [Google Scholar] [CrossRef]
- Le, K.; Bilgir, O.; Bianchini, R.; Martonosi, M.; Nguyen, T.D. Managing the cost, energy consumption, and carbon footprint of internet services. Acm Sigmetrics Perform. Eval. Rev. 2010, 38, 357–358. [Google Scholar] [CrossRef]
- Tromp, J. Cuckoo cycle: A memory bound graph-theoretic proof-of-work. In International Conference on Financial Cryptography and Data Security; Springer: Berlin/Heidelberg, Germany, 2015; pp. 49–62. [Google Scholar]
- Hogan, M.; Liu, F.; Sokol, A.; Tong, J. Nist cloud computing standards roadmap. Nist Spec. Publ. 2011, 35, 6–11. [Google Scholar]
- Lamine, E.; Guédria, W.; Rius Soler, A.; Ayza Graells, J.; Fontanili, F.; Janer-García, L.; Pingaud, H. An Inventory of Interoperability in Healthcare Ecosystems: Characterization and Challenges. Enterp. Interoperability INTEROP-PGSO Vis. 2017, 1, 167–198. [Google Scholar]
- Choy, S.; Wong, B.; Simon, G.; Rosenberg, C. A hybrid edge-cloud architecture for reducing on-demand gaming latency. Multimed. Syst. 2014, 20, 503–519. [Google Scholar] [CrossRef] [Green Version]
- Annual Salary of Blockchain Developer in the USA. Available online: https://www.blockchain-council.org/blockchain/what-is-the-salary-for-a-blockchain-developer-in-the-usa/ (accessed on 19 May 2021).
- Microsoft Azure Blockchain Service Pricing. Available online: https://azure.microsoft.com/en-us/pricing/details/blockchain-service/ (accessed on 19 May 2021).
- Microsoft Surface Laptop. Available online: https://www.microsoft.com/en-us/p/surface-laptop-go/94fc0bdgq7wv?activetab=pivot:overviewtab (accessed on 19 May 2021).
- Hardware Requirements for a Bitcoin Node. Available online: https://bitcoin.org/en/posts/how-to-run-a-full-node#why-is-running-a-full-bitcoin-node-important (accessed on 19 May 2021).
- Microsoft Azure Cloud Storage Cost. Available online: https://azure.microsoft.com/en-us/pricing/details/storage/ (accessed on 19 May 2021).
- Energy Consumption of the Bitcoin Network. Available online: https://www.thebalance.com/how-much-power-does-the-bitcoin-network-use-391280#:~:text=If%20this%20data%20is%20correct,hours%20(TWh)%20per%20year.&text=One%20watt%20per%20gigahash%20per,is%20likely%20a%20conservative%20estimate (accessed on 19 May 2021).
- Number of Bitcoin Nodes. Available online: https://thenextweb.com/news/bitcoin-100000-nodes-vulnerable-cryptocurrency#:~:text=Bitcoin%20has%20nearly%20100%2C000%20nodes%2C%20but%20over%2050%25%20run%20vulnerable%20code (accessed on 19 May 2021).
- Electric Rates in the, US. Available online: https://www.electricchoice.com/electricity-prices-by-state/#:~:text=The%20average%20electricity%20rate%20is,is%2013.31%20cents%20per%20kWh (accessed on 19 May 2021).





| Work | Healthcare System Approach | Area of Focus | Contribution(s) |
|---|---|---|---|
| [25] | Cloud computing | Cloud computing in e-health | Categorization of the cloud-based works, depending on the studied areas, into: (1) framework, (2) application, and (3) security and privacy. |
| [26] | Opportunities, challenges and applications of cloud-based healthcare | Analysis of cloud computing-based healthcare in terms of opportunities (management and technical), issues (technical, legal, security and privacy), and applications (information processing and monitoring). Discussion of research and implementation implication of the system. | |
| [27] | Security challenges in cloud-based healthcare | Investigation of security challenges and recommendation for secure communication and interoperability in cloud-based healthcare. | |
| [28] | Cloud computing in healthcare | Categorization of the works based on contributions: (1) framework development, (2) application development, (3) broker development, and (4) security and privacy mechanisms development. | |
| [29] | Blockchain | Blockchain in healthcare | Categorization of the works based on contributions (framework/architecture, algorithm, consensus protocol, and bench-marking metric) and applicability (data sharing, access control, audit trail, and supply chain management). |
| [30] | Blockchain platforms with healthcare as an example | Comparison of blockchain platforms based on the following features: (1) network type, (2) consensus protocol used, (3) hardware requirement, (4) smart contract support, (5) transaction throughput, (6) scripting language, and (7) open source support. | |
| [31] | Blockchain in healthcare | Overview of blockchain and categorization of the work based on contributions: (1) EMRs sharing, (2) supply chain management, (3) biomedical research and education, (4) remote patient monitoring, (5) health insurance claims and (6) health data analytics. Challenges and limitations of blockchain-based healthcare system | |
| [32] | Blockchain implementation in healthcare | Assessment of blockchain feasibility for efficient EHRs management. | |
| [33] | Taxonomy, challenges and recommendations for blockchain-based healthcare system | Overview of blockchain and categorization of the work based on applicability: (1) clinical/medical data sharing, (2) remote patient monitoring, (3) clinical trials, and (4) health insurance. Motivation, challenges, and recommendation for a blockchain-based healthcare system. | |
| This paper | Integrated blockchain-cloud (BcC) | Taxonomy of Integrated BcC healthcare system architectures, challenges and solutions | Importance of integrated BcC healthcare system and taxonomy of existing BcC architectures. Comparison of integrated BcC platforms. Survey of different healthcare applications domains benefited by integrated BcC. Discussion of issues existing in an integrated BcC healthcare system along with possible solutions for future research directions. |
| Encapsulated BcC Platforms | Blockchain Network | Consensus | Description | Channel Support | |
|---|---|---|---|---|---|
| Cloud | Blockchain | ||||
| Microsoft Azure | Ethereum, Hyperledger Fabric, Corda, Chain, and Quorum | Consortium | Istanbul byzantine fault tolerance | Azure Blockchain Service is a BaaS with built-in consortium management that enables quick network deployment and operations with smart contract capabilities. It can be deployed using Azure portal/CLI or through Microsoft Visual Studio Code using the Azure blockchain extension. The services are offered in two tiers: (1) basic, for development and testing, and (2) standard, for deployment. | Yes (Hyperledger Fabric) |
| Amazon | Hyperledger Fabric | Consortium | - | Amazon Managed Blockchain enables easy creation of blockchain networks. The platform uses a voting API, that allows network participants to vote for adding/removing members. | Yes |
| Oracle | Hyperledger Fabric | Hybrid | Raft | Oracle Blockchain Platform enables blockchain configuration, development and execution of smart contracts, and monitoring through a web console. External applications update/query via client SDKs or REST API calls. | Yes |
| IBM | Hyperledger Fabric | Private, public and hybrid | Pluggable consensus | IBM Blockchain Platform allows to develop, test and deploy blockchain applications with smart contract capabilities using Visual Studio code extension. The platform supports multiple languages for the development of smart contracts. | Yes |
| Ethereum | Hybrid | Configurable consensus | Google blockchain enables deployment of blockchain applications with easy API integration. It allows the use of a traditional SQL database for blockchain data update/query. | No | |
| SAP | Multichain, Hyperledger Fabric and Quorum | - | - | SAP Cloud Platform Blockchain Service enables development and deployment of blockchain applications from scratch, allows to link external blockchain nodes to the cloud or to connect an external blockchain to SAP’s powerful memory data platform, HANA. | Yes (Hyperledger Fabric) |
| Hewlett- Packard (HP) | Ethereum | - | - | HPE Mission Critical Blockchain enables fault tolerant and highly scalable blockchain applications development with smart contract integration. | No |
| Alibaba | Hyperledger Fabric, Ant and Quorum | Consortium | - | Alibaba Cloud BaaS is developed on top of Alibaba cloud container service for Kubernetes clusters enabling quick development and deployment of blockchain solutions. Alibaba Cloud BaaS API allows users to manage the blockchain objects and cloud resources. | Yes (Hyperledger Fabric) |
| Huawei | Hyperledger Fabric | Consortium | Solo, fast byzantine fault tolerance, and Kafka | Huawei Blockchain Service based on Huawei containers enables easy creation, deployment, and management of blockchain solutions. | Yes (Hyperledger Fabric) |
| Baidu | Permissioned Ethereum, Hyperledger Fabric, and Baidu XuperChain | - | Pluggable consensus | Baidu BaaS enables easy development and deployment of blockchain applications with multichain and smart contracts features. | Yes |
| Work | Cloud Database | Blockchain Transaction | |||
|---|---|---|---|---|---|
| Transaction Types | Inclusion of Health Record’s Hash | Access Control Policy | |||
| Record Update Event | Record Query Event | ||||
| [49] | Encrypted health record | ✓ | ✓ | ✗ | ✗ |
| [50] | ✓ | ✓ | ✓ | ✗ | |
| [51] | ✓ | ✓ | ✗ | ✗ | |
| [52] | ✓ | ✗ | ✓ | ✓ | |
| [53] | ✓ | ✗ | ✗ | ✗ | |
| [54] | ✗ | ✗ | ✗ | ✗ | |
| [55] | ✓ | ✗ | ✓ | ✓ | |
| [56] | ✓ | ✗ | ✓ | ✗ | |
| [57] | ✓ | ✗ | ✗ | ✗ | |
| [58] | ✓ | ✗ | ✓ | ✓ | |
| [59] | ✓ | ✓ | ✓ | ✗ | |
| [60] | ✓ | ✓ | ✗ | ✗ | |
| [61] | Encrypted health record and the extraction signature | ✓ | ✓ | ✗ | ✓ |
| [62] | Health record | ✓ | ✓ | ✗ | ✓ |
| [63] | ✓ | ✗ | ✓ | ✗ | |
| [64] | ✗ | ✓ | ✗ | ✓ | |
| [65] | ✓ | ✗ | ✗ | ✗ | |
| [66] | ✓ | ✗ | ✓ | ✗ | |
| [67] | ✓ | ✓ | ✓ | ✓ | |
| [68] | ✓ | ✓ | ✗ | ✗ | |
| [69] | ✓ | ✓ | ✓ | ✓ | |
| [70] | ✓ | ✓ | ✗ | ✗ | |
| [71] | ✗ | ✓ | ✗ | ✗ | |
| [72] | ✓ | ✓ | ✗ | ✗ | |
| Healthcare System | Security | Privacy | Scalability | Real-Time Data Access | Remarks | |
|---|---|---|---|---|---|---|
| Cloud-based | ✗ | ✗ | ✓ | ✗ | The system scales but suffers from security and privacy issues. The health records can not be accessed in real-time as they are stored in the cloud. | |
| Blockchain-based | ✓ | ✓ | ✗ | ✓ | The system ensures security and privacy, and enables real-time of the health records from the local copy of the ledger. However, it does not scale. | |
| Integrated BcC | Encapsulated | ✗ | ✗ | ✓ | ✗ | The system scales but suffers from security and privacy issues. The health records can not be accessed in real-time as they are stored in the cloud. |
| Non-encapsulated | ✓ | ✓ | ✓ | ✗ | The system scales and ensures security and privacy. The health records can not be accessed in real-time as they are stored in the cloud. | |
| BcC Architecture | Cost | |
|---|---|---|
| Encapsulated | Node | $2785.68 */year |
| Transaction | $0.0001 * (50 transactions/day are not charged) | |
| Cloud storage (ledger) | $0.6 */GB/year | |
| Non-encapsulated | Node | ≈$1000 ** (4 years maintenance) |
| Cloud storage (health records) | $0.00972 ***/GB/year | |
| Blockchain developer | $136,000/year [85] | |
| Operation (energy) | $8309.7 ****/year | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ismail, L.; Materwala, H.; Hennebelle, A. A Scoping Review of Integrated Blockchain-Cloud (BcC) Architecture for Healthcare: Applications, Challenges and Solutions. Sensors 2021, 21, 3753. https://doi.org/10.3390/s21113753
Ismail L, Materwala H, Hennebelle A. A Scoping Review of Integrated Blockchain-Cloud (BcC) Architecture for Healthcare: Applications, Challenges and Solutions. Sensors. 2021; 21(11):3753. https://doi.org/10.3390/s21113753
Chicago/Turabian StyleIsmail, Leila, Huned Materwala, and Alain Hennebelle. 2021. "A Scoping Review of Integrated Blockchain-Cloud (BcC) Architecture for Healthcare: Applications, Challenges and Solutions" Sensors 21, no. 11: 3753. https://doi.org/10.3390/s21113753








