Performance and Characteristics of Wearable Sensor Systems Discriminating and Classifying Older Adults According to Fall Risk: A Systematic Review
Abstract
:1. Introduction
- RQ1
- What is the evidence of SFRA in terms of (a) discriminative capability, and (b) classification performance?
- RQ2
- Which of the previously identified risk factors for study bias can be identified among the included studies? The risk factors analyzed included: (a) low use of prospective study design, (b) use of small study samples with low amounts of fall events, (c) low consensus in features used in SFRA models; and (d) misuse of model validation methods.
2. Materials and Methods
2.1. Literature Search
2.2. Study Selection
2.3. Data Extraction
2.4. Research Questions and Data Analysis
- RQ1
- What is the evidence of SFRA in terms of (a) discriminative capacity, and (b) classification performance?
- RQ2
- Which of the previously identified risk factors for study bias can be identified among the included studies? The risk factors analyzed included: (a) low use of prospective study design, (b) use of small study samples with low amounts of fall events, (c) low consensus in features used in SFRA models, and (d) misuse of model validation methods.
3. Results
3.1. Study Characteristics
3.1.1. Authors Involved and Places Where the Research Was Conducted
3.1.2. Study Populations
3.1.3. Faller/Non-Faller (or Equivalent) Labelling Method
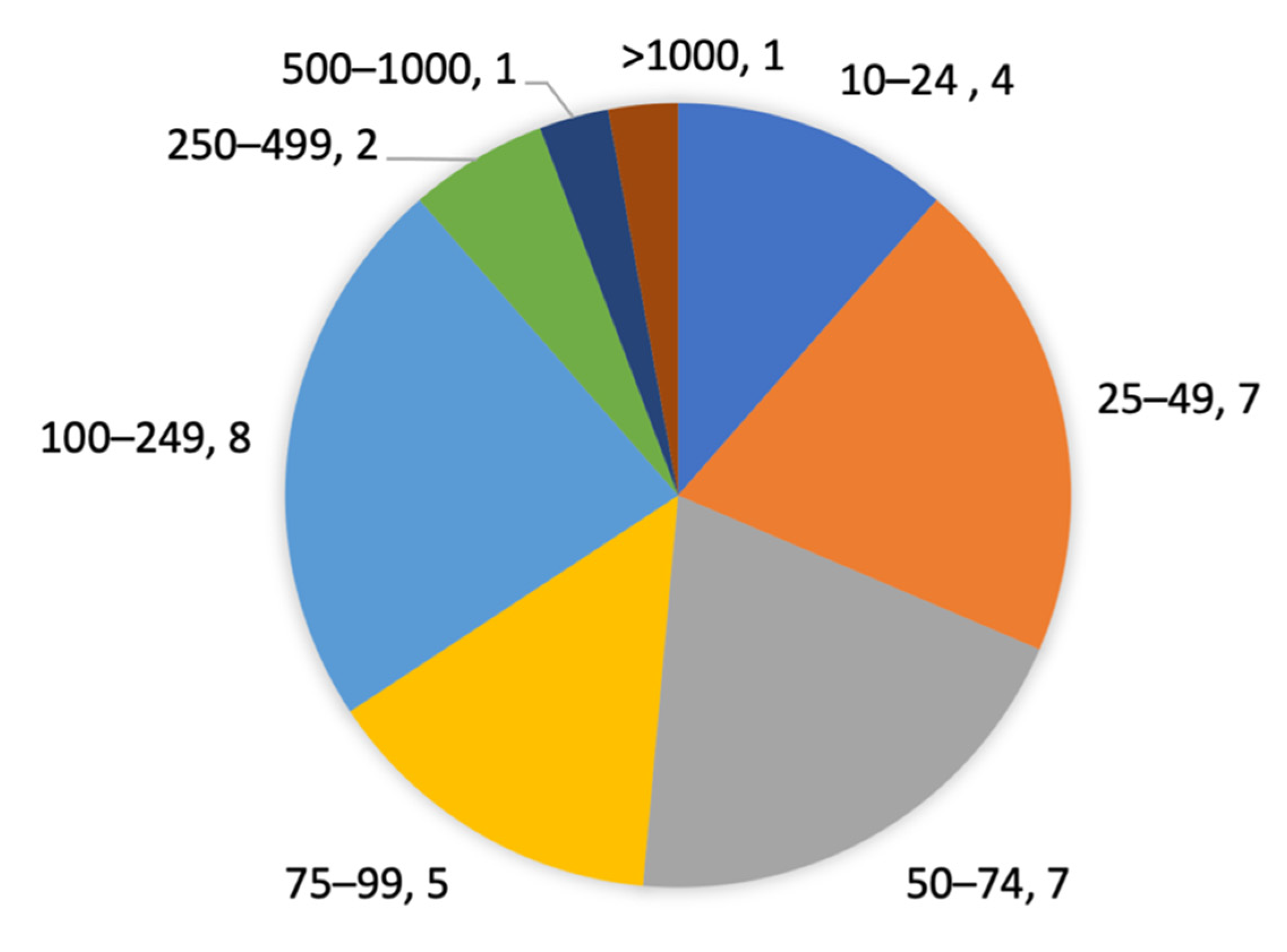
3.1.4. Size and Proportion of Participants Labelled as Fallers of Study Samples
3.1.5. Sensor-Based Fall Risk Assessment Tasks and Degree of Supervision
3.2. Wearable Sensor Used for Fall Risk Assessment
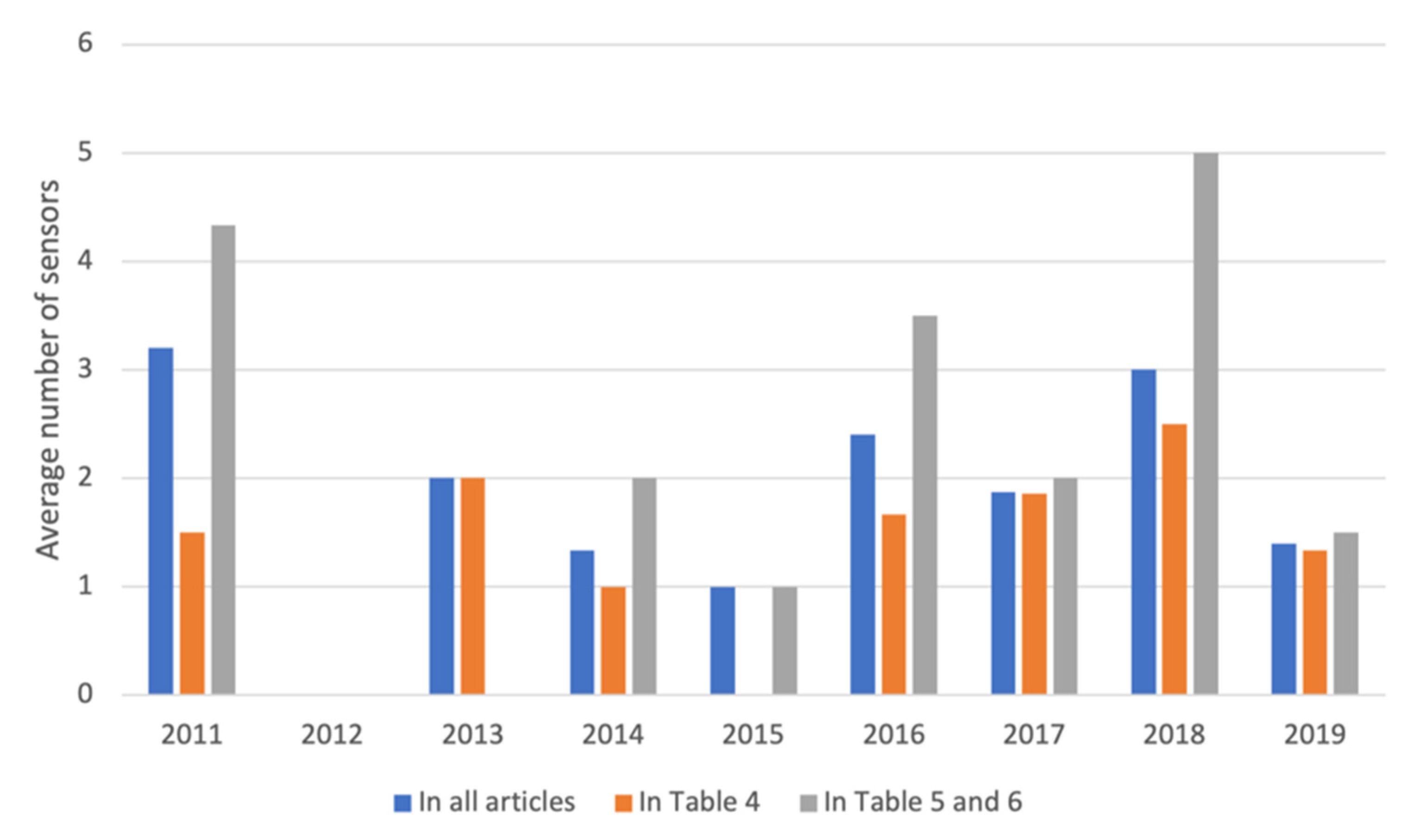
3.2.1. Number of Wearable Sensors
3.2.2. Sensor Types
3.2.3. Distribution of Wearable Sensors at Different Body Locations
3.3. Signal Processing
3.3.1. Sensor Features
3.3.2. Feature Selection
3.3.3. Fall Risk Assessment
3.4. Identification of Triads and Assessment of Applicability on Classification Methods/Models
3.5. Statistical Analyses on the Sensor-Based Methods’ Capabilities to Assess Fall Risk
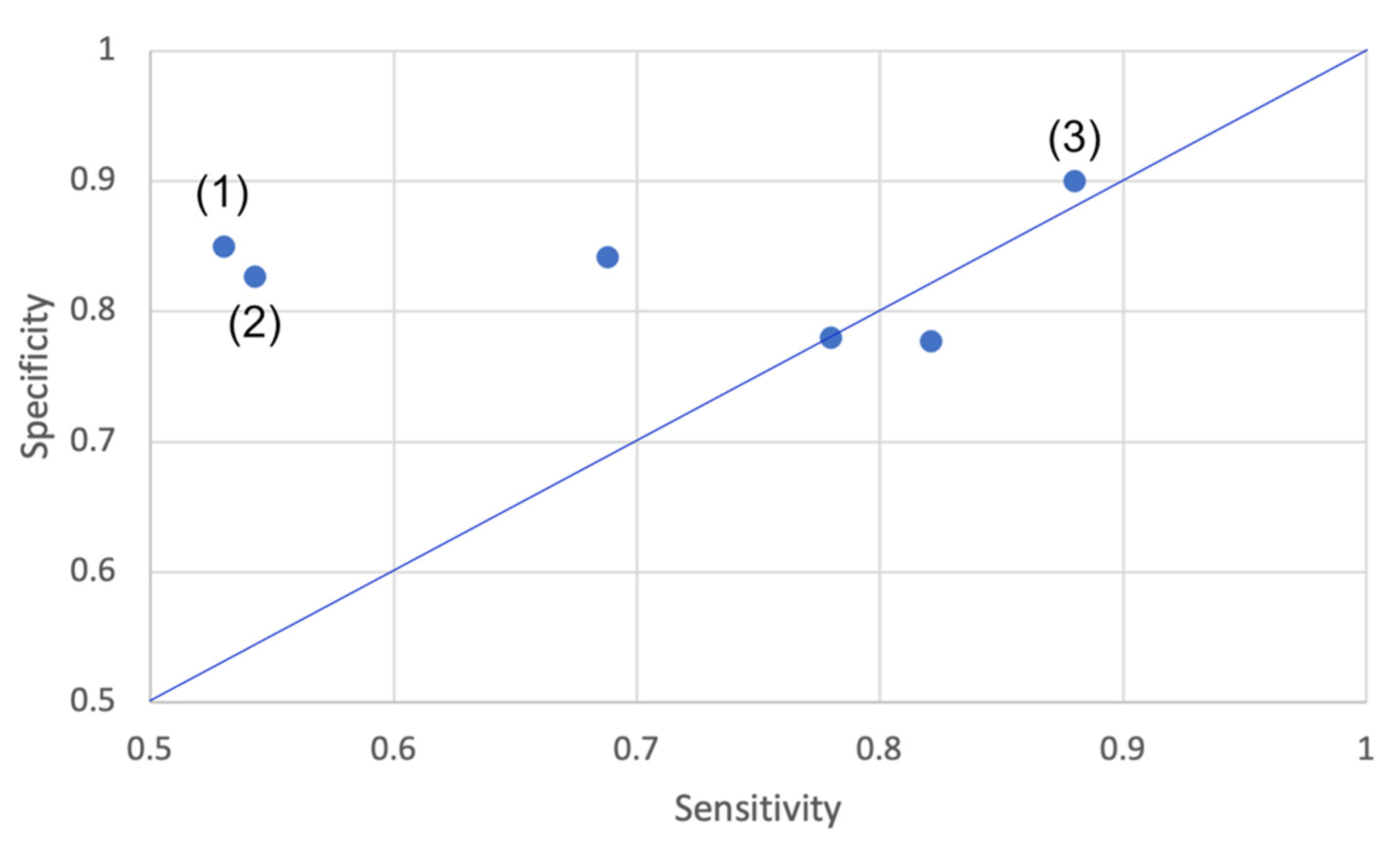
3.5.1. Capability in Discriminating Groups with Varied Level of Fall Risk
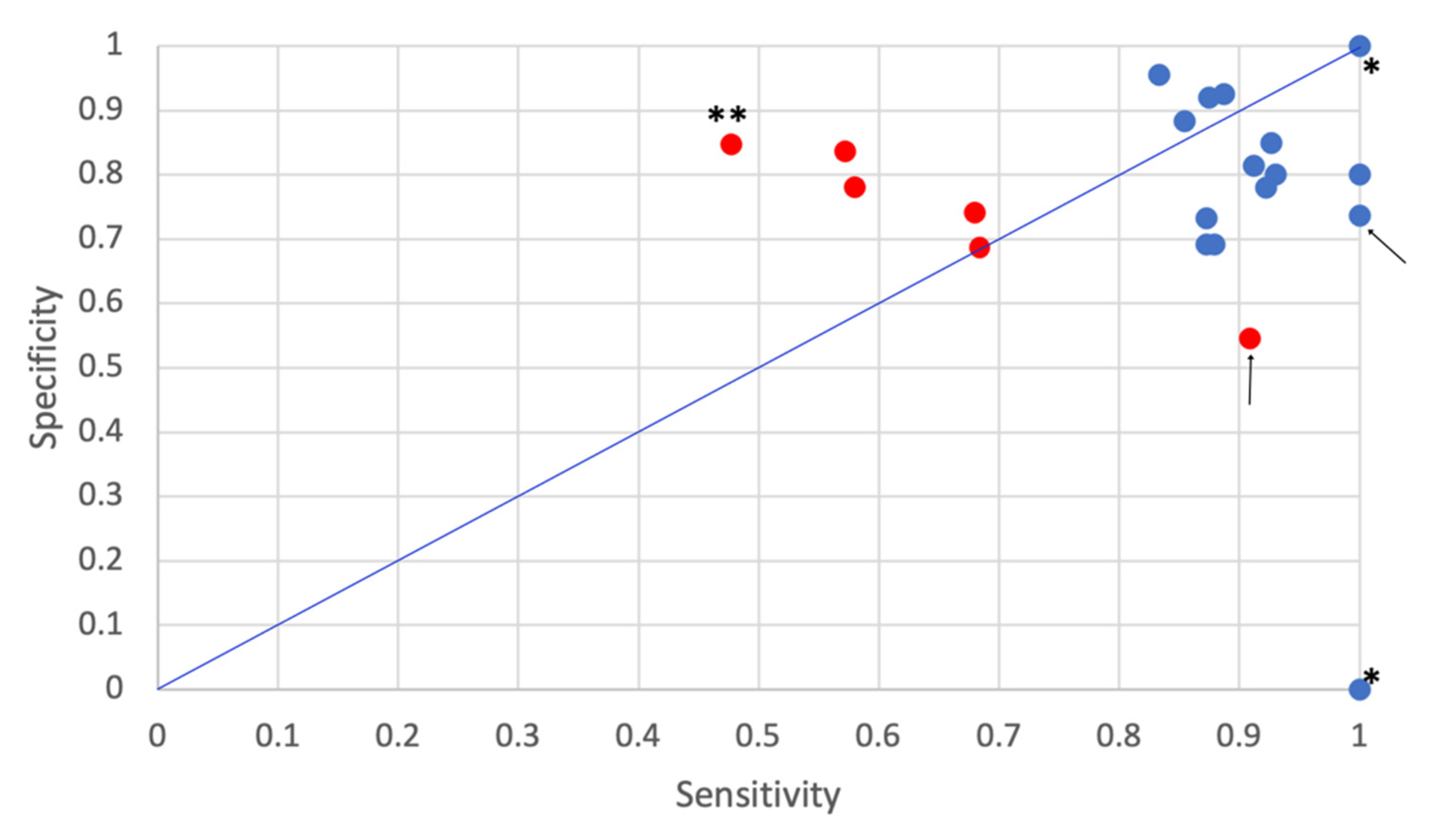
3.5.2. Capability in Classifying Individuals as Fallers/Non-Fallers (or Equivalent)
4. Discussion
5. Conclusions
6. Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| Acc | Accuracy | MML | Minimum Message Length |
| accel | Accelerometer | NEAT | Neuro evolution of augmenting topologies |
| Ada boost | Adaptive boosting | NB | Naïve Bayes(ian) |
| ADL | Activity in daily life | NN | Neural networks |
| ANOVA | Analysis of variance | NPV | Negative Predictive Value |
| ANCOVA | Analysis of co-variance | PLS-DA | Partial least square discriminatory analysis |
| AP | Anterior-posterior | POM | Proportional odds models |
| AUC | Area Under Curve (Operating Characteristics-curve) | PPV | Positive Predictive Value |
| Bag | Bootstrap aggregation | PRO | Prospective falls occurrence (followed number indicating period in months for prospective falls occurrence) |
| BBS | Bergs Balance Scale | QTUG | Quantitative TUG (a commercial tool) |
| BMI | Body Mass Index | RAI-HC | Resident Assessment Instrument—Home care |
| BST | Biometric Signature Trajectory | RBNC | Radial basis function network classifier |
| BT | Boosted tree | RCME | Refined composite multiscale entropy |
| C-GAITS | Comprehensive Gait Assessment using Inertial sensor | RE | Retrospective falls history (followed number indicating time period in months for falls history) |
| CI | Confidence intervals | RF | Random forest |
| CLIN | Clinical assessment methods | RMPE | Refined multiscale permutation entropies |
| COG | Center of gravity | RMS | Root Mean Square |
| CS | Cross-sectional | ROC | Receiver operating characteristic |
| CV | Cross validation | SagAngVel | Angular velocity in the sagittal plane |
| DT | Decision tree | SD | Standard Deviation |
| DTW | Dynamic Time Warping | SEF | Spectral Edge Frequency |
| EM | Expectation Maximization | SEMI-SUP | Semi-supervised |
| Err | Error | Sens | Sensitivity |
| F1-score | Harmonic mean of precision and Sens | SFRA | Sensor-based fall risk assessment |
| FoF | Fear of Falling | 6MWT | Six-Minutes Walking Test |
| FRE | Fall risk estimate | Spec | Specificity |
| FTSS | 5 times Sit-to-stand test | SSI | Step Stability Index |
| GMM | Gaussian Mixture Models | SSQ | Simulator Sickness Questionnaire |
| gyro | Gyroscope | SUP | Supervised |
| HR | Harmonic Ratio | SVM | Support vector machine |
| ICC | Intra-class correlation coefficient | TUG | Timed Up and Go |
| IMF | Intrinsic Mode Function | UEF | Upper extremities’ function |
| KNN | K-nearest neighbor | UNSUP | Unsupervised |
| LDS | Local Dynamic Stability | UT | Upper trunk |
| MANCOVA | Multivariate ANCOVA | Val | Validation |
| MCC | Matthew’s Correlation Coefficient | VR | Virtual reality |
| MGC | Minimum ground clearance | VRHMD | VR head-mounted display |
| ML | Medio-lateral | VT | Vertical |
Appendix A
| Variables | Type of Collected Data |
|---|---|
| 1. First author | Free text |
| 2. Title | Free text |
| 3. Journal | Free text |
| 4. Publication year | 2010–2020 |
| 5. Population of older people in sample | Patients/Community-dwelling/Residential home (or similar)/Other |
| 6. Faller/non-faller labelling method | RE and/or PRO and/or CLIN or other. For CLIN and PRO, the number of months used for collection of RE and PRO was collected. |
| 7. Number of participants 60 years in sample | Number |
| 8. Proportion of single fallers in sample | Percentage (0–100%) |
| 9. Proportion of multiple fallers in sample | Percentage (0–100%) |
| 10. Assessment task monitored by wearable sensors | Free text |
| 11. Degree of supervision during task | SUP/SEMI-SUP/UNSUP |
| 12. Number of wearable sensors | Number |
| 13. Type of wearable sensors | Free text |
| 14. Wearable sensor position(s) | Free text |
| 15. Number of sensor features | Number |
| 16. Feature selection methods | Free text |
| 17. Signal processing methods used to discriminate/classify older adults according to fall risk (a) Wearable sensor features or (b) Models/algorithms able to discriminate significantly between fallers/non-fallers with machine learning (c) Models/algorithms able to discriminate significantly between fallers/non-fallers without machine learning | (a) Free text or (b) Free text or (c) Free text |
| 18. Number of fallers/number of participants | Number/Number |
| 19. Discrimination/classification performance, either (a) Sensor features’ performance in discriminating groups with different level of fall risk (fallers/non-fallers) (b) Methods’/model’s performance in discriminating groups with different level of fall risk (fallers/non-fallers) (c) Sensor features’ performance metrics in classifying individuals as fallers/non-fallers. Only the highest performance metrics are reported. (d) Model’s performance metrics in classifying individuals as fallers/non-fallers. Only the highest performance metrics for each model are reported. | (a) and (b) Free text (c) and (d) Free text including performance metrics values |
| 20. For studies using classification methods/models (performance extracted in 19 b and d): (a) Classification models/algorithms included in discrimination method (b) Model validation method (c) Comments (of study methodology in relation to recommendations of previous review) | Free text (if used) |
| 21. For studies analyzing discriminatory performance (performance extracted in 19 (a)–(b): Number and type of features able to discriminate groups with different level of fall risk (fallers/non-fallers) | Free text |
Appendix B


Appendix C
| Ref No. | Feature Selection Methods |
|---|---|
| [19] | 1. Assessment of intra-and inter- observer reliability for gait parameters (ICC, CV of standard error of measurement) 2. Assessment of whether each parameter differed significantly between fallers/non-fallers and between walks (ANOVA and t-test, Wilcoxon-signed-rank and Kruskall–Wallis tests for step time asymmetry) 3. Analysis of each gait parameters’ predictive value (Stepwise logistic regression: forward likelihood ratio) 4. Analysis of discriminate capacity (ROC curve) |
| [21] | 1. Assessment of whether each parameter differed significantly between repetitions for each participant (ANOVA) 2. Assessment of whether each parameter differed significantly between fallers/non-fallers (One-way ANOVA) |
| [24] | 1. Assessment if whether characteristics and gait variables differed significantly between fallers/non-fallers (independent t-tests or χ2 tests) 2. Analysis of each variable and falls incidence (Stepwise logistic regression: forward stepwise selection from all variables that were significantly associated with falling), 3. Estimation of cut-off values for gait variables significantly associated with falling in logistic regression to predict falls (ROC curve) |
| [25] | 1. Assessment of whether SSI differed significantly between obstacle negotiation and baseline for controls/fallers (Wilcoxon Signed Rank) 2. Assessment of whether SSI differed significantly between fallers/controls under s different walking conditions (Mann–Whitney test) |
| [26] | Assessment of whether each parameter differed significantly between fallers/non-fallers (Two-sided Student’s t-test) |
| [30] | 1. Assessment of the abilities of median LDS of each individual parameter setting to distinguish fallers/non-fallers (Univariate logistic regression with a 10-fold CV and AUC) and testing significant discrimination ability of each parameter setting (bootstrapping with 2000 resamples) 2. Comparison the 3 algorithms’ ability to distinguish fallers/non-fallers of best performing parameter setting (Univariate logistic regression with a 10-fold CV and AUC) 3. Selection of the best performing model for the 3 algorithms (Stepwise multivariate logistic regression with stepwise backward feature selection) |
| [31] | Selection of RCME/RMPE metrics with highest discriminatory ability (PLS-DA with a backward feature selection) |
| [33] | 1. Assessment of whether each turning parameter differed significantly between non-fallers, single fallers, recurrent fallers based on RE-12 (One-way ANOVA) 2. Assessment of whether turning parameters differed significantly between non-fallers/fallers based on PRO-6 (One-way ANOVA) |
| [34] | 1. Assessment of significant differences in postural sway (RMS and NPL sway in both AP and ML directions) between balance tasks (Friedman test, Wilcoxon signed ranks test for post hoc pairwise comparisons) 2. Assessment of test-retest reliability of lower extremity muscle strength (ICC) 3. Analysis of association between postural sway and muscle strength with gait speed, number of comorbidities, grip strength and frailty index (Spearman rank correlation) 4. Assessment of whether body sway and lower extremity strength differed significantly between fallers/non-fallers (Mann–Whitney U test) |
| [35] | 1. Assessment of univariate group difference in the demographics and the walking patterns of fallers and non-fallers and further to adjust significant demographic differences between fallers/non-fallers (ANOVA, ANCOVA) 2. Assessment of associations between demographic, health, sensorimotor, psychological, and cognitive factors with the gait/mobility assessments (Pearson’s correlation and Partial Pearson’s correction (after adjusting for sex, age)) |
| [37] | 1. Assessment of whether each demographic parameter and adverse health outcomes differed significantly between the UEF index defined groups (non-frail/frail) (ANOVA) 2. Analysis of the association between the UEF index with each health outcome (Logistic regression (for nominal health outcomes) and ANOVA regression (for continuous health outcomes)) |
| [38] | 1. Assessment of the SSQ-score pre-and post-exposure (one-sample t-test and signed rank test) 2. Assessment of variable-module’s test-retest reliability for in identifying differences between 5 experimental conditions and baseline conditions (Paired t-test and Pearson’s correlation) |
| [39] | Identification of key outcome measures with significant impact on faller status (faller/non-faller) (Stepwise logistic regression, Pearson correlation to check multi-collinearity between all outcome measure pairs) |
| [40] | 1. Assessment of performance difference for TUG parameters between single task (ST), motor task (MT) and cognitive dual-task (CT) conditions (MANCOVA) 2. Assessment of the difference in individual parameters from the three TUG conditions between groups of fallers/non-fallers (ANCOVA) |
| [41] | 1. Assessment of differences between fallers and non-multiple fallers (two-sample t-test, Fisher’s exact test (for gender), Mann–Whitney-U test (for age and BMI), Wilcoxon’s signed-rank test (for pairwise differences in the gait parameters from two contrasting terrains), Benjamini-Hochberg adjustments (to control for multiple comparisons)) 2. Logistic regression, Benjamini-Hochberg adjustments on p-values (to identify individual gait parameters that were associated with multiple falls) |
| [42] | 1. Assessment of differences between fallers/non-fallers/multiple fallers in demographics and clinical and basic gait assessment (Mann–Whitney U test) 2. Analysis of each significant variable’s strength to predict falls (Logistic regression and ROC curve) |
| [43] | 1. Assessment of differences in socio-demographic parameters and subjective questionnaires among three balance groups (One-way ANOVA model) 2. Assessment of differences in balance parameters between groups (ANOVA models for normally distributed data according to Shapiro–Wilk test, Friedman test with calculation of Cohen’s effect size for data not normally distributed according to Shapiro–Wilk test) 3. Analysis of association between changes in COG sway body sway and changes with local-control(slope) and central-control(slope-log) changes due to vibration (linear Pearson correlations) |
| [44] | Assessment of differences in gait parameters between low-risk/high-risk patients (Independent samples t-test) |
| [45] | Assessment of whether the amount of DTW difference between reference and elderly fallers differed significantly from DTW differences of elderly non-fallers and reference (ANOVA) (DTW measures similarity in BST between elderly fallers and a reference BST) |
| [47] | 1. Assessment of normality of data (Shapiro–Wilk test) and of homoscedasticity (Levene’s Test of Equality of Variances) 2.Assessment of falls history (faller/non-faller) on Micro and Macro gait characteristics (General linear modelling) 3. For gait characteristics with a fall history interaction: Post hoc secondary analysis (Tukey’s test) to identify subgroups (fallers/non-fallers among OAs) that are significantly different from each other. |
| [48] | 1. Calculation of sway index (GMM, EM and MML algorithm) 2. Assessment of differences between non-fallers/fallers/multiple fallers in standing sway indices and BBS (ANOVA) 3. Assessment of the performance of 4 sway indices and BBS in predicting (once- and multiple) fallers (ROC-curve) |
| [50] | 1. Assessment of differences in demographics and gait parameters between genders (unpaired t-tests/χ2 tests) 2. Assessment of structural validity and sub-domain construct validity of the C-GAITS score (exploratory factor analysis using Unweighted least squares as extraction method) 3. Assessment of the internal consistency of the C-GAITS score (Cronbach’s alpha coefficient) 4. Assessment of correlation between C-GAITS score and walking speed (Single linear regression) 5. Assessment of association of C-GAITS score and subscale scores with variables (Unpaired t-tests) |
| Ref No. | Feature Selection Methods |
|---|---|
| [22] | 1. Assessment of significant differences between fallers and non-fallers in gait velocity and SagAngVel variables (Mann–Whitney Wilcoxon rank sum) 2. Assessment of correlation of each SagAngVel value with BBS score, manual TUG time, and gait velocity (Pearson’s correlation) |
| [23] | Pre-processing of multi-parameter datasets prior to classification modelling using a wrapper feature selection algorithm to exclude parameters with low information (wrapper subset evaluator, employing the simple logistic algorithm) |
| [27] | Sequential forward feature selection within CV procedure |
| [36] | 1. FREsensor feature selection by using nested CV 2. Validation of FREsensor using an independent dataset |
| [49] | 1. Assessment of whether FREcombined differed significantly between fallers/non-fallers (one-way ANOVA) 2. Assessment of whether mobility impairment scores (calculated from percentile scores of QTUG parameters grouped in five functional categories) (one-way ANOVA) |
| Ref No. | Feature Selection Methods |
|---|---|
| [20] | 1. Assessment of significant differences between fallers and non-fallers in each feature (t-test using Holm correction, Behrens-Fisher test) 2. Feature selection (Method in the forward wrapper selection algorithm family |
| [28] | 1.Assessment of associations between functional stair performance and participants characteristics (Spearman’s rank correlations) 2.Assessment of post-hoc medians and interquartile ranges (IQR) of stair climbing performance for subgroups with different stair-ascent strategies (Kruskal–Wallis) |
| [29] | 1. Assessment of the ability of models to classify fallers/non-fallers based (Acc, F1-score, MCC) 2. Ranking analysis for each model type: (a) NB models (n = 62), (b) SVM models (n = 155), (c) NN models (n = 155) 3. Ranking analysis of best performing models for NB, SVM, NN models (15 of each) and ClinAsses models (5) |
| [32] | 1. Assessment of the ability of the entire feature set to discriminate between the groups of older fallers/non-fallers (4 machine learning algorithms in Matlab) 2.Assessment of the ability of the individual features to distinguish between older fallers/non-fallers (Linear regression analysis) |
| [46] | 1. Assessment of whether each of the 155 outcome measures differed significantly between faller/non-faller groups (two-sample t-tests) 2. Assessment of discriminative power of each of the 38 measures (ROC analysis) 3. Building models to classify faller/non-faller by use of 6 supervised machine learning models incorporating the 38 significant measures as predictor variables and fall status as response variable 4. Validation of classification models (10-fold CV): Acc 5. Statistical analysis of overall classification accuracy of SVM and the 5 other models (two-sample t-test) |
| [51] | 1. Wearable data tested for normality (Shapiro–Wilks) 2. Assessment of whether means (or median) of each variable differed significantly between groups non-fallers/once-fallers/multiple-fallers (one-way ANOVA or Kruskal–Wallis H test) 3. Assessment of differences between groups with repeated measurements of physical activity, heart rate, and night sleep (two-way ANOVA) 4. Building models and evaluating their performance for three-class and binary fall risk classification (POM, logistic regression, DT, RF) including (a) Removal of collinear variables (multicollinear test); (b) Ranking the variables (predictors) importance in fall risk classification (recursive feature algorithm in Caret R package); (c) Training models on wearable, RAI-HC, wearable + RAI-HC |
References
- World Health Organization. Falls. Available online: https://www.who.int/news-room/fact-sheets/detail/falls (accessed on 6 August 2021).
- Rubenstein, L.Z.; Josephson, K.R. Falls and their prevention in elderly people: What does the evidence show? Med. Clin. N. Am. 2006, 90, 807–824. [Google Scholar] [CrossRef] [PubMed]
- Stevens, J.A.; Corso, P.S.; Finkelstein, E.A.; Miller, T.R. The costs of fatal and non-fatal falls among older adults. Inj. Prev. 2006, 12, 290–295. [Google Scholar] [CrossRef] [Green Version]
- Ambrose, A.F.; Paul, G.; Hausdorff, J.M. Risk factors for falls among older adults: A review of the literature. Maturitas 2013, 75, 51–61. [Google Scholar] [CrossRef]
- Gillespie, L.D.; Robertson, M.C.; Gillespie, W.J.; Sherrington, C.; Gates, S.; Clemson, L.M.; Lamb, S.E. Interventions for preventing falls in older people living in the community. Cochrane Database Syst. Rev. 2012, 2012, CD007146. [Google Scholar] [CrossRef] [PubMed]
- Hamm, J.; Money, A.G.; Atwal, A.; Paraskevopoulos, I. Fall prevention intervention technologies: A conceptual framework and survey of the state of the art. J. Biomed. Inform. 2016, 59, 319–345. [Google Scholar] [CrossRef] [Green Version]
- Shany, T.; Redmond, S.J.; Marschollek, M.; Lovell, N.H. Assessing fall risk using wearable sensors: A practical discussion. A review of the practicalities and challenges associated with the use of wearable sensors for quantification of fall risk in older people. Z. Gerontol. Geriatr. 2012, 45, 694–706. [Google Scholar] [CrossRef] [PubMed]
- Howcroft, J.; Kofman, J.; Lemaire, E.D. Review of fall risk assessment in geriatric populations using inertial sensors. J. Neuroeng. Rehabil. 2013, 10, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Shany, T.; Wang, K.; Liu, Y.; Lovell, N.H.; Redmond, S.J. Review: Are we stumbling in our quest to find the best predictor? Over-optimism in sensor-based models for predicting falls in older adults. Healthc. Technol. Lett. 2015, 2, 79–88. [Google Scholar] [CrossRef] [Green Version]
- Palumbo, P.; Palmerini, L.; Chiari, L. A probabilistic model to investigate the properties of prognostic tools for falls. Methods Inf. Med. 2015, 54, 189–197. [Google Scholar] [CrossRef]
- Harrell, F.E., Jr.; Lee, K.L.; Mark, D.B. Multivariable prognostic models: Issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat. Med. 1996, 15, 361–387. [Google Scholar] [CrossRef]
- Roeing, K.L.; Hsieh, K.L.; Sosnoff, J.J. A systematic review of balance and fall risk assessments with mobile phone technology. Arch. Gerontol. Geriatr. 2017, 73, 222–226. [Google Scholar] [CrossRef]
- Sun, R.P.; Sosnoff, J.J. Novel sensing technology in fall risk assessment in older adults: A systematic review. BMC Geriatr. 2018, 18, 14. [Google Scholar] [CrossRef] [Green Version]
- Montesinos, L.; Castaldo, R.; Pecchia, L. Wearable Inertial Sensors for Fall Risk Assessment and Prediction in Older Adults: A Systematic Review and Meta-Analysis. IEEE Trans. Neural. Syst. Rehabil. Eng. 2018, 26, 573–582. [Google Scholar] [CrossRef] [Green Version]
- Rucco, R.; Sorriso, A.; Liparoti, M.; Ferraioli, G.; Sorrentino, P.; Ambrosanio, M.; Baselice, F. Type and Location of Wearable Sensors for Monitoring Falls during Static and Dynamic Tasks in Healthy Elderly: A Review. Sensors 2018, 18, 1613. [Google Scholar] [CrossRef] [Green Version]
- Bet, P.; Castro, P.C.; Ponti, M.A. Fall detection and fall risk assessment in older person using wearable sensors: A systematic review. Int. J. Med. Inform. 2019, 130, 103946. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Luijendijk, H.J. How to create PICO questions about diagnostic tests. BMJ Evid. Based Med. 2021. [Google Scholar] [CrossRef]
- Bautmans, I.; Jansen, B.; Van Keymolen, B.; Mets, T. Reliability and clinical correlates of 3D-accelerometry based gait analysis outcomes according to age and fall-risk. Gait Posture 2011, 33, 366–372. [Google Scholar] [CrossRef]
- Caby, B.; Kieffer, S.; de Saint Hubert, M.; Cremer, G.; Macq, B. Feature extraction and selection for objective gait analysis and fall risk assessment by accelerometry. Biomed. Eng. Online 2011, 10, 1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Doheny, E.P.; Fan, C.W.; Foran, T.; Greene, B.R.; Cunningham, C.; Kenny, R.A. An instrumented sit-to-stand test used to examine differences between older fallers and non-fallers. In Proceedings of the 2011 33rd Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Boston, MA, USA, 30 August–3 September 2011; Volume 2011, pp. 3063–3066. [Google Scholar] [CrossRef]
- Greene, B.R.; McGrath, D.; Foran, T.G.; Doheny, E.P.; Caulfield, B. Body-worn sensor based surrogates of minimum ground clearance in elderly fallers and controls. In Proceedings of the 2011 33rd Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Boston, MA, USA, 30 August–3 September 2011; Volume 2011, pp. 6499–6502. [Google Scholar] [CrossRef]
- Marschollek, M.; Rehwald, A.; Wolf, K.H.; Gietzelt, M.; Nemitz, G.; zu Schwabedissen, H.M.; Schulze, M. Sensors vs. experts—A performance comparison of sensor-based fall risk assessment vs. conventional assessment in a sample of geriatric patients. BMC Med. Inform. Decis. Mak. 2011, 11, 48. [Google Scholar] [CrossRef] [Green Version]
- Doi, T.; Hirata, S.; Ono, R.; Tsutsumimoto, K.; Misu, S.; Ando, H. The harmonic ratio of trunk acceleration predicts falling among older people: Results of a 1-year prospective study. J. Neuroeng. Rehabil. 2013, 10, 7. [Google Scholar] [CrossRef] [Green Version]
- Cui, X.; Peng, C.K.; Costa, M.D.; Weiss, A.; Goldberger, A.L.; Hausdorff, J.M. Development of a new approach to quantifying stepping stability using ensemble empirical mode decomposition. Gait Posture 2014, 39, 495–500. [Google Scholar] [CrossRef] [Green Version]
- Ejupi, A.; Brodie, M.; Gschwind, Y.J.; Schoene, D.; Lord, S.; Delbaere, K. Choice stepping reaction time test using exergame technology for fall risk assessment in older people. In Proceedings of the 2014 36th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Chicago, IL, USA, 26–30 August 2014; Volume 2014, pp. 6957–6960. [Google Scholar] [CrossRef]
- Greene, B.R.; McGrath, D.; Caulfield, B. A comparison of cross-sectional and prospective algorithms for falls risk assessment. In Proceedings of the 2014 36th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Chicago, IL, USA, 26–30 August 2014; Volume 2014, pp. 4527–4530. [Google Scholar] [CrossRef]
- Brodie, M.A.; Wang, K.J.; Delbaere, K.; Persiani, M.; Lovell, N.H.; Redmond, S.J.; Del Rosario, M.B.; Lord, S.R. New Methods to Monitor Stair Ascents Using a Wearable Pendant Device Reveal How Behavior, Fear, and Frailty Influence Falls in Octogenarians. IEEE Trans. Biomed. Eng. 2015, 62, 2595–2601. [Google Scholar] [CrossRef]
- Howcroft, J.; Lemaire, E.D.; Kofman, J. Wearable-Sensor-Based Classification Models of Faller Status in Older Adults. PLoS ONE 2016, 11, e0153240. [Google Scholar] [CrossRef] [Green Version]
- Ihlen, E.A.F.; Weiss, A.; Beck, Y.; Helbostad, J.L.; Hausdorff, J.M. A comparison study of local dynamic stability measures of daily life walking in older adult community-dwelling fallers and non-fallers. J. Biomech. 2016, 49, 1498–1503. [Google Scholar] [CrossRef] [PubMed]
- Ihlen, E.A.F.; Weiss, A.; Bourke, A.; Helbostad, J.L.; Hausdorff, J.M. The complexity of daily life walking in older adult community-dwelling fallers and non-fallers. J. Biomech. 2016, 49, 1420–1428. [Google Scholar] [CrossRef] [PubMed]
- Iluz, T.; Weiss, A.; Gazit, E.; Tankus, A.; Brozgol, M.; Dorfman, M.; Mirelman, A.; Giladi, N.; Hausdorff, J.M. Can a Body-Fixed Sensor Reduce Heisenberg’s Uncertainty When It Comes to the Evaluation of Mobility? Effects of Aging and Fall Risk on Transitions in Daily Living. J. Gerontol. A Biol. Sci. Med. Sci. 2016, 71, 1459–1465. [Google Scholar] [CrossRef] [Green Version]
- Mancini, M.; Schlueter, H.; El-Gohary, M.; Mattek, N.; Duncan, C.; Kaye, J.; Horak, F.B. Continuous Monitoring of Turning Mobility and Its Association to Falls and Cognitive Function: A Pilot Study. J. Gerontol. A Biol. Sci. Med. Sci. 2016, 71, 1102–1108. [Google Scholar] [CrossRef] [Green Version]
- Alqahtani, B.A.; Ferchak, M.A.; Huppert, T.J.; Sejdic, E.; Perera, S.; Greenspan, S.L.; Sparto, P.J. Standing balance and strength measurements in older adults living in residential care communities. Aging Clin. Exp. Res. 2017, 29, 1021–1030. [Google Scholar] [CrossRef]
- Brodie, M.A.; Coppens, M.J.; Ejupi, A.; Gschwind, Y.J.; Annegarn, J.; Schoene, D.; Wieching, R.; Lord, S.R.; Delbaere, K. Comparison between clinical gait and daily-life gait assessments of fall risk in older people. Geriatr. Gerontol. Int. 2017, 17, 2274–2282. [Google Scholar] [CrossRef]
- Greene, B.R.; Redmond, S.J.; Caulfield, B. Fall Risk Assessment through Automatic Combination of Clinical Fall Risk Factors and Body-Worn Sensor Data. IEEE J. Biomed. Health Inform. 2017, 21, 725–731. [Google Scholar] [CrossRef] [PubMed]
- Joseph, B.; Toosizadeh, N.; Orouji Jokar, T.; Heusser, M.R.; Mohler, J.; Najafi, B. Upper-Extremity Function Predicts Adverse Health Outcomes among Older Adults Hospitalized for Ground-Level Falls. Gerontology 2017, 63, 299–307. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saldana, S.J.; Marsh, A.P.; Rejeski, W.J.; Haberl, J.K.; Wu, P.; Rosenthal, S.; Ip, E.H. Assessing balance through the use of a low-cost head-mounted display in older adults: A pilot study. Clin. Interv. Aging 2017, 12, 1363–1370. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sample, R.B.; Kinney, A.L.; Jackson, K.; Diestelkamp, W.; Bigelow, K.E. Identification of key outcome measures when using the instrumented timed up and go and/or posturography for fall screening. Gait Posture 2017, 57, 168–171. [Google Scholar] [CrossRef]
- Smith, E.; Walsh, L.; Doyle, J.; Greene, B.; Blake, C. Effect of a dual task on quantitative Timed Up and Go performance in community-dwelling older adults: A preliminary study. Geriatr. Gerontol. Int. 2017, 17, 1176–1182. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Delbaere, K.; Brodie, M.A.D.; Lovell, N.H.; Kark, L.; Lord, S.R.; Redmond, S.J. Differences Between Gait on Stairs and Flat Surfaces in Relation to Fall Risk and Future Falls. IEEE J. Biomed. Health Inform. 2017, 21, 1479–1486. [Google Scholar] [CrossRef] [PubMed]
- Bizovska, L.; Svoboda, Z.; Janura, M.; Bisi, M.C.; Vuillerme, N. Local dynamic stability during gait for predicting falls in elderly people: A one-year prospective study. PLoS ONE 2018, 13, e0197091. [Google Scholar] [CrossRef] [Green Version]
- Ehsani, H.; Mohler, J.; Marlinski, V.; Rashedi, E.; Toosizadeh, N. The influence of mechanical vibration on local and central balance control. J. Biomech. 2018, 71, 59–66. [Google Scholar] [CrossRef]
- Genovese, V.; Mannini, A.; Guaitolini, M.; Sabatini, A.M. Wearable Inertial Sensing for ICT Management of Fall Detection, Fall Prevention, and Assessment in Elderly. Technologies 2018, 6, 91. [Google Scholar] [CrossRef] [Green Version]
- Ghahramani, M.; Naghdy, F.; Stirling, D.; Naghdy, G.; Potter, J.; Roach, M. Assessing the Risk of Fall in Older People through Turning Test. In Proceedings of the 2018 IEEE International Symposium on Medical Measurements and Applications (MeMeA), Rome, Italy, 11–13 June 2018; pp. 1–6. [Google Scholar] [CrossRef]
- Qiu, H.; Rehman, R.Z.U.; Yu, X.; Xiong, S. Application of Wearable Inertial Sensors and A New Test Battery for Distinguishing Retrospective Fallers from Non-fallers among Community-dwelling Older People. Sci. Rep. 2018, 8, 16349. [Google Scholar] [CrossRef]
- Del Din, S.; Galna, B.; Godfrey, A.; Bekkers, E.M.J.; Pelosin, E.; Nieuwhof, F.; Mirelman, A.; Hausdorff, J.M.; Rochester, L. Analysis of Free-Living Gait in Older Adults With and Without Parkinson’s Disease and With and Without a History of Falls: Identifying Generic and Disease-Specific Characteristics. J. Gerontol. A Biol. Sci. Med. Sci. 2019, 74, 500–506. [Google Scholar] [CrossRef] [PubMed]
- Ghahramani, M.; Stirling, D.; Naghdy, F.; Naghdy, G.; Potter, J. Body postural sway analysis in older people with different fall histories. Med. Biol. Eng. Comput. 2019, 57, 533–542. [Google Scholar] [CrossRef]
- Greene, B.R.; McManus, K.; Redmond, S.J.; Caulfield, B.; Quinn, C.C. Digital assessment of falls risk, frailty, and mobility impairment using wearable sensors. NPJ Digit. Med. 2019, 2, 125. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Misu, S.; Asai, T.; Doi, T.; Sawa, R.; Ueda, Y.; Murata, S.; Saito, T.; Sugimoto, T.; Isa, T.; Tsuboi, Y.; et al. Development and validation of Comprehensive Gait Assessment using InerTial Sensor score (C-GAITS score) derived from acceleration and angular velocity data at heel and lower trunk among community-dwelling older adults. J. Neuroeng. Rehabil. 2019, 16, 62. [Google Scholar] [CrossRef] [Green Version]
- Yang, Y.; Hirdes, J.P.; Dubin, J.A.; Lee, J. Fall Risk Classification in Community-Dwelling Older Adults Using a Smart Wrist-Worn Device and the Resident Assessment Instrument-Home Care: Prospective Observational Study. JMIR Aging 2019, 2, e12153. [Google Scholar] [CrossRef] [Green Version]
- Ihlen, E.A.; Goihl, T.; Wik, P.B.; Sletvold, O.; Helbostad, J.; Vereijken, B. Phase-dependent changes in local dynamic stability of human gait. J. Biomech. 2012, 45, 2208–2214. [Google Scholar] [CrossRef]
- Kantz, H. A robust method to estimate the maximal Lyapunov exponent of a time series. Phys. Lett. A 1994, 185, 77–87. [Google Scholar] [CrossRef]
- Rosenstein, M.T.; Collins, J.J.; De Luca, C.J. A practical method for calculating largest Lyapunov exponents from small data sets. Phys. D Nonlinear Phenom. 1993, 65, 117–134. [Google Scholar] [CrossRef]
- Cummings, S.R.; Nevitt, M.C.; Kidd, S. Forgetting falls. The limited accuracy of recall of falls in the elderly. J. Am. Geriatr. Soc. 1988, 36, 613–616. [Google Scholar] [CrossRef]
- Concato, J.; Feinstein, A.R.; Holford, T.R. The risk of determining risk with multivariable models. Ann. Intern. Med. 1993, 118, 201–210. [Google Scholar] [CrossRef]
- King, G.; Zeng, L. Logistic Regression in Rare Events Data. Political Anal. 2001, 9, 137–163. [Google Scholar] [CrossRef] [Green Version]
- Isaksson, A.; Wallman, M.; Göransson, H.; Gustafsson, M.G. Cross-validation and bootstrapping are unreliable in small sample classification. Pattern Recognit. Lett. 2008, 29, 1960–1965. [Google Scholar] [CrossRef] [Green Version]





| Objective/Aim | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| To make a systematic review of the performance of wearable sensor systems in discriminating/classifying older adults according to their fall risk. The following PICO elements [18] were used: Population of interest: Persons being 60 years and older without severe cognitive impairment. Investigated test result: Person classified as faller according to SFRA Comparator test result: Person classified as non-faller according to SFRA Outcome: Person classified as faller (or equivalent, e.g., high risk) according to Retrospective falls history (RE), Prospective fall occurrence (PRO) or Clinical assessment methods (CLIN) Study design: Prospective and Cross-Sectional studies | 1. Original, peer-reviewed journal articles/conference papers published and indexed during Jan 2010–April 2020 in English language. 2. Participants labelled as (single/multiple-) fallers/non-fallers or high/low risk based on:
4. Wearable or mobile inertial sensors used to characterize movements by extracting features from sensor signals. 5. Evidence of SFRAs in terms of (a) discriminative capacity (statistically significant discriminatory features) and/or (b) classification performance (accuracy, sensitivity, specificity). Inclusion criteria 2–4 were based on a previous systematic review of SFRA [14]. | Papers must not include participants with severe cognitive impairment, e.g., dementia. Papers must not only include measurements of total physical activity by activity monitors. |
| Outcomes | ||
| (a) Qualitative data on features with statistically significant discriminative capacity (p < 0.05). (b) Quantitative data on classification performance (accuracy, sensitivity, specificity). |
| Database | Search Phrase | Search Date | Number of Articles |
|---|---|---|---|
| Web of Science Core Collection | TOPIC: (fall AND risk AND assessment) AND TOPIC:(inertial sensors) AND TOPIC:(geriatric OR older OR senior) AND TOPIC: (clinical) | 20 September 2019 | 31 |
| IEEE Xplore | TOPIC: (fall AND risk AND assessment) AND TOPIC:(inertial sensors) AND TOPIC:(geriatric OR older OR senior) AND TOPIC: (clinical) | 30 October 2019 | 21 |
| Web of Science Core Collection | TOPIC: ((fall AND risk AND assessment) AND (inertial sensors OR wearable OR technology OR device OR accelerometer OR gyroscope OR magnetometer) AND (geriatric OR older OR senior OR old) AND (clinical)) | 6 March 2020 | 129 |
| IEEE Xplore | TOPIC: fall AND risk AND assessment AND clinical AND (“inertial sensors” OR wearable OR technology OR device OR accelerometer OR gyroscope OR magnetometer) AND (geriatric OR older OR old OR senior) Filters Applied: Conferences Journals | 12 March 2020 | 32 |
| Pubmed | ((((fall[All Fields] AND (“risk”[MeSH Terms] OR “risk”[All Fields])) AND (“Assessment”[Journal] OR “assessment”[All Fields])) AND clinical[All Fields]) AND (geriatric[All Fields] OR older[All Fields] OR old[All Fields] OR senior[All Fields])) AND (“inertial sensors”[All Fields] OR wearable[All Fields] OR (“technology”[MeSH Terms] OR “technology”[All Fields]) OR (“equipment and supplies”[MeSH Terms] OR (“equipment”[All Fields] AND “supplies”[All Fields]) OR “equipment and supplies”[All Fields] OR “device”[All Fields]) OR accelerometer[All Fields] OR gyroscope[All Fields] OR magnetometer[All Fields]) | 27 March 2020 | 120 |
| Medline | fall AND risk AND assessment AND clinical AND (“inertial sensors” OR wearable OR technology OR device OR accelerometer OR gyroscope OR magnetometer) AND (geriatric OR older OR old OR senior) Expanders Limiters: Apply equivalent subjects Journals: Scholarly (Peer Reviewed) Journals Source Types: Academic Journals Language: English | 3 April 2020 | 281 |
| First Author, Year | Ref No. | Study Population | Faller/Non-Faller Labelling Method | Classification Outcome | Participants (% Fallers) | Assessment Task | Degree of Supervision |
|---|---|---|---|---|---|---|---|
| Bautmans, 2011 | [19] | Other | Retrospective falls (6 months) and Clinical assessment (Tinetti, TUG) | non-faller/faller | 81 (49%) | Walking (2 × 18 m) | SUP |
| Caby, 2011 | [20] | Hospitalized patients | Retrospective falls (12 months) and Clinical assessment (Tinetti, Mini Motor Test) | non-faller not at risk/faller at risk of falling | 20 (75%) | Walking (25m) | SUP |
| Doheny, 2011 | [21] | Community-dwelling | Retrospective falls (60 months) and Clinical assessment (FoF and Cardiovascular risk factors) | non-faller/faller (≥2 falls/1 fall seeking medical care) | 39 (49%) | FTSS | SUP |
| Greene, 2011 | [22] | Community-dwelling | Retrospective falls (60 months) | non-faller/faller | 114 (47%) | Walking (30 m continuous) | SUP |
| Marschollek, 2011 | [23] | Patients, geriatric | Prospective falls (12 months) | non-faller/faller | 46 (41%) | TUG test Walking (20 m) | SUP |
| Doi, 2013 | [24] | Community-dwelling | Prospective falls (12 months) | non-faller/faller | 73 (22%) | Walking (15 m) | SUP |
| Cui, 2014 | [25] | Community-dwelling | Retrospective falls (12 months) | non-faller/faller (≥2 falls) | 81 (49%) | Walking (3 conditions) | SUP |
| Ejupi, 2014 | [26] | Community-dwelling | Retrospective falls (12 months) | non-faller/faller | 104 (35%) | Choice Stepping Reaction Test | SUP |
| Greene, 2014 | [27] | Community-dwelling | Retrospective falls (60 months) and Prospective falls (24 months) | non-faller/faller | RE: 909 (NA) PRO: 259 (NA) Val: 55 (0%) | TUG test | SUP |
| Brodie, 2015 | [28] | Community-dwelling | Prospective falls (12 months) | non-faller/faller/multi-faller | 52 (42% single, 17% multi) | Stair ascent | SEMI-SUP at research facility |
| Howcroft, 2016 | [29] | Other | Retrospective falls (6 months) | non-faller/faller | 100 (24%) | Walking (7.62 m, single- and dual-task condition) | SUP |
| Ihlen, 2016 | [30] | Community-dwelling | Retrospective falls (12 months) | non-faller/faller | 71 (45%) | 4 FTSS at home for 1 day | SUP at home |
| Ihlen, 2016 | [31] | Community-dwelling | Retrospective falls (12 months) | non-faller/faller | 71 (45%) | Walking (daily life) | UNSUP 3 days at home |
| Iluz, 2016 | [32] | Other | Retrospective falls (12 months) | non-faller/faller | 71 (46%) | ADL (identified sit-to-walk and walk-to-sit transitions) | UNSUP 3 days at home |
| Mancini, 2016 | [33] | Other | Retrospective falls (12 months) and Prospective falls (6 months) | non-faller/faller/multiple-faller (RE) non-faller (PRO) | 35 (RE: 34% single, 20% multi; PRO: 20%) | ADL | UNSUP 1 week at home |
| Alqahtani, 2017 | [34] | In residential care | Retrospective falls (12 months) | non-faller/faller | 29 (66%) | Standing balance test | SUP |
| Brodie, 2017 | [35] | Community-dwelling | Retrospective falls (12 months) | non-faller/faller | 96 (34%) | ADL | UNSUP, 1 week at home |
| Greene, 2017 | [36] | Community-dwelling | Retrospective falls (12 months) | non-faller/faller | 22 (50%) | TUG test | SUP |
| Joseph, 2017 | [37] | Patients, bedbound in hospital | Clinical assessment (UEF index) | frail/non-frail | 101 (52%) | UEF assessment | SUP |
| Saldana, 2017 | [38] | In continuing-care retirement community | Clinical assessment (Questions including retrospective falls and FoF) | low-risk/at-risk | 13 (38%) | Standing balance with VR room rotation | SUP |
| Sample, 2017 | [39] | Other | Retrospective falls (12 months) | non-faller/faller | 148 (40%) | TUG test | SUP |
| Smith, 2017 | [40] | Community-dwelling | Retrospective falls (12 months) | non-faller/faller | 37 (43%) | TUG test (single-, motor- and cognitive dual task) | SUP |
| Wang, 2017 | [41] | Community-dwelling | Prospective falls (12 months) | multiple-faller/non-multiple-faller | 81 (14%) | Walking (flat surface and stairs) | SEMI-SUP at research facility |
| Bizovska, 2018 | [42] | Other | Prospective falls (12 months) | non-faller/faller/multiple-faller | 131 (27%, multi 11%) | Walking (25 m) | SUP |
| Ehsani, 2018 | [43] | Other | Clinical assessment (Questions including retrospective falls, 12 months) | high fall-risk/low fall-risk | 20 (50%) | Upright standing balance (eyes open/closed, with/without vibration) | SUP |
| Genovese, 2018 | [44] | Patients | Determined by clinical partners | high fall-risk/ age matched low fall-risk | 50 (50%) | 6MWT | SUP |
| Ghahramani, 2018 | [45] | Community-dwelling | Retrospective falls (time period not presented) | non-faller/multiple-faller | 45 (49% multi) | Turning test | SUP |
| Qiu, 2018 | [46] | Community-dwelling females | Retrospective falls (60 months) | non-faller/faller | 196 (42%) | Battery of clinical tests including assessment of standing balance, stability, sit-stand-transitions, walking, motor function, reaction and FoF | SUP |
| Del Din, 2019 | [47] | Other | Retrospective falls (6 months and 18 months (0 falls to identify non-faller)) | non-faller/faller | 172 (71%) | Free living gait | UNSUP, 1 week at home |
| Ghahramani, 2019 | [48] | Community-dwelling | Retrospective falls (12 months) | non-faller/faller/multiple-faller | 86 (21% single, 44% multi) | Standing balance tests | SUP |
| Greene, 2019 | [49] | Stratified sample | Retrospective falls (12 months) | non-faller/faller | 6295 (14% single, 12% multi) | TUG test | SUP |
| Misu, 2019 | [50] | Community-dwelling | Retrospective falls (12 months) | RE-12 non-faller/faller | 378 (17%) | Walking (15 m) | SUP |
| Yang, 2019 | [51] | Community-dwelling | Retrospective falls (3 months) | non-faller/faller/multiple-faller | 40 (20% single, 40% multi) | ADL | UNSUP, 1 week at home |
| Ref No. | Assessment Task | No. and Type of Wearable Sensor(s) | Sensor Position(s) | No. of Sensor Features | Feature Selection Methods | Wearable Sensor Features Able to Discriminate Significantly between Fallers/Non-Fallers |
|---|---|---|---|---|---|---|
| [19] | 2 × 18 m walking | 1 3D accel | Pelvis (sacrum between the spinae ilaca posterior superior) | 6 | ANOVA and t-test, Wilcoxon-signed-rank, Kruskall–Wallis tests, stepwise logistic regression with forward likelihood ratio and ROC curve | Gait speed |
| [21] | FTSS | 2 inertial sensors (3D accel data used) | Anterior of right thigh, sternum | 19 | ANOVA and one-way ANOVA | Mean sit-stand-time, total jerk, total SEF, Mean sit-stand-sit SEF, Mean-stand-sit SEF, Mean sit-stand SEF |
| [24] | 15 m walking | 2 3D accel | Upper trunk (C7 spinous process) and lower trunk (L3 spinous process) | 6 | Independent t-tests or χ2 tests, stepwise logistic regression with forward stepwise selection and ROC curve | HR in VT direction in Upper trunk |
| [25] | Walking under 3 different conditions | 1 inertial sensor (3D accel data used) | Lower back (belt) | 1 1 | Wilcoxon Signed Rank and Mann Whitney test | SSI |
| [26] | Choice stepping Reaction Test (in exergame) | 1 3D accel | Around neck (sternum height) inside clothes | 6 | Two-sided Student’s t-test | Reaction time, Total stability time |
| [30] | 4 FTSS at home for 1 day | 1 inertial sensor (3D accel data used) | Lower back (belt around waist) | 1 2 | Univariate logistic regression and stepwise multivariate logistic regression with stepwise backward feature selection | LDS calculated by the Ihlen algorithm (Equation (2)) [52] with optimal identified parameter setting |
| [31] | Daily life walking | 1 inertial sensor (3D accel data used) | Lower back (belt) | 60 | PLS-DA with a backward feature selection | RCME and RMPE for trunk acceleration and trunk velocity |
| [33] | ADL | 3 inertial sensors (3D gyro data used) | Posterior trunk at about L5 (belt) and on the top of each foot (on shoes) | 6 | One-way ANOVA | RE-12: turn duration, mean peak speed of turning, mean number of steps/turns, Coefficient of Variation of turn angle; PRO-6: Coefficient of Variation of steps per turn |
| [34] | Standing balance test | 1 2D accel and 1D load cell | Pelvis (Iliac crest) | 16 | Friedman test, Wilcoxon signed ranks test, Spearman rank correlation and Mann-Whitney U test | RMS sway acceleration in ML direction during semi-tandem stance |
| [35] | ADL | 1 3D accel + barometer | Pending around neck | 7 | ANOVA, ANCOVA, Pearson’s correlation and Partial Pearson’s correction | Gait endurance and within walk variability in daily life |
| [37] | UEF assessment | 2 3D gyro | Upper arm (near the biceps and to wrist) | 8 | ANOVA, Logistic regression (for nominal health outcomes) and ANOVA regression (for continuous health outcomes) | UEF index including speed, power and speed reduction |
| [38] | Standing balance with VR room rotation | 1 VRHMD (6D inertial sensor + camera) and a force plate | Head | 10 under each condition | One-sample t-test, signed rank test, paired t-test and Pearson’s correlation | VRHMD AP velocity while eyes open in VR module “balance” |
| [39] | TUG test | 4 inertial sensor (3D accel and 3D gyro) and a force plate | Chest, lower back, each foot | 8 (plus 9 post-urography parameters) | Stepwise logistic regression and Pearson correlation | Combination of Sit-to-Stand Duration, Stand-to-Sit Duration, Turn Peak Velocity, AP Sway Range, Height |
| [40] | TUG test under single- motor- and cognitive dual task | 2 inertial sensors (3D accel and 3D gyro) | Anterior of shank (shin) | 10 | MANCOVA and ANCOVA | Cadence, stride velocity, stride time |
| [41] | Walking on flat surface and stairs | 2 inertial sensors (3D accel data used) | Lower back and right ankle | 15 | Two-sample t-test, Fisher’s exact test, Mann-Whitney-U test, Wilcoxon’s signed-rank test, Benjamini-Hochberg adjustments, and logistic regression | Stair descent rate |
| [42] | 25 m walking | 3 3D accel | Trunk (near L5) and on both shanks (15 cm above malleolus) | 6 (plus 3 Tinetti scores) | Mann-Whitney U test, logistic regression, and ROC curve | Only combined with Tinetti balance- and Tinetti total score ML trunk short term Lyapunov exponent was able to predict falls |
| [43] | Upright standing balance (eyes open/closed, with/without vibration | 2 3D gyro | Lower back and shin | 8 | ANOVA, Friedman test, linear Pearson correlations | Local-controlslope, for eye-closed when vibration stimuli were applied |
| [44] | 6MWT | 1 3D accel, 3D gyro, 3D magneto- and barometer | Lower trunk (L3 spinous process) | 8 | t-test | Walked distance, cadence, RMS of vertical acceleration, stride time |
| [45] | Turning test | 4 inertial sensors (3D gyro used) | Chest, pelvis, and upper legs | 1 3 | ANOVA, DTW algorithm | BST |
| [47] | Free living gait | 1 3D accel | Lower back | 21 | Shapiro–Wilk test, Levene’s Test of Equality of Variances, general linear modelling, and Tukey’s test | Step velocity variability |
| [48] | Standing balance test | 1 inertial sensor (3D gyro data used) | Lower back (above pelvis) | 4 | GMM, EM, and MML algorithm, ANOVA and ROC-curve | Standing with feet together sway index, standing with one foot in front sway index |
| [50] | 15 m walking | 2 inertial sensors (3D accel and 3D gyro) | Right heel (posterior surface) and trunk (L3 spinous process) | 10 | Unpaired t-tests/χ2 tests, unweighted least squares as extraction method and Cronbach’s alpha coefficient | C-GAITS score |
| Ref No. | Assessment Task | No. and Type of Wearable Sensor(S) | Sensor Position(s) | No. of Sensor Features | Feature Selection Methods | Models Able to Discriminate Significantly between Fallers/Non-Fallers |
|---|---|---|---|---|---|---|
| [22] | 30 m continuous walk | 2 inertial sensors (3D accel and 3D gyro) | Mid-point of anterior shank | 10 | Mann–Whitney Wilcoxon rank sum and Pearson’s correlation | MGC estimation by regression models (MGC model and MGC variance model) using the features mean SagAngVel at mid-swing points, mean absolute valued SagAngVel and min SagAngVel |
| [23] | TUG test and 20 m walk | 1 3D accel | Lower back (belt around waist) | 14 | Wrapper feature selection algorithm (wrapper subset evaluator employing the simple logistic algorithm) | Logistic regression models CONV (using conventional clinical assessment data) and SENSOR (using sensor data from TUG and overall physical activity) |
| [27] | TUG test | 2 inertial sensors (3D accel and 3D gyro) | Anterior of each shin, shank bone (tibial bone) | 52 | Sequential forward feature selection | Regularized discriminant classifier models using 52 temporal, spatial, turning, and rotational features from TUG |
| [36] | TUG test | 2 inertial sensors (3D accel and 3D gyro) | Mid-point of left and right anterior shank (shin) | 44 | Nested CV | Classification model FREcombined which combines FREsensor (regularized discriminant model using QTUG parameters during standing walking and turning) and FREclin (logistic regression model using clinical data on fall risk factors |
| [49] | TUG test | 2 inertial sensors (3D accel and 3D gyro) | Mid-point of left and right anterior shank (shin) | 71 | One-way ANOVA | FREcombined (i.e, the weighted average of the two FRE models FREsensor (regularized discriminant model using IMU-data from TUG + anthropomorphic data) and FREclinical (logistic regression model using clinical questionnaire data) Each mobility score (speed, turn, transfers, symmetry, variability) in mobility impairment score was significantly associated with falls history |
| Ref No. | Assessment Task | No. and Type of Wearable Sensor(s) | Sensor Position(s) | No. of Sensor Features | Feature Selection Methods | Methods/Models Able to Discriminate Significantly between Fallers/Non-Fallers |
|---|---|---|---|---|---|---|
| [20] | 25 m walking | 10 3D accel | Mid-point of anterior shank | 10 | t-test using Holm correction, Behrens-Fisher test, forward wrapper selection algorithm family | RBNC, SVM, KNN, NB |
| [28] | Stair ascent | 1 3D accel + 1 barometer | Lower back (belt around waist) | 14 | Spearman’s rank correlations, Kruskal–Wallis | Wavelet DT with adaptive threshold |
| [29] | Walking 7.62m under single and dual tasks | 4 3D accel + 2 pressure sensing insoles | Anterior of each shin, shank bone (tibial bone) | 146 | Acc, F1-score, MCC | SVM, NN, NB |
| [32] | Identified sit-to-walk and walk-to-sit transitions in ADL | 1 inertial sensor (3D accel data used) | Low back (belt) | 72 | 4 machine learning algorithms in Matlab), linear regression analysis | Ada Boost, SVM, bag, NB |
| [46] | Battery of 5 clinical tests including assessment of standing balance, stability, sit-stand-transitions, walking, motor function, reaction, and FoF | 5 inertial sensors (3D accel, 3D gyro and 3D magnetometer) | Low back, upper and lower legs | 155 | Two-sample t-tests, ROC analysis | Logistic regression, NB, DT, RF, BT, SVM |
| [51] | ADL | 1 3D accel + 1 photoelectric heart rate sensor | Wrist | 38 1 | One-way and two-way ANOVA, Kruskal–Wallis H test, multicollinear test, recursive feature algorithm in Caret R package | Three-class classification: POM and two machine learning algorithms (DT and RF) Binary classification: Three machine learning algorithms (logistic regression, DT, RF) |
| Ref No. | No. of Fallers/No. of Participants (Faller/Non-Faller Labelling Method) | Sensor Features’ Performance in Discriminating Groups with Different Level of Fall Risk (Fallers/Non-Fallers) | No. of Features and Type of Assessment Task Able to Discriminate Groups with Different Level of Fall Risk (Fallers/Non-Fallers) |
|---|---|---|---|
| [21] | 19/39 (RE-60, CLIN) | Fallers took significantly longer time to complete sit-stand transitions than non-fallers; Fallers exhibited increased jerk over the complete assessment than non-fallers; SEF was significantly higher for fallers than non-fallers for the total test, sit-stand-sit components, sit-stand and stand-sit transitions | 6, sit-stand and stand-sit transitions |
| [25] | 39/81 (RE-12) | The SSI was significantly higher for fallers than non-fallers under all three walking conditions (baseline with and without harness, obstacle negotiation with harness) | 3, gait |
| [26] | 36/104 (RE-12) | Significantly longer times to regain balance after movement initiation and slower stability time for fallers than for non-fallers. | 2, stability/balance |
| [33] | 19/35 (RE-12) 7/35 (PRO-6) | RE-12: Mean turn duration, mean peek speed of turning and mean number of steps/turn and the coefficient of variance of the turn angle were significantly different between multiple-fallers and non-fallers. Multiple-fallers had a longer turn duration, slower mean peak speed of turning, a higher number of steps/turn, and showed a lower coefficient of variance of turn angle than non-fallers. Multiple-fallers took a significantly higher number of steps/turn and showed a lower coefficient of variance of turn angle than fallers. PRO-6: 7/35 fell during the 6-month period. The coefficient of variance of steps per turn was significantly larger for fallers and multiple-fallers than for non-fallers. | RE-12: 4, turning and gait PRO-6: 1, gait |
| [34] | 19/29 (RE-12) | RMS sway acceleration for ML direction during semi-tandem stance was significantly higher among fallers than non-fallers. | 1, stability/balance |
| [35] | 33/96 (RE-12) | After adjusting for demographics, fallers had significantly lower gait endurance and higher within walk variability in daily life than non-fallers. | 2, gait |
| [37] | 53/101 (UEF I) | The UEF index (adjusted for age, gender, BMI, age, discharge disposition) was a predictor for 30-day prospective falls. The UEF index, which assesses frailty, was higher in the frail group than in the non-frail group. | 1, upper extremity |
| [38] | 5/13 (CLIN incl. RE) | People at-risk of falling changed their head tilt in the AP direction significantly faster than people not at risk. Only reliable variables (identified from test-retest reliability evaluations) were included in the analysis. | 1, stability/balance |
| [40] | 16/37 (RE-12) | Fallers had a significantly higher cadence, higher stride velocity and shorter stride time than non-fallers. | 3, gait |
| [41] | 11/81 (PRO-12) | Stair descent rate was significantly higher among multiple-fallers than non-multiple-fallers | 1, stair negotiation |
| [43] | 10/20 (CLIN incl. RE) | When vibration was induced in the eyes-closed condition, the people with a high fall risk changed the local-controlslope significantly less than people with a low fall risk | 1, stability/balance |
| [44] | 25/50 (determined by clinical partners) | People with a high fall-risk had a significantly shorter walked distance, lower cadence, lower RMS (vertical acceleration) and higher stride time than people with a low fall-risk. | 4, gait |
| [45] | 22/45 (RE) | The DTW difference between the reference BST and each participant’s BST was significantly higher among elderly multiple fallers than non-fallers. | 1, balance/stability |
| [47] | 122/172 (RE-18/RE-6) | Step velocity variability was significantly lower among older adult fallers than older adult non-fallers. | 1, gait |
| [50] | 65/378 (RE-18) | Statistically significant lower C-GAITS score among fallers than non-fallers. | 1, gait: |
| Ref No. | No. of Fallers/No. of Participants (Faller/Non-Faller Labelling Method) | Classification Models/Algorithms Included in Discrimination Method | Model Validation Method | Methods’/Models’ Performance in Discriminating Groups with Different Level of Fall Risk (Fallers/Non-Fallers) | No. of Features and Type of Assessment Task Able to Discriminate Groups with Different Level of Fall Risk (Fallers/Non-Fallers) |
|---|---|---|---|---|---|
| [22] | 54/114 (RE-60) | 2 regression algorithms of minimum ground clearance | NA | Fallers had a significantly lower mean SagAngVel at mid-swing points, mean SagAngVel absolute value and min SagAngVel than non-fallers. | 3, gait |
| [28] | 31/52 (PRO-12) | Machine learning algorithms (wavelet DT with adaptive threshold) using barometer and Accel features for classifying stair negotiation | Annotated video and 4-fold CV (x4 times) | PRO significantly correlated with reduced stair ascent stability (HR-AP, r = −0.35). | 1, stair negotiation |
| [49] | 1637/6295 (RE-12) | Regularized discriminant model (sensor data), logistic regression model (clinical data) | Validation of models previously reported | FREcombined significantly associated with RE (F = 214.19, ρ < 0.0001). Each mobility score (speed, turn, transfers, symmetry, variability) in mobility impairment score was significantly associated with falls history. | NA |
| Ref No. | No. of Fallers/No. of Participants (Faller/Non-Faller Labelling Method) | Sensor Features’ Performance in Discriminating Groups with Different Level of Fall Risk (Fallers/Non-Fallers) | Comment |
|---|---|---|---|
| [19] | 40/81 (RE-6, CLIN) | Gait speed (cut-off 1.158 m/s): Acc = 77%; Sens = 78%; Spec = 78%; AUC = 0.83 | |
| [24] | 16/71 (PRO-12) | UT HR-VT: AUC = 0.81 (95% CI: 0.69–0.83; p < 0.001). Sens = 68.8% and Spec = 84.2% at cutoff value 1.89 based on the Youden index. | 95% CI for AUC presented (as suggested in previous reviews) |
| [30] | 32/71 (RE-12) | Kantz’ algorithm [53] with the best performing parameter: AUC = 0.73 (95% CI:0.60–0.85; p = 0.003) Ihlen’s algorithm [52] with the best performing parameter: AUC = 0.75 (CI:0.60–0.82; p > 0.001) Rosenstein’s algorithm [54] with the best performing parameter: AUC = 0.59 (CI:0.44–0.71; non-significant) | 95% CI for AUC of as well as pairwise comparison of AUC of models presented (as suggested in previous reviews) |
| [31] | 32/71 (RE-12) | Mean (Equation (1)) RCME for trunk acceleration: Sens = 0.84; Spec = 0.85; AUC = 0.81; Err = 0.15 Mean (Equation 1) RCME for trunk velocity: Sens = 0.78; Spec = 0.90; AUC = 0.83; Err = 0.15 Mean (Equation (1)) RPME for trunk acceleration: Sens = 0.88; Spec = 0.90; AUC = 0.88; Err = 0.11 Mean (Equation (1)) RPME for trunk velocity: Sens = 0.75; Spec = 0.87; AUC = 0.82; Err = 0.18 | |
| [39] | 59/148 (RE-12) | Height, sit-to-stand duration, stand-to-sit duration, turn peak velocity, AP sway range: Sens = 54.3%, Spec = 82.7%; max re-scaled R2 = 0.3244 | |
| [42] | 50/131 (PRO-12) | Combination of Tinetti balance score, Tinetti total score and ML trunk short term Lyapunov exponent: AUC = 0.760, Sens = 0.80, Spec = 0.7 ML trunk short term Lyapunov exponent alone is found insufficient for distinguishing groups. ML trunk short term Lyapunov exponent comparing non-fallers and multiple-fallers. AUC = 0.673; Sens: 0.53; Spec: 0.85 | Performance metrics for Tinetti scores presented as suggested in previous reviews. |
| [48] | 56/86 (RE-12) | Standing with feet together sway index: Sens = 78.6%; Spec = 75.7%; AUC = 0.84 (95% CI: 0.75–0.92) Standing with one foot in front sway index: Sens = 82.1%; Spec = 77.7%; AUC = 0.90 (95% CI: 0.82–0.97) | 95% CIs for all AUCs presented. Performance metrics of CLIN BBS presented (both aspects suggested in previous reviews) |
| Ref No. | No. of Fallers/No. of Participants (Faller/Non-Faller Labelling Method) | Classification Models/Algorithms Included in Discrimination Method | Model Validation Method | Methods’/Models’ Performance in Discriminating Groups with Different Level of Fall Risk (Fallers/Non-Fallers) | Comment |
|---|---|---|---|---|---|
| [20] | 15/20 (RE-6, CLIN) | 4 machine learning algorithms: NB, RBNC, KNN, SVM | Leave-one-out CV | NB: Sens = 1; Spec = 1; Err = 0 for 4 combinations of selected features RBNC: Sens = 1; Spec = 0.8; Err = 0.05 for 1 selected feature KNN: Sens = 0.93; Spec = 0.8; Err = 0.05 for 1 selected feature combination SVC: Sens = 1; Spec = 0; Err = 0.25 for 1 selected feature combination | Small sample Very high-performance metrics (authors conclude that NB probably is over fitted) |
| [23] | 19/46 (PRO-12) | Logistic regression models (SENSOR, CONV) | Ten-fold CV (x10 times) | SENSOR: Acc = 70%; Sens = 58%; Spec = 78%; NPV = 72%; PPV = 65%; Brier score = 0.21; AUC = 0.72 CONV: Acc = 72%; Sens = 68%; Spec = 74%; NPV = 77%; PPV = 65%; Brier score = 0.20; AUC = 0.74 | Small sample Performance metrics of clinical assessment tools provided (as suggested in previous reviews) |
| [27] | Number of fallers not reported in RE-60 and PRO-24 data samples/RE-60: 909 PRO-24: 259 Val: 55 (non-fallers) | Regularized discriminant classifier algorithms (Cross-sectional, prospective) | Ten-fold CV (x10 times) and validation using independent data set with healthy control subjects | 1. Ten-fold CV (×10 times) Cross-sectional model (RE dataset): Acc = 70.02%; Sens = 47.73%; Spec = 84.72%; PPV = 70.14%; NPV = 69.19%; AUC = 0.67 Prospective model (PRO dataset): Acc = 76.27%; Sens = 57.20%; Spec = 83.63%; PPV = 59.86%; NPV = 82.54%; AUC = 0.69 2. Validation using independent datasets with healthy older adults Cross-sectional model (CS1 + CS2 non-faller): Acc = 94.11% PRO-model (CS1 + CS2 non-faller): Acc = 79.38% | Validation both by CV and by use of independent datasets (as suggested in previous reviews) Validation with independent dataset: Cross-sectional single task Acc > 81% |
| [29] | 24/100 (RE-6) | 3 machine learning algorithms: multi-layer perceptron NN, NB, SVM | Hold-out method (75% training set and 25% test set). Derived using either single task data or dual task data | Best fall risk classification model based on single task i.e., walk without cognitive load: 4 models with identical performance (SVM degree 2—using data from insoles-pelvis. SVM degree 3—using data from insoles-head-pelvis, NN 9 nodes—using data from insoles-pelvis, and NN 20—using data from insoles-head-pelvis-left shank): Acc = 84.0%; F1-score = 0.600; MCC = 0.521 Best fall risk classification model based on dual task (DT), i.e., walk with cognitive load: 1 SVM degree 1 model using data from insoles and pelvis: Acc = 80.0%; Sens = 100.0%; Spec = 73.7%; PPV = 54.5%; NPV = 100.0%; F1 = 0.706; MCC = 0.634 Comparison of 10 best ST models and 10 best DT models, all but one ST model outperformed the DT models. | Hold-out method used for model validation (preferred over CV in [9].) Single task data models: Best Acc > 81% |
| [32] | 33/71 (RE-12, at least 2 falls) | 4 machine learning algorithms (Ada Boost, SVM, bag, NB) | Stratified two-fold CV (×20 times) | Machine learning algorithms using features from Daily-Living Transitions: AdaBoost (mean number of (no) features = 18.25): Acc = 87.90%; Sens = 88.84%; Spec = 87.22% SVM (mean no features = 25.50): Acc = 90.64%; Sens = 89.23%; Spec = 91.66% Bag (mean no features = 10.25): Acc = 87.09%; Sens = 83.84%; Spec = 89.44% NB (mean no features = 19.10): Acc = 87.74%; Sens = 78.46%; Spec = 94.44% Machine learning algorithms using features from Daily-Living Transitions and functional laboratory tests: Ada Boost (mean no features = 13.55): Acc = 90.16%; Sens = 87.50%; Spec = 91.94% SVM (mean no features = 22.60): Acc = 91.00%; Sens = 88.75%; Spec = 92.50% Bag (mean no features = 16.05): Acc = 87.16%; Sens = 85.41%; Spec = 88.33% NB (mean no features = 15.65): Acc = 90.66%; Sens = 83.33%; Spec = 95.50% Machine learning algorithms using features from functional laboratory tests: AdaBoost (mean no features = 2.60): Acc = 70.00%; Sens = 56.66%; Spec = 78.88% SVM (mean no features = 1.70): Acc = 70.66%; Sens = 42.90%; Spec = 89.16% Bag (mean no features = 2.60): Acc = 72.50%; Sens = 68.75%; Spec = 75.00% NB (mean no features = 2.05): Acc = 70.66%; Sens = 44.16%; Spec = 88.33% | Authors find that features extracted from daily life can distinguish better between fallers and non-fallers than features from functional laboratory tests. The discrimination was only slightly improved by combining the features. Acc for model using data from Daily Living transitions > 81% |
| [36] | 11/22 (RE-12) | FREsensor—regularized discriminant model (sensor data) FREclin—logistic regression model (clinical data) FREcombined—classifier combined theory | Classification performance: Leave-one out CV FREsensor features and model selection: Ten-fold CV (×10 times) Validation of FREsensor using independent dataset | Classification performance using leave-one-out CV: FREcombined: Acc = 68.48%; Sens = 68.36%; Spec = 68.57%; PPV = 61.11%; NPV = 75.00% FREsensor: Acc = 66.82%; Sens = 74.01%; Spec = 61.63%; PPV = 58.22%; NPV = 76.65% FREclin:: Acc = 58.53%; Sens = 35.93%; Spec = 78.90%; PPV = 54.55%; NPV = 63.61% Validation of FREsensor using independent dataset with community-dwelling older adults with 95% CI in []: Acc = 72.70 [54.12–91.34] %; Sens = 90.91 [78.90–100.0] %; Spec = 54.50 [33.69–75.31] %; PPV = 66.67 [46.97–86.37] %; NPV = 85.71 [71.09–100.0] % | Independent validation of clinical, sensor and combined FRE classifier models: FREsensor model validated on independent dataset and 95% CIs for performance metrics provided (as recommended in previous reviews) |
| [46] | 82/196 (RE-60) | 6 Machine learning algorithms: SVM, BT, RF, DT, NB, logistic regression | Ten-fold CV (×10 times) Two sample t-test for comparing overall classification Acc. | SVM: Acc = 89.42 ± 4.82%; Sens = 92.67 ± 6.17%; Spec = 84.90 ± 8.68% BT: Acc = 87.09 ± 5.56%; Sens = 91.23 ± 6.71%; Spec = 81.37 ± 9.37% RF: Acc = 86.39 ± 5.41%; Sens = 92.23 ± 5.49%; Spec = 78.06 ± 10.63% DT: Acc = 81.64 ± 6.09%; Sens = 87.25 ± 7.56%; Spec = 73.29 ± 10.62% NB: Acc = 80.05 ± 6.11%; Sens = 87.91 ± 6.60%; Spec = 69.16 ± 11.80%) Logistic regression: Acc = 79.70 ± 6.37%; Sens = 87.24 ± 6.75%; Spec = 69.23 ± 11.94% | 95% CIs provided for each performance metrics (as recommended in previous reviews). Two sample t-tests on overall classification Acc showed that a significantly higher Acc was achieved using SVM. Best Acc > 81% |
| [51] | 24/40 (RE-3, non/once/multi) | Three-class classification model using features from wearables and/or RAI-HC: POM, and the machine learning algorithms DT and RF Binary classification model using features from wearables and/or RAI-HC: logistic regression, DT and RF | Leave-one-out CV | 1. Three class classification (non-fallers, fallers, multiple-fallers): (a) best performance RF: Acc = 0.838 ± 0.199; Recall = 0.775 ± 0.233; Precision = 0.730 ± 0.259; F1 = 0.748 ± 0.248 (b) DT: Acc = 0.757 ± 0.221; Recall = 0.703 ± 0.254; Precision = 0.643 ± 0.275; F1 = 0.662 ± 0.266 (c) worst performance POM: Acc = 0.676 ± 0.170; Recall = 0.626 ± 0.195; Precision = 0.593 ± 0.195; F1 = 0.584 ± 0.191 2. Binary classification (non-fallers + fallers vs. multiple-fallers): (a) best performance RF: AUC = 0.894 ± 0.155; Acc = 0.892 ± 0.160; Recall = 0.908 ± 0.135; Precision = 0.928 ± 0.106; F1 = 0.888 ± 0.166 (b) DT: AUC = 0.858 ± 0.160, Acc = 0.838 ± 0.200; Recall = 0.869 ± 0.154; Precision = 0.851 ± 0.226; F1 = 0.829 ± 0.218 (c) worst performance logistic regression: AUC = 0.838 ± 0.234; Acc = 0.703 ± 0.172; Recall = 0.676 ± 0.200; Precision = 0.657 ± 0.281; F1 = 0.626 ± 0.231 3. Binary classification (non-fallers vs. fallers + multiple-fallers): (a) best performance RF: AUC = 0.865 ± 0.125; Acc = 0.865 ± 0.132; Recall = 0.865 ± 0.125; Precision = 0.908 ± 0.094; F1 = 0.853 ± 0.139 (b) DT: AUC = 0.842 ± 0.229, Acc = 0.865 ± 0.192; Recall = 0.851 ± 0.213; Precision = 0.886 ± 0.202; F1 = 0.849 ± 0.214 (c) worst performance logistic regression: AUC = 0.743 ± 0.251; Acc = 0.784 ± 0.224; Recall = 0.766 ± 0.232; Precision = 0.778 ± 0.255; F1 = 0.755 ± 0.246 | 95% CI provided for each performance metrics (as recommended in previous reviews). Pruning used in training of DT models to avoid overfitting. Acc > 81% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kristoffersson, A.; Du, J.; Ehn, M. Performance and Characteristics of Wearable Sensor Systems Discriminating and Classifying Older Adults According to Fall Risk: A Systematic Review. Sensors 2021, 21, 5863. https://doi.org/10.3390/s21175863
Kristoffersson A, Du J, Ehn M. Performance and Characteristics of Wearable Sensor Systems Discriminating and Classifying Older Adults According to Fall Risk: A Systematic Review. Sensors. 2021; 21(17):5863. https://doi.org/10.3390/s21175863
Chicago/Turabian StyleKristoffersson, Annica, Jiaying Du, and Maria Ehn. 2021. "Performance and Characteristics of Wearable Sensor Systems Discriminating and Classifying Older Adults According to Fall Risk: A Systematic Review" Sensors 21, no. 17: 5863. https://doi.org/10.3390/s21175863
APA StyleKristoffersson, A., Du, J., & Ehn, M. (2021). Performance and Characteristics of Wearable Sensor Systems Discriminating and Classifying Older Adults According to Fall Risk: A Systematic Review. Sensors, 21(17), 5863. https://doi.org/10.3390/s21175863








