Wearable Devices Suitable for Monitoring Twenty Four Hour Heart Rate Variability in Military Populations
Abstract
:1. Introduction
2. Materials and Methods
3. Results
- Bittium FarosTM (Bittium, Oulu, Finland);
- Bodyguard 2 (Firstbeat Technologies Ltd., Jyväskylä, Finland);
- Actiheart (CamNtech Ltd., Cambridgeshire, UK);
- AidlabTM (AidlabTM, Gdańsk, Poland);
- Polar H10 (Polar Electro UK Ltd., Warwick, UK);
- Equivital EQ-02 (Equivital, Cambridge, UK);
- Empatica E4 (Empatica Inc, Boston, United States);
- Biovotion Everion® (Biofourmis, Boston, United States).
- Garmin Fenix® 6X and 6S (Garmin Ltd., Southampton, UK);
- Garmin Tactix® Charlie/Delta (Garmin Ltd., Southampton, UK);
- Polar Vantage V (Polar Electro UK Ltd., Warwick, UK);
- Actigraph wGT3X-BT (Actigraph, Pensacola, United States).
3.1. ECG Monitors
3.1.1. Bittium FarosTM 360
3.1.2. Actiheart
3.1.3. Firstbeat Bodyguard 2
3.2. Clothing Garments
3.2.1. AidlabTM
3.3. Chest, Shoulder and Arm Straps/Bands
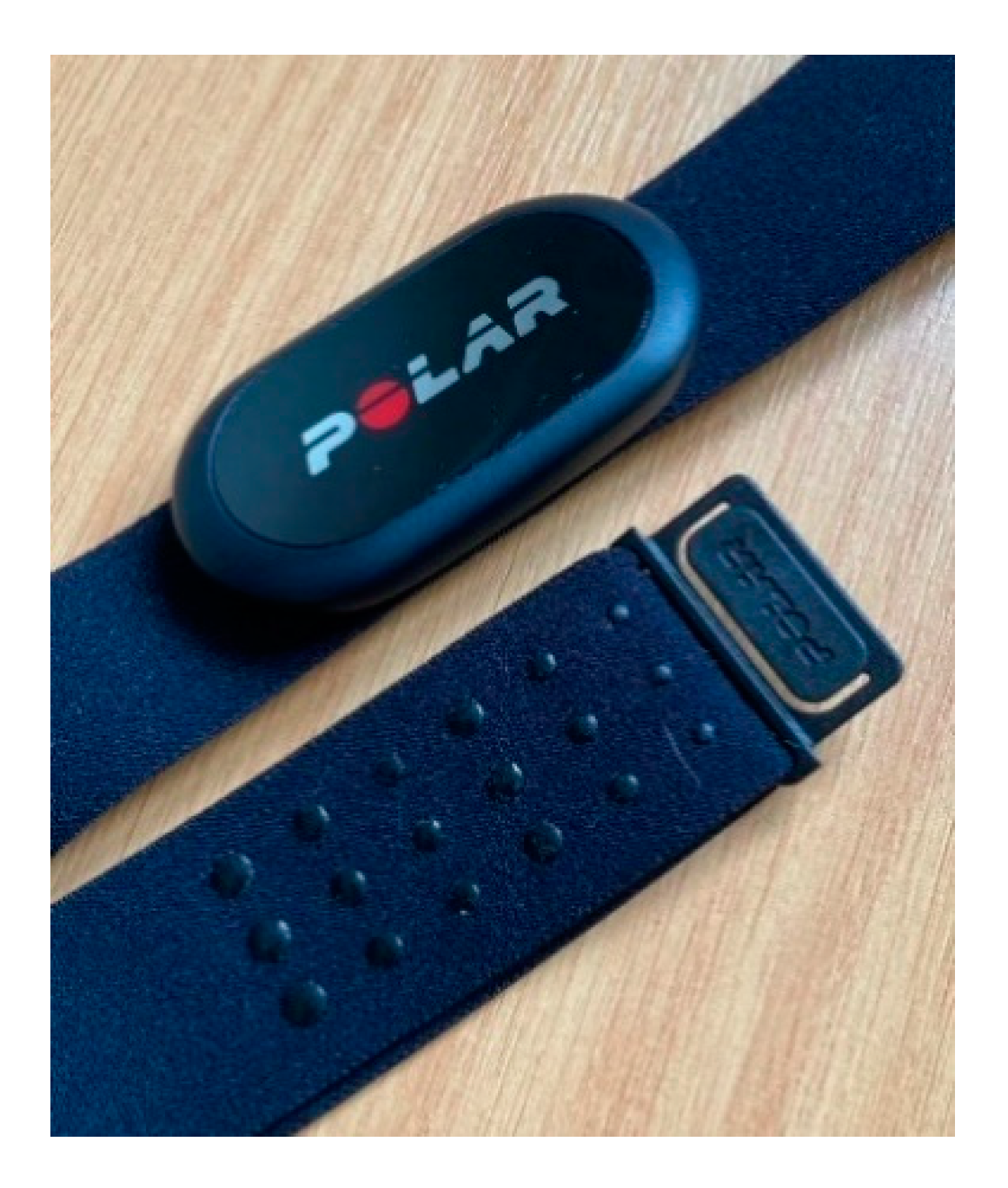
3.3.1. Polar H10 Heart Rate Monitor
3.3.2. Equivital EQ-02

3.3.3. Biovotion Everion®
3.4. Wrist Watches
3.4.1. Empatica E4
3.4.2. Polar Vantage V
3.4.3. Garmin Watches
3.4.4. Actigraph wGT3X-BT
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- The, A.F.; Reijmerink, I.; van der Laan, M.; Cnossen, F. Heart rate variability as a measure of mental stress in surgery: A systematic review. Int. Arch. Occup. Environ. Health 2020. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shaffer, F.; Ginsberg, J.P. An overview of heart rate variability metrics and norms. Front. Public Health 2017, 5, 258. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gilgen-Ammann, R.; Schweizer, T.; Wyss, T. RR interval signal quality of a heart rate monitor and an ECG Holter at rest and during exercise. Eur. J. Appl. Physiol. 2019, 119, 1525–1532. [Google Scholar] [CrossRef] [PubMed]
- Georgiou, K.; Larentzakis, A.V.; Khamis, N.N.; Alsuhaibani, G.I.; Alaska, Y.A.; Giallafos, E.J. Can wearable devices accurately measure heart rate variability? A systematic review. Folia Med. 2018, 60, 7–20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Singh, N.; Moneghetti, K.J.; Christle, J.W.; Hadley, D.; Froelicher, V.; Plews, D. Heart rate variability: An old metric with new meaning in the era of using health technologies for health and exercise training guidance. Part two: Prognosis and training. Arrhythm Electrophysiol. Rev. 2018, 7, 247–255. [Google Scholar] [CrossRef] [PubMed]
- Sassi, R.; Cerutti, S.; Lombardi, F.; Malik, M.; Huikuri, H.V.; Peng, C.K.; Schmidt, G.; Yamamoto, Y. Advances in heart rate variability signal analysis: Joint position statement by the e-Cardiology ESC Working Group and the European Heart Rhythm Association co-endorsed by the Asia Pacific Heart Rhythm Society. Europace 2015, 17, 1341–1353. [Google Scholar] [CrossRef] [PubMed]
- Malik, M.; Hnatkova, K.; Huikuri, H.; Lombardi, F.; Schmidt, G.; Zabel, M. CrossTalk proposal: Heart rate variability is a valid measure of cardiac autonomic responsiveness. J. Physiol. 2019, 597, 2595–2598. [Google Scholar] [CrossRef] [PubMed]
- Grant, C.C.; van Rensburg, D.C.; Strydom, N.; Viljoen, M. Importance of tachogram length and period of recording during noninvasive investigation of the autonomic nervous system. Ann. Noninvasive Electrocardiol. 2011, 16, 131–139. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.G.; Cheon, E.J.; Bai, D.S.; Lee, Y.H.; Koo, B.H. Stress and Heart Rate Variability: A Meta-Analysis and Review of the Literature. Psychiatry Investig. 2018, 15, 235–245. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Camm, A.J.; Malik, M.; Bigger, J.T.; Breithardt, G.; Cerutti, S.; Cohen, R.J.; Coumel, P.; Fallen, E.L.; Kennedy, H.L.; Kleiger, R.E.; et al. Heart rate variability: Standards of measurement, physiological interpretation and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Eur. Heart J. 1996, 17, 354–381. [Google Scholar]
- Lazzeroni, D.; Ziloli, C.; Colio, F.; Catellani, G.; Paglialonga, L.; Marazzi, P.; Moderato, L.; Bini, M.; Camaiora, U.; Geroldi, S.; et al. Relationship between ultra-low frequency of heart rate variability and autonomic function assessed by both 24H Holter ECG monitoring and cardiopulmonary exercise testing. Eur. Heart J. Suppl. 2019, 21, 197. [Google Scholar]
- Pagani, M.; Lombardi, F.; Guzzetti, S.; Rimoldi, O.; Furlan, R.; Pizzinelli, P.; Sandrone, G.; Malfatto, G.; Dell’Orto, S.; Piccaluga, E. Power spectral analysis of heart rate and arterial pressure variabilities as a marker of sympatho-vagal interaction in man and conscious dog. Circ. Res. 1986, 59, 178–193. [Google Scholar] [CrossRef] [Green Version]
- Billman, G.E. The LF/HF ratio does not accurately measure cardiac sympatho-vagal balance. Front. Physiol. 2013, 4, 26. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hernando, D.; Hernando, A.; Casajus, J.A.; Laguna, P.; Garatachea, N.; Bailon, R. Methodological framework for heart rate variability analysis during exercise: Application to running and cycling stress testing. Med. Biol. Eng. Comput. 2018, 56, 781–794. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, D.F.; Ferraro, Z.M.; Adamo, K.B.; Machado, F.A. Endurance Running Training Individually Guided by HRV in Untrained Women. J. Strength Cond. Res. 2019, 33, 736–746. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, S.; Ramsay, T.; Huebsch, L.; Flanagan, S.; McDiarmid, S.; Batkin, I.; McIntyre, L.; Sundaresan, S.R.; Maziak, D.E.; Shamji, F.M.; et al. Continuous multi-parameter heart rate variability analysis heralds onset of sepsis in adults. PLoS ONE 2009, 4, e6642. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, C.; Alamili, M.; Rosenberg, J.; Gogenur, I. Heart rate variability is reduced during acute uncomplicated diverticulitis. J. Crit. Care 2016, 32, 189–195. [Google Scholar] [CrossRef] [PubMed]
- Forte, G.; Favieri, F.; Casagrande, M. Heart Rate Variability and Cognitive Function: A Systematic Review. Front. Neurosci. 2019, 13. [Google Scholar] [CrossRef] [PubMed]
- Shah, A.J.; Su, S.; Veledar, E.; Bremner, J.D.; Goldstein, F.C.; Lampert, R.; Goldberg, J.; Vaccarino, V. Is heart rate variability related to memory performance in middle-aged men? Psychosom. Med. 2011, 73, 475–482. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hansen, A.L.; Johnsen, B.H.; Thayer, J.F. Vagal influence on working memory and attention. Int. J. Psychophysiol. 2003, 48, 263–274. [Google Scholar] [CrossRef]
- Lewis, M.J.; Kingsley, M.; Short, A.L.; Simpson, K. Rate of reduction of heart rate variability during exercise as an index of physcal work capacity. Scand. J. Med. Sci. Sports 2007, 17, 696–702. [Google Scholar] [CrossRef]
- Messerotti Benvenuti, S.; Mennella, R.; Buodo, G.; Palomba, D. Dysphoria is associated with reduced cardiac vagal withdrawal duringthe imagery of pleasant scripts: Evidence for the positive attenuation hypothesis. Biol. Psychol. 2015, 106, 28–38. [Google Scholar] [CrossRef] [PubMed]
- Flatt, A.A.; Esco, M.R. Heart rate variability stabilization in athletes: Towards more convenient data acquisition. Clin. Physiol. Funct. Imaging 2016, 36, 331–336. [Google Scholar] [CrossRef] [PubMed]
- Morgan, C.A., 3rd; Aikins, D.E.; Steffian, G.; Coric, V.; Southwick, S. Relation between cardiac vagal tone and performance in male military personnel exposed to high stress: Three prospective studies. Psychophysiology 2007, 44, 120–127. [Google Scholar] [CrossRef] [PubMed]
- Dobbs, W.C.; Fedewa, M.V.; MacDonald, H.V.; Holmes, C.J.; Cicone, Z.S.; Plews, D.J.; Esco, M.R. The Accuracy of Acquiring Heart Rate Variability from Portable Devices: A Systematic Review and Meta-Analysis. Sports Med. 2019, 49, 417–435. [Google Scholar] [CrossRef] [PubMed]
- Plews, D.J.; Laursen, P.B.; Kilding, A.E.; Buchheit, M. Evaluating Training Adaptation with Heart-Rate Measures: A Methodological Comparison. Int. J. Sports Physiol. Perform. 2013, 8, 688–691. [Google Scholar] [CrossRef] [PubMed]
- Kinnunen, H.; Rantanen, A.; Kentta, T.; Koskimaki, H. Feasible assessment of recovery and cardiovascular health: Accuracy of nocturnal HR and HRV assessed via ring PPG in comparison to medical grade ECG. Physiol. Meas. 2020, 41, 04NT01. [Google Scholar] [CrossRef] [PubMed]
- Bent, B.; Goldstein, B.A.; Kibbe, W.A.; Dunn, J.P. Investigating sources of inaccuracy in wearable optical heart rate sensors. NPJ Digit. Med. 2020, 3, 18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vescio, B.; Salsone, M.; Gambardella, A.; Quattrone, A. Comparison between Electrocardiographic and Earlobe Pulse Photoplethysmographic Detection for Evaluating Heart Rate Variability in Healthy Subjects in Short- and Long-Term Recordings. Sensors 2018, 18, 844. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Laarni, J.; Pakarinen, S.; Bordi, M.; Kallinen, K.; Narvainen, J.; Kortelainen, H.; Lukander, K.; Pettersson, K.; Havola, J.; Pihlainen, K. Promoting Soldier Cognitive Readiness for Battle Tank Operations Through Bio-signal Measurements. In International Conference in Applied Human Factors and Ergonomics; Springer: Cham, Switzerland, 2019; pp. 142–154. [Google Scholar]
- Bittium. Bittium FarosTM—Cardiac Monitoring. Available online: https://www.bittium.com/medical/bittium-faros (accessed on 28 January 2021).
- Kristiansen, J.; Korshøj, M.; Skotte, J.H.; Jespersen, T.; Søgaard, K.; Mortensen, O.S.; Holtermann, A. Comparison of two systems for long-term heart rate variability monitoring in free-living conditions- a pilot study. Biomed. Eng. Online 2011, 10, 1–14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brage, S.; Westgate, K.; Franks, P.W.; Stegle, O.; Wright, A.; Ekelund, U.; Wareham, N.J. Estimation of Free-Living Energy Expenditure by Heart Rate and Movement Sensing: A Doubly-Labelled Water Study. PLoS ONE 2015, 10. [Google Scholar] [CrossRef] [Green Version]
- Hallman, D.M.; Sato, T.; Kristiansen, J.; Gupta, N.; Skotte, J.; Holtermann, A. Prolonged Sitting is Associated with Attenuated Heart Rate Variability during Sleep in Blue-Collar Workers. Int. J. Environ. Res. Public Health 2015, 12, 14811–14827. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- CamNtech. Actiheart 5. Available online: https://www.camntech.com/actiheart-5/ (accessed on 28 January 2021).
- Bogdány, T.; Boros, S.; Szemerszky, R.; Köteles, F. Validation of the Firstbeat TeamBelt and BodyGuard2 systems. Magy. Sporttudományi Szle. 2016, 17, 5–12. [Google Scholar]
- Parak, J.; Korhonen, I. Accuracy of Firstbeat Bodyguard 2 Beat-to-Beat Heart Rate Monitor; White Paper; Firstbeat Technology Ltd.: Tampere, Finland, 2013. [Google Scholar]
- Firstbeat Ltd. Bodyguard 2. Available online: https://shop.firstbeat.com/product/bodyguard-2/ (accessed on 28 January 2021).
- Czekaj, L.; Daniszewski, M.; Domaszewicz, J. Validation of the Aidlab solution for measuring Heart Rate Variability; Aidlab: Gdańsk, Poland, 2019. [Google Scholar]
- Cheatham, S.W.; Kolber, M.J.; Ernst, M.P. Concurrent validity of resting pulse-rate measurements: A comparison of 2 smartphone applications, the polar H7 belt monitor, and a pulse oximeter with bluetooth. J. Sport Rehabil. 2015, 24, 171–178. [Google Scholar] [CrossRef] [PubMed]
- Giles, D.; Draper, N.; Neil, W. Validity of the Polar V800 heart rate monitor to measure RR intervals at rest. Eur. J. Appl. Physiol. 2016, 116, 563–571. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tharion, W.J.; Hoyt, R.W. Form Factor Evaluation of Open Body Area Network (OBAN) Physiological Status Monitoring (PSM) System Prototype Designs; U.S. Army Research Insititue of Environmental Medicine: Natick, MA, USA, 2018. [Google Scholar]
- Teien, H.K.; Castellani, J.; Martini, S.; Pasiakos, S.M. Physiological monitoring during multi-day Norwegian ski patrols in the artic. J. Sci. Med. Sport 2017, 20, S134–S135. [Google Scholar] [CrossRef]
- Reiger, A.; Stoll, R.; Kreuzfeld, S.; Behrens, K.; Weippert, M. Heart rate and heart rate variability as indirect markers of surgeons’ intraoperative stress. Int. Arch. Occup. Environ. Health 2014, 87, 165–174. [Google Scholar] [CrossRef] [PubMed]
- Tharion, W.J.; Buller, M.J.; Potter, A.W.; Karis, A.J.; Goetz, V.; Hoyt, R. Acceptability and usability of an ambulatory health monitoring system for use by military personnel. IIE Trans. Occup. Ergon. Human Factors 2013, 1, 203–214. [Google Scholar] [CrossRef]
- Tharion, W.J.; Buller, M.J.; Clements, C.M.; Dominguez, D.; Sampsonis, C.; Mullen, S.P.; Karis, A.J.; Potter, A.W. Human Factors Evaluation of Equvital EQ-02 Physiological Status Monitoring System; Army Research Institute of Environmental Medicine: Natick, MA, USA, 2013. [Google Scholar]
- Akintola, A.A.; van de Pol, V.; Bimmel, D.; Maan, A.C.; van Heemst, D. Comparative Analysis of the Equivital EQ02 Lifemonitor with Holter Ambulatory ECG Device for Continuous Measurement of ECG, Heart Rate, and Heart Rate Variability: A Validation Study for Precision and Accuracy. Front. Physiol. 2016, 7, 391. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Equivital. eq lifemonitor. Available online: https://www.equivital.com/products/eq02-lifemonitor (accessed on 28 January 2021).
- Barrios, L.; Oldrati, P.; Santini, S.; Lutterotti, A. Evaluating the accuracy of heart rate sensors based on photoplethysmography for in-the-wild analysis. In Proceedings of the 13th EAI International Conference on Pervasive Computing Technologies for Healthcare, Trento, Italy, 20–23 May 2019; pp. 251–261. [Google Scholar]
- McCarthy, C.; Pradhan, N.; Redpath, C.; Adler, A. Validation of the Empatica E4 wristband. In Proceedings of the IEEE EMBS International Student Conference, Ottawa, ON, Canada, 29–31 May 2016; pp. 1–4. [Google Scholar]
- Pietilä, J.; Mehrang, S.; Tolonen, J.; Helander, E.; Jimison, H.; Pavel, M.; Korhonen, I. Evaluation of the accuracy and reliability for photoplethysmography based heart rate and beat-to-beat detection during daily activities. In Proceedings of the 37th Annual International Conference IEEE Engineering Medicine Biology Society, Milano, Italy, 25–29 August 2015; pp. 145–148. [Google Scholar] [CrossRef]
- Speer, K.E.; Semple, S.; Naumovski, N.; McKune, A.J. Measuring heart rate variability using commercially available devices in healthy children: A validity and reliability study. Eur. J. Investig. Health Psychol. Educ. 2020, 10, 390–404. [Google Scholar] [CrossRef] [Green Version]
- Morrin, N.M.; Stone, M.R.; Henderson, K.J. Reproducability of 24-h ambulatory blood pressure and measures of autonomic function. Blood Press. Monit. 2017, 22, 169. [Google Scholar] [CrossRef] [PubMed]




| Assessment Criteria | Rating | ||
|---|---|---|---|
| 1. Is the device capable of continuous HRV measurement? | No | n/a. | Yes. |
| 2. Does it measure a range of HRV parameters? | No, only 1 HRV parameter is measured. | Yes, but limited selection. | Yes, a full range of HRV parameters can be measured. |
| 3. Does the device produce valid HRV measures? (compared against criterion measures) | Demonstrates poor validity, or validity unknown. | Yes, but results are poor-moderate OR HRV measures are only valid during rest OR validity study is limited. | Yes valid during all conditions. Results are good to excellent validity. |
| 4. Does the device have a battery life >24 h? | Battery life is less than 24 h | Battery life is 24–36 h | Battery life is >36 h |
| 5. Does the device have an internal memory capacity? | No internal memory at all/ no information available. | Internal memory is ≤24 h | Internal memory is >24 h |
| 6. Can the raw data be accessed? | No raw data, only processed data are available. | Yes, but has to be accessed through another platform or device or through agreement with company. | Yes, directly through CSV, FIT file or other open format. |
| 7. Is the device robust? | No | Yes to some degree, but some features of it may require further investigation for their ability to withstand harsh conditions/ movements. | Yes. |
| 8. Is the device suitable for use with military populations? | No, unlikely | This device has potential to be used with military populations, although this has not been assessed. | Yes very suitable for military populations. |

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© Crown copyright (2020), Defence Science and Technology Laborato-ry (Dstl). This materialis licensed under the terms of the Open Gov-ernment Licence except where otherwise stated.To view this li-cence, visit: http://www.nationalarchives.gov.uk/doc/open-government-licence/version/3).
Share and Cite
Hinde, K.; White, G.; Armstrong, N. Wearable Devices Suitable for Monitoring Twenty Four Hour Heart Rate Variability in Military Populations. Sensors 2021, 21, 1061. https://doi.org/10.3390/s21041061
Hinde K, White G, Armstrong N. Wearable Devices Suitable for Monitoring Twenty Four Hour Heart Rate Variability in Military Populations. Sensors. 2021; 21(4):1061. https://doi.org/10.3390/s21041061
Chicago/Turabian StyleHinde, Katrina, Graham White, and Nicola Armstrong. 2021. "Wearable Devices Suitable for Monitoring Twenty Four Hour Heart Rate Variability in Military Populations" Sensors 21, no. 4: 1061. https://doi.org/10.3390/s21041061
APA StyleHinde, K., White, G., & Armstrong, N. (2021). Wearable Devices Suitable for Monitoring Twenty Four Hour Heart Rate Variability in Military Populations. Sensors, 21(4), 1061. https://doi.org/10.3390/s21041061





