Mobile 5P-Medicine Approach for Cardiovascular Patients
Abstract
:1. Introduction
- Before the planning of the system, analysis of the state-of-the-art about the current applications which use mobile and wearable personal devices for promoting personalized digital health care must be performed.
- Identify the implementation challenges when applying the approach to real implementations.
- Analyze the required device features, because, for the use and implementation of the system, a minimum hardware and software requirements are needed.
- Analyze the required sensors because different sensors are needed for the data acquisition that will help the healthcare professionals in the monitoring of the cardiovascular patients.
- Increase the patients’ autonomy with the easy and seamless contact with healthcare providers and professionals.
2. State-of-the-Art
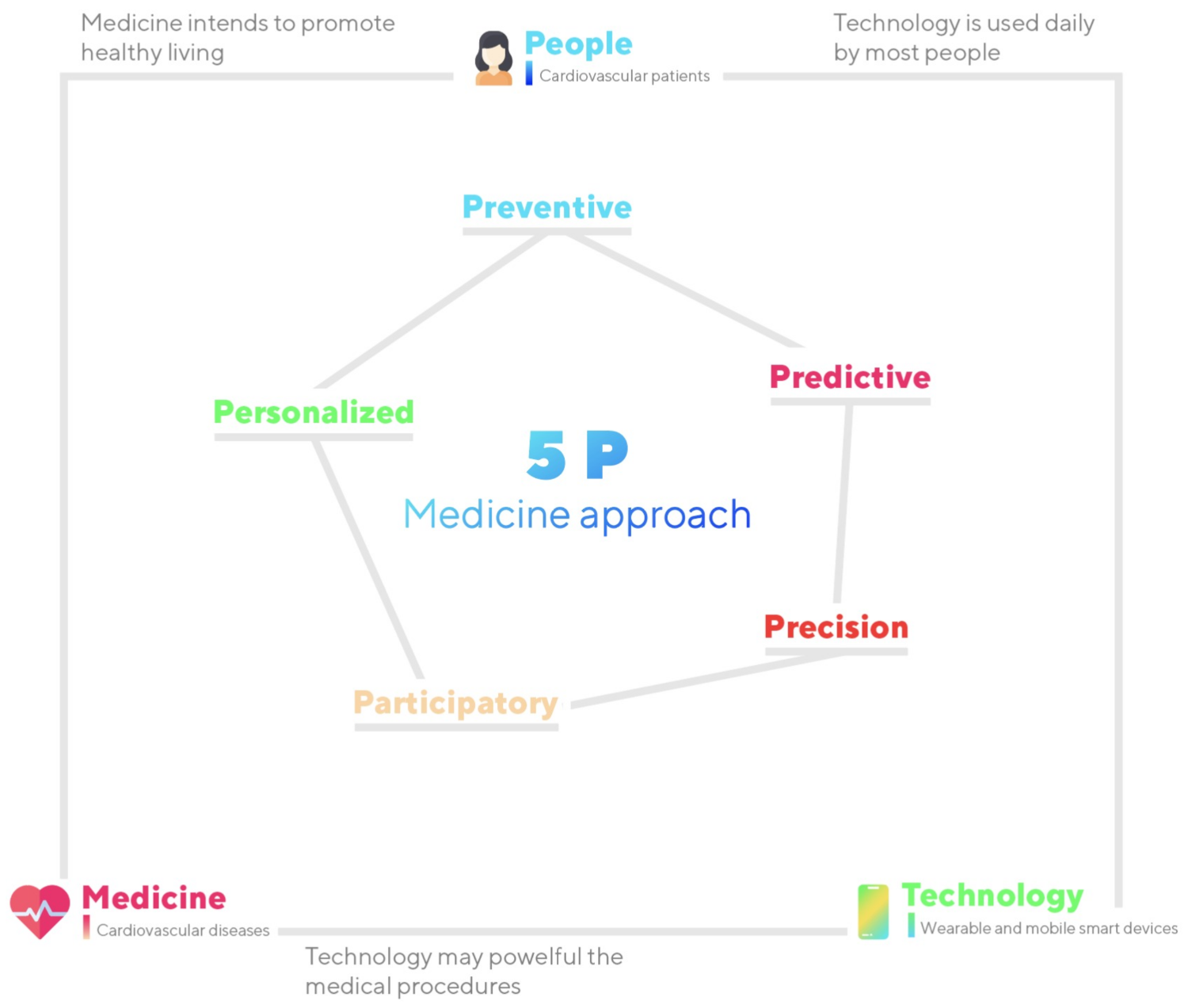
2.1. 5P-Medicine Concept
2.2. Patient Empowerment
2.3. Wearable and Smart Mobile Devices
2.4. Cardiovascular Diseases and Technology
2.5. Bio-Signals Acquisition and Processing
3. Methods and Expected Results
3.1. Research Background
3.2. Research Design
3.2.1. Data Acquisition
3.2.2. Data Analysis
3.2.3. Data Analysis in Developing Countries
3.2.4. Data Analysis in Developed Countries
3.2.5. Development and Integration of Final System
3.3. Methods for Patient Empowerment and System Analysis
3.4. Expected Results
4. Discussion
4.1. Multidisciplinary Approach Required
4.2. Experimental Challenges
4.3. Complexity and Specificity of System
- Data acquisition and processing: It must have low latency times to acquire and process data. The frequencies of data acquisition from the different sensors/equipment must be adjusted to obtain better results.
- Data processing: The time for data processing can sometimes be high, and the solution’s development time is affected. The nonexistence of rules for analyzing the data is another problem related to data processing, where the data should be tested with different processing methodologies.
- Data fusion: The acquired data have different natures, and the complexity of the data fusion and processing may be adapted to the different kinds of data. Various sensors retrieve distinct types of data.
- Amount of data: The proposed approach must be prepared to transmit and store a large amount of data related to different sensors.
- Interaction between sensors and patients: The patients must be taught and familiarized with the different sensors and mobile devices before using the system.
- Acquisition of health parameters: As the proposed approach is related to the acquisition of health parameters, the system must consider different rules for data protection and security during the data transmission and analysis.
- Patients: The proposed approach must be adapted to the patients. The data acquired from the different patients must be anonymized and labeled for the healthcare professional’s knowledge responsible for the patient. Only features related to the different data types must be processed because the different data types may identify the patients. Finally, the time zones of the various countries must be controlled to synchronize the results obtained and contacts with different intervenients.
- Features extracted from the data acquired: During the development and testing of the developed methods, the best set of features must be identified to increase the results’ accuracy.
- User interface: The user interface of the proposed approach must be user-friendly for the different ages of the people as the movements for older adults are more limited than children.
4.4. Modeling Challenges
4.5. Integration with Real World
4.6. Limitations of Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Meskó, B.; Drobni, Z.; Bényei, É.; Gergely, B.; Győrffy, Z. Digital health is a cultural transformation of traditional healthcare. Mhealth 2017, 3, 38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bridges, J.F.; Crossnohere, N.L.; Schuster, A.L.; Miller, J.A.; Pastorini, C.; Aslakson, R.A. A patient and community-centered approach selecting endpoints for a randomized trial of a novel advance care planning tool. Patient Prefer. Adherence 2018, 12, 241. [Google Scholar] [CrossRef] [Green Version]
- Goldfield, N.I.; Crittenden, R.; Fox, D.; McDonough, J.; Nichols, L.; Rosenthal, E.L. COVID-19 Crisis Creates Opportunities for Community-Centered Population Health: Community Health Workers: At the Center. J. Ambul. Care Manag. 2020, 43, 184–190. [Google Scholar] [CrossRef] [PubMed]
- McAllister, M.; Dunn, G.; Payne, K.; Davies, L.; Todd, C. Patient empowerment: The need to consider it as a measurable patient-reported outcome for chronic conditions. BMC Health Serv. Res. 2012, 12, 1–8. [Google Scholar] [CrossRef]
- Islam, S.R.; Kwak, D.; Kabir, M.H.; Hossain, M.; Kwak, K.S. The internet of things for health care: A comprehensive survey. IEEE Access 2015, 3, 678–708. [Google Scholar] [CrossRef]
- Vashist, S.K.; Schneider, E.M.; Luong, J.H. Commercial smartphone-based devices and smart applications for personalized healthcare monitoring and management. Diagnostics 2014, 4, 104–128. [Google Scholar] [CrossRef] [PubMed]
- Xu, K.; Chen, Y.; Okhai, T.A.; Snyman, L.W. Micro optical sensors based on avalanching silicon light-emitting devices monolithically integrated on chips. Opt. Mater. Express 2019, 9, 3985–3997. [Google Scholar] [CrossRef]
- Dick, R.S.; Steen, E.B.; Detmer, D.E. The Computer-Based Patient Record: An Essential Technology for Health Care; National Academies Press: Washington, DC, USA, 1997. [Google Scholar]
- Miah, S.J.; Hasan, J.; Gammack, J.G. On-cloud healthcare clinic: An e-health consultancy approach for remote communities in a developing country. Telemat. Inform. 2017, 34, 311–322. [Google Scholar] [CrossRef]
- WHO. Cardiovascular Diseases (CVDs). 2016. Available online: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (accessed on 5 September 2021).
- Goradel, N.H.; Hour, F.G.; Negahdari, B.; Malekshahi, Z.V.; Hashemzehi, M.; Masoudifar, A.; Mirzaei, H. Stem cell therapy: A new therapeutic option for cardiovascular diseases. J. Cell. Biochem. 2018, 119, 95–104. [Google Scholar] [CrossRef]
- Francula-Zaninovic, S.; Nola, I.A. Management of Measurable Variable Cardiovascular Disease’ Risk Factors. Curr. Cardiol. Rev. 2018, 14, 153–163. [Google Scholar] [CrossRef] [PubMed]
- Tang, G.Y.; Meng, X.; Li, Y.; Zhao, C.N.; Liu, Q.; Li, H.B. Effects of vegetables on cardiovascular diseases and related mechanisms. Nutrients 2017, 9, 857. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baraldi, E.; Gregori, G.L.; Perna, A. Network evolution and the embedding of complex technical solutions: The case of the Leaf House network. Ind. Mark. Manag. 2011, 40, 838–852. [Google Scholar] [CrossRef]
- Gardes, J.; Maldivi, C.; Boisset, D.; Aubourg, T.; Vuillerme, N.; Demongeot, J. Maxwell®: An Unsupervised Learning Approach for 5P Medicine. Stud. Health Technol. Inform. 2019, 264, 1464–1465. [Google Scholar] [CrossRef]
- Zheng, Y.L.; Ding, X.R.; Poon, C.C.Y.; Lo, B.P.L.; Zhang, H.; Zhou, X.L.; Yang, G.Z.; Zhao, N.; Zhang, Y.T. Unobtrusive Sensing and Wearable Devices for Health Informatics. IEEE Trans. Biomed. Eng. 2014, 61, 1538–1554. [Google Scholar] [CrossRef] [PubMed]
- Kos, A.; Milutinović, V.; Umek, A. Challenges in wireless communication for connected sensors and wearable devices used in sport biofeedback applications. Future Gener. Comput. Syst. 2019, 92, 582–592. [Google Scholar] [CrossRef]
- Amerini, I.; Becarelli, R.; Caldelli, R.; Melani, A.; Niccolai, M. Smartphone fingerprinting combining features of on-board sensors. IEEE Trans. Inf. Forensics Secur. 2017, 12, 2457–2466. [Google Scholar] [CrossRef]
- Appelboom, G.; Camacho, E.; Abraham, M.E.; Bruce, S.S.; Dumont, E.L.; Zacharia, B.E.; D’Amico, R.; Slomian, J.; Reginster, J.Y.; Bruyère, O.; et al. Smart wearable body sensors for patient self-assessment and monitoring. Arch. Public Health 2014, 72, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kvedar, J.; Coye, M.J.; Everett, W. Connected health: A review of technologies and strategies to improve patient care with telemedicine and telehealth. Health Aff. 2014, 33, 194–199. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hood, L.; Friend, S.H. Predictive, personalized, preventive, participatory (P4) cancer medicine. Nat. Rev. Clin. Oncol. 2011, 8, 184–187. [Google Scholar] [CrossRef] [PubMed]
- Pravettoni, G.; Gorini, A. A P5 cancer medicine approach: Why personalized medicine cannot ignore psychology: P5 medicine. J. Eval. Clin. Pract. 2011, 17, 594–596. [Google Scholar] [CrossRef] [PubMed]
- Van den Heuvel, J.F.; Groenhof, T.K.; Veerbeek, J.H.; van Solinge, W.W.; Lely, A.T.; Franx, A.; Bekker, M.N. eHealth as the Next-Generation Perinatal Care: An Overview of the Literature. J. Med. Internet Res. 2018, 20, e202. [Google Scholar] [CrossRef]
- Granja, C.; Janssen, W.; Johansen, M.A. Factors Determining the Success and Failure of eHealth Interventions: Systematic Review of the Literature. J. Med. Internet Res. 2018, 20, e10235. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gluyas, H. Patient-centred care: Improving healthcare outcomes. Nurs. Stand. (Royal Coll. Nurs. (Great Britain): 1987) 2015, 30, 50–57. [Google Scholar] [CrossRef] [PubMed]
- WHO Guidelines on Hand Hygiene in Health Care: First Global Patient Safety Challenge Clean Care Is Safer Care Patient Empowerment and Health Care; World Health Organization: Geneva, Switzerland, 2009.
- Kambhampati, S.; Ashvetiya, T.; Stone, N.J.; Blumenthal, R.S.; Martin, S.S. Shared Decision-Making and Patient Empowerment in Preventive Cardiology. Curr. Cardiol. Rep. 2016, 18, 49. [Google Scholar] [CrossRef]
- Lau, M.; Campbell, H.; Tang, T.; Thompson, D.J.; Elliott, T. Impact of Patient Use of an Online Patient Portal on Diabetes Outcomes. Can. J. Diabetes 2014, 38, 17–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Risling, T.; Martinez, J.; Young, J.; Thorp-Froslie, N. Evaluating Patient Empowerment in Association With eHealth Technology: Scoping Review. J. Med. Internet Res. 2017, 19, e329. [Google Scholar] [CrossRef] [PubMed]
- Calvillo, J.; Román, I.; Roa, L.M. How technology is empowering patients? A literature review. Health Expect. 2015, 18, 643–652. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lettieri, E.; Fumagalli, L.P.; Radaelli, G.; Bertele’, P.; Vogt, J.; Hammerschmidt, R.; Lara, J.L.; Carriazo, A.; Masella, C. Empowering patients through eHealth: A case report of a pan-European project. BMC Health Serv. Res. 2015, 15, 309. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huniche, L.; Dinesen, B.; Grann, O.; Toft, E.; Nielsen, C. Empowering patients with COPD using Tele-homecare technology. Stud. Health Technol. Inform. 2010, 155, 48–54. [Google Scholar]
- LeBaron, V.; Hayes, J.; Gordon, K.; Alam, R.; Homdee, N.; Martinez, Y.; Ogunjirin, E.; Thomas, T.; Jones, R.; Blackhall, L.; et al. Leveraging Smart Health Technology to Empower Patients and Family Caregivers in Managing Cancer Pain: Protocol for a Feasibility Study. JMIR Res. Protoc. 2019, 8, e16178. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tripoliti, E.E.; Karanasiou, G.S.; Kalatzis, F.G.; Naka, K.K.; Fotiadis, D.I. The Evolution of mHealth Solutions for Heart Failure Management. Adv. Exp. Med. Biol. 2018, 1067, 353–371. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ting, D.S.W.; Carin, L.; Dzau, V.; Wong, T.Y. Digital technology and COVID-19. Nat. Med. 2020, 26, 459–461. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smith, A.C.; Thomas, E.; Snoswell, C.L.; Haydon, H.; Mehrotra, A.; Clemensen, J.; Caffery, L.J. Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19). J. Telemed. Telecare 2020, 26, 309–313. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Majumder, S.; Mondal, T.; Deen, M. Wearable Sensors for Remote Health Monitoring. Sensors 2017, 17, 130. [Google Scholar] [CrossRef] [PubMed]
- Dunn, J.; Runge, R.; Snyder, M. Wearables and the medical revolution. Pers. Med. 2018, 15, 429–448. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Greiwe, J.; Nyenhuis, S.M. Wearable Technology and How This Can Be Implemented into Clinical Practice. Curr. Allergy Asthma Rep. 2020, 20, 36. [Google Scholar] [CrossRef]
- Kruse, C.S.; Frederick, B.; Jacobson, T.; Monticone, D.K. Cybersecurity in healthcare: A systematic review of modern threats and trends. Technol. Health Care 2017, 25, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fanucci, L.; Saponara, S.; Bacchillone, T.; Donati, M.; Barba, P.; Sanchez-Tato, I.; Carmona, C. Sensing Devices and Sensor Signal Processing for Remote Monitoring of Vital Signs in CHF Patients. IEEE Trans. Instrum. Meas. 2013, 62, 553–569. [Google Scholar] [CrossRef]
- Haghi, M.; Thurow, K.; Stoll, R. Wearable Devices in Medical Internet of Things: Scientific Research and Commercially Available Devices. Healthc. Inform. Res. 2017, 23, 4. [Google Scholar] [CrossRef]
- Chow, C.K.; Jolly, S.; Rao-Melacini, P.; Fox, K.A.; Anand, S.S.; Yusuf, S. Association of Diet, Exercise, and Smoking Modification With Risk of Early Cardiovascular Events After Acute Coronary Syndromes. Circulation 2010, 121, 750–758. [Google Scholar] [CrossRef] [Green Version]
- Artinian, N.T.; Fletcher, G.F.; Mozaffarian, D.; Kris-Etherton, P.; Horn, L.V.; Lichtenstein, A.H.; Kumanyika, S.; Kraus, W.E.; Fleg, J.L.; Redeker, N.S.; et al. Interventions to Promote Physical Activity and Dietary Lifestyle Changes for Cardiovascular Risk Factor Reduction in Adults. Circulation 2010, 122, 406–441. [Google Scholar] [CrossRef] [PubMed]
- Chow, C.K.; Ariyarathna, N.; Islam, S.M.S.; Thiagalingam, A.; Redfern, J. mHealth in Cardiovascular Health Care. Hear. Lung Circ. 2016, 25, 802–807. [Google Scholar] [CrossRef] [PubMed]
- Hickey, K.T.; Hauser, N.R.; Valente, L.E.; Riga, T.C.; Frulla, A.P.; Creber, R.M.; Whang, W.; Garan, H.; Jia, H.; Sciacca, R.R.; et al. A single-center randomized, controlled trial investigating the efficacy of a mHealth ECG technology intervention to improve the detection of atrial fibrillation: The iHEART study protocol. BMC Cardiovasc. Disord. 2016, 16, 152. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Varma, N.; Cygankiewicz, I.; Turakhia, M.P.; Heidbuchel, H.; Hu, Y.F.; Chen, L.Y.; Couderc, J.P.; Cronin, E.M.; Estep, J.D.; Grieten, L.; et al. 2021 ISHNE/HRS/EHRA/APHRS Expert Collaborative Statement on mHealth in Arrhythmia Management: Digital Medical Tools for Heart Rhythm Professionals: From the International Society for Holter and Noninvasive Electrocardiology/Heart Rhythm Society/European Heart Rhythm Association/Asia-Pacific Heart Rhythm Society. Circ. Arrhythmia Electrophysiol. 2021, 14, e009204. [Google Scholar] [CrossRef]
- DeVore, A.D.; Wosik, J.; Hernandez, A.F. The Future of Wearables in Heart Failure Patients. JACC Heart Fail. 2019, 7, 922–932. [Google Scholar] [CrossRef]
- Hershman, S.G.; Bot, B.M.; Shcherbina, A.; Doerr, M.; Moayedi, Y.; Pavlovic, A.; Waggott, D.; Cho, M.K.; Rosenberger, M.E.; Haskell, W.L.; et al. Physical activity, sleep and cardiovascular health data for 50,000 individuals from the MyHeart Counts Study. Sci. Data 2019, 6, 24. [Google Scholar] [CrossRef] [Green Version]
- Oresko, J.J.; Jin, Z.; Cheng, J.; Huang, S.; Sun, Y.; Duschl, H.; Cheng, A.C. A Wearable Smartphone-Based Platform for Real-Time Cardiovascular Disease Detection Via Electrocardiogram Processing. IEEE Trans. Inf. Technol. Biomed. 2010, 14, 734–740. [Google Scholar] [CrossRef]
- Rapin, M.; Braun, F.; Adler, A.; Wacker, J.; Frerichs, I.; Vogt, B.; Chetelat, O. Wearable Sensors for Frequency-Multiplexed EIT and Multilead ECG Data Acquisition. IEEE Trans. Biomed. Eng. 2019, 66, 810–820. [Google Scholar] [CrossRef]
- Banaee, H.; Ahmed, M.; Loutfi, A. Data Mining for Wearable Sensors in Health Monitoring Systems: A Review of Recent Trends and Challenges. Sensors 2013, 13, 17472–17500. [Google Scholar] [CrossRef] [Green Version]
- Miao, F.; Cheng, Y.; He, Y.; He, Q.; Li, Y. A Wearable Context-Aware ECG Monitoring System Integrated with Built-in Kinematic Sensors of the Smartphone. Sensors 2015, 15, 11465–11484. [Google Scholar] [CrossRef] [Green Version]
- Poongodi, T.; Rathee, A.; Indrakumari, R.; Suresh, P. IoT Sensing Capabilities: Sensor Deployment and Node Discovery, Wearable Sensors, Wireless Body Area Network (WBAN), Data Acquisition. In Principles of Internet of Things (IoT) Ecosystem: Insight Paradigm; Intelligent Systems Reference Library; Peng, S.L., Pal, S., Huang, L., Eds.; Springer International Publishing: Geneva, Switzerland, 2020; Volume 174, pp. 127–151. [Google Scholar] [CrossRef]
- Dubey, H.; Yang, J.; Constant, N.; Amiri, A.M.; Yang, Q.; Makodiya, K. Fog Data: Enhancing Telehealth Big Data Through Fog Computing. In Proceedings of the ASE BigData & SocialInformatics 2015, ASE BD & SI’15, Kaohsiung, Taiwan, 7–9 October 2015; pp. 1–6. [Google Scholar]
- Melillo, P.; Orrico, A.; Scala, P.; Crispino, F.; Pecchia, L. Cloud-Based Smart Health Monitoring System for Automatic Cardiovascular and Fall Risk Assessment in Hypertensive Patients. J. Med. Syst. 2015, 39, 109. [Google Scholar] [CrossRef] [PubMed]
- Mohammed, K.I.; Zaidan, A.A.; Zaidan, B.B.; Albahri, O.S.; Alsalem, M.A.; Albahri, A.S.; Hadi, A.; Hashim, M. Real-Time Remote-Health Monitoring Systems: A Review on Patients Prioritisation for Multiple-Chronic Diseases, Taxonomy Analysis, Concerns and Solution Procedure. J. Med. Syst. 2019, 43, 223. [Google Scholar] [CrossRef] [PubMed]
- Ping, P.; Hermjakob, H.; Polson, J.S.; Benos, P.V.; Wang, W. Biomedical Informatics on the Cloud: A Treasure Hunt for Advancing Cardiovascular Medicine. Circ. Res. 2018, 122, 1290–1301. [Google Scholar] [CrossRef] [PubMed]
- Mora, H.; Gil, D.; Terol, R.M.; Azorín, J.; Szymanski, J. An IoT-Based Computational Framework for Healthcare Monitoring in Mobile Environments. Sensors 2017, 17, 2302. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Azimi, I.; Pahikkala, T.; Rahmani, A.M.; Niela-Vilén, H.; Axelin, A.; Liljeberg, P. Missing data resilient decision-making for healthcare IoT through personalization: A case study on maternal health. Future Gener. Comput. Syst. 2019, 96, 297–308. [Google Scholar] [CrossRef]
- Gia, T.N.; Jiang, M.; Rahmani, A.M.; Westerlund, T.; Liljeberg, P.; Tenhunen, H. Fog Computing in Healthcare Internet of Things: A Case Study on ECG Feature Extraction. In Proceedings of the 2015 IEEE International Conference on Computer and Information Technology; Ubiquitous Computing and Communications; Dependable, Autonomic and Secure Computing; Pervasive Intelligence and Computing, Liverpool, UK, 26–28 October 2015; pp. 356–363. [Google Scholar] [CrossRef]
- Kenneth, E.; Rajendra, A.; Kannathal, N.; Lim, C.M. Data Fusion of Multimodal Cardiovascular Signals. In Proceedings of the 2005 IEEE Engineering in Medicine and Biology 27th Annual Conference, Shanghai, China, 1–4 September 2005; pp. 4689–4692. [Google Scholar] [CrossRef]
- Kannathal, N.; Acharya, U.R.; Ng, E.; Krishnan, S.; Min, L.C.; Laxminarayan, S. Cardiac health diagnosis using data fusion of cardiovascular and haemodynamic signals. Comput. Methods Programs Biomed. 2006, 82, 87–96. [Google Scholar] [CrossRef]
- King, R.C.; Villeneuve, E.; White, R.J.; Sherratt, R.S.; Holderbaum, W.; Harwin, W.S. Application of data fusion techniques and technologies for wearable health monitoring. Med. Eng. Phys. 2017, 42, 1–12. [Google Scholar] [CrossRef]
- Van den Heuvel, E.R.; Vasan, R.S. Statistics in cardiovascular medicine: There is still gold in the old. Heart 2018, 104, 1227. [Google Scholar] [CrossRef]
- Ang, L.M.; Seng, K.P. Big Sensor Data Applications in Urban Environments. Big Data Res. 2016, 4, 1–12. [Google Scholar] [CrossRef]
- Dash, S.; Shakyawar, S.K.; Sharma, M.; Kaushik, S. Big data in healthcare: Management, analysis and future prospects. J. Big Data 2019, 6, 54. [Google Scholar] [CrossRef] [Green Version]
- Rajabion, L.; Shaltooki, A.A.; Taghikhah, M.; Ghasemi, A.; Badfar, A. Healthcare big data processing mechanisms: The role of cloud computing. Int. J. Inf. Manag. 2019, 49, 271–289. [Google Scholar] [CrossRef]
- Saheb, T.; Izadi, L. Paradigm of IoT big data analytics in the healthcare industry: A review of scientific literature and mapping of research trends. Telemat. Inform. 2019, 41, 70–85. [Google Scholar] [CrossRef]
- PLUX Wireless Biosignals. Available online: https://plux.info/ (accessed on 10 September 2021).
- Matias, I.; Garcia, N.; Pirbhulal, S.; Felizardo, V.; Pombo, N.; Zacarias, H.; Sousa, M.; Zdravevski, E. Prediction of Atrial Fibrillation using artificial intelligence on Electrocardiograms: A systematic review. Comput. Sci. Rev. 2021, 39, 100334. [Google Scholar] [CrossRef]
- Kelders, S.M.; van Zyl, L.E.; Ludden, G.D.S. The Concept and Components of Engagement in Different Domains Applied to eHealth: A Systematic Scoping Review. Front. Psychol. 2020, 11, 926. [Google Scholar] [CrossRef]
- Baumel, A.; Kane, J.M. Examining Predictors of Real-World User Engagement with Self-Guided eHealth Interventions: Analysis of Mobile Apps and Websites Using a Novel Dataset. J Med. Internet Res 2018, 20, e11491. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Gemert-Pijnen, L.; Kelders, S.M.; Kip, H.; Sanderman, R. eHealth Research, Theory and Development: A Multi-Disciplinary Approach; Routledge: Abingdon, UK, 2018. [Google Scholar]
- Baumel, A.; Yom-Tov, E. Predicting user adherence to behavioral eHealth interventions in the real world: Examining which aspects of intervention design matter most. Transl. Behav. Med. 2018, 8, 793–798. [Google Scholar] [CrossRef] [PubMed]
- Gorst, S.L.; Armitage, C.J.; Brownsell, S.; Hawley, M.S. Home Telehealth Uptake and Continued Use Among Heart Failure and Chronic Obstructive Pulmonary Disease Patients: A Systematic Review. Ann. Behav. Med. 2014, 48, 323–336. [Google Scholar] [CrossRef] [Green Version]
- Xu, K. Silicon electro-optic micro-modulator fabricated in standard CMOS technology as components for all silicon monolithic integrated optoelectronic systems. J. Micromech. Microeng. 2021, 31, 054001. [Google Scholar] [CrossRef]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pires, I.M.; Denysyuk, H.V.; Villasana, M.V.; Sá, J.; Lameski, P.; Chorbev, I.; Zdravevski, E.; Trajkovik, V.; Morgado, J.F.; Garcia, N.M. Mobile 5P-Medicine Approach for Cardiovascular Patients. Sensors 2021, 21, 6986. https://doi.org/10.3390/s21216986
Pires IM, Denysyuk HV, Villasana MV, Sá J, Lameski P, Chorbev I, Zdravevski E, Trajkovik V, Morgado JF, Garcia NM. Mobile 5P-Medicine Approach for Cardiovascular Patients. Sensors. 2021; 21(21):6986. https://doi.org/10.3390/s21216986
Chicago/Turabian StylePires, Ivan Miguel, Hanna Vitaliyivna Denysyuk, María Vanessa Villasana, Juliana Sá, Petre Lameski, Ivan Chorbev, Eftim Zdravevski, Vladimir Trajkovik, José Francisco Morgado, and Nuno M. Garcia. 2021. "Mobile 5P-Medicine Approach for Cardiovascular Patients" Sensors 21, no. 21: 6986. https://doi.org/10.3390/s21216986
APA StylePires, I. M., Denysyuk, H. V., Villasana, M. V., Sá, J., Lameski, P., Chorbev, I., Zdravevski, E., Trajkovik, V., Morgado, J. F., & Garcia, N. M. (2021). Mobile 5P-Medicine Approach for Cardiovascular Patients. Sensors, 21(21), 6986. https://doi.org/10.3390/s21216986










