Artificial Intelligence-Enabled ECG Algorithm Based on Improved Residual Network for Wearable ECG
Abstract
:1. Introduction
2. Materials and Methods
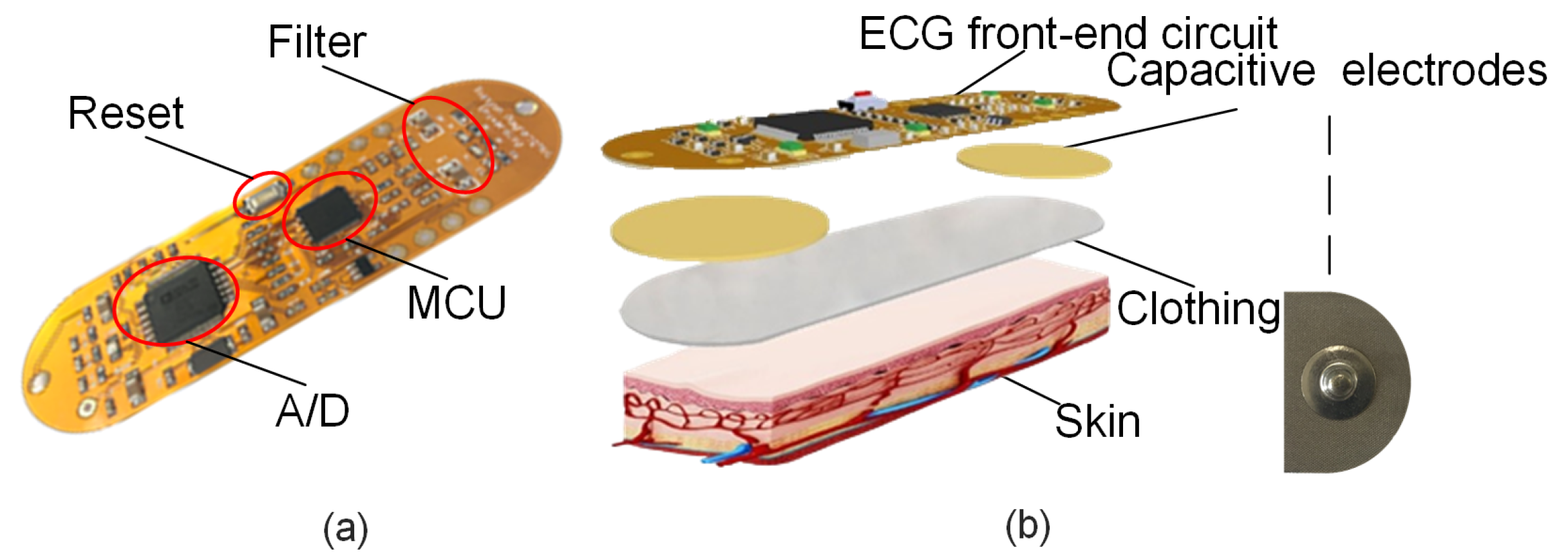
2.1. ECG Acquisition Module
2.1.1. Conductive Fabric Electrodes
2.1.2. ECG Acquisition Circuit
2.2. ECG Classification Algorithm
2.2.1. Deep ResNet and Its Improvement
2.2.2. SELU Activation Function
2.2.3. Source of Dataset and Evaluation Index
2.2.4. Comparative Network Experiment
2.2.5. Confusion Matrix and Indicators
2.3. Mobile Terminal App
- User information management;
- ECG signal receiving and display;
- Historical measurement information recording;
- ECG science knowledge display functions.
2.3.1. User Registration and Login
2.3.2. Reception and Display of ECG Signals
2.3.3. Record of Historical Measurement Information
2.3.4. Popularization of ECG Knowledge
2.4. Implementation of Cloud Diagnostic Platform
2.4.1. Python Internet Modules
2.4.2. Python/MatLab Mixed Programming
2.5. Experimental Tests
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ECG | Electrocardiogram |
| ResNet | Residual network |
| SELU | Scaled exponential linear units |
| IoT | Internet of Things |
| LSTM | Long and short-term memory |
| CNN | Convolution neural network |
| ADC | Analog-to-digital conversion |
| BLE | Bluetooth Low Energy |
| GAFs | Gramian angular fields |
| 2D | Two-dimensional |
| BN | Batch normalization |
| LTAF | Long-term AF |
| GASF | Gramian Summation Angular Field |
| PAC | Premature atrial contraction |
| PVC | Premature ventricular contraction |
| N | Normal |
| AF | Atrial fibrillation |
| VT | Ventricular tachycardia |
| SBR | Sinus bradycardia |
| AT | Atrial tachycardia |
| Ppr | Precision rate |
| Sen | Sensitivity |
| Spe | Specificity |
| Acc | Accuracy |
| MLP | Multi-layer perception |
References
- Hamine, S.; Gerth-Guyette, E.; Faulx, D.; Green, B.B.; Ginsburg, A.S. Impact of mHealth chronic disease management on treatment adherence and patient outcomes: A systematic review. J. Med. Internet Res. 2015, 17, e52. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sacks, F.M.; Lichtenstein, A.H.; Wu, J.; Appel, L.J.; Creager, M.A.; Kris-Etherton, P.; Miller, M.; Rimm, E.B.; Rudel, L.L.; Robinson, J.G.; et al. Dietary fats and cardiovascular disease: A presidential advisory from the American Heart Association. Circulation 2017, 136, e1–e23. [Google Scholar] [CrossRef] [PubMed]
- Walker, A.L.; Muhlestein, J.B. Smartphone electrocardiogram monitoring: Current perspectives. Adv. Health Care Technol. 2018, 4, 15–24. [Google Scholar] [CrossRef] [Green Version]
- Liu, C.; Zhang, X.; Zhao, L.; Liu, F.; Chen, X.; Yao, Y.; Li, J. Signal quality assessment and lightweight QRS detection for wearable ECG SmartVest system. IEEE Internet Things 2018, 6, 1363–1374. [Google Scholar] [CrossRef]
- Oh, S.L.; Ng, E.Y.; Tan, R.S.; Acharya, U.R. Automated diagnosis of arrhythmia using combination of CNN and LSTM techniques with variable length heart beats. Comput. Biol. Med. 2018, 102, 278–287. [Google Scholar] [CrossRef] [PubMed]
- Krianyaz, S.; Ince, T.; Gabbouj, M. Real-Time Patient-Specific ECG Classification by 1-D Convolutional Neural Networks. IEEE Trans. Biomed. Eng. 2016, 63, 664–675. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.G.; Oates, T. Encoding Time Series as Images for Visual Inspection and Classification Using Tiled Convolutional Neural Networks. IEEE Trans. Biomed. Eng. 2015, 7, 40–46. [Google Scholar] [CrossRef]
- He, K.; Zhang, X.; Ren, S.; Sun, J. Deep Residual Learning for Image Recognition. In Proceedings of the Conference on Computer Vision and Pattern Recognition, Las Vegas, NV, USA, 27–30 June 2016. [Google Scholar]
- Zhang, K.; Sun, M.; Han, T.X.; Yuan, X.; Guo, L.; Liu, T. Residual Networks of Residual Networks: Multilevel Residual Networks. IEEE Trans. Circuits Syst. Video Technol. 2018, 28, 1303–1314. [Google Scholar] [CrossRef] [Green Version]
- He, K.; Zhang, X.; Ren, S.; Sun, J. Identity Mappings in Deep Residual Network. In Proceedings of the European Conference on Computer Vision, Amsterdam, The Netherlands, 11–14 October 2016. [Google Scholar]
- Klambauer, G.; Unterthiner, T.; Mayr, A.; Hochreiter, S. Self-Normalizing Neural Networks. J. Korean Soc. Precis. Eng. 2017, 1706, 02515. [Google Scholar]
- Amirshahi, A.; Hashemi, M. ECG Classification Algorithm Based on STDP and R-STDP Neural Networks for Real-Time Monitoring on Ultra Low-Power Personal Wearable Devices. IEEE Trans. Biomed. Circuits Syst. 2019, 13, 1483–1493. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hu, Y.H.; Palreddy, S.; Tompkins, W.J. A patient-adaptable ECG beat classifier using a mixture of experts approach. IEEE Trans. Biomed. Eng. 1997, 44, 891–900. [Google Scholar] [CrossRef] [PubMed]
- Ince, T.; Krianyaz, S.; Gabboui, M. A Generic and Robust System for Automated Patient-Specific Classification of ECG Signals. IEEE Trans. Biomed. Eng. 2009, 56, 1415–1426. [Google Scholar] [CrossRef] [PubMed]
- Feng, K.; Pi, X.; Liu, H.; Sun, K. Myocardial Infarction Classification Based on Convolutional Neural Network and Recurrent Neural Network. Appl. Sci. 2019, 9, 1879. [Google Scholar] [CrossRef] [Green Version]
- Shirin, H.M.; Mohsen, A.; Reza, S.; Chon, K.H. Automated Method for Discrimination of Arrhythmias Using Time, Frequency, and Nonlinear Features of Electrocardiogram Signals. Sensors 2018, 18, 2090. [Google Scholar] [CrossRef] [Green Version]
- Bashar, S.K.; Han, D.; Zieneddin, F.; Ding, E.; Fitzgibbons, T.P.; Walkey, A.J.; McManus, D.D.; Javidi, B.; Chon, K.H. Novel Density Poincare Plot Based Machine Learning Method to Detect Atrial Fibrillation from Premature Atrial/Ventricular Contractions. IEEE Trans. Biomed. Eng. 2020, 68, 448–460. [Google Scholar] [CrossRef] [PubMed]
- Dash, S.; Chon, K.H.; Lu, S.; Raeder, E.A. Automatic Real Time Detection of Atrial Fibrillation. Ann. Biomed. Eng. 2009, 3, 1701–1709. [Google Scholar] [CrossRef] [PubMed]













| Types | Samples | Training Set | Testing Set |
|---|---|---|---|
| AF | 1841 | 1472 | 369 |
| AT | 500 | 400 | 100 |
| N | 4800 | 3840 | 960 |
| PAC | 328 | 262 | 66 |
| PVC | 2106 | 1684 | 422 |
| SBR | 1855 | 1484 | 371 |
| VT | 294 | 235 | 59 |
| Total | 11,724 | 9377 | 2347 |
| Network | Accuracy |
|---|---|
| Resnet50-ReLu | 95.4% |
| Improved Resnet50-ReLu | 97.5% |
| Improved Resnet50-SELU | 98.3% |
| Real Category | Categories of Prediction | |||||||
|---|---|---|---|---|---|---|---|---|
| AF | AT | N | PAC | PVC | SBR | VT | Total | |
| AF | 357 | 0 | 4 | 1 | 3 | 2 | 2 | 369 |
| AT | 0 | 100 | 0 | 0 | 0 | 0 | 0 | 100 |
| N | 3 | 0 | 950 | 3 | 4 | 0 | 0 | 960 |
| PAC | 1 | 0 | 1 | 62 | 0 | 2 | 0 | 66 |
| PVC | 1 | 0 | 3 | 1 | 415 | 2 | 0 | 422 |
| SBR | 4 | 0 | 0 | 0 | 0 | 366 | 1 | 371 |
| VT | 2 | 1 | 1 | 0 | 0 | 0 | 55 | 59 |
| Total | 368 | 101 | 959 | 67 | 422 | 372 | 58 | 2347 |
| Categories | Ppr | Sen | Spe | F1 Score |
|---|---|---|---|---|
| AF | 96.7% | 97.0% | 99.3% | 96.8% |
| AT | 99.0% | 100.0% | 100.0% | 99.5% |
| N | 99.1% | 98.6% | 99.5% | 98.8% |
| PAC | 95.4% | 95.4% | 99.9% | 95.4% |
| PVC | 98.6% | 98.6% | 99.6% | 98.6% |
| SBR | 98.7% | 98.9% | 99.7% | 98.8% |
| VT | 94.8% | 95.0% | 99.9% | 94.9% |
| Average | 98.1% | 97.6% | 99.7% | 97.6% |
| Patient ID | Age | Height | Weight | Past Medical History | Test Results |
|---|---|---|---|---|---|
| a | 68 | 170 cm | 90 kg | AF | N, AF |
| b | 45 | 170 cm | 85 kg | Incidental PAC | N |
| c | 40 | 168 cm | 70 kg | PAC | N, PAC |
| d | 43 | 167 cm | 85 kg | PVC, AF | N, AF |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, H.; An, Z.; Zuo, S.; Zhu, W.; Zhang, Z.; Zhang, S.; Zhang, C.; Song, W.; Mao, Q.; Mu, Y.; et al. Artificial Intelligence-Enabled ECG Algorithm Based on Improved Residual Network for Wearable ECG. Sensors 2021, 21, 6043. https://doi.org/10.3390/s21186043
Li H, An Z, Zuo S, Zhu W, Zhang Z, Zhang S, Zhang C, Song W, Mao Q, Mu Y, et al. Artificial Intelligence-Enabled ECG Algorithm Based on Improved Residual Network for Wearable ECG. Sensors. 2021; 21(18):6043. https://doi.org/10.3390/s21186043
Chicago/Turabian StyleLi, Hongqiang, Zhixuan An, Shasha Zuo, Wei Zhu, Zhen Zhang, Shanshan Zhang, Cheng Zhang, Wenchao Song, Quanhua Mao, Yuxin Mu, and et al. 2021. "Artificial Intelligence-Enabled ECG Algorithm Based on Improved Residual Network for Wearable ECG" Sensors 21, no. 18: 6043. https://doi.org/10.3390/s21186043
APA StyleLi, H., An, Z., Zuo, S., Zhu, W., Zhang, Z., Zhang, S., Zhang, C., Song, W., Mao, Q., Mu, Y., Li, E., & García, J. D. P. (2021). Artificial Intelligence-Enabled ECG Algorithm Based on Improved Residual Network for Wearable ECG. Sensors, 21(18), 6043. https://doi.org/10.3390/s21186043









