Sleep and COVID-19. A Case Report of a Mild COVID-19 Patient Monitored by Consumer-Targeted Sleep Wearables
Abstract
:1. Introduction
2. Materials and Methods
2.1. Clinical Case
2.2. Subjective Sleep Data: From Incubation Phase to Recovery
2.3. Objective Sleep Data Assessment
2.4. Data Analysis
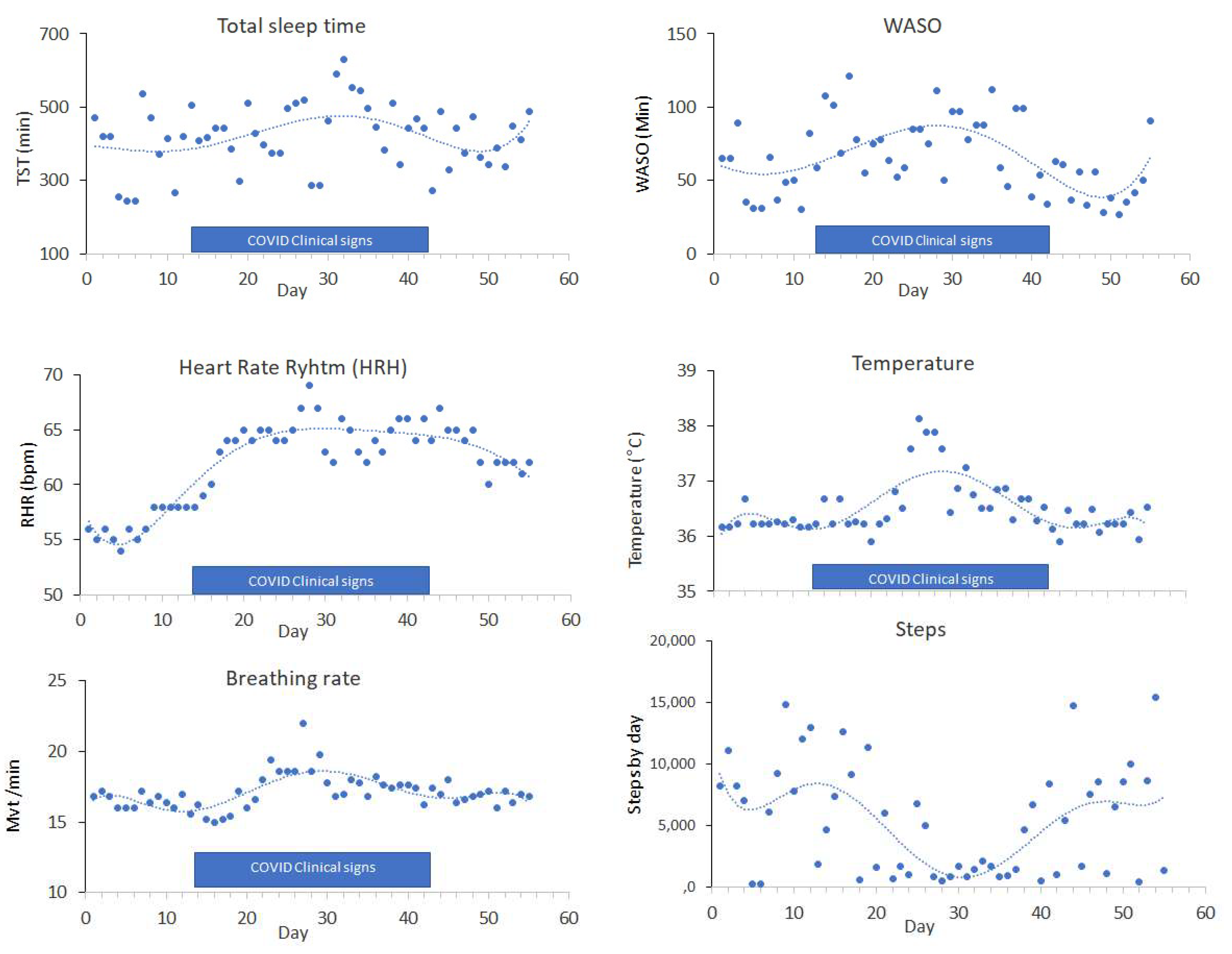
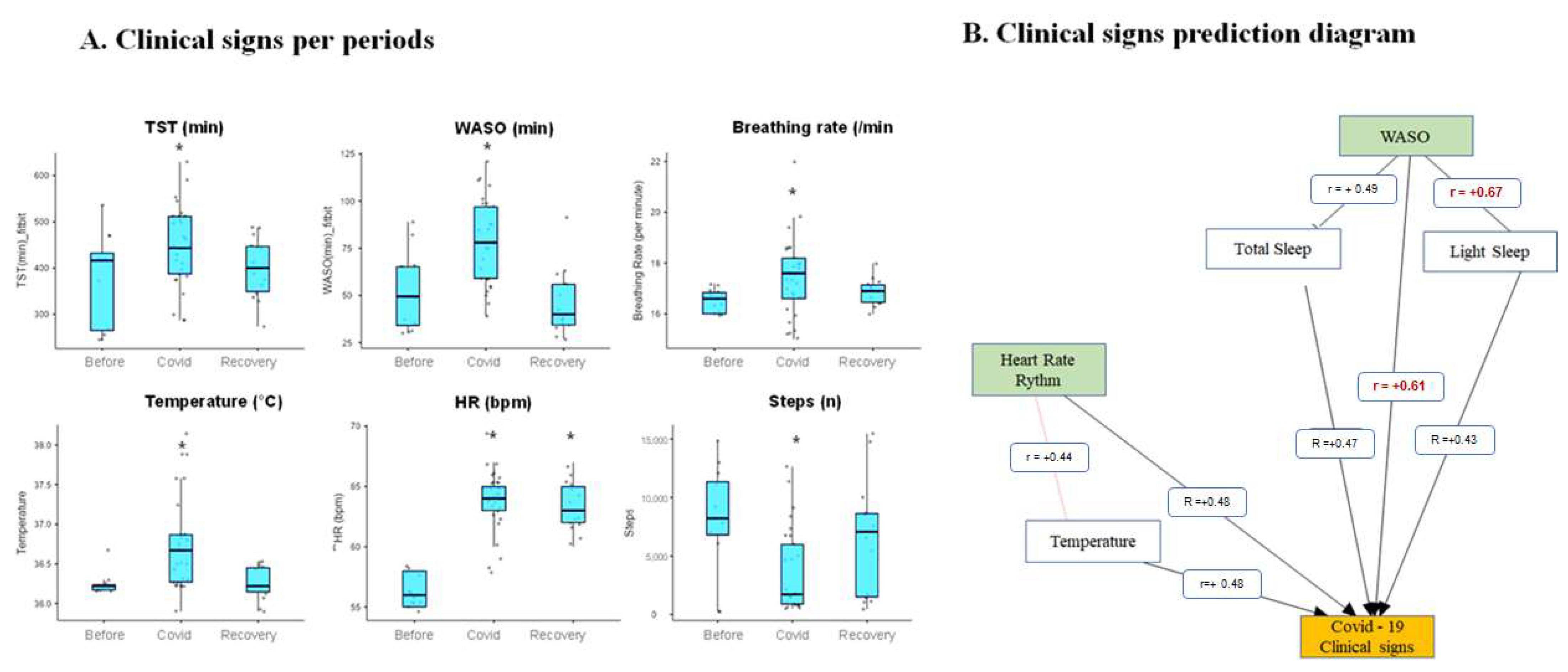
3. Results
4. Ethics Declarations
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. Coronavirus Disease (COVID-2019) Situation Report. 25 August 2020; WHO: Geneva, Switzerland, 2020; Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/ (accessed on 25 August 2020).
- Salzberger, B.; Buder, F.; Lampl, B.; Ehrenstein, B.; Hitzenbichler, F.; Holzmann, T.; Schmidt, B.; Hanses, F. Epidemiology of SARS-CoV-2. Infection 2021, 49, 233–239. [Google Scholar] [CrossRef] [PubMed]
- Bent, B.; Dunn, J.P. Wearables in the SARS-CoV-2 Pandemic: What Are They Good for? JMIR mHealth uHealth 2020, 8, e25137. [Google Scholar] [CrossRef] [PubMed]
- Altini, M.; Kinnunen, H. The promise of Sleep: A Multi-Sensor Approach for Accurate Sleep Stage Detection Using The Oura Ring. Sensors 2021, 21, 4302. [Google Scholar] [CrossRef] [PubMed]
- Haghayegh, S.; Khoshnevis, S.; Smolensky, M.H.; Diller, K.R.; Castriotta, R.J. Accuracy of Wristband Fitbit Models in Assessing Sleep: Systematic Review and Meta-Analysis. J. Med. Internet Res. 2019, 21, e16273. [Google Scholar] [CrossRef] [PubMed]
- Elbaz, M.; Robbins, R.; Bouchequet, P.; Czeiler, C.; Leger, D. Examining Sleep Duration and Social Jetlag From a Popular Wearable Sleep Tracker in France and Canada. Sleep 2020, 43, A170. [Google Scholar] [CrossRef]
- Natarajan, A.; Su, H.-W.; Heneghan, C. Assessment of physiological signs associated with COVID-19 measured using wearable devices. NPJ Digit. Med. 2020, 30, 156. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Xu, D.; Xie, B.; Zhang, Y.; Huang, H.; Liu, H.; Chen, H.; Sun, Y.; Shang, Y.; Hashimoto, K.; et al. Poor-sleep is associated with slow recovery from lymphopenia and an increased need for ICU care in hospitalized patients with COVID-19: A retrospective cohort study. Brain Behav. Immun. 2020, 88, 50–58. [Google Scholar] [CrossRef] [PubMed]
- Beck, F.; Leger, D.; Cortaredona, S.; Verger, P.; Peretti-Watel, P.; COCONEL Group. Would we recover better sleep at the end of Covid-19? A relative improvement observed at the population level with the end of the lockdown in France. Sleep Med. 2021, 78, 115–119. [Google Scholar] [CrossRef] [PubMed]
- Ibarra-Coronado, E.G.; Pantaleón-Martínez, A.M.; Velazquéz-Moctezuma, J.; Prospéro-García, O.; Méndez-Díaz, M.; Pérez-Tapia, M.; Pavón, L.; Morales-Montor, J. The Bidirectional Relationship Between Sleep and Immunity Against Infections. J. Immunol. Res. 2015, 2015, 678164. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gill, C.M.; Piggott, L.M.; Kent, B.D. Sleep medicine and coronavirus disease 2019. Curr. Opin. Pulm. Med. 2021, 27, 529–534. [Google Scholar] [CrossRef] [PubMed]
| Name | Fitbit Versa 2 (Fitbit Now Part of Google) | Oura Ring (Oura) | iSleepWatch for AppleWatch5 (iSommeil) |
|---|---|---|---|
| Picture |  |  |  |
| Resting Heart Rate | YES | YES | YES |
| Body Temperature | NO | YES | NO |
| Actigraphy 3 axis accelerometer | YES | YES | YES |
| Respiratory rate | YES | YES | NO |
| Snoring | NO | NO | YES |
| Sleep analysis validation reference | Haghayegh et al., 2019 [5] | Altini et al., 2021 [4] | Elbaz et al., 2020 [6] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Metlaine, A.; Sauvet, F.; Chennaoui, M.; Leger, D.; Elbaz, M. Sleep and COVID-19. A Case Report of a Mild COVID-19 Patient Monitored by Consumer-Targeted Sleep Wearables. Sensors 2021, 21, 7944. https://doi.org/10.3390/s21237944
Metlaine A, Sauvet F, Chennaoui M, Leger D, Elbaz M. Sleep and COVID-19. A Case Report of a Mild COVID-19 Patient Monitored by Consumer-Targeted Sleep Wearables. Sensors. 2021; 21(23):7944. https://doi.org/10.3390/s21237944
Chicago/Turabian StyleMetlaine, Arnaud, Fabien Sauvet, Mounir Chennaoui, Damien Leger, and Maxime Elbaz. 2021. "Sleep and COVID-19. A Case Report of a Mild COVID-19 Patient Monitored by Consumer-Targeted Sleep Wearables" Sensors 21, no. 23: 7944. https://doi.org/10.3390/s21237944
APA StyleMetlaine, A., Sauvet, F., Chennaoui, M., Leger, D., & Elbaz, M. (2021). Sleep and COVID-19. A Case Report of a Mild COVID-19 Patient Monitored by Consumer-Targeted Sleep Wearables. Sensors, 21(23), 7944. https://doi.org/10.3390/s21237944







