Validity and Reliability of a Smartphone App for Gait and Balance Assessment
Abstract
:1. Introduction
2. Methods
2.1. Participants
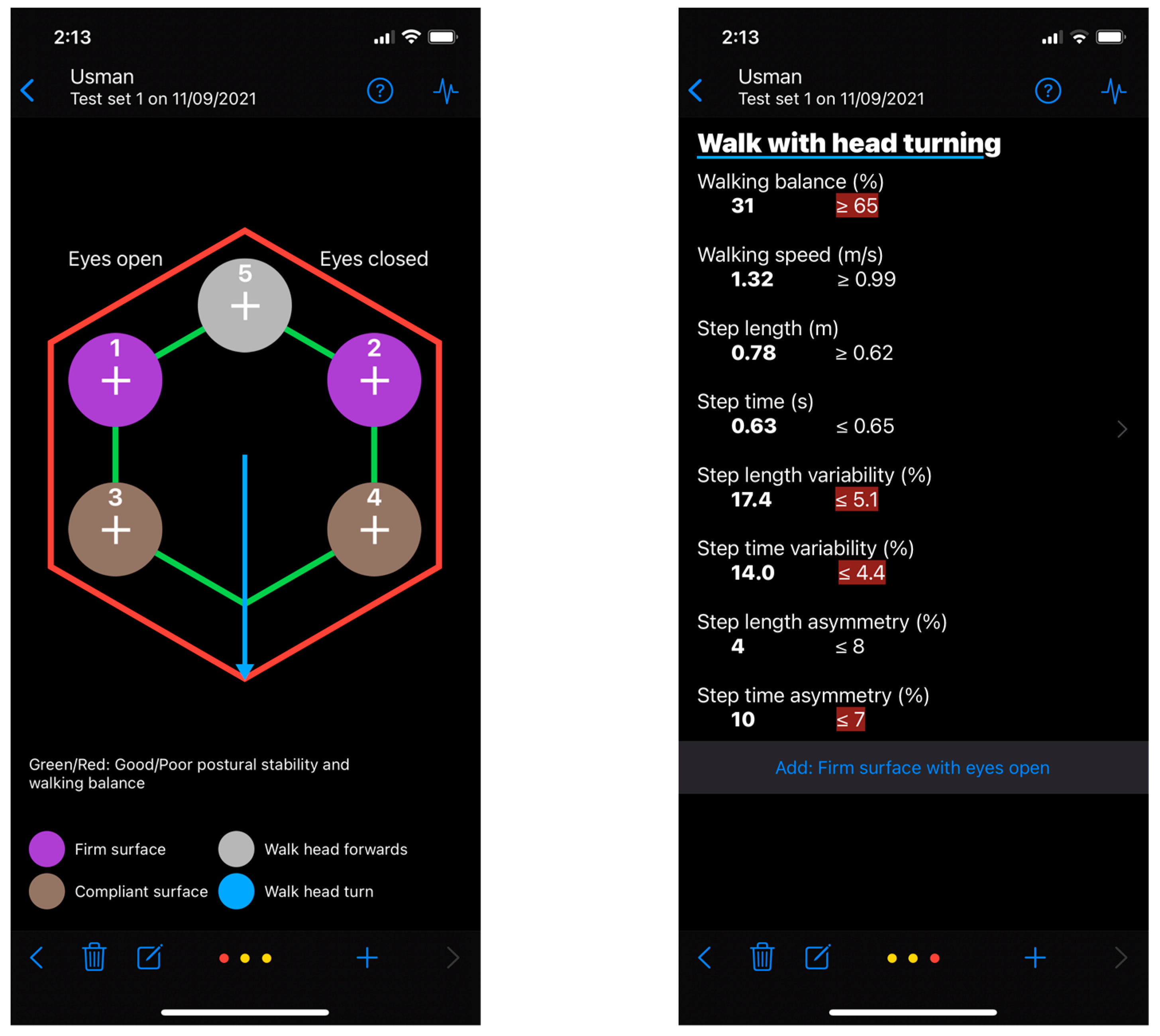
2.2. The Gait&Balance App
2.3. Experimental Procedure
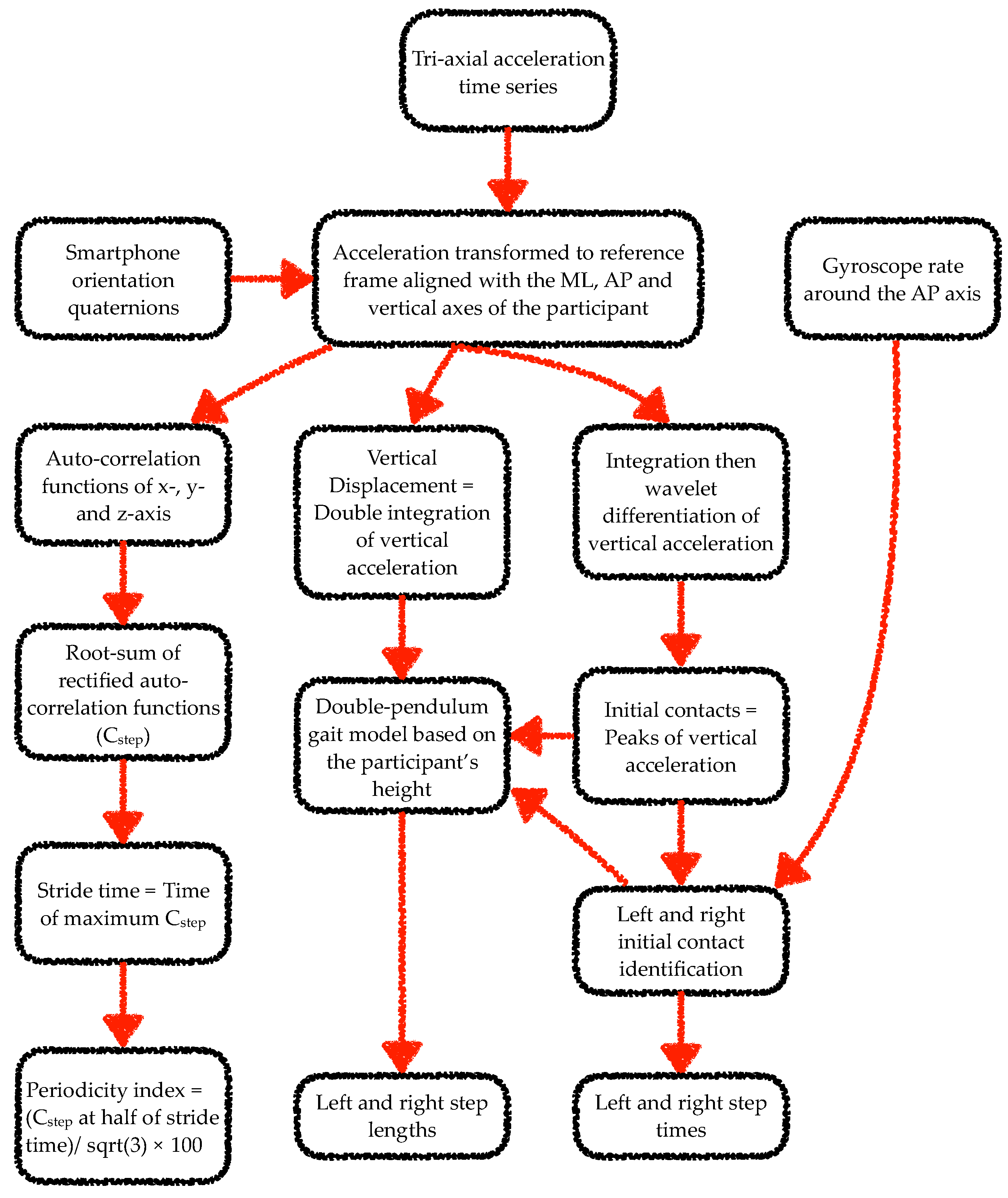
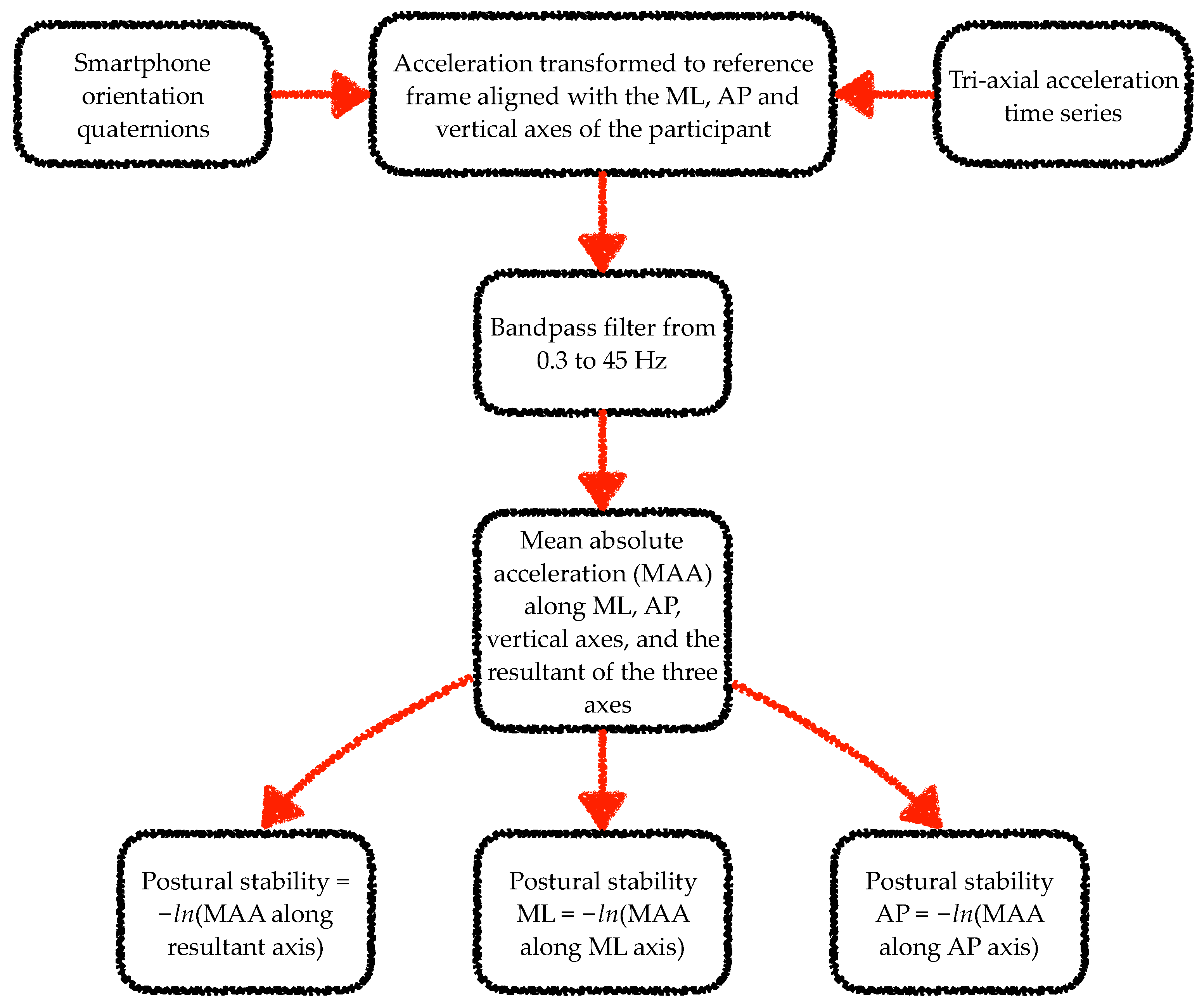
2.4. Data Processing
2.5. Gait and Balance Outcomes
- (a)
- Periodicity index (also known as gait symmetry index [44]; units: %)
- This parameter was computed from the root-sum of rectified auto-correlation functions of the tri-axial acceleration signals (Cstep) at half stride time. Stride time was computed by dividing the index of the maximum value of Cstep by the sample rate. Periodicity was quantified as a percentage of the maximum possible value of Cstep (). Low periodicity scores may indicate step asymmetry and/or a high variability across strides. For the 3D MoCap system, the displacement signal was first numerically differentiated twice to obtain acceleration. A wavelet-based differentiation algorithm was used to avoid the amplification of high-frequency noise caused by numerical differentiation [50]. Periodicity was calculated for each 6-s walking trial, and its mean value across the trials was estimated by taking the median of the four individual trial values. Median was used as the best estimator for mean in the presence of data skew resulting from a potential algorithm or signal anomaly [51]. This outcome encompassed the step symmetry between the right and left step within a stride and the gait regularity across strides.
- (b)
- Average step length (SLAv, units: m)
- This parameter was computed as the mean of the AP distance between two consecutive initial contacts of alternative feet. For the 3D MoCap system, step lengths were calculated based on the AP distance between contralateral ankle markers. The final score was estimated by taking the median of all the step lengths from the four laps.
- (c)
- Average step time (STAv, units: s)
- This parameter was computed as the mean of the time between two consecutive initial contacts of alternative feet.
- (d)
- Step length variability (SLVr, units: %)
- Step length variability was calculated as the root mean square of the SD of left step lengths and the SD of right step lengths and expressed as the mean step length percentage. The SD of left/right step length was estimated as times the interquartile range (IQR) of all the left/right step lengths collated from the four 6-s trials. IQR was used as the best estimator for SD to account for data skew resulting from a potential algorithm or signal anomaly [51].
- (e)
- Step time variability (STVr, units: %)
- Step time variability was calculated as the root mean square of the SD of left step times and the SD of right step times and expressed as the mean step time percentage.
- (f)
- Step length asymmetry (SLAs, units: %)
- This parameter was computed as the percentage difference between left and right mean step lengths compared to the overall mean step length.
- (g)
- Step time asymmetry (STAs, units: %)
- This parameter was computed as the percentage difference between left and right mean step times compared to the overall mean step time.
- (h)
- Walking speed (WS, units: m/s)
- (a)
- Postural stability (PS, units: −ln[m/s2])
- Postural stability was computed as the negative natural logarithm of the mean of the absolute acceleration along mediolateral, anterior–posterior, and vertical axes resultant vector. Postural stability was also computed separately for the mediolateral (PSML) and the anterior–posterior axis (PSAP). As the negative natural logarithm was taken, high postural stability scores meant a low centre of mass accelerations and, thus, a good balance performance. For the 3D MoCap system, acceleration time series were constructed from displacement signals by double differentiation. A wavelet-based differentiation method was used to reduce the amplification of the sensor noise caused by numerical differentiation [50]. This parameter evaluated the participants’ stability through the analysis of the smartphone acceleration as an index of the participants’ centre of mass acceleration.
2.6. Statistical Analyses
2.6.1. Validity of Gait and Balance Outcomes
2.6.2. Reliability and Responsiveness of Gait and Balance Outcomes
2.6.3. Assumptions, Data Presentation and Interpretation
3. Results
3.1. Validity of Gait and Balance Outcomes
3.2. Reliability and Responsiveness of Gait and Balance Outcomes
4. Discussion
4.1. Validity of Gait and Balance Outcomes Obtained from the Smartphone Application
4.2. Reliability of Gait and Balance Outcomes Obtained from the Smartphone Application
4.3. Clinical Implications
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Agrawal, Y.; Carey, J.P.; Della Santina, C.C.; Schubert, M.C.; Minor, L.B. Disorders of balance and vestibular function in US adults: Data from the National Health and Nutrition Examination Survey, 2001–2004. Arch. Intern. Med. 2009, 169, 938–944. [Google Scholar] [CrossRef] [PubMed]
- Mendel, B.; Bergenius, J.; Langius, A. Dizziness symptom severity and impact on daily living as perceived by patients suffering from peripheral vestibular disorder. Clin. Otolaryngol. 1999, 24, 286–293. [Google Scholar] [CrossRef]
- Schlick, C.; Schniepp, R.; Loidl, V.; Wuehr, M.; Hesselbarth, K.; Jahn, K. Falls and fear of falling in vertigo and balance disorders: A controlled cross-sectional study. J. Vestib. Res. 2016, 25, 241–251. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mira, E. Improving the quality of life in patients with vestibular disorders: The role of medical treatments and physical reha-bilitation. Int. J. Clin. Pract. 2008, 62, 109–114. [Google Scholar] [CrossRef] [PubMed]
- Guidetti, G. Posturography in vestibular work-up of the patient. A review. Acta Oto-Rhino-Laryngol. Belg. 1992, 46, 45–51. [Google Scholar]
- Prosperini, L.; Fortuna, D.; Giannì, C.; Leonardi, L.; Pozzilli, C. The Diagnostic Accuracy of Static Posturography in Predicting Accidental Falls in People with Multiple Sclerosis. Neurorehabilit. Neural Repair 2012, 27, 45–52. [Google Scholar] [CrossRef]
- Prosperini, L.; Pozzilli, C. The Clinical Relevance of Force Platform Measures in Multiple Sclerosis: A Review. Mult. Scler. Int. 2013, 2013, 756564 . [Google Scholar] [CrossRef] [Green Version]
- Kim, S.D.; Allen, N.E.; Canning, C.G.; Fung, V.S.C. Postural Instability in Patients with Parkinson’s Disease. CNS Drugs 2012, 27, 97–112. [Google Scholar] [CrossRef]
- An, M.; Shaughnessy, M. The effects of exercise-based rehabilitation on balance and gait for stroke patients: A systematic review. J. Neurosci. Nurs. 2011, 43, 298–307. [Google Scholar] [CrossRef] [Green Version]
- Piirtola, M.; Era, P. Force Platform Measurements as Predictors of Falls among Older People—A Review. Gerontology 2006, 52, 1–16. [Google Scholar] [CrossRef]
- Marchetti, G.F.; Lin, C.-C.; Alghadir, A.; Whitney, S.L. Responsiveness and Minimal Detectable Change of the Dynamic Gait Index and Functional Gait Index in Persons with Balance and Vestibular Disorders. J. Neurol. Phys. Ther. 2014, 38, 119–124. [Google Scholar] [CrossRef]
- Cohen, H.S.; Kimball, K.T. Usefulness of some current balance tests for identifying individuals with disequilibrium due to vestibular impairments. J. Vestib. Res. 2009, 18, 295–303. [Google Scholar] [CrossRef]
- Wrisley, D.M.; Marchetti, G.F.; Kuharsky, D.K.; Whitney, S.L. Reliability, Internal Consistency, and Validity of Data Obtained with the Functional Gait Assessment. Phys. Ther. 2004, 84, 906–918. [Google Scholar] [CrossRef] [Green Version]
- Tanji, H.; Gruber-Baldini, A.L.; Anderson, K.E.; Pretzer-Aboff, I.; Reich, S.G.; Fishman, P.S.; Weiner, W.J.; Shulman, L.M. A comparative study of physical performance measures in Parkinson's disease. Mov. Disord. 2008, 23, 1897–1905. [Google Scholar] [CrossRef]
- Boulgarides, L.K.; McGinty, S.M.; A Willett, J.; Barnes, C.W. Use of Clinical and Impairment-Based Tests to Predict Falls by Community-Dwelling Older Adults. Phys. Ther. 2003, 83, 328–339. [Google Scholar] [CrossRef]
- Blum, L.; Korner-Bitensky, N. Usefulness of the Berg Balance Scale in Stroke Rehabilitation: A Systematic Review. Phys. Ther. 2008, 88, 559–566. [Google Scholar] [CrossRef]
- Baert, I.; Smedal, T.; Kalron, A.; Rasova, K.; Heric-Mansrud, A.; Ehling, R.; Minguez, I.E.; Nedeljkovic, U.; Tacchino, A.; Hellinckx, P.; et al. Responsiveness and meaningful improvement of mobility measures following MS rehabilitation. Neurology 2018, 91, e1880–e1892. [Google Scholar] [CrossRef]
- Hasegawa, N.; Shah, V.V.; Harker, G.; Carlson-Kuhta, P.; Nutt, J.G.; Lapidus, J.A.; Jung, S.H.; Barlow, N.; King, L.A.; Horak, F.B. Responsiveness of Objective vs. Clinical Balance Domain Outcomes for Exercise Intervention in Parkinson’s Disease. Front. Neurol. 2020, 11, 940. [Google Scholar] [CrossRef]
- Del Rosario, M.B.; Redmond, S.J.; Lovell, N.H. Tracking the Evolution of Smartphone Sensing for Monitoring Human Movement. Sensors 2015, 15, 18901–18933. [Google Scholar] [CrossRef] [Green Version]
- Kosse, N.M.; Caljouw, S.R.; Vervoort, D.; Vuillerme, N.; Lamoth, C. Validity and Reliability of Gait and Postural Control Analysis Using the Tri-axial Accelerometer of the iPod Touch. Ann. Biomed. Eng. 2014, 43, 1935–1946. [Google Scholar] [CrossRef]
- Chiu, Y.-L.; Tsai, Y.-J.; Lin, C.-H.; Hou, Y.-R.; Sung, W.-H. Evaluation of a smartphone-based assessment system in subjects with chronic ankle instability. Comput. Methods Programs Biomed. 2016, 139, 191–195. [Google Scholar] [CrossRef]
- Han, S.; Lee, D.; Lee, S. A study on the reliability of measuring dynamic balance ability using a smartphone. J. Phys. Ther. Sci. 2016, 28, 2515–2518. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arcuria, G.; Marcotulli, C.; Amuso, R.; Dattilo, G.; Galasso, C.; Pierelli, F.; Casali, C. Developing a smartphone application, triaxial accelerometer-based, to quantify static and dynamic balance deficits in patients with cerebellar ataxias. J. Neurol. 2019, 267, 625–639. [Google Scholar] [CrossRef]
- Hou, Y.-R.; Chiu, Y.-L.; Chiang, S.-L.; Chen, H.-Y.; Sung, W.-H. Development of a Smartphone-Based Balance Assessment System for Subjects with Stroke. Sensors 2019, 20, 88. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pacini Panebianco, G.; Bisi, M.C.; Stagni, R.; Fantozzi, S. Analysis of the performance of 17 algorithms from a systematic review: Influence of sensor position, analysed variable and computational approach in gait timing estimation from IMU measurements. Gait Posture 2018, 66, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Godfrey, A.; Del Din, S.; Barry, G.; Mathers, J.; Rochester, L. Instrumenting gait with an accelerometer: A system and algorithm examination. Med Eng. Phys. 2015, 37, 400–407. [Google Scholar] [CrossRef] [PubMed]
- Amick, R.Z.; Chaparro, A.; Patterson, J.A. Test-Retest Reliability of the sway Balance Mobile Application. J. Mob. Technol. Med. 2015, 4, 40–47. [Google Scholar] [CrossRef] [Green Version]
- Jeremy, A.P.; Amick, R.Z.; Thummar, T.; Rogers, M.E. Validation of measures from the smartphone sway balance application: A pilot study. Int. J. Sports Phys. Ther. 2014, 9, 135. [Google Scholar]
- Pinho, A.S.; Salazar, A.P.; Hennig, E.M.; Spessato, B.C.; Domingo, A.; Pagnussat, A.S. Can We Rely on Mobile Devices and Other Gadgets to Assess the Postural Balance of Healthy Individuals? A Systematic Review. Sensors 2019, 19, 2972. [Google Scholar] [CrossRef] [Green Version]
- Yvon, C.; Najuko-Mafemera, A.; Kanegaonkar, R. The D+R Balance application: A novel method of assessing postural sway. J. Laryngol. Otol. 2015, 129, 773–778. [Google Scholar] [CrossRef] [Green Version]
- Mancini, M.; King, L.; Salarian, A.; Holmstrom, L.; McNames, J.; Horak, F.B. Mobility Lab to Assess Balance and Gait with Synchronized Body-worn Sensors. J Bioeng Biomed Sci. 2011, 1, 7. [Google Scholar] [CrossRef]
- Manor, B.; Yu, W.; Zhu, H.; Harrison, R.; Lo, O.Y.; Lipsitz, L.; Travison, T.; Pascual-Leone, A.; Zhou, J. Smartphone App-Based Assessment of Gait During Normal and Dual-Task Walking: Demonstration of Validity and Reliability. JMIR Mhealth Uhealth 2018, 6, e36. [Google Scholar] [CrossRef]
- Nishiguchi, S.; Yamada, M.; Nagai, K.; Mori, S.; Kajiwara, Y.; Sonoda, T.; Yoshimura, K.; Yoshitomi, H.; Ito, H.; Okamoto, K.; et al. Reliability and validity of gait analysis by android-based smartphone. Telemed J E Health 2012, 18, 292–296. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Silsupadol, P.; Teja, K.; Lugade, V. Reliability and validity of a smartphone-based assessment of gait parameters across walking speed and smartphone locations: Body, bag, belt, hand, and pocket. Gait Posture 2017, 58, 516–522. [Google Scholar] [CrossRef] [PubMed]
- Zhong, R.; Rau, P.-L.P. A Mobile Phone–Based Gait Assessment App for the Elderly: Development and Evaluation. JMIR Mhealth Uhealth 2020, 8, e14453. [Google Scholar] [CrossRef]
- Ford-Smith, C.D.; Wyman, J.F.; Elswick, R.; Fernandez, T.; Newton, R.A. Test-retest reliability of the sensory organization test in noninstitutionalized older adults. Arch. Phys. Med. Rehabil. 1995, 76, 77–81. [Google Scholar] [CrossRef]
- Wrisley, D.M.; Whitney, S.L. The effect of foot position on the modified clinical test of sensory interaction and balance. Arch. Phys. Med. Rehabil. 2004, 85, 335–338. [Google Scholar] [CrossRef]
- Moe-Nilssen, R.; Helbostad, J.L. Trunk accelerometry as a measure of balance control during quiet standing. Gait Posture 2001, 16, 60–68. [Google Scholar] [CrossRef]
- Shumway-Cook, A.; Horak, F.B. Assessing the influence of sensory interaction on balance: Suggestion from the field. Phys. Ther. 1986, 66, 1548–1550. [Google Scholar] [CrossRef]
- Cohen, H.S.; Mulavara, A.P.; Peters, B.T.; Sangi-Haghpeykar, H.; Bloomberg, J.J. Standing balance tests for screening people with vestibular impairments. Laryngoscope 2013, 124, 545–550. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McCamley, J.; Donati, M.; Grimpampi, E.; Mazzà, C. An enhanced estimate of initial contact and final contact instants of time using lower trunk inertial sensor data. Gait Posture 2012, 36, 316–318. [Google Scholar] [CrossRef] [PubMed]
- Trojaniello, D.; Ravaschio, A.; Hausdorff, J.M.; Cereatti, A. Comparative assessment of different methods for the estimation of gait temporal parameters using a single inertial sensor: Application to elderly, post-stroke, Parkinson's disease and Huntington's disease subjects. Gait Posture 2015, 42, 310–316. [Google Scholar] [CrossRef]
- Zhao, Q.; Zhang, B.; Wang, J.; Feng, W.; Jia, W.; Sun, M. Improved method of step length estimation based on inverted pendulum model. Int. J. Distrib. Sens. Netw. 2017, 13. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Smuck, M.; Legault, C.; Ith, M.A.; Muaremi, A.; Aminian, K. Gait Symmetry Assessment with a Low Back 3D Accelerometer in Post-Stroke Patients. Sensors 2018, 18, 3322. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Del Din, S.; Hickey, A.; Ladha, C.; Stuart, S.; Bourke, A.K.; Esser, P.; Rochester, L.; Godfrey, A.; Stuart, S. Instrumented gait assessment with a single wearable: An introductory tutorial. F1000Research 2016, 5, 2323. [Google Scholar] [CrossRef] [Green Version]
- Martinez-Mendez, R.; Sekine, M.; Tamura, T. Postural sway parameters using a triaxial accelerometer: Comparing elderly and young healthy adults. Comput. Methods Biomech. Biomed. Eng. 2012, 15, 899–910. [Google Scholar] [CrossRef] [PubMed]
- Saunders, N.W.; Koutakis, P.; Kloos, A.D.; Kegelmeyer, D.A.; Dicke, J.D.; Devor, S.T. Reliability and Validity of a Wireless Accelerometer for the Assessment of Postural Sway. J. Appl. Biomech. 2015, 31, 159–163. [Google Scholar] [CrossRef]
- O’Connor, C.M.; Thorpe, S.; O’Malley, M.J.; Vaughan, C. Automatic detection of gait events using kinematic data. Gait Posture 2007, 25, 469–474. [Google Scholar] [CrossRef]
- Lord, S.; Galna, B.; Rochester, L. Moving forward on gait measurement: Toward a more refined approach. Mov. Disord. 2013, 28, 1534–1543. [Google Scholar] [CrossRef]
- Shao, X.; Ma, C. A general approach to derivative calculation using wavelet transform. Chemom. Intell. Lab. Syst. 2003, 69, 157–165. [Google Scholar] [CrossRef]
- Wan, X.; Wang, W.; Liu, J.; Tong, T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res. Methodol. 2014, 14, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Kim, S. ppcor: An R Package for a Fast Calculation to Semi-partial Correlation Coefficients. Commun. Stat. Appl. Methods 2015, 22, 665–674. [Google Scholar] [CrossRef] [Green Version]
- Nakagawa, S.; Johnson, P.C.D.; Schielzeth, H. The coefficient of determination R 2 and intra-class correlation coefficient from generalized linear mixed-effects models revisited and expanded. J. R. Soc. Interface 2017, 14, 20170213. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weir, J.P. Quantifying Test-Retest Reliability Using the Intraclass Correlation Coefficient and the SEM. J. Strength Cond. Res. 2005, 19, 231–240. [Google Scholar] [CrossRef] [PubMed]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef] [Green Version]
- Husted, J.A.; Cook, R.J.; Farewell, V.T.; Gladman, D.D. Methods for assessing responsiveness: A critical review and recommendations. J Clin Epidemiol 2000, 53, 459–468. [Google Scholar] [CrossRef]
- Cole, T.J. Too many digits: The presentation of numerical data. Arch. Dis. Child. 2015, 100, 608–609. [Google Scholar] [CrossRef] [Green Version]
- Munro, B.H. Statistical Methods for Health Care Research, 5th ed.; Lippincott Williams & Wilkins: Philadelphia, PN, USA, 2005; Volume XIII, 494 p. [Google Scholar]
- Silsupadol, P.; Prupetkaew, P.; Kamnardsiri, T.; Lugade, V. Smartphone-Based Assessment of Gait During Straight Walking, Turning, and Walking Speed Modulation in Laboratory and Free-Living Environments. IEEE J. Biomed. Health Inform. 2019, 24, 1188–1195. [Google Scholar] [CrossRef]
- Kim, W.-S.; Choi, H.; Jung, J.-W.; Yoon, J.S.; Jeoung, J.H. Asymmetry and Variability Should Be Included in the Assessment of Gait Function in Poststroke Hemiplegia with Independent Ambulation During Early Rehabilitation. Arch. Phys. Med. Rehabil. 2020, 102, 611–618. [Google Scholar] [CrossRef]
- Heredia-Jimenez, J.; Orantes-Gonzalez, E.; Soto-Hermoso, V. Variability of gait, bilateral coordination, and asymmetry in women with fibromyalgia. Gait Posture 2016, 45, 41–44. [Google Scholar] [CrossRef]
- Laroche, D.P.; Cook, S.B.; Mackala, K. Strength Asymmetry Increases Gait Asymmetry and Variability in Older Women. Med. Sci. Sports Exerc. 2012, 44, 2172–2181. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yogev, G.; Plotnik, M.; Peretz, C.; Giladi, N.; Hausdorff, J.M. Gait asymmetry in patients with Parkinson's disease and elderly fallers: When does the bilateral coordination of gait require attention? Exp. Brain Res. 2007, 177, 336–346. [Google Scholar] [CrossRef]
- Wong, D.W.-C.; Lam, W.K.; Lee, W.C.-C. Gait asymmetry and variability in older adults during long-distance walking: Implications for gait instability. Clin. Biomech. 2020, 72, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Hill, C.N.; Romero, M.L.; Rogers, M.; Queen, R.M.; Brolinson, P.G. Effect of osteopathic manipulation on gait asymmetry. J. Osteopath. Med. 2021. [Google Scholar] [CrossRef] [PubMed]
- Peraza, L.R.; Kinnunen, K.M.; McNaney, R.; Craddock, I.J.; Whone, A.L.; Morgan, C.; Joules, R.; Wolz, R. An Automatic Gait Analysis Pipeline for Wearable Sensors: A Pilot Study in Parkinson’s Disease. Sensors 2021, 21, 8286. [Google Scholar] [CrossRef]
- Hopkins, W.G. Measures of reliability in sports medicine and science. Sports Med. 2000, 30, 1–15. [Google Scholar] [CrossRef] [Green Version]
- Galna, B.; Lord, S.; Rochester, L. Is gait variability reliable in older adults and Parkinson's disease? Towards an optimal testing protocol. Gait Posture. 2013, 37, 580–585. [Google Scholar] [CrossRef] [PubMed]
- Perera, S.; Smith, C.; Coffman, L.; Brach, J. Number of Steps Needed for Reliable Gait Variability Measurement. In Gerontologist; Oxford Univ Press Inc.: Cary, NC, USA, 2016. [Google Scholar]
- Alqahtani, B.A.; Sparto, P.J.; Whitney, S.L.; Greenspan, S.L.; Perera, S.; Brach, J.S. Psychometric properties of instrumented postural sway measures recorded in community settings in independent living older adults. BMC Geriatr. 2020, 20, 82. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Williams, J.M.; Dorey, C.; Clark, S.; Clark, C. The within-day and between-day reliability of using sacral accelerations to quantify balance performance. Phys. Ther. Sport 2016, 17, 45–50. [Google Scholar] [CrossRef] [PubMed]
- Mazza, C.; Alcock, L.; Aminian, K.; Becker, C.; Bertuletti, S.; Bonci, T.; Brown, P.; Brozgol, M.; Buckley, E.; Carsin, A.E.; et al. Technical validation of real-world monitoring of gait: A multicentric observational study. BMJ Open. 2021, 12, e050785. [Google Scholar] [CrossRef] [PubMed]

| Participant No. | Sex | Age (Years) | Height (cm) | Mass (kg) |
|---|---|---|---|---|
| 1 | Female | 37 | 152 | 50.9 |
| 2 | Female | 27 | 168 | 76.2 |
| 3 | Male | 25 | 180 | 87.3 |
| 4 | Female | 27 | 166.5 | 63 |
| 5 | Male | 39 | 164.5 | 63.9 |
| 6 | Female | 36 | 168.6 | 64.7 |
| 7 | Male | 28 | 186 | 84.2 |
| 8 | Male | 38 | 170 | 95.7 |
| 9 | Male | 53 | 177 | 76.7 |
| 10 | Female | 32 | 164.3 | 65.5 |
| 11 | Male | 27 | 176.6 | 71.1 |
| 12 | Male | 57 | 179.5 | 83.4 |
| 13 | Female | 28 | 159.4 | 83.2 |
| 14 | Male | 47 | 178.5 | 81.3 |
| 15 | Male | 48 | 174.5 | 75.3 |
| 16 | Female | 41 | 162 | 68.8 |
| 17 | Female | 43 | 161 | 54.4 |
| 18 | Female | 59 | 163 | 57.5 |
| 19 | Female | 59 | 155 | 67.4 |
| 20 | Male | 30 | 181.5 | 85.2 |
| 21 | Male | 46 | 175.5 | 71.1 |
| 22 | Male | 51 | 180 | 78.3 |
| 23 | Female | 46 | 163 | 62.4 |
| 24 | Female | 68 | 159 | 65 |
| 25 | Female | 52 | 157 | 66 |
| 26 | Male | 61 | 166 | 86.4 |
| 27 | Male | 67 | 183 | 104.4 |
| 28 | Male | 69 | 178 | 104.1 |
| 29 | Female | 60 | 152 | 81.5 |
| 30 | Female | 63 | 145 | 54.1 |
| Outcome | MoCap | G&B App | 95% LoA | LoA% | Agreement Interpretation | rp [95% CI] | Consistency Interpretation |
|---|---|---|---|---|---|---|---|
| Comfortable walking with the head forward | |||||||
| Periodicity (%) | 68 ± 3 | 70 ± 3 | −2, 7 | 10 | Moderate | 0.69 [0.55, 0.79] | Moderate |
| SLAv (m) | 0.68 ± 0.06 | 0.67 ± 0.06 | −0.07, 0.07 | 11 | Moderate | 0.81 [0.72, 0.87] | Moderate |
| STAv (s) | 0.54 ± 0.04 | 0.54 ± 0.04 | −0.01, 0.02 | 3 | Excellent | 0.99 [0.98, 0.99] | Excellent |
| SLVr (%) | 4 ± 1 | 3 ± 1 | −4, 2 | 109 | Poor | 0.20 [−0.02, 0.39] | Poor |
| STVr (%) | 2.5 ± 0.8 | 2.9 ± 1 | −1.5, 2.2 | 80 | Poor | 0.40 [0.20, 0.57] | Poor |
| SLAs (%) | 4 ± 3 | 3 ± 2 | −8, 5 | 217 | Poor | 0.37 [0.17, 0.54] | Poor |
| STAs (%) | 2 ± 2 | 3 ± 2 | −3, 6 | 212 | Poor | 0.37 [0.17, 0.54] | Poor |
| WS (m/s) | 1.27 ± 0.16 | 1.25 ± 0.14 | −0.15, 0.12 | 12 | Moderate | 0.91 [0.86, 0.94] | Good |
| Comfortable walking while turning the head | |||||||
| Periodicity (%) | 67 ± 3 | 69 ± 3 | −2, 6 | 8 | Good | 0.77 [0.67, 0.84] | Moderate |
| SLAv (m) | 0.64 ± 0.05 | 0.65 ± 0.05 | −0.06, 0.07 | 10 | Moderate | 0.80 [0.70, 0.86] | Moderate |
| STAv (s) | 0.55 ± 0.04 | 0.56 ± 0.04 | −0.01, 0.02 | 3 | Excellent | 0.99 [0.98, 0.99] | Excellent |
| SLVr (%) | 5 ± 2 | 3 ± 1 | −6, 3 | 140 | Poor | 0.37 [0.17, 0.54] | Poor |
| STVr (%) | 2.5 ± 0.9 | 3.0 ± 0.8 | −1.3, 2.2 | 79 | Poor | 0.44 [0.24, 0.59] | Poor |
| SLAs (%) | 5 ± 4 | 3 ± 3 | −8, 5 | 197 | Poor | 0.52 [0.34, 0.66] | Poor |
| STAs (%) | 2 ± 2 | 3 ± 2 | −4, 7 | 283 | Poor | 0.14 [−0.07, 0.34] | Poor |
| WS (m/s) | 1.18 ± 0.13 | 1.16 ± 0.13 | −0.13, 0.11 | 11 | Moderate | 0.88 [0.82, 0.92] | Good |
| Outcome | rp [95% CI] | Interpretation |
|---|---|---|
| PS | 0.87 [0.84, 0.89] | Good |
| PSML | 0.73 [0.68, 0.78] | Moderate |
| PSAP | 0.95 [0.93, 0.96] | Excellent |
| Outcome | Task | Test 1, Test 2, Test 3 | F, p | SEM, SEM% | ICCAll [95% CI], Interpretation | ICC2−3 [95% CI] Interpretation |
|---|---|---|---|---|---|---|
| Periodicity (%) | WTHF | 70 ± 3, 70 ± 3, 71 ± 2 | 2.48, 0.1 | 1, 1 | 0.85 [0.75, 0.92], ℍ | 0.90 [0.79, 0.95], ℍ |
| WTHT | 68 ± 3, 69 ± 3, 70 ± 3 | 8.64, 0.001 | 1, 1 | 0.84 [0.71, 0.92], ℍ | 0.88 [0.75, 0.94], ℍ | |
| Between-task ANOVA | 20.23, <0.001 | |||||
| SLAv (m) | WTHF | 0.67 ± 0.06, 0.67 ± 0.06, 0.68 ± 0.05 | 2.78, 0.1 | 0.01, 2 | 0.93 [0.87, 0.96], ℍ | 0.96 [0.92, 0.98], 𝔼 |
| WTHT | 0.64 ± 0.05, 0.65 ± 0.05, 0.65 ± 0.05 | 16.72, <0.001 | 0.01, 2 | 0.91 [0.77, 0.96], ℍ | 0.96 [0.85, 0.98], 𝔼 | |
| Between-task ANOVA | 40.22, <0.001 | |||||
| STAv (s) | WTHF | 0.55 ± 0.04, 0.54 ± 0.04, 0.53 ± 0.04 | 6.72, 0.008 | 0.01, 3 | 0.85 [0.73, 0.92], ℍ | 0.95 [0.88, 0.97], ℍ |
| WTHT | 0.57 ± 0.05, 0.56 ± 0.05, 0.55 ± 0.04 | 10.59, <0.001 | 0.01, 2 | 0.90 [0.80, 0.95], ℍ | 0.96 [0.91, 0.98], 𝔼 | |
| Between-task ANOVA | 9.34, 0.005 | |||||
| SLVr (%) | WTHF | 3.2 ± 0.8, 2.9 ± 0.8, 3.1 ± 0.8 | 2.1, 0.1 | 0.6, 19 | 0.48 [0.26, 0.68], ℙ | 0.53 [0.23, 0.75], ℙ |
| WTHT | 3.9 ± 1.1, 3.4 ± 0.9, 3.2 ± 0.7 | 6.06, 0.006 | 0.8, 26 | 0.16 [−0.30, 0.39], ℙ | 0.32 [−0.3, 0.60], ℙ | |
| Between-task ANOVA | 0.15, 0.7 | |||||
| STVr (%) | WTHF | 3.2 ± 1.1, 2.8 ± 1, 2.6 ± 0.8 | 3.79, 0.030 | 0.9, 33 | 0.14 [−0.50, 0.38], ℙ | 0.40 [−0.32, 0.40], ℙ |
| WTHT | 3.3 ± 0.9, 2.8 ± 0.7, 2.9 ± 0.8 | 3.24, 0.049 | 0.7, 25 | 0.23 [0.20., 0.47], ℙ | 0.20 [−0.17, 0.52], ℙ | |
| Between-task ANOVA | 3.18, 0.090 | |||||
| SLAs (%) | WTHF | 3 ± 2, 3 ± 3, 3 ± 2 | 0.88, 0.400 | 1, 34 | 0.79 [0.66, 0.88], 𝕄 | 0.80 [0.62, 0.90], 𝕄 |
| WTHT | 4 ± 3, 3 ± 2, 3 ± 2 | 3.54, 0.044 | 2, 54 | 0.61 [0.42, 0.78], ℙ | 0.74 [0.53, 0.87], 𝕄 | |
| Between-task ANOVA | 1.22, 0.279 | |||||
| STAs (%) | WTHF | 4 ± 2, 3 ± 2, 3 ± 2 | 1.54, 0.227 | 1, 44 | 0.58 [0.38, 0.75], ℙ | 0.71 [0.47, 0.85], ℙ |
| WTHT | 3 ± 3, 3 ± 2, 3 ± 2 | 0.37, 0.686 | 2, 50 | 0.61 [0.41, 0.77], ℙ | 0.66 [0.39, 0.82], ℙ | |
| Between-task ANOVA | 0.29, 0.593 | |||||
| WS (m/s) | WTHF | 1.23 ± 0.15, 1.26 ± 0.13, 1.27 ± 0.13 | 5.73, 0.014 | 0.05, 4 | 0.85 [0.73, 0.92], ℍ | 0.92 [0.85, 0.96], ℍ |
| WTHT | 1.13 ± 0.13, 1.17 ± 0.13, 1.19 ± 0.12 | 16.14, <0.001 | 0.04, 4 | 0.83 [0.63, 0.92], 𝕄 | 0.93 [0.82, 0.97], ℍ | |
| Between-task ANOVA | 35.57, <0.001 | |||||
| Outcome | Task | Test 1, Test 2, Test 3 | F, p | SEM, SEM% | ICCAll [95% CI], Interpretation | ICC2−3 [95% CI], Interpretation |
|---|---|---|---|---|---|---|
| PS | FSEO | 3.57 ± 0.26, 3.54 ± 0.26, 3.6 ± 0.25 | 2.20, 0.1 | 0.1, 3 | 0.84 [0.73, 0.91], ℍ | 0.86 [0.71, 0.94], ℍ |
| FSEC | 3.47 ± 0.32, 3.48 ± 0.29, 3.53 ± 0.29 | 3.29, 0.048 | 0.09, 3 | 0.91 [0.84, 0.95], ℍ | 0.92 [0.83, 0.96], ℍ | |
| CSEO | 3.06 ± 0.27, 3.17 ± 0.32, 3.21 ± 0.28 | 20.83, <0.001 | 0.1, 3 | 0.83 [0.60, 0.93], 𝕄 | 0.93 [0.86, 0.97], ℍ | |
| CSEC | 2.84 ± 0.34, 2.83 ± 0.26, 2.87 ± 0.32 | 0.60, 0.6 | 0.2, 6 | 0.72 [0.56, 0.84], 𝕄 | 0.73 [0.52, 0.86], 𝕄 | |
| Between-task ANOVA | 189.73, <0.001 | |||||
| PSML | FSEO | 4.24 ± 0.29, 4.21 ± 0.29, 4.29 ± 0.29 | 4.58, 0.015 | 0.1, 3 | 0.84 [0.73, 0.92], ℍ | 0.84 [0.61, 0.93], 𝕄 |
| FSEC | 4.15 ± 0.36, 4.17 ± 0.31, 4.24 ± 0.32 | 4.72, 0.019 | 0.1, 3 | 0.88 [0.79, 0.94], ℍ | 0.91 [0.79, 0.96], ℍ | |
| CSEO | 3.77 ± 0.27, 3.91 ± 0.33, 3.95 ± 0.30 | 16.97, <0.001 | 0.1, 3 | 0.77 [0.52, 0.89], 𝕄 | 0.89 [0.79, 0.95], ℍ | |
| CSEC | 3.64 ± 0.34, 3.63 ± 0.30, 3.67 ± 0.34 | 0.61, 0.5 | 0.2, 4 | 0.75 [0.60, 0.86], 𝕄 | 0.74 [0.53, 0.87], 𝕄 | |
| Between-task ANOVA | 110.53, <0.001 | |||||
| PSAP | FSEO | 4.19 ± 0.22, 4.16 ± 0.20, 4.2 ± 0.22 | 0.66, 0.5 | 0.1, 3 | 0.71 [0.54, 0.84], 𝕄 | 0.78 [0.59, 0.89], 𝕄 |
| FSEC | 4.06 ± 0.28, 4.06 ± 0.25, 4.1 ± 0.27 | 1.46, 0.2 | 0.1, 2 | 0.87 [0.78, 0.93], ℍ | 0.88 [0.77, 0.94], ℍ | |
| CSEO | 3.72 ± 0.21, 3.81 ± 0.23, 3.83 ± 0.23 | 10.15, 0.001 | 0.1, 3 | 0.77 [0.58, 0.88], 𝕄 | 0.89 [0.78, 0.94], ℍ | |
| CSEC | 3.45 ± 0.27, 3.43 ± 0.21, 3.48 ± 0.25 | 0.76, 0.5 | 0.1, 4 | 0.67 [0.49, 0.81], ℙ | 0.65 [0.38, 0.81], ℙ | |
| Between-task ANOVA | 187.82, <0.001 | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rashid, U.; Barbado, D.; Olsen, S.; Alder, G.; Elvira, J.L.L.; Lord, S.; Niazi, I.K.; Taylor, D. Validity and Reliability of a Smartphone App for Gait and Balance Assessment. Sensors 2022, 22, 124. https://doi.org/10.3390/s22010124
Rashid U, Barbado D, Olsen S, Alder G, Elvira JLL, Lord S, Niazi IK, Taylor D. Validity and Reliability of a Smartphone App for Gait and Balance Assessment. Sensors. 2022; 22(1):124. https://doi.org/10.3390/s22010124
Chicago/Turabian StyleRashid, Usman, David Barbado, Sharon Olsen, Gemma Alder, Jose L. L. Elvira, Sue Lord, Imran Khan Niazi, and Denise Taylor. 2022. "Validity and Reliability of a Smartphone App for Gait and Balance Assessment" Sensors 22, no. 1: 124. https://doi.org/10.3390/s22010124
APA StyleRashid, U., Barbado, D., Olsen, S., Alder, G., Elvira, J. L. L., Lord, S., Niazi, I. K., & Taylor, D. (2022). Validity and Reliability of a Smartphone App for Gait and Balance Assessment. Sensors, 22(1), 124. https://doi.org/10.3390/s22010124










