Leap Motion Controller Video Game-Based Therapy for Upper Extremity Motor Recovery in Patients with Central Nervous System Diseases. A Systematic Review with Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Protocol Review
2.2. Search Strategy and Data Sources
2.3. Study Selection and Inclusion Criteria
2.4. Data Extraction
2.5. Outcomes
2.6. Assessment of Evidence Quality and Risk of Bias
2.7. Statistical Analysis
2.8. Additional Analysis
3. Results
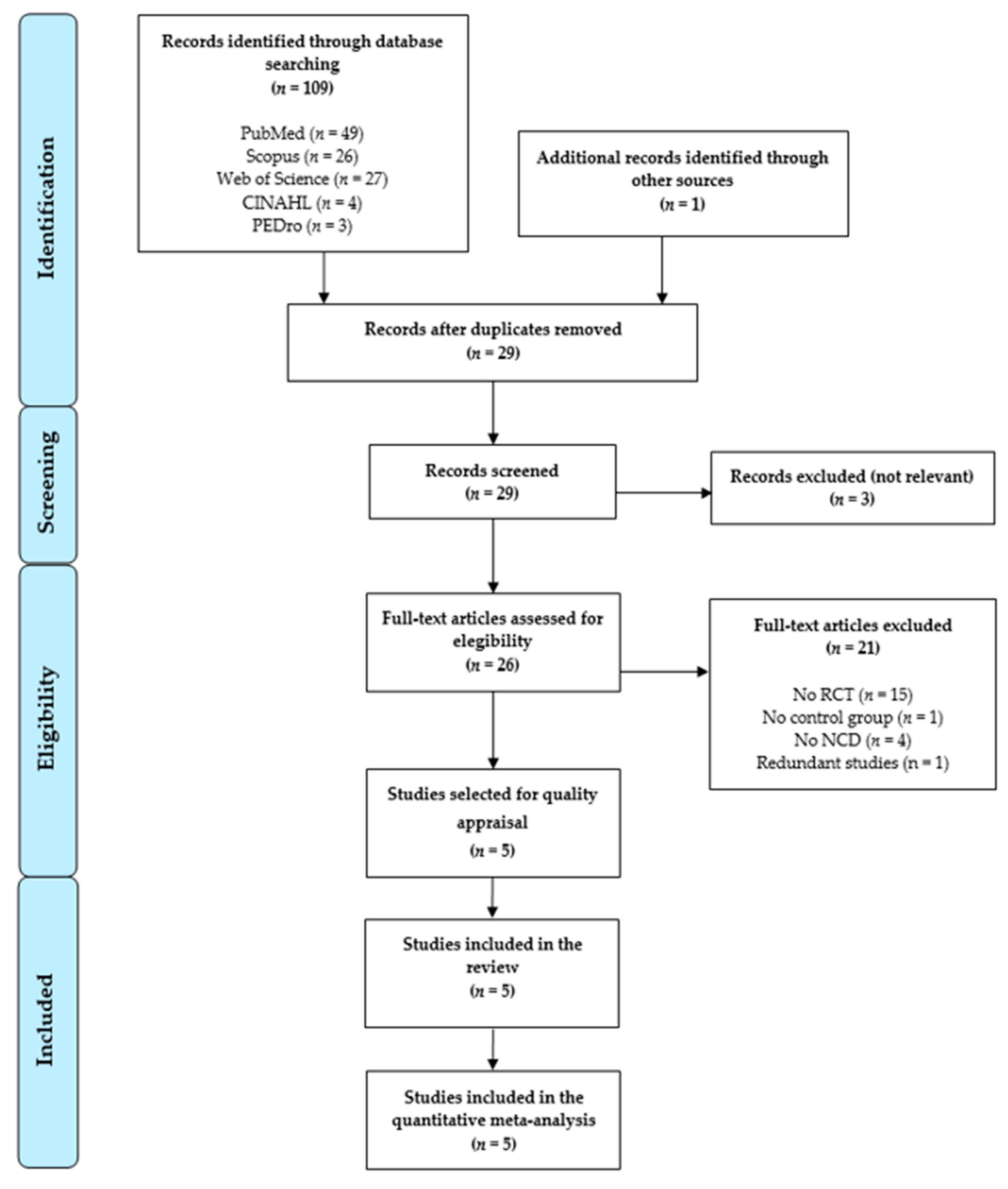
3.1. Study Selection
3.2. Main Characteristics of the Studies Included in the Review
3.3. Risk of Bias Assessment
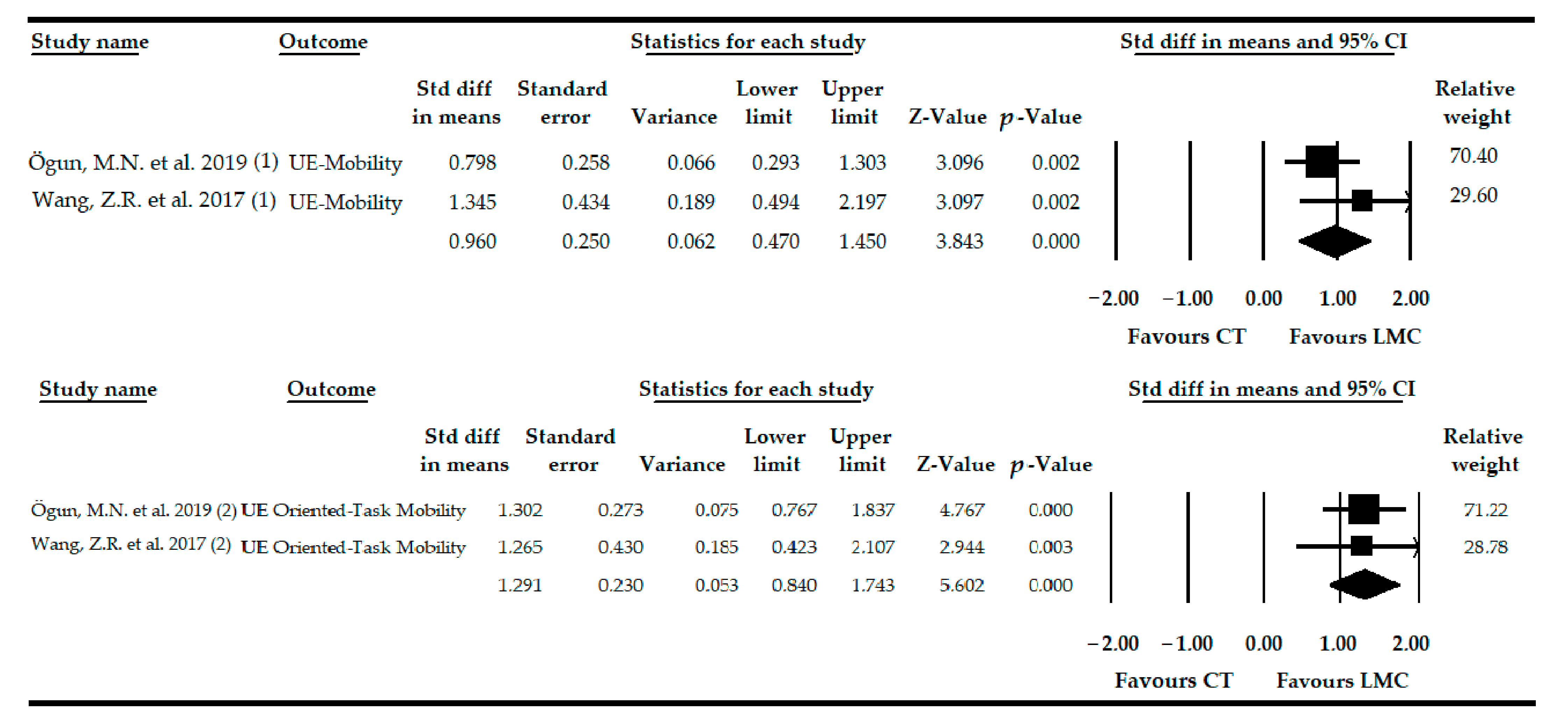
3.4. Effect of LMC-Video Game Based Therapy on the Recovery of UE Mobility in Patients with Stroke
3.5. Effect of LMC-Video Game Based Therapy to Restore the UE Mobility-Oriented Task in Patients with Stroke
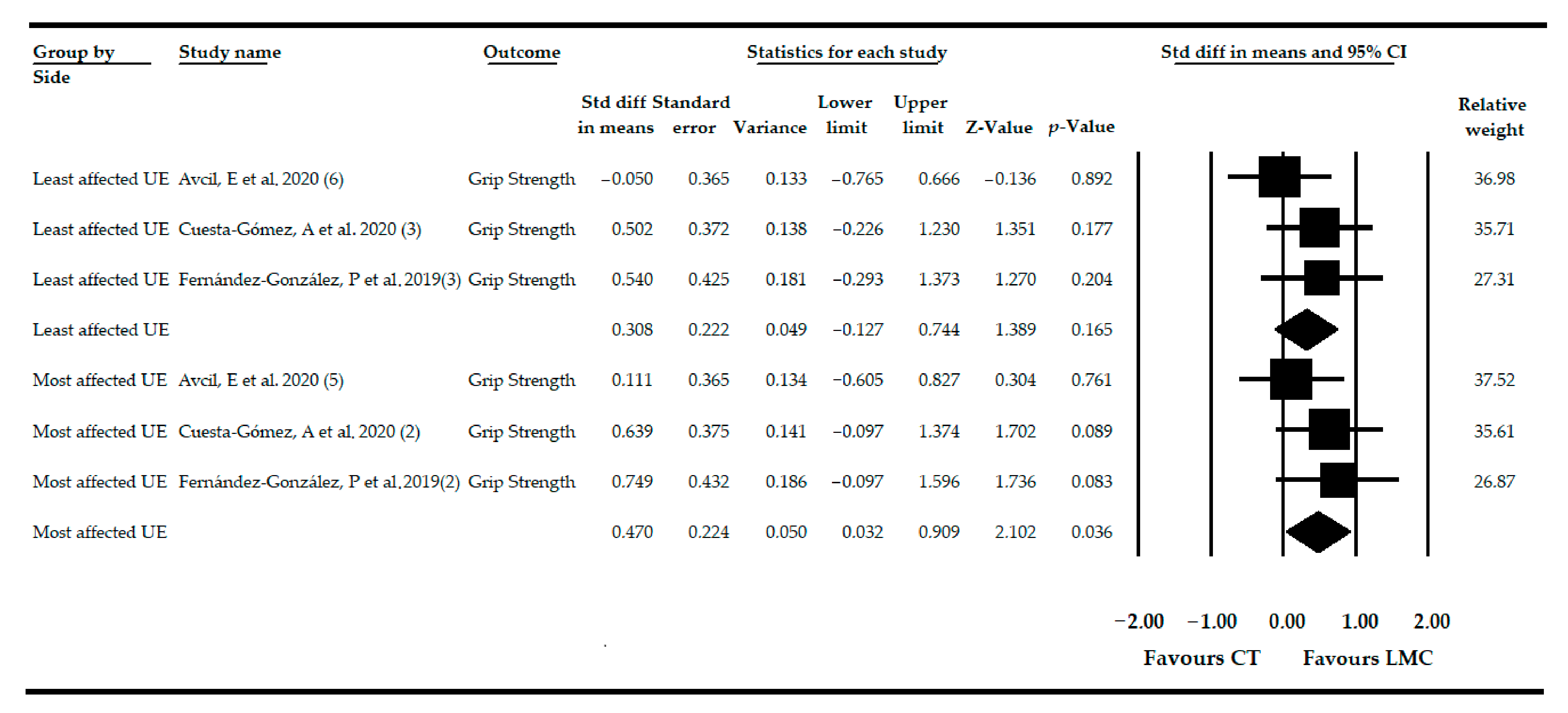
3.6. Effect of LMC-Video Game Based Therapy on Grip Strength in Non-Acute CNSDs
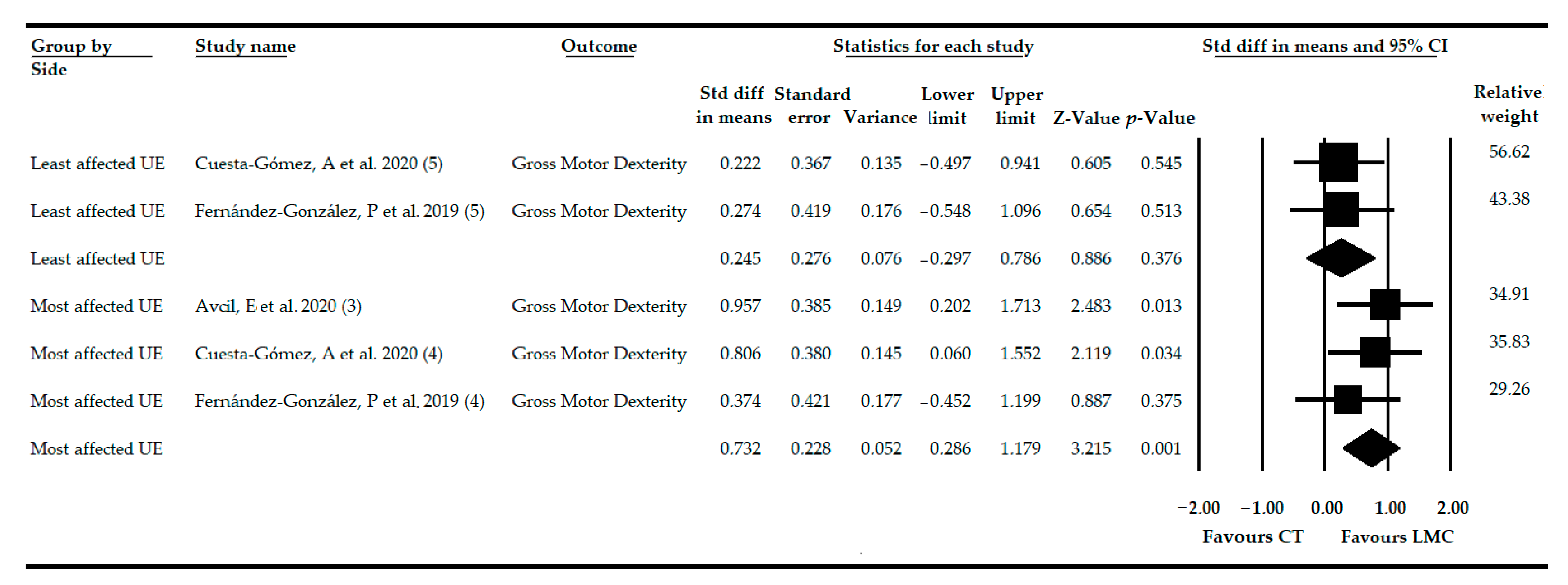
3.7. Effect of LMC-Video Game Based Therapy on Gross Motor Dexterity in Non-Acute CNSD
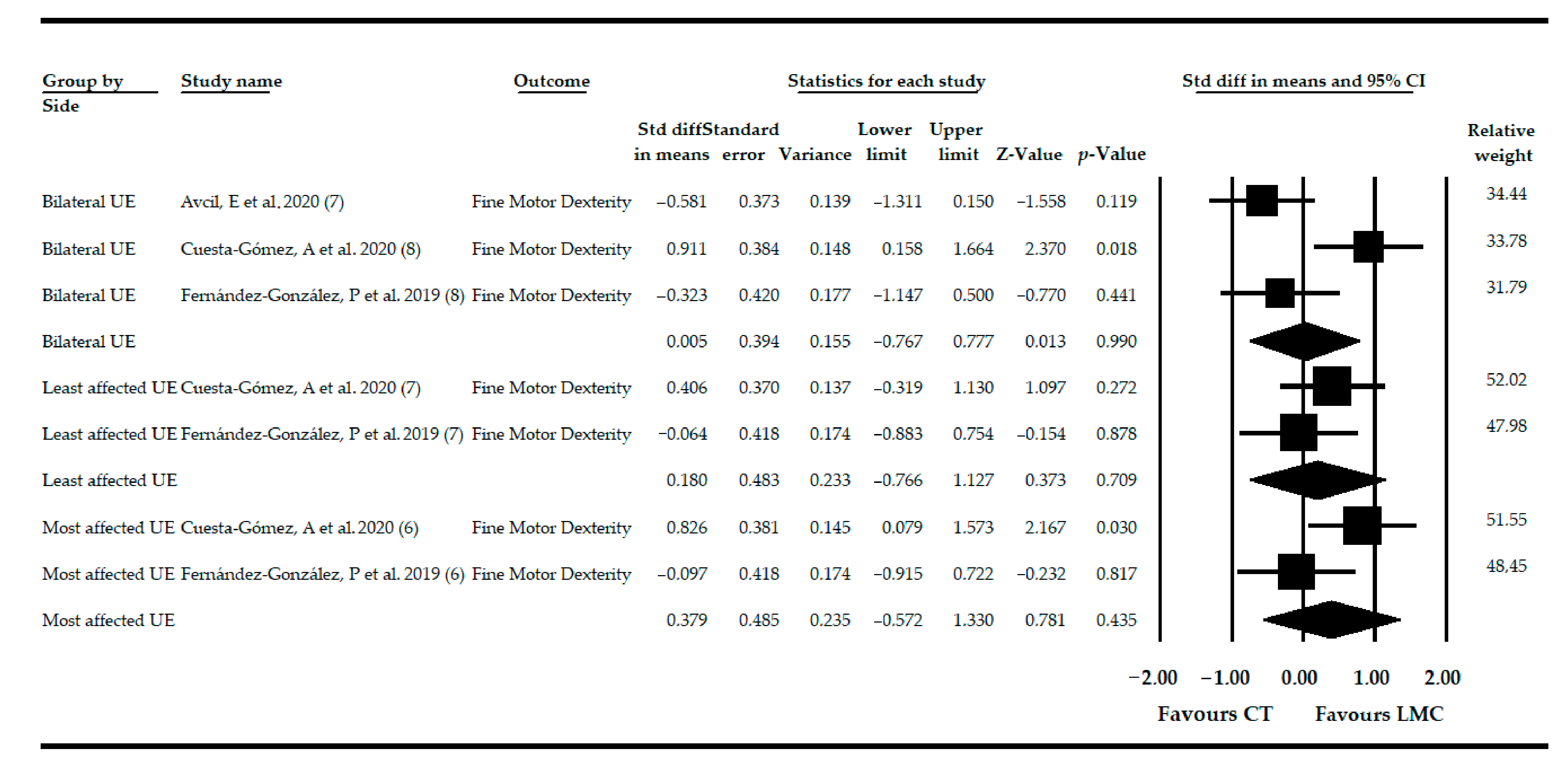
3.8. Effect of LMC-Video Game Based Therapy on Fine Motor Dexterity in Non-Acute CNSD
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Del Pozo-Cruz, B.; Adsuar, J.C.; Parraca, J.A.; del Pozo-Cruz, J.; Olivares, P.R.; Gusi, N. Using Whole-Body Vibration Training in Patients Affected with Common Neurological Diseases: A Systematic Literature Review. J. Altern. Complement. Med. 2012, 18, 29–41. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murphy, S.J.; Werring, D.J. Stroke: Causes and clinical features. Medicine 2020, 48, 561–566. [Google Scholar] [CrossRef] [PubMed]
- Rosenbaum, P.; Paneth, N.; Leviton, A.; Goldstein, M.; Bax, M. A report: The definition and classification of cerebral palsy April 2006. Dev. Med. Child Neurol. 2007, 49, 8–14. [Google Scholar]
- Gautam, R.; Sharma, M. Prevalence and Diagnosis of Neurological Disorders Using Different Deep Learning Techniques: A Meta-Analysis. J. Med. Syst. 2020, 44, 49. [Google Scholar] [CrossRef]
- Baek, K.; Doñamayor, N.; Morris, L.S.; Strelchuk, D.; Mitchell, S.; Mikheenko, Y.; Yeoh, S.Y.; Phillips, W.; Zandi, M.; Jenaway, A.; et al. Impaired awareness of motor intention in functional neurological disorder: Implications for voluntary and functional movement. Psychol. Med. 2017, 47, 1624–1636. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nonnekes, J.; Goselink, R.J.M.; Růžička, E.; Fasano, A.; Nutt, J.G.; Bloem, B.R. Neurological disorders of gait, balance and posture: A sign-based approach. Nat. Rev. Neurol. 2018, 14, 183–189. [Google Scholar] [CrossRef]
- Zhu, W.; Jiang, Y. Determinants of quality of life in patients with hemorrhagic stroke: A path analysis. Medicine 2019, 98, e13928. [Google Scholar] [CrossRef] [PubMed]
- Schallert, W.; Fluet, M.-C.; Kesselring, J.; Kool, J. Evaluation of upper limb function with digitizing tablet-based tests: Reliability and discriminative validity in healthy persons and patients with neurological disorders. Disabil. Rehabil. 2020, 1–9. [Google Scholar] [CrossRef]
- Bakers, J.N.E.; van den Berg, L.H.; Ajeks, T.G.; Holleman, M.J.; Verhoeven, J.; Beelen, A.; Visser-Meily, J.M.A.; van Eijk, R.P.A. Portable fixed dynamometry: Towards remote muscle strength measurements in patients with motor neuron disease. J. Neurol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Bohannon, R. Muscle strength and muscle training after stroke. J. Rehabil. Med. 2007, 39, 14–20. [Google Scholar] [CrossRef] [Green Version]
- Auld, M.L.; Boyd, R.N.; Moseley, G.L.; Ware, R.S.; Johnston, L.M. Impact of Tactile Dysfunction on Upper-Limb Motor Performance in Children with Unilateral Cerebral Palsy. Arch. Phys. Med. Rehabil. 2012, 93, 696–702. [Google Scholar] [CrossRef] [PubMed]
- Carlsson, H.; Gard, G.; Brogårdh, C. Upper-limb sensory impairments after stroke: Self-reported experiences of daily life and rehabilitation. J. Rehabil. Med. 2018, 50, 45–51. [Google Scholar] [CrossRef] [Green Version]
- Ballantyne, R.; Rea, P.M. A Game Changer: The Use of Digital Technologies in the Management of Upper Limb Rehabilitation; Springer: Cham, Switzerland, 2019; pp. 117–147. [Google Scholar]
- Pomeroy, V.; Aglioti, S.M.; Mark, V.W.; McFarland, D.; Stinear, C.; Wolf, S.L.; Corbetta, M.; Fitzpatrick, S.M. Neurological Principles and Rehabilitation of Action Disorders. Neurorehabil. Neural Repair 2011, 25, 33S–43S. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Levac, D.; Glegg, S.; Colquhoun, H.; Miller, P.; Noubary, F. Virtual Reality and Active Videogame-Based Practice, Learning Needs, and Preferences: A Cross-Canada Survey of Physical Therapists and Occupational Therapists. Games Health J. 2017, 6, 217–228. [Google Scholar] [CrossRef]
- Turolla, A.; Venneri, A.; Farina, D.; Cagnin, A.; Cheung, V.C.K. Rehabilitation Induced Neural Plasticity after Acquired Brain Injury. Neural Plast. 2018, 2018, 1–3. [Google Scholar] [CrossRef] [Green Version]
- da Silva Ribeiro, N.M.; Ferraz, D.D.; Pedreira, É.; Pinheiro, Í.; da Silva Pinto, A.C.; Neto, M.G.; dos Santos, L.R.A.; Pozzato, M.G.G.; Pinho, R.S.; Masruha, M.R. Virtual rehabilitation via Nintendo Wii® and conventional physical therapy effectively treat post-stroke hemiparetic patients. Top. Stroke Rehabil. 2015, 22, 299–305. [Google Scholar] [CrossRef] [PubMed]
- Barreca, S.; Wolf, S.L.; Fasoli, S.; Bohannon, R. Treatment Interventions for the Paretic Upper Limb of Stroke Survivors: A Critical Review. Neurorehabil. Neural Repair 2003, 17, 220–226. [Google Scholar] [CrossRef]
- Jakob, I.; Kollreider, A.; Germanotta, M.; Benetti, F.; Cruciani, A.; Padua, L.; Aprile, I. Robotic and Sensor Technology for Upper Limb Rehabilitation. PM R 2018, 10, S189–S197. [Google Scholar] [CrossRef] [Green Version]
- Levin, M.F.; Weiss, P.L.; Keshner, E.A. Emergence of Virtual Reality as a Tool for Upper Limb Rehabilitation: Incorporation of Motor Control and Motor Learning Principles. Phys. Ther. 2015, 95, 415–425. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Massetti, T.; da Silva, T.D.; Crocetta, T.B.; Guarnieri, R.; de Freitas, B.L.; Bianchi Lopes, P.; Watson, S.; Tonks, J.; de Mello Monteiro, C.B. The Clinical Utility of Virtual Reality in Neurorehabilitation: A Systematic Review. J. Cent. Nerv. Syst. Dis. 2018, 10, 117957351881354. [Google Scholar] [CrossRef] [PubMed]
- Ventura, S.; Brivio, E.; Riva, G.; Baños, R.M. Immersive Versus Non-immersive Experience: Exploring the Feasibility of Memory Assessment through 360° Technology. Front. Psychol. 2019, 10. [Google Scholar] [CrossRef] [PubMed]
- Gatica-Rojas, V.; Méndez-Rebolledo, G. Virtual reality interface devices in the reorganization of neural networks in the brain of patients with neurological diseases. Neural Regen. Res. 2014, 9, 888. [Google Scholar] [CrossRef]
- Kim, W.-S.; Cho, S.; Park, S.H.; Lee, J.-Y.; Kwon, S.; Paik, N.-J. A low cost kinect-based virtual rehabilitation system for inpatient rehabilitation of the upper limb in patients with subacute stroke. Medicine 2018, 97, e11173. [Google Scholar] [CrossRef] [PubMed]
- Turolla, A.; Dam, M.; Ventura, L.; Tonin, P.; Agostini, M.; Zucconi, C.; Kiper, P.; Cagnin, A.; Piron, L. Virtual reality for the rehabilitation of the upper limb motor function after stroke: A prospective controlled trial. J. Neuroeng. Rehabil. 2013, 10, 85. [Google Scholar] [CrossRef] [PubMed]
- Kim, W.-S.; Cho, S.; Ku, J.; Kim, Y.; Lee, K.; Hwang, H.-J.; Paik, N.-J. Clinical Application of Virtual Reality for Upper Limb Motor Rehabilitation in Stroke: Review of Technologies and Clinical Evidence. J. Clin. Med. 2020, 9, 3369. [Google Scholar] [CrossRef]
- Miclaus, R.; Roman, N.; Caloian, S.; Mitoiu, B.; Suciu, O.; Onofrei, R.R.; Pavel, E.; Neculau, A. Non-Immersive Virtual Reality for Post-Stroke Upper Extremity Rehabilitation: A Small Cohort Randomized Trial. Brain Sci. 2020, 10, 655. [Google Scholar] [CrossRef]
- Wu, J.; Loprinzi, P.D.; Ren, Z. The Rehabilitative Effects of Virtual Reality Games on Balance Performance among Children with Cerebral Palsy: A Meta-Analysis of Randomized Controlled Trials. Int. J. Environ. Res. Public Health 2019, 16, 4161. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Norouzi, E.; Gerber, M.; Pühse, U.; Vaezmosavi, M.; Brand, S. Combined virtual reality and physical training improved the bimanual coordination of women with multiple sclerosis. Neuropsychol. Rehabil. 2020, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Santos, P.; Machado, T.; Santos, L.; Ribeiro, N.; Melo, A. Efficacy of the Nintendo Wii combination with Conventional Exercises in the rehabilitation of individuals with Parkinson’s disease: A randomized clinical trial. NeuroRehabilitation 2019, 45, 255–263. [Google Scholar] [CrossRef]
- Leemhuis, E.; Esposito, R.M.; De Gennaro, L.; Pazzaglia, M. Go Virtual to Get Real: Virtual Reality as a Resource for Spinal Cord Treatment. Int. J. Environ. Res. Public Health 2021, 18, 1819. [Google Scholar] [CrossRef]
- Vanbellingen, T.; Filius, S.J.; Nyffeler, T.; van Wegen, E.E.H. Usability of Videogame-Based Dexterity Training in the Early Rehabilitation Phase of Stroke Patients: A Pilot Study. Front. Neurol. 2017, 8. [Google Scholar] [CrossRef] [Green Version]
- Khademi, M.; Mousavi Hondori, H.; McKenzie, A.; Dodakian, L.; Lopes, C.V.; Cramer, S.C. Free-hand interaction with leap motion controller for stroke rehabilitation. In Proceedings of the CHI ’14 Extended Abstracts on Human Factors in Computing Systems; ACM: New York, NY, USA, 2014; pp. 1663–1668. [Google Scholar]
- Niechwiej-Szwedo, E.; Gonzalez, D.; Nouredanesh, M.; Tung, J. Evaluation of the Leap Motion Controller during the performance of visually-guided upper limb movements. PLoS ONE 2018, 13, e0193639. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oña, E.D.; Balaguer, C.; Cano-de la Cuerda, R.; Collado-Vázquez, S.; Jardón, A. Effectiveness of Serious Games for Leap Motion on the Functionality of the Upper Limb in Parkinson’s Disease: A Feasibility Study. Comput. Intell. Neurosci. 2018, 2018, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Bachmann, D.; Weichert, F.; Rinkenauer, G. Review of Three-Dimensional Human-Computer Interaction with Focus on the Leap Motion Controller. Sensors 2018, 18, 2194. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jiang, X.; Xu, W.; Sweeney, L.; Li, Y.; Gross, R.; Yurovsky, D. New directions in contact free hand recognition. In Proceedings of the 2007 IEEE International Conference on Image Processing, San Antonio, TX, USA, 16 September–19 October 2007; Volume 2, pp. 389–392. [Google Scholar]
- Han, J.; Gold, N.E. Lessons Learned in Exploring the Leap MotionTM Sensor for Gesture-Based Instrument Design; Goldsmiths University of London: London, UK, 2014. [Google Scholar]
- Skals, S.; Rasmussen, K.P.; Bendtsen, K.M.; Yang, J.; Andersen, M.S. A musculoskeletal model driven by dual Microsoft Kinect Sensor data. Multibody Syst. Dyn. 2017, 41, 297–316. [Google Scholar] [CrossRef] [Green Version]
- Bachmann, D.; Weichert, F.; Rinkenauer, G. Evaluation of the leap motion controller as a new contact-free pointing device. Sensors 2014, 15, 214–233. [Google Scholar] [CrossRef] [Green Version]
- Cikajlo, I.; Peterlin Potisk, K. Advantages of using 3D virtual reality based training in persons with Parkinson’s disease: A parallel study. J. Neuroeng. Rehabil. 2019, 16, 119. [Google Scholar] [CrossRef] [Green Version]
- Kim, S.; Park, S.; Lee, O. Development of a Diagnosis and Evaluation System for Hemiplegic Patients Post-Stroke Based on Motion Recognition Tracking and Analysis of Wrist Joint Kinematics. Sensors 2020, 20, 4548. [Google Scholar] [CrossRef]
- Ferreira, S.C.; Chaves, R.O.; Seruffo, M.C.d.R.; Pereira, A.; Azar, A.P.D.S.; Dias, Â.V.; Dos Santos, A.D.A.S.; Brito, M.V.H. Empirical Evaluation of a 3D Virtual Simulator of Hysteroscopy Using Leap Motion for Gestural Interfacing. J. Med. Syst. 2020, 44, 198. [Google Scholar] [CrossRef]
- Nizamis, K.; Rijken, N.; Mendes, A.; Janssen, M.; Bergsma, A.; Koopman, B. A Novel Setup and Protocol to Measure the Range of Motion of the Wrist and the Hand. Sensors 2018, 18, 3230. [Google Scholar] [CrossRef] [Green Version]
- Weichert, F.; Bachmann, D.; Rudak, B.; Fisseler, D. Analysis of the Accuracy and Robustness of the Leap Motion Controller. Sensors 2013, 13, 6380–6393. [Google Scholar] [CrossRef] [Green Version]
- Smeragliuolo, A.H.; Hill, N.J.; Disla, L.; Putrino, D. Validation of the Leap Motion Controller using markered motion capture technology. J. Biomech. 2016, 49, 1742–1750. [Google Scholar] [CrossRef]
- Chophuk, P.; Chumpen, S.; Tungjitkusolmun, S.; Phasukkit, P. Hand postures for evaluating trigger finger using leap motion controller. In Proceedings of the BMEiCON 2015—8th Biomedical Engineering International Conference, Pattaya, Thailand, 25–27 November 2015. [Google Scholar]
- Fonk, R.; Schneeweiss, S.; Simon, U.; Engelhardt, L. Hand Motion Capture from a 3D Leap Motion Controller for a Musculoskeletal Dynamic Simulation. Sensors 2021, 21, 1199. [Google Scholar] [CrossRef] [PubMed]
- Gamboa, E.; Serrato, A.; Castro, J.; Toro, D.; Trujillo, M. Advantages and Limitations of Leap Motion from a Developers’, Physical Therapists’, and Patients’ Perspective. Methods Inf. Med. 2020, 59, 110–116. [Google Scholar] [CrossRef]
- Iosa, M.; Morone, G.; Fusco, A.; Castagnoli, M.; Fusco, F.R.; Pratesi, L.; Paolucci, S. Leap motion controlled videogame-based therapy for rehabilitation of elderly patients with subacute stroke: A feasibility pilot study. Top. Stroke Rehabil. 2015, 22, 306–316. [Google Scholar] [CrossRef] [PubMed]
- Johnson, L.; Bird, M.-L.; Muthalib, M.; Teo, W.-P. An Innovative STRoke Interactive Virtual thErapy (STRIVE) Online Platform for Community-Dwelling Stroke Survivors: A Randomized Controlled Trial. Arch. Phys. Med. Rehabil. 2020, 101, 1131–1137. [Google Scholar] [CrossRef] [PubMed]
- Schuster-Amft, C.; Eng, K.; Suica, Z.; Thaler, I.; Signer, S.; Lehmann, I.; Schmid, L.; McCaskey, M.A.; Hawkins, M.; Verra, M.L.; et al. Effect of a four-week virtual reality-based training versus conventional therapy on upper limb motor function after stroke: A multicenter parallel group randomized trial. PLoS ONE 2018, 13, e0204455. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chiu, H.-C.; Ada, L.; Lee, H.-M. Upper limb training using Wii Sports Resort TM for children with hemiplegic cerebral palsy: A randomized, single-blind trial. Clin. Rehabil. 2014, 28, 1015–1024. [Google Scholar] [CrossRef]
- Karamians, R.; Proffitt, R.; Kline, D.; Gauthier, L.V. Effectiveness of Virtual Reality- and Gaming-Based Interventions for Upper Extremity Rehabilitation Poststroke: A Meta-analysis. Arch. Phys. Med. Rehabil. 2020, 101, 885–896. [Google Scholar] [CrossRef]
- Domínguez-Téllez, P.; Moral-Muñoz, J.A.; Salazar, A.; Casado-Fernández, E.; Lucena-Antón, D. Game-Based Virtual Reality Interventions to Improve Upper Limb Motor Function and Quality of Life After Stroke: Systematic Review and Meta-analysis. Games Health J. 2020, 9, 1–10. [Google Scholar] [CrossRef]
- Webster, A.; Poyade, M.; Rooney, S.; Paul, L. Upper limb rehabilitation interventions using virtual reality for people with multiple sclerosis: A systematic review. Mult. Scler. Relat. Disord. 2021, 47, 102610. [Google Scholar] [CrossRef] [PubMed]
- Tarakci, E.; Arman, N.; Tarakci, D.; Kasapcopur, O. Leap Motion Controller–based training for upper extremity rehabilitation in children and adolescents with physical disabilities: A randomized controlled trial. J. Hand Ther. 2019. [Google Scholar] [CrossRef]
- Karashanov, A.; Manolova, A.; Neshov, N. Application for hand rehabilitation using Leap Motion Sensor based on a gamification approach. Int. J. Adv. Res. Sci. Eng. 2016, 5, 61–69. [Google Scholar]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. J. Clin. Epidemiol. 2009, 62, 1006–1012. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Green, S. Cochrane Handbook for Systematic Reviews of Intervention Version 5.1.0 [Updated March 2011]; The Cochrane Collaboration: London, UK, 2011. [Google Scholar]
- Obrero-Gaitán, E.; Osuna-Pérez, M.C.; Zagalaz-Anula, N.; Cortés-Pérez, I.; Montor-Cárdenas, D. Leap Motion Controller Video Game Based Therapy for Upper Limb Rehabilitation in Patients with Neurological Disorders. A Systematic Review with Meta-analysis. PROSPERO 2020 CRD42020200771. Available online: https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=200771 (accessed on 6 February 2021).
- Hozo, S.P.; Djulbegovic, B.; Hozo, I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med. Res. Methodol. 2005, 5, 13. [Google Scholar] [CrossRef] [Green Version]
- Atkins, D.; Best, D.; Briss, P.A.; Eccles, M.; Falck-Ytter, Y.; Flottorp, S.; Guyatt, G.H.; Harbour, R.T. Grading quality of evidence and strength of recommendations. BMJ 2004, 328, 1490. [Google Scholar] [CrossRef] [Green Version]
- Meader, N.; King, K.; Llewellyn, A.; Norman, G.; Brown, J.; Rodgers, M.; Moe-Byrne, T.; Higgins, J.P.; Sowden, A.; Stewart, G. A checklist designed to aid consistency and reproducibility of GRADE assessments: Development and pilot validation. Syst. Rev. 2014, 3, 82. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Altman, D.G.; Gotzsche, P.C.; Juni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.C. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [Green Version]
- Higgins, J.P.T.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [Green Version]
- Borenstein, M.; Hedges, L.; Higgins, J.; Rothstein, H. Comprehensive Meta-Analysis Software Version 3. Available online: https://www.meta-analysis.com/ (accessed on 1 February 2021).
- Cooper, H.; Hedges, L.V.; Valentine, J.C. The Handbook of Research Synthesis and Meta-Analysis; Russell Sage Foundation: New York, NY, USA, 2009. [Google Scholar]
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials. Control. Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Cohen, J Statistical Power Analysis for the Behavioral Sciences; Academic Press: New York, NY, USA, 1977.
- Faraone, S.V. Interpreting estimates of treatment effects: Implications for managed care. P T 2008, 33, 700–711. [Google Scholar]
- Rücker, G.; Schwarzer, G. Beyond the forest plot: The drapery plot. Res. Synth. Methods 2020. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Egger, M. Funnel plots for detecting bias in meta-analysis: Guidelines on choice of axis. J. Clin. Epidemiol. 2001, 54, 1046–1055. [Google Scholar] [CrossRef]
- Egger, M.; Smith, G.D.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test measures of funnel plot asymmetry. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef] [Green Version]
- Higgins, J.; Thompson, S.; Deeks, J.; Altman, D. Statistical heterogeneity in systematic reviews of clinical trials: A critical appraisal of guidelines and practice. J. Heal. Serv. Res. Policy 2002, 7, 51–61. [Google Scholar] [CrossRef] [PubMed]
- Avcil, E.; Tarakci, D.; Arman, N.; Tarakci, E. Upper extremity rehabilitation using video games in cerebral palsy: A randomized clinical trial. Acta Neurol. Belg. 2020. [Google Scholar] [CrossRef]
- Cuesta-Gómez, A.; Sánchez-Herrera-Baeza, P.; Oña-Simbaña, E.D.; Martínez-Medina, A.; Ortiz-Comino, C.; Balaguer-Bernaldo-de-Quirós, C.; Jardón-Huete, A.; Cano-de-la-Cuerda, R. Effects of virtual reality associated with serious games for upper limb rehabilitation in patients with multiple sclerosis: Randomized controlled trial. J. Neuroeng. Rehabil. 2020, 17, 90. [Google Scholar] [CrossRef]
- Fernández-González, P.; Carratalá-Tejada, M.; Monge-Pereira, E.; Collado-Vázquez, S.; Sánchez-Herrera Baeza, P.; Cuesta-Gómez, A.; Oña-Simbaña, E.D.; Jardón-Huete, A.; Molina-Rueda, F.; Balaguer-Bernaldo de Quirós, C.; et al. Leap motion controlled video game-based therapy for upper limb rehabilitation in patients with Parkinson’s disease: A feasibility study. J. Neuroeng. Rehabil. 2019, 16, 133. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Wang, P.; Xing, L.; Mei, L.; Zhao, J.; Zhang, T. Leap Motion-based virtual reality training for improving motor functional recovery of upper limbs and neural reorganization in subacute stroke patients. Neural Regen. Res. 2017, 12, 1823. [Google Scholar] [CrossRef] [PubMed]
- Ögün, M.N.; Kurul, R.; Yasar, M.F.; Turkoglu, S.A.; Avci, Ş.; Yildiz, N. Effect of Leap Motion-based 3D Immersive Virtual Reality Usage on Upper Extremity Function in Ischemic Stroke Patients. Arq. Neuropsiquiatr. 2019, 77, 681–688. [Google Scholar] [CrossRef] [Green Version]
- Pilla, A.; Trigili, E.; McKinney, Z.; Fanciullacci, C.; Malasoma, C.; Posteraro, F.; Crea, S.; Vitiello, N. Robotic Rehabilitation and Multimodal Instrumented Assessment of Post-stroke Elbow Motor Functions—A Randomized Controlled Trial Protocol. Front. Neurol. 2020, 11. [Google Scholar] [CrossRef]
- Manuli, A.; Maggio, M.G.; Tripoli, D.; Gullì, M.; Cannavò, A.; La Rosa, G.; Sciarrone, F.; Avena, G.; Calabrò, R.S. Patients’ perspective and usability of innovation technology in a new rehabilitation pathway: An exploratory study in patients with multiple sclerosis. Mult. Scler. Relat. Disord. 2020, 44, 102312. [Google Scholar] [CrossRef]
- Bai, Z.; Fong, K.N.K.; Zhang, J.J.; Chan, J.; Ting, K.H. Immediate and long-term effects of BCI-based rehabilitation of the upper extremity after stroke: A systematic review and meta-analysis. J. Neuroeng. Rehabil. 2020, 17, 57. [Google Scholar] [CrossRef]
- Viglialoro, R.M.; Condino, S.; Turini, G.; Mamone, V.; Carbone, M.; Ferrari, V.; Ghelarducci, G.; Ferrari, M.; Gesi, M. Interactive serious game for shoulder rehabilitation based on real-time hand tracking. Technol. Health Care 2020, 28, 403–414. [Google Scholar] [CrossRef] [PubMed]
- Gotz, M.; Jarriault, S. Programming and reprogramming the brain: A meeting of minds in neural fate. Development 2017, 144, 2714–2718. [Google Scholar] [CrossRef] [Green Version]
- Voss, P.; Thomas, M.E.; Cisneros-Franco, J.M.; de Villers-Sidani, E. Dynamic Brains and the Changing Rules of Neuroplasticity: Implications for Learning and Recovery. Front. Psychol. 2017, 8, 1657. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hara, Y. Brain plasticity and rehabilitation in stroke patients. J. Nippon Med. Sch. 2015, 82, 4–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lindmark, A.; Norrving, B.; Eriksson, M. Socioeconomic status and survival after stroke—Using mediation and sensitivity analyses to assess the effect of stroke severity and unmeasured confounding. BMC Public Health 2020, 20, 554. [Google Scholar] [CrossRef]
- Langhorne, P.; Coupar, F.; Pollock, A. Motor recovery after stroke: A systematic review. Lancet Neurol. 2009, 8, 741–754. [Google Scholar] [CrossRef]
- Sommerfeld, D.K.; Eek, E.U.-B.; Svensson, A.-K.; Holmqvist, L.W.; von Arbin, M.H. Spasticity After Stroke. Stroke 2004, 35, 134–139. [Google Scholar] [CrossRef] [Green Version]
- Bressi, F.; Bravi, M.; Campagnola, B.; Bruno, D.; Marzolla, A.; Santacaterina, F.; Miccinilli, S.; Sterzi, S. Robotic treatment of the upper limb in chronic stroke and cerebral neuroplasticity: A systematic review. J. Biol. Regul. Homeost. Agents 2020, 34, 11–44. [Google Scholar] [PubMed]
- Lee, H.-S.; Lim, J.-H.; Jeon, B.-H.; Song, C.-S. Non-immersive Virtual Reality Rehabilitation Applied to a Task-oriented Approach for Stroke Patients: A Randomized Controlled Trial. Restor. Neurol. Neurosci. 2020. [Google Scholar] [CrossRef] [PubMed]
- Keller, J.; Štětkářová, I.; Macri, V.; Kühn, S.; Pětioký, J.; Gualeni, S.; Simmons, C.D.; Arthanat, S.; Zilber, P. Virtual reality-based treatment for regaining upper extremity function induces cortex grey matter changes in persons with acquired brain injury. J. Neuroeng. Rehabil. 2020, 17, 127. [Google Scholar] [CrossRef] [PubMed]
- Long, Y.; Ouyang, R.; Zhang, J. Effects of virtual reality training on occupational performance and self-efficacy of patients with stroke: A randomized controlled trial. J. Neuroeng. Rehabil. 2020, 17, 150. [Google Scholar] [CrossRef]
- García Muñoz, C.; Casuso Holgado, M.J. Efectividad de la Wii Fit Balance frente a otras intervenciones para la recuperación del equilibrio en pacientes postictus. Revisión sistemática y metaanálisis. Rev. Neurol. 2019, 69, 271. [Google Scholar] [CrossRef] [PubMed]
- Saposnik, G.; Cohen, L.G.; Mamdani, M.; Pooyania, S.; Ploughman, M.; Cheung, D.; Shaw, J.; Hall, J.; Nord, P.; Dukelow, S.; et al. Efficacy and safety of non-immersive virtual reality exercising in stroke rehabilitation (EVREST): A randomised, multicentre, single-blind, controlled trial. Lancet Neurol. 2016, 15, 1019–1027. [Google Scholar] [CrossRef] [Green Version]
- Laver, K.E.; Lange, B.; George, S.; Deutsch, J.E.; Saposnik, G.; Crotty, M. Virtual reality for stroke rehabilitation. Cochrane database Syst. Rev. 2017, 11, CD008349. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Psychouli, P.; Katzis, K.; Elliott, M. Home-Based Training Support for Stroke Patients Using the Leap Motion and StandInExercise Stand. Stud. Health Technol. Inform. 2018, 251, 55–58. [Google Scholar]
- Bostanci, H.; Emir, A.; Tarakci, D.; Tarakci, E. Video game-based therapy for the non-dominant hand improves manual skills and grip strength. Hand Surg. Rehabil. 2020, 39, 265–269. [Google Scholar] [CrossRef]
- Clutterbuck, G.; Auld, M.; Johnston, L. Active exercise interventions improve gross motor function of ambulant/semi-ambulant children with cerebral palsy: A systematic review. Disabil. Rehabil. 2019, 41, 1131–1151. [Google Scholar] [CrossRef]
- Jonsdottir, J.; Bertoni, R.; Lawo, M.; Montesano, A.; Bowman, T.; Gabrielli, S. Serious games for arm rehabilitation of persons with multiple sclerosis. A randomized controlled pilot study. Mult. Scler. Relat. Disord. 2018, 19, 25–29. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Şahin, S.; Köse, B.; Aran, O.T.; Bahadır Ağce, Z.; Kayıhan, H. The Effects of Virtual Reality on Motor Functions and Daily Life Activities in Unilateral Spastic Cerebral Palsy: A Single-Blind Randomized Controlled Trial. Games Health J. 2020, 9, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Rathinam, C.; Mohan, V.; Peirson, J.; Skinner, J.; Nethaji, K.S.; Kuhn, I. Effectiveness of virtual reality in the treatment of hand function in children with cerebral palsy: A systematic review. J. Hand Ther. 2019, 32, 426–434.e1. [Google Scholar] [CrossRef]
- Liu, X.; Zhu, Y.; Huo, H.; Wei, P.; Wang, L.; Sun, A.; Hu, C.; Yin, X.; Lv, Z.; Fan, Y. Design of Virtual Guiding Tasks With Haptic Feedback for Assessing the Wrist Motor Function of Patients With Upper Motor Neuron Lesions. IEEE Trans. Neural Syst. Rehabil. Eng. 2019, 27, 984–994. [Google Scholar] [CrossRef]
- McCall, J.V.; Ludovice, M.C.; Blaylock, J.A.; Kamper, D.G. A Platform for Rehabilitation of Finger Individuation in Children with Hemiplegic Cerebral Palsy. In Proceedings of the 2019 IEEE 16th International Conference on Rehabilitation Robotics (ICORR), Toronto, ON, Canada, 24–28 June 2019; pp. 343–348. [Google Scholar]
- Guna, J.; Jakus, G.; Pogačnik, M.; Tomažič, S.; Sodnik, J. An Analysis of the Precision and Reliability of the Leap Motion Sensor and Its Suitability for Static and Dynamic Tracking. Sensors 2014, 14, 3702–3720. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, H.S.; Park, Y.J.; Park, S.W. The Effects of Virtual Reality Training on Function in Chronic Stroke Patients: A Systematic Review and Meta-Analysis. Biomed Res. Int. 2019, 2019, 1–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johansen, T.; Strøm, V.; Simic, J.; Rike, P. Effectiveness of training with motion-controlled commercial video games for hand and arm function in people with cerebral palsy: A systematic review and meta-analysis. J. Rehabil. Med. 2020, 52, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Yeamkuan, S.; Chamnongthai, K. 3D Point-of-Intention Determination Using a Multimodal Fusion of Hand Pointing and Eye Gaze for a 3D Display. Sensors 2021, 21, 1155. [Google Scholar] [CrossRef]
| DATABASE | SEARCH STRATEGY |
|---|---|
| PubMed Medline | (“leap motion”[tiab] OR “leap motion controller”[tiab] OR leap motion sensor[tiab] OR LMC[tiab]) AND (upper extremity[mh] OR upper extremity[tiab] OR upper limb[tiab]) |
| Web of Science | (*leap motion controller*) AND (*upper extremity* OR *upper limb*) |
| Scopus | [TITLE-ABS-KEY (“leap motion controller”) AND (“upper limb” OR “upper extremity”)] |
| PEDro | Leap motion AND upper limb |
| CINAHL | (AB leap motion OR AB leap motion controller) AND (AB upper extremity OR AB upper limb) |
| EXPERIMENTAL GROUP | COMPARISON GROUP | OUTCOMES | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sample | Intervention | Sample | Control | |||||||||||||||||||
| Author and Year | Country | K | N | ND | Evol (years) | Ne | Age | M:F | Type | Weeks | Ses/ Week | Min | Nc | Age | M:F | Type | Weeks | Ses/ Week | Min | Type | Test | Time |
| Avcil, E et al. (2020) [76] | Turkey | 4 | 30 | Cerebral Palsy | NR | 15 | 10.93 | 8:7 | LMC + NWT | 8 | 3 | 60 | 15 | 11.07 | 9:6 | CT | 8 | 3 | 60 | GS | Dynamometer | Immediate |
| GMD | MMDT | |||||||||||||||||||||
| FMD | DHI | |||||||||||||||||||||
| Cuesta-Gómez, A. et al. (2020) [77] | Spain | 7 | 30 | Multiple Sclerosis | 15.20 | 16 | 49.86 | 7:9 | LMC + CT | 10 | 2 | 60 | 14 | 42.66 | 5:9 | CT | 10 | 2 | 60 | GS | Dynamometer | Immediate |
| GMD | BBT | |||||||||||||||||||||
| FMD | PPT | |||||||||||||||||||||
| Fernández-González, P. et al. (2019) [78] | Spain | 7 | 23 | Parkinson Disease | NR | 12 | 65.77 | 6:6 | LMC | 6 | 2 | 30 | 11 | 73.63 | 5:6 | CT | 6 | 2 | 30 | GP | Dynamometer | Immediate |
| GMD | BBT | |||||||||||||||||||||
| FMD | PPT | |||||||||||||||||||||
| Wang, Z. et al. (2017) [79] | China | 2 | 26 | Stroke | 0.13 | 13 | 55.3 | 11:2 | LMC + OT | 4 | 5 | 45 | 13 | 53.4 | 11:2 | CT | 4 | 5 | 45 | UE motor function | FM-UE | Immediate |
| ARAT | ||||||||||||||||||||||
| Ögün, M.N. et al. (2019) [80] | Turkey | 2 | 65 | Stroke | 0.28 | 33 | 61.48 | 28:5 | LMC | 6 | 3 | 60 | 32 | 59.75 | 23:9 | CT +Pas VR | 6 | 3 | 60 | UE motor function | WMFT | Immediate |
| Selection Bias | Performance Bias | Detection Bias | Attrition Bias | Reporting Bias | Other Bias | ||
|---|---|---|---|---|---|---|---|
| Author and Year | Random Sequence Generation | Concealment of Randomization Sequence | Blinding of Participants | Blinding of Outcomes Assessors | Incomplete Outcome Data | Selective Reporting | Other, Ideally Prespecified |
| Avcil, E. et al. (2020) [76] | - | + | + | ? | - | - | - |
| Cuesta-Gómez, A. et al. (2020) [77] | - | + | + | - | - | - | - |
| Fernández-González, P. et al. (2019) [78] | - | + | + | + | - | - | - |
| Wang, Z. et al. (2017) [79] | - | + | + | - | - | - | - |
| Ögün, M.N. et al. (2019) [80] | - | + | + | - | - | - | - |
| Summary of Findings | Quality of Evidence (GRADE) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pooled Effect Het | Publication Bias | ||||||||||||||
| K | N | Ns | SMD | 95% CI | I2 (p-Value) | (Egger p-Value) | Trim and Fill | Risk of Bias | Incons | Indirect | Imprec | Pub. Bias | Quality | ||
| Adj SMD | % of Var | ||||||||||||||
| STROKE | |||||||||||||||
| Overall UE Mobility | 2 | 91 | 45.5 | 0.96 | 0.47; 1.45 | 0% (0.31) | - | - | - | Medium | No | No | Yes | Likely | Very low |
| Overall UE Oriented-Task Mobility | 2 | 91 | 45.5 | 1.29 | 0.84; 1.74 | 0% (0.94) | - | - | - | Medium | No | No | Yes | Likely | Very low |
| NON-ACUTE CNSD (CP, MS, and PD) | |||||||||||||||
| GRIP STRENGTH | |||||||||||||||
| Overall Most Affected UE | 3 | 83 | 27.6 | 0.47 | 0.03; 0.90 | 0% (0.45) | 0.49 | 0.47 | 0% | Medium | No | No | Yes | Low | Low |
| Overall Least Affected UE | 3 | 83 | 27.6 | 0.30 | −0.12; 0.74 | 0% (0.46) | 0.58 | 0.30 | 0% | Medium | No | No | Yes | Low | Low |
| GROSS MOTOR DEXTERITY | |||||||||||||||
| Overall Most Affected UE | 3 | 83 | 27.6 | 0.73 | 0.28; 1.17 | 0% (0.57) | 0.24 | 0.73 | 0% | Medium | No | No | Yes | Low | Low |
| Overall Least Affected UE | 2 | 53 | 26.5 | 0.24 | −0.29; 0.78 | 0% (0.92) | - | - | - | Medium | No | No | Yes | Likely | Very low |
| FINE MOTOR DEXTERITY | |||||||||||||||
| Overall Most Affected UE | 2 | 53 | 26.5 | 0.37 | −0.57; 1.33 | 0% (0.31) | - | - | - | Medium | No | No | Yes | Likely | Very low |
| Overall Least Affected UE | 2 | 53 | 26.5 | 0.18 | −0.77; 1.12 | 0% (0.39) | - | - | - | Medium | No | No | Yes | Likely | Very low |
| Overall Bilateral UE | 3 | 83 | 27.6 | 0.01 | −0.76; 0.77 | 0% (0.38) | 0.95 | <0.01 | 0% | Medium | No | No | Yes | Low | Low |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cortés-Pérez, I.; Zagalaz-Anula, N.; Montoro-Cárdenas, D.; Lomas-Vega, R.; Obrero-Gaitán, E.; Osuna-Pérez, M.C. Leap Motion Controller Video Game-Based Therapy for Upper Extremity Motor Recovery in Patients with Central Nervous System Diseases. A Systematic Review with Meta-Analysis. Sensors 2021, 21, 2065. https://doi.org/10.3390/s21062065
Cortés-Pérez I, Zagalaz-Anula N, Montoro-Cárdenas D, Lomas-Vega R, Obrero-Gaitán E, Osuna-Pérez MC. Leap Motion Controller Video Game-Based Therapy for Upper Extremity Motor Recovery in Patients with Central Nervous System Diseases. A Systematic Review with Meta-Analysis. Sensors. 2021; 21(6):2065. https://doi.org/10.3390/s21062065
Chicago/Turabian StyleCortés-Pérez, Irene, Noelia Zagalaz-Anula, Desirée Montoro-Cárdenas, Rafael Lomas-Vega, Esteban Obrero-Gaitán, and María Catalina Osuna-Pérez. 2021. "Leap Motion Controller Video Game-Based Therapy for Upper Extremity Motor Recovery in Patients with Central Nervous System Diseases. A Systematic Review with Meta-Analysis" Sensors 21, no. 6: 2065. https://doi.org/10.3390/s21062065
APA StyleCortés-Pérez, I., Zagalaz-Anula, N., Montoro-Cárdenas, D., Lomas-Vega, R., Obrero-Gaitán, E., & Osuna-Pérez, M. C. (2021). Leap Motion Controller Video Game-Based Therapy for Upper Extremity Motor Recovery in Patients with Central Nervous System Diseases. A Systematic Review with Meta-Analysis. Sensors, 21(6), 2065. https://doi.org/10.3390/s21062065











