Gait Parameters in Healthy Preschool and School Children Assessed Using Wireless Inertial Sensor
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Protocol of Gait Analysis
- Pelvic obliquity: upward (positive) or downward (negative) movement of the pelvis in the frontal (F) plane;
- Pelvic tilt: anterior or posterior movement of the pelvis in the sagittal (S) plane;
- Pelvic rotation: internal (positive) or external (negative) movement of the pelvis in the transversal (T) plane.
2.3. Statistical Analysis
3. Results
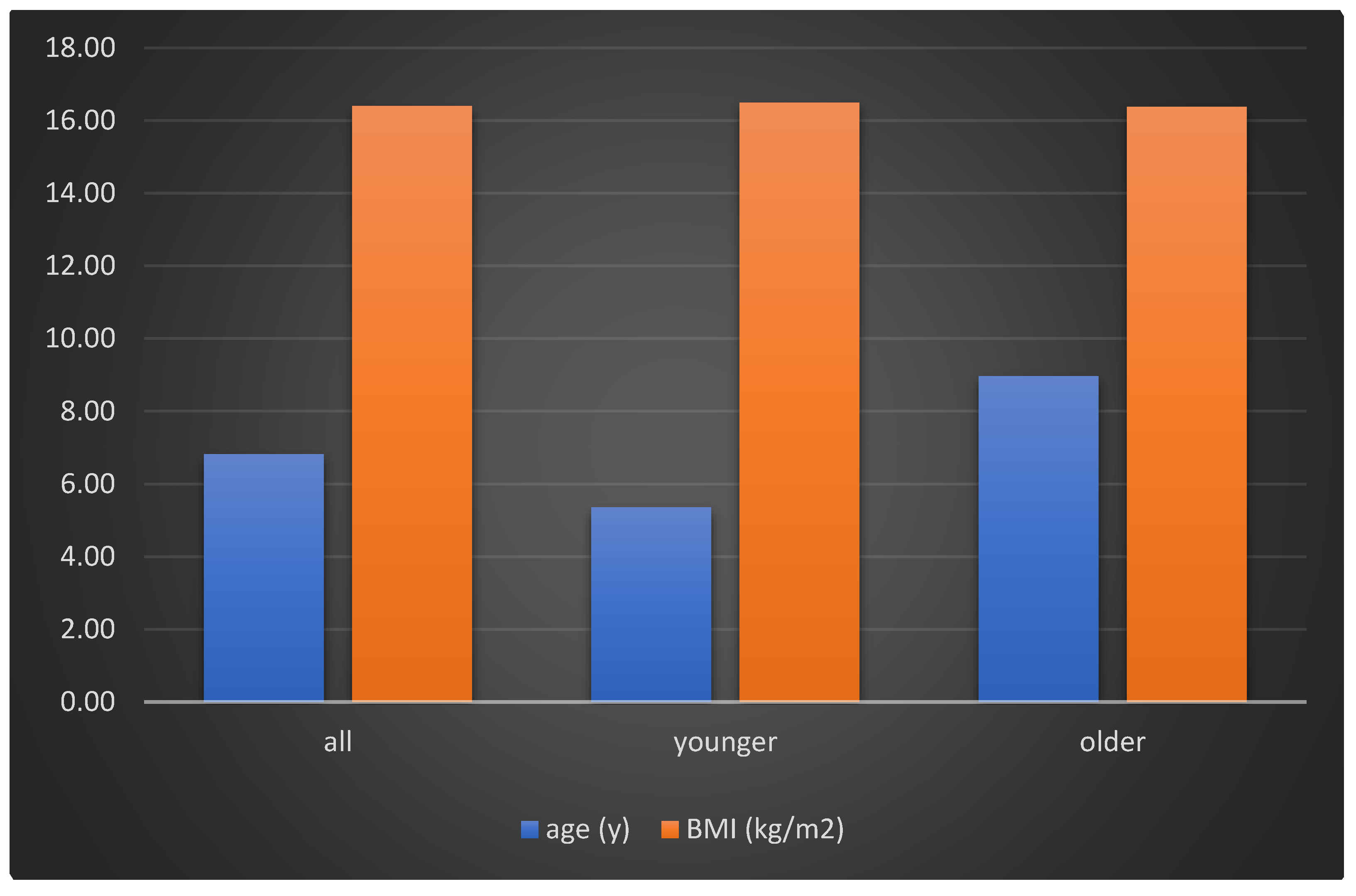
3.1. Participants’ Demographics
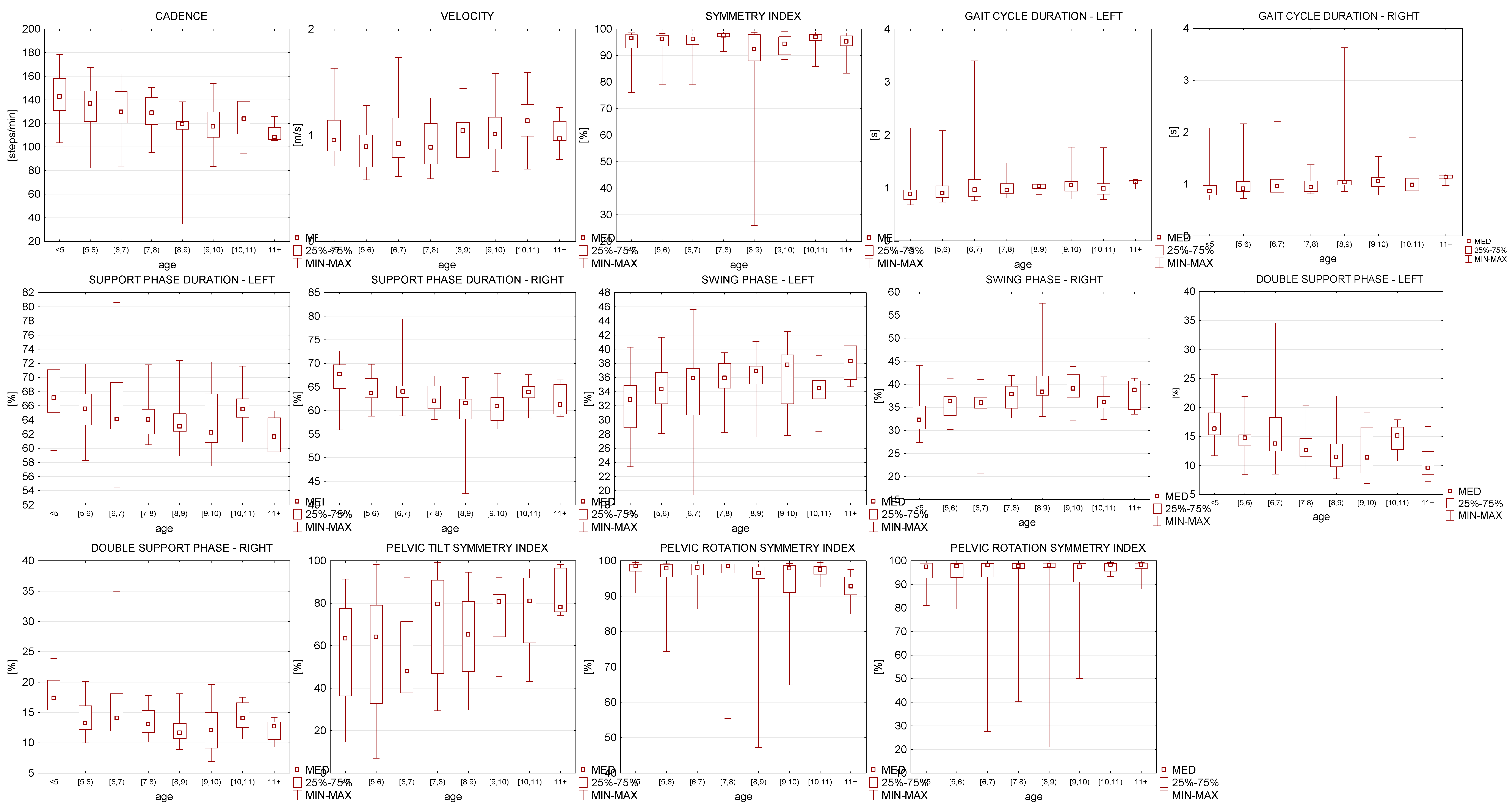
3.2. Spatiotemporal Gait Parameters
3.3. Correlation Coefficient Investigation
3.4. Gait Parameters Due to Annual Division
3.5. Gait Parameters Due to Preschool and School Groups
3.6. Differences between Left and Right Side in the Gait Parameters
3.7. Gait Parameters Divided into Two Groups Due to Sex
4. Discussion
Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Müller, J.; Müller, S.; Baur, H.; Mayer, F. Intra-individual gait speed variability in healthy children aged 1–15 years. Gait Posture 2013, 38, 631–636. [Google Scholar] [CrossRef] [PubMed]
- Bach, M.M.; Daffertshofer, A.; Dominici, N. The development of mature gait patterns in children during walking and running. Eur. J. Appl. Physiol. 2021, 121, 1073–1085. [Google Scholar] [CrossRef] [PubMed]
- Dusing, S.C.; Thorpe, D.E. A normative sample of temporal and spatial gait parameters in children using the GAITRite® electronic walkway. Gait Posture 2007, 25, 135–139. [Google Scholar] [CrossRef] [PubMed]
- Thorpe, D.E.; Dusing, S.C.; Moore, C.G. Repeatability of temporospatial gait measures in children using the GAITRite electronic walkway. Arch. Phys. Med. Rehabil. 2005, 86, 2342–2346. [Google Scholar] [CrossRef] [PubMed]
- Smith, Y.; Louw, Q.; Brink, Y. The three-dimensional kinematics and spatiotemporal parameters of gait in 6-10 year old typically developed children in the Cape Metropole of South Africa—A pilot study. BMC Pediatrics 2016, 16, 200. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kennedy, R.A.; Carroll, K.; McGinley, J.L.; Paterson, K.L. Walking and weakness in children: A narrative review of gait and functional ambulation in paediatric neuromuscular disease. J. Foot Ankle Res. 2020, 13, 10. [Google Scholar] [CrossRef] [Green Version]
- Wojciechowski, E.; Sman, A.; Cornett, K.; Raymond, J.; Refshauge, K.; Menezes, M.P.; Burns, J. Gait patterns of children and adolescents with Charcot-Marie-Tooth disease. Gait Posture 2017, 56, 89–94. [Google Scholar] [CrossRef]
- Rabuffetti, M.; Recalcati, M.; Ferrarin, M. Trans-femoral amputee gait: Socket-pelvis constraints and compensation strategies. Prosthet. Orthot. Int. 2005, 29, 183–192. [Google Scholar] [CrossRef]
- Carcreff, L.; Gerber, C.N.; Paraschiv-Ionescu, A.; De Coulon, G.; Newman, C.J.; Aminian, K.; Armand, S. Comparison of gait characteristics between clinical and daily life settings in children with cerebral palsy. Sci. Rep. 2020, 10, 2091. [Google Scholar] [CrossRef]
- Dziuba, A.K.; Tylkowska, M.; Jaroszczuk, S. Index of mechanical work in gait of children with cerebral palsy. Acta Bioeng. Biomech. 2014, 16, 77–87. [Google Scholar]
- Buderath, P.; Gärtner, K.; Frings, M.; Christiansen, H.; Schoch, B.; Konczak, J.; Gizewski, E.R.; Hebebrand, J.; Timmann, D. Postural and gait performance in children with attention deficit/hyperactivity disorder. Gait Posture 2009, 29, 249–254. [Google Scholar] [CrossRef]
- Gieysztor, E.; Pecuch, A.; Kowal, M.; Borowicz, W.; Paprocka-Borowicz, M. Pelvic symmetry is influenced by asymmetrical tonic neck reflex during young children’s gait. Int. J. Environ. Res. Public Health 2020, 17, 4759. [Google Scholar] [CrossRef]
- Smith, M.; Ward, E.; Williams, C.M.; Banwell, H.A. Differences in walking and running gait in children with and without developmental coordination disorder: A systematic review and meta-analysis. Gait Posture 2021, 83, 177–184. [Google Scholar] [CrossRef]
- Agostini, V.; Nascimbeni, A.; Di Nardo, F.; Fioretti, S.; Burattini, L.; Knaflitz, M. Dependence of gait parameters on height in typically developing children. In Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society, EMBS, Milan, Italy, 25–29 August 2015; pp. 7598–7601. [Google Scholar]
- Van Hamme, A.; El Habachi, A.; Samson, W.; Dumas, R.; Chèze, L.; Dohin, B. Gait parameters database for young children: The influences of age and walking speed. Clin. Biomech. 2015, 30, 572–577. [Google Scholar] [CrossRef] [Green Version]
- Del Din, S.; Godfrey, A.; Rochester, L. Validation of an Accelerometer to Quantify a Comprehensive Battery of Gait Characteristics in Healthy Older Adults and Parkinson’s Disease: Toward Clinical and at Home Use. IEEE J. Biomed. Heal. Inform. 2016, 20, 838–847. [Google Scholar] [CrossRef]
- Sankarpandi, S.K.; Baldwin, A.J.; Ray, J.; Mazzà, C. Reliability of inertial sensors in the assessment of patients with vestibular disorders: A feasibility study. BMC Ear, Nose Throat Disord. 2017, 17, 1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Voss, S.; Joyce, J.; Biskis, A.; Parulekar, M.; Armijo, N.; Zampieri, C.; Tracy, R.; Palmer, A.S.; Fefferman, M.; Ouyang, B.; et al. Normative database of spatiotemporal gait parameters using inertial sensors in typically developing children and young adults. Gait Posture 2020, 80, 206–213. [Google Scholar] [CrossRef]
- Schedler, S.; Abeck, E.; Muehlbauer, T. Relationships between types of balance performance in healthy individuals: Role of age. Gait Posture 2021, 84, 352–356. [Google Scholar] [CrossRef] [PubMed]
- Manicolo, O.; Grob, A.; Lemola, S.; Arx, P.H. von Age-related decline of gait variability in children with attention-deficit/hyperactivity disorder: Support for the maturational delay hypothesis in gait. Gait Posture 2016, 44, 245–249. [Google Scholar] [CrossRef] [PubMed]
- Papadopoulos, N.; McGinley, J.L.; Bradshaw, J.L.; Rinehart, N.J. An investigation of gait in children with Attention Deficit Hyperactivity Disorder: A case controlled study. Psychiatry Res. 2014, 218, 319–323. [Google Scholar] [CrossRef] [PubMed]
- Viteckova, S.; Kutilek, P.; Svoboda, Z.; Krupicka, R.; Kauler, J.; Szabo, Z. Gait symmetry measures: A review of current and prospective methods. Biomed. Signal Process. Control 2018, 42, 89–100. [Google Scholar] [CrossRef]
- Shin, S.Y.; Lee, R.K.; Spicer, P.; Sulzer, J. Does kinematic gait quality improve with functional gait recovery? A longitudinal pilot study on early post-stroke individuals. J. Biomech. 2020, 105, 109761. [Google Scholar] [CrossRef] [PubMed]
- Ismailidis, P.; Hegglin, L.; Egloff, C.; Pagenstert, G.; Kernen, R.; Eckardt, A.; Ilchmann, T.; Nüesch, C.; Mündermann, A. Side to side kinematic gait differences within patients and spatiotemporal and kinematic gait differences between patients with severe knee osteoarthritis and controls measured with inertial sensors. Gait Posture 2021, 84, 24–30. [Google Scholar] [CrossRef] [PubMed]
- Moreno-Hernández, A.; Rodríguez-Reyes, G.; Quiñones-Urióstegui, I.; Núñez-Carrera, L.; Pérez-SanPablo, A.I. Temporal and spatial gait parameters analysis in non-pathological Mexican children. Gait Posture 2010, 32, 78–81. [Google Scholar] [CrossRef]
- Lythgo, N.; Wilson, C.; Galea, M. Basic gait and symmetry measures for primary school-aged children and young adults whilst walking barefoot and with shoes. Gait Posture 2009, 30, 502–506. [Google Scholar] [CrossRef]
- Brady, K.; Kiernan, D. Centre of pressure error with increasing gait velocity: The clinical impact on predicted inverse dynamics during gait in children with typical development. Gait Posture 2020, 82, 96–99. [Google Scholar] [CrossRef]
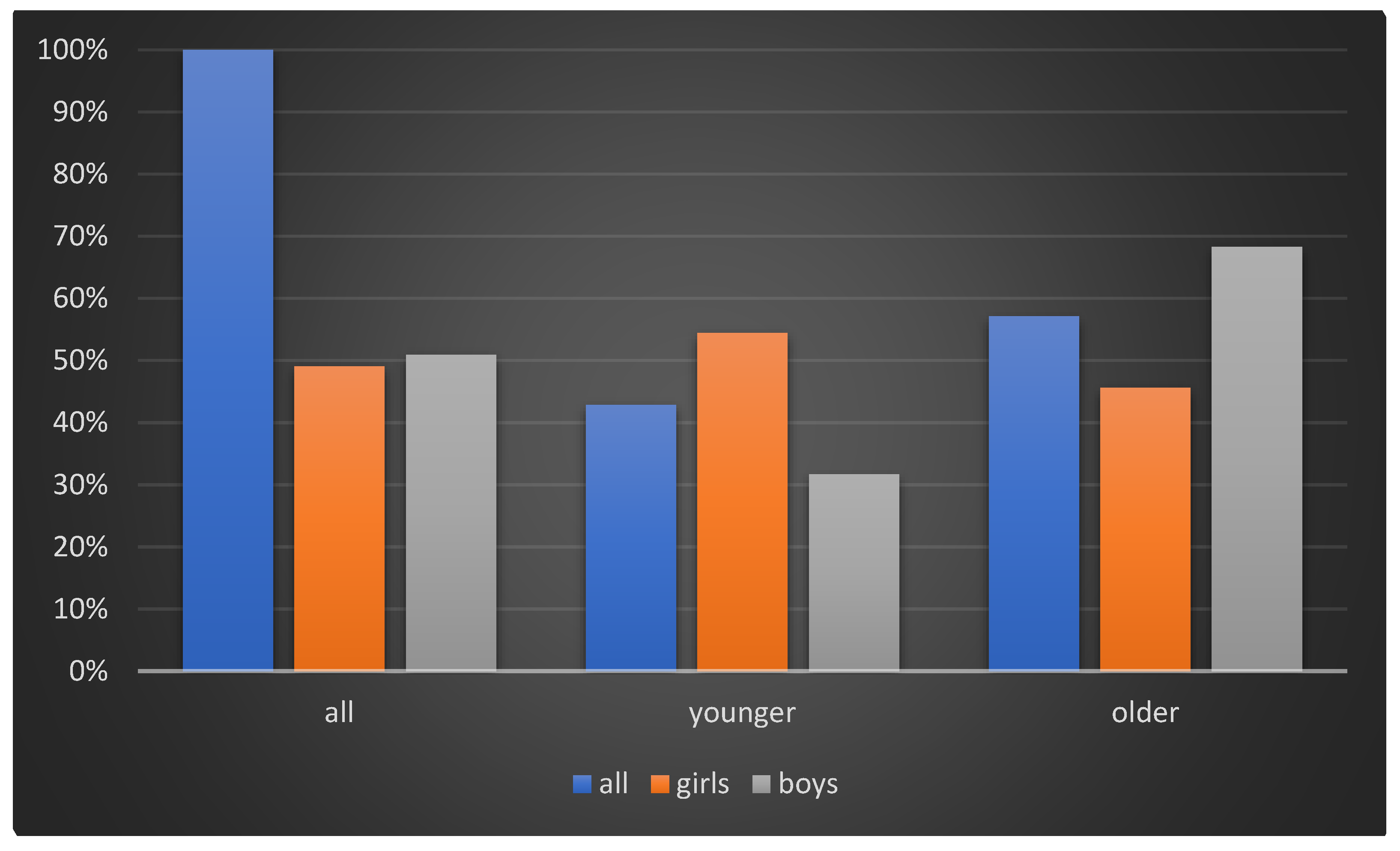
| All | P Group | S Group | |
|---|---|---|---|
| n | |||
| Female | 79 (49%) | 43 (61%) | 36 (40%) |
| Male | 82 (51%) | 27 (39%) | 55 (60%) |
| Total | 161 | 70 | 91 |
| Age (y) | |||
| Female | 7.16 (±2.15) | 4.93 (±0.76) | 8.29 (±1.56) |
| Male | 6.46 (±2.06) | 4.89 (±0.75) | 8.24 (±1.71) |
| Total | 6.82 (±2.13) | 4.91 (±0.75) | 8.26 (±1.64) |
| Weight (kg) | |||
| Female | 22.65 (±6.44) | 19.19 (±4.30) | 26.78 (±6.15) |
| Male | 25.98 (±7.94) | 20.26 (±3.71) | 28.68 (±7.99) |
| Total | 24.34 (±7.40) | 19.60 (±4.09) | 27.93 (±7.34) |
| Height (cm) | |||
| Female | 118.56 (±15.08) | 108.07 (±7.65) | 131.08 (±11.83) |
| Male | 123.00 (±13.40) | 110.19 (±5.89) | 129.05 (±11.55) |
| Total | 120.81 (±14.38) | 108.87 (±7.07) | 129.86 (±11.64) |
| BMI (kg/m2) | |||
| Female | 15.96 (±2.64) | 16.38 (±2.97) | 15.45 (±2.11) |
| Male | 16.88 (±2.75) | 16.69 (±2.78) | 16.98 (±2.72) |
| Total | 16.43 (±2.72) | 16.50 (±2.88) | 16.37 (±2.60) |
| P Group | S Group | p-Value | |
|---|---|---|---|
| mean age (y) | 5.35 (±0.97) | 8.95 (±1.4) | p < 0.001 |
| mean body height (m) | 1.12 (±0.8) | 1.34 (±0.11) | p < 0.001 |
| mean body weight (kg) | 21 (±4) | 30 (±8) | p < 0.001 |
| BMI (kg/m2) | 16.5 | 16.4 | p > 0.05 |
| All Children | Preschool | School | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Spatiotemporal Gait Parameters | |||||||||||
| Mean | SD | Median | Mean | SD | Median | Mean | SD | Median | p-Value | ||
| gait cycle duration (s) | left | 0.93 | 0.20 | 0.89 | 0.85 | 0.17 | 0.80 | 0.99 | 0.20 | 0.96 | 0.000 |
| right | 0.92 | 0.19 | 0.89 | 0.84 | 0.17 | 0.80 | 0.98 | 0.19 | 0.97 | 0.000 | |
| step length (%) | left | 75.79 | 17.43 | 73.10 | 75.81 | 21.51 | 72.70 | 75.77 | 13.51 | 73.70 | 0.987 |
| right | 75.50 | 17.18 | 73.90 | 75.63 | 21.65 | 73.30 | 75.39 | 12.76 | 74.10 | 0.931 | |
| support phase duration (%) | left | 65.54 | 4.27 | 65.10 | 67.13 | 4.26 | 66.30 | 64.33 | 3.86 | 63.50 | 0.000 |
| right | 64.03 | 3.91 | 63.55 | 65.94 | 4.06 | 66.10 | 62.59 | 3.09 | 62.50 | 0.000 | |
| support phase duration (%) | left | 65.54 | 4.27 | 65.10 | 67.13 | 4.26 | 66.30 | 64.33 | 3.86 | 63.50 | 0.000 |
| right | 64.03 | 3.91 | 63.55 | 65.94 | 4.06 | 66.10 | 62.59 | 3.09 | 62.50 | 0.000 | |
| swing phase (%) | left | 34.46 | 4.27 | 34.90 | 32.87 | 4.26 | 33.70 | 35.67 | 3.86 | 36.50 | 0.000 |
| right | 35.97 | 3.91 | 36.45 | 34.06 | 4.06 | 33.90 | 37.41 | 3.09 | 37.50 | 0.000 | |
| double support duration (%) | left | 14.59 | 4.02 | 14.35 | 16.23 | 3.42 | 15.50 | 13.35 | 4.00 | 12.70 | 0.000 |
| right | 14.62 | 3.83 | 14.10 | 16.27 | 4.17 | 16.10 | 13.37 | 2.99 | 12.90 | 0.000 | |
| single support duration (%) | left | 36.26 | 3.89 | 36.70 | 34.48 | 3.79 | 34.30 | 37.61 | 3.38 | 37.70 | 0.000 |
| right | 34.81 | 3.96 | 35.40 | 33.45 | 4.02 | 33.60 | 35.85 | 3.58 | 36.50 | 0.000 | |
| Gait symmetry index (%) | |||||||||||
| Mean | SD | Median | Mean | SD | Median | Mean | SD | Median | p-value | ||
| pelvic tilt (S) | 62.55 | 24.31 | 68.80 | 55.69 | 25.76 | 62.70 | 67.76 | 21.76 | 72.00 | 0.002 | |
| pelvic obliquity (F) | 96.00 | 5.83 | 98.00 | 96.83 | 4.24 | 98.50 | 95.37 | 6.72 | 97.50 | 0.117 | |
| pelvic rotation (T) | 94.68 | 9.94 | 97.95 | 94.53 | 9.51 | 97.70 | 94.79 | 10.24 | 98.10 | 0.868 | |
| Age | BMI | ||
|---|---|---|---|
| cadence (steps/min) | −0.43* | 0.17 | |
| velocity (m/s) | 0.12 | 0.09 | |
| gait cycle duration (s) | left | 0.10 | −0.04 |
| right | 0.12 | −0.06 | |
| step length (%) | left | −0.06 | 0.04 |
| right | −0.06 | 0.05 | |
| support phase duration (%) | left | −0.31* | 0.15 |
| right | −0.42* | 0.08 | |
| swing phase (%) | left | 0.31* | −0.15 |
| right | 0.42* | −0.08 | |
| double support duration (%) | left | −0.38* | 0.10 |
| right | −0.38* | 0.10 | |
| single support duration (%) | left | 0.44* | 0.00 |
| right | 0.32* | −0.13 | |
| pelvic tilt (S) | 0.32* | −0.03 | |
| pelvic obliquity (F) | −0.17 | −0.08 | |
| pelvic rotation (T) | −0.01 | −0.05 |
| Cadence (Steps/min) | Velocity (m/s) | Step Length (cm) | ||
|---|---|---|---|---|
| all children | mean | 130.99 | 0.99 | 94.91 |
| SD | 19.89 | 0.58 | 4.37 | |
| min | 82.10 | 0.58 | 76.10 | |
| max | 178.30 | 1.73 | 99.00 | |
| preschool | mean | 139.37 | 0.96 | 94.70 |
| SD | 20.55 | 0.24 | 4.76 | |
| min | 82.10 | 0.58 | 76.10 | |
| max | 178.30 | 1.63 | 98.70 | |
| school | mean | 124.64 | 1.01 | 95.07 |
| SD | 16.78 | 0.25 | 4.04 | |
| min | 83.60 | 0.59 | 79.00 | |
| max | 161.90 | 1.73 | 99.00 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gieysztor, E.; Kowal, M.; Paprocka-Borowicz, M. Gait Parameters in Healthy Preschool and School Children Assessed Using Wireless Inertial Sensor. Sensors 2021, 21, 6423. https://doi.org/10.3390/s21196423
Gieysztor E, Kowal M, Paprocka-Borowicz M. Gait Parameters in Healthy Preschool and School Children Assessed Using Wireless Inertial Sensor. Sensors. 2021; 21(19):6423. https://doi.org/10.3390/s21196423
Chicago/Turabian StyleGieysztor, Ewa, Mateusz Kowal, and Małgorzata Paprocka-Borowicz. 2021. "Gait Parameters in Healthy Preschool and School Children Assessed Using Wireless Inertial Sensor" Sensors 21, no. 19: 6423. https://doi.org/10.3390/s21196423
APA StyleGieysztor, E., Kowal, M., & Paprocka-Borowicz, M. (2021). Gait Parameters in Healthy Preschool and School Children Assessed Using Wireless Inertial Sensor. Sensors, 21(19), 6423. https://doi.org/10.3390/s21196423






