Opportunities for Smartphone Sensing in E-Health Research: A Narrative Review
Abstract
:1. Introduction
2. Materials and Methods
- What health conditions have been examined using smartphone sensing?
- What data-collection approaches have been used and what are their trade-offs?
- What applications and resources have been used?
- What were the researchers’ motivations for their data-collection and -analysis approaches?
2.1. Search Terms
2.2. Search Strategy
2.3. Inclusion Criteria
- Empirical research that uses smartphone sensing to monitor a health condition;
- Empirical research that explores perceptions and challenges of smartphone sensing.
3. Results
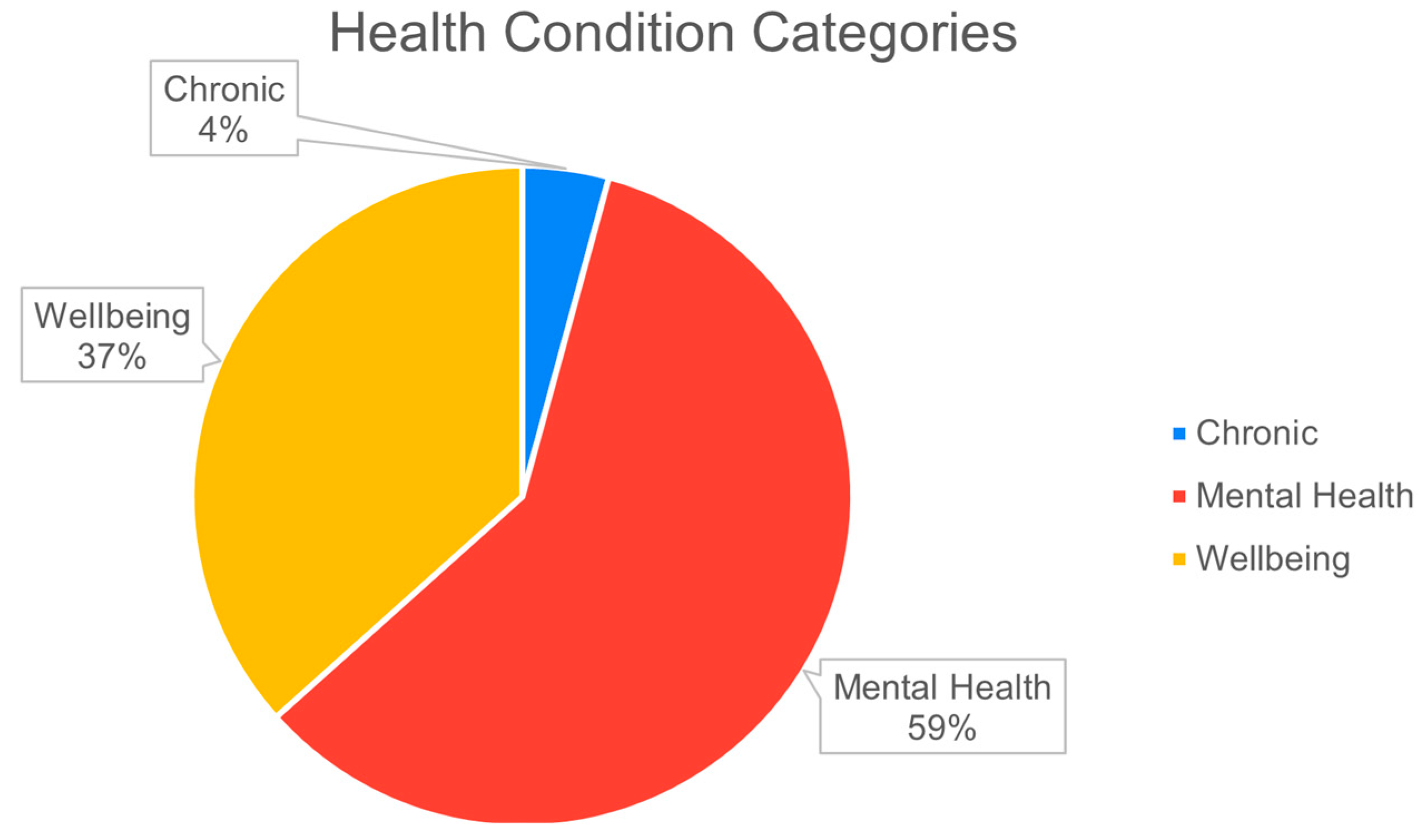
3.1. Health Conditions That Have Been Studied
3.1.1. General Wellbeing
3.1.2. Chronic Health Condition (Parkinson’s)
3.1.3. Mental Health Conditions
3.2. Data-Collection Approaches
3.2.1. Actively Collected Data
- 1.
- Demographic information
- 2.
- Clinical scale/questionnaire responses
- 3.
- Ecological Momentary Assessments (EMA)/self-reports
3.2.2. Passively Sensed Data
- 1.
- Trade-off between power consumption and data-collection rate
- 2.
- Placement of device
- 3.
- Data storage and transmission.
- 4.
- Device operating system
- 5.
- Privacy concerns.
3.3. Applications, Frameworks, and Resources Used in the Studies
3.4. Motivations for Data-Collection and -Analysis Approaches
- Exploratory studies:Four studies were exploratory, presenting the design of their sensing systems and evaluated the data-collection capabilities of their applications. For example, ref. [58] presents a nonobtrusive sleep-detecting application and evaluates how reliably it could detect sleeping behaviors.
- Monitoring change in behavioral patterns:In seven studies, the emphasis was to monitor human behavior using smartphone-sensed data. For example, Refs. [24,25] monitored changes in mental health and behavior during the COVID-19 pandemic, by examining changes in smartphone-sensed data. They examined how factors such as physical activity, sociability, and mobility of students changed due to the pandemic, which provided an indication of their mental health.
- Identifying correlation between smartphone-sensed features and wellbeing factors:In 24 studies, the emphasis was to examine the statistical significance of features extracted from smartphones with wellbeing behaviors. For example, Ref. [86] collected data from the microphone sensor to evaluate if audio features were correlated to self-reported measures of depression. In another example, Ref. [7] collected location data to determine if there was a correlation between time spent at home and self-reported depressive symptoms.
- Identifying feature correlations and using machine learning to predict behavior:These types of studies (22 studies) not only identified correlation between smartphone-sensed features, but also built machine-learning models to evaluate if these were able to predict user behavior. For example, Ref. [60] found location and activity features that correlated with drinking episodes. They then built a machine-learning framework to classify instances of drinking vs nondrinking and tested the performance of their system.
- Comparing activity-recognition performance of machine-learning models:Such studies aimed to evaluate the activity recognition of different machine-learning models. For example, Ref. [49] the performance of five types of ensemble classifiers to classify six activities (walking, walking upstairs, walking downstairs, sitting, standing, and lying).
4. Discussion
4.1. Predominance of Mental Health Studies
4.2. Opportunities for Standardization of Sensing Approaches
4.3. Opportunities for Using Machine-Learning Advancements in E-Health Research
4.4. Sensing Trends over the Years and Future Scope
5. Limitations and Future Work
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| Acronym | Meaning |
| GPS | Global Positioning System |
| HAR | Human Activity Recognition |
| NLR | Narrative Literature Review |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| PHQ | Patient Health Questionnaire |
| UCLA | University of California, Los Angeles |
| EMA | Ecological Momentary Assessments |
| Wi-Fi | Wireless Fidelity |
| ML | Machine Learning |
References
- Smartphone Ownership Is Growing Rapidly around the World, but Not Always Equally. Pew Research Center. Available online: https://www.pewresearch.org/global/2019/02/05/smartphone-ownership-is-growing-rapidly-around-the-world-but-not-always-equally/ (accessed on 6 April 2022).
- Miškinytė, A.; Dėdelė, A. Objective Assessment of Physical Activity Patterns Based on Accelerometer and GPS Data in Adults. Travel Behav. Soc. 2021, 25, 112–119. [Google Scholar] [CrossRef]
- Harari, G.M.; Gosling, S.D.; Wang, R.; Chen, F.; Chen, Z.; Campbell, A.T. Patterns of Behavior Change in Students over an Academic Term: A Preliminary Study of Activity and Sociability Behaviors Using Smartphone Sensing Methods. Comput. Hum. Behav. 2017, 67, 129–138. [Google Scholar] [CrossRef]
- Grimaldi, S.; Partonen, T.; Saarni, S.I.; Aromaa, A.; Lönnqvist, J. Indoors Illumination and Seasonal Changes in Mood and Behavior Are Associated with the Health-Related Quality of Life. Health Qual. Life Outcomes 2008, 6, 56. [Google Scholar] [CrossRef] [PubMed]
- Espiritu, R.C.; Kripke, D.F.; Ancoli-Israel, S.; Mowen, M.A.; Mason, W.J.; Fell, R.L.; Klauber, M.R.; Kaplan, O.J. Low Illumination Experienced by San Diego Adults: Association with Atypical Depressive Symptoms. Biol. Psychiatry 1994, 35, 403–407. [Google Scholar] [CrossRef]
- Time Spent on Average on a Smartphone in the U.S. 2021. Statista. Available online: https://www.statista.com/statistics/1224510/time-spent-per-day-on-smartphone-us/ (accessed on 6 April 2022).
- Laiou, P.; Kaliukhovich, D.A.; Folarin, A.A.; Ranjan, Y.; Rashid, Z.; Conde, P.; Stewart, C.; Sun, S.; Zhang, Y.; Matcham, F.; et al. The Association Between Home Stay and Symptom Severity in Major Depressive Disorder: Preliminary Findings From a Multicenter Observational Study Using Geolocation Data From Smartphones. JMIR Mhealth Uhealth 2022, 10, e28095. [Google Scholar] [CrossRef] [PubMed]
- Yue, C.; Ware, S.; Morillo, R.; Lu, J.; Shang, C.; Bi, J.; Kamath, J.; Russell, A.; Bamis, A.; Wang, B. Fusing Location Data for Depression Prediction. IEEE Trans. Big Data 2018, 7, 355–370. [Google Scholar] [CrossRef]
- Wu, C.; Barczyk, A.N.; Craddock, R.C.; Harari, G.M.; Thomaz, E.; Shumake, J.D.; Beevers, C.G.; Gosling, S.D.; Schnyer, D.M. Improving Prediction of Real-Time Loneliness and Companionship Type Using Geosocial Features of Personal Smartphone Data. Smart Health 2021, 20, 100180. [Google Scholar] [CrossRef]
- Ehatisham-ul-Haq, M.; Azam, M.A.; Asim, Y.; Amin, Y.; Naeem, U.; Khalid, A. Using Smartphone Accelerometer for Human Physical Activity and Context Recognition In-the-Wild. Procedia Comput. Sci. 2020, 177, 24–31. [Google Scholar] [CrossRef]
- O’Brien, M.K.; Shawen, N.; Mummidisetty, C.K.; Kaur, S.; Bo, X.; Poellabauer, C.; Kording, K.; Jayaraman, A. Activity Recognition for Persons With Stroke Using Mobile Phone Technology: Toward Improved Performance in a Home Setting. J. Med. Internet Res. 2017, 19, e184. [Google Scholar] [CrossRef]
- Bae, S.W.; Chung, T.; Islam, R.; Suffoletto, B.; Du, J.; Jang, S.; Nishiyama, Y.; Mulukutla, R.; Dey, A. Mobile Phone Sensor-Based Detection of Subjective Cannabis Intoxication in Young Adults: A Feasibility Study in Real-World Settings. Drug Alcohol Depend. 2021, 228, 108972. [Google Scholar] [CrossRef]
- Wang, R.; Chen, F.; Chen, Z.; Li, T.; Harari, G.; Tignor, S.; Zhou, X.; Ben-Zeev, D.; Campbell, A.T. StudentLife: Using Smartphones to Assess Mental Health and Academic Performance of College Students. In Mobile Health; Rehg, J., Murphy, S., Kumar, S., Eds.; Springer: Cham, Switzerland, 2017. [Google Scholar] [CrossRef]
- Zhang, H.; Hanci, E.; Gashi, S.; Matthews, O.; Kimm, H. Moodbook: An Application for Continuous Monitoring of Social Media Usage and Mood. In Proceedings of the 2018 ACM International Joint Conference on Pervasive and Ubiquitous Computing and 2018 ACM International Symposium on Wearable Computers, Singapore, 8–12 October 2018; pp. 1150–1155. [Google Scholar] [CrossRef]
- Zhang, X.; Li, W.; Chen, X.; Lu, S. MoodExplorer: Towards Compound Emotion Detection via Smartphone Sensing. Proc. ACM Interact. Mob. Wearable Ubiquitous Technol. 2018, 1, 1–30. [Google Scholar] [CrossRef]
- Torkamaan, H.; Ziegler, J. Mobile Mood Tracking. Proc. ACM Interact. Mob. Wearable Ubiquitous Technol. 2020, 4, 1–30. [Google Scholar] [CrossRef]
- Dogrucu, A.; Perucic, A.; Isaro, A.; Ball, D.; Toto, E.; Rundensteiner, E.A.; Agu, E.; Davis-Martin, R.; Boudreaux, E. Moodable: On Feasibility of Instantaneous Depression Assessment Using Machine Learning on Voice Samples with Retrospectively Harvested Smartphone and Social Media Data. Smart Health 2020, 17, 100118. [Google Scholar] [CrossRef]
- Rebolledo, M.; Eiben, A.E.; Bartz-Beielstein, T. Bayesian Networks for Mood Prediction Using Unobtrusive Ecological Momentary Assessments. In Applications of Evolutionary Computation; Castillo, P.A., Jiménez Laredo, J.L., Eds.; Lecture Notes in Computer Science; Springer: Cham, Switzerland, 2021; Volume 12694, pp. 373–387. [Google Scholar] [CrossRef]
- Niemeijer, K.; Mestdagh, M.; Kuppens, P. Tracking Subjective Sleep Quality and Mood With Mobile Sensing: Multiverse Study. J. Med. Internet Res. 2022, 24, e25643. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Zhuang, F.; Li, W.; Ying, H.; Xiong, H.; Lu, S. Inferring Mood Instability via Smartphone Sensing: A Multi-View Learning Approach. In Proceedings of the 27th ACM International Conference on Multimedia, Nice, France, 21–25 October 2019; pp. 1401–1409. [Google Scholar] [CrossRef]
- Suhara, Y.; Xu, Y.; Pentland, A.S. DeepMood: Forecasting Depressed Mood Based on Self-Reported Histories via Recurrent Neural Networks. In Proceedings of the 26th International World Wide Web Conference, WWW 2017, Perth, Australia, 3–7 April 2017; pp. 715–724. [Google Scholar] [CrossRef]
- Müller, S.R.; Peters, H.; Matz, S.C.; Wang, W.; Harari, G.M. Investigating the Relationships between Mobility Behaviours and Indicators of Subjective Well–Being Using Smartphone–Based Experience Sampling and GPS Tracking. Eur. J. Personal. 2020, 34, 714–732. [Google Scholar] [CrossRef]
- Fahim, M.; Baker, T.; Khattak, A.M.; Alfandi, O. Alert Me: Enhancing Active Lifestyle via Observing Sedentary Behavior Using Mobile Sensing Systems. In Proceedings of the 2017 IEEE 19th International Conference on e-Health Networking, Applications and Services, Healthcom 2017, Dalian, China, 12–15 October 2017; pp. 1–4. [Google Scholar] [CrossRef]
- Huckins, J.F.; da Silva, A.W.; Wang, W.; Hedlund, E.; Rogers, C.; Nepal, S.K.; Wu, J.; Obuchi, M.; Murphy, E.I.; Meyer, M.L.; et al. Mental Health and Behavior of College Students During the Early Phases of the COVID-19 Pandemic: Longitudinal Smartphone and Ecological Momentary Assessment Study. J. Med. Internet Res. 2020, 22, e20185. [Google Scholar] [CrossRef] [PubMed]
- Mack, D.L.; DaSilva, A.W.; Rogers, C.; Hedlund, E.; Murphy, E.I.; Vojdanovski, V.; Plomp, J.; Wang, W.; Nepal, S.K.; Holtzheimer, P.E.; et al. Mental Health and Behavior of College Students During the COVID-19 Pandemic: Longitudinal Mobile Smartphone and Ecological Momentary Assessment Study, Part II. J. Med. Internet Res. 2021, 23, e28892. [Google Scholar] [CrossRef]
- MacLeod, L.; Suruliraj, B.; Gall, D.; Bessenyei, K.; Hamm, S.; Romkey, I.; Bagnell, A.; Mattheisen, M.; Muthukumaraswamy, V.; Orji, R.; et al. A Mobile Sensing App to Monitor Youth Mental Health: Observational Pilot Study. JMIR Mhealth Uhealth 2021, 9, e20638. [Google Scholar] [CrossRef]
- Thakur, S.S.; Roy, R.B. Predicting Mental Health Using Smart-Phone Usage and Sensor Data. J. Ambient. Intell. Humaniz. Comput. 2021, 12, 9145–9161. [Google Scholar] [CrossRef]
- Abujrida, H.; Agu, E.; Pahlavan, K. Machine Learning-Based Motor Assessment of Parkinson’s Disease Using Postural Sway, Gait and Lifestyle Features on Crowdsourced Smartphone Data. Biomed. Phys. Eng. Express 2020, 6, 035005. [Google Scholar] [CrossRef]
- Abujrida, H.; Agu, E.; Pahlavan, K. Smartphone-Based Gait Assessment to Infer Parkinson’s Disease Severity Using Crowdsourced Data. In Proceedings of the 2017 IEEE Healthcare Innovations and Point of Care Technologies, HI-POCT 2017, Bethesda, MD, USA, 6–8 November 2017; pp. 208–211. [Google Scholar] [CrossRef]
- Zhang, H.; Guo, G.; Song, C.; Xu, C.; Cheung, K.; Alexis, J.; Li, H.; Li, D.; Wang, K.; Xu, W. PDLens: Smartphone Knows Drug Effectiveness among Parkinson’s via Daily-Life Activity Fusion. In Proceedings of the Annual International Conference on Mobile Computing and Networking, MOBICOM, London, UK, 21–25 September 2020; Volume 20, pp. 150–163. [Google Scholar] [CrossRef]
- Postolache, G.; Postolache, O. Smartphone Sensing Technologies for Tailored Parkinson’s Disease Diagnosis and Monitoring. In Mobile Solutions and Their Usefulness in Everyday Life; EAI/Springer Innovations in Communication and Computing; Springer: Cham, Switzerland, 2019; pp. 251–273. [Google Scholar] [CrossRef]
- Ferreira, D.; Kostakos, V.; Dey, A.K. AWARE: Mobile Context Instrumentation Framework. Front. ICT 2015, 2, 6. [Google Scholar] [CrossRef] [Green Version]
- Torous, J.; Kiang, M.V.; Lorme, J.; Onnela, J.P. New Tools for New Research in Psychiatry: A Scalable and Customizable Platform to Empower Data Driven Smartphone Research. JMIR Ment. Health 2016, 3, e5165. [Google Scholar] [CrossRef] [PubMed]
- Lind, M.N.; Byrne, M.L.; Wicks, G.; Smidt, A.M.; Allen, N.B. The Effortless Assessment of Risk States (EARS) Tool: An Interpersonal Approach to Mobile Sensing. JMIR Ment. Health 2018, 5, e10334. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Green, B.N.; Johnson, C.D.; Adams, A. Writing Narrative Literature Reviews for Peer-Reviewed Journals: Secrets of the Trade. J. Chiropr. Med. 2006, 5, 101–117. [Google Scholar] [CrossRef] [Green Version]
- Torous, J.; Larsen, M.E.; Depp, C.; Cosco, T.D.; Barnett, I.; Nock, M.K.; Firth, J. Smartphones, Sensors, and Machine Learning to Advance Real-Time Prediction and Interventions for Suicide Prevention: A Review of Current Progress and Next Steps. Curr. Psychiatry Rep. 2018, 20, 51. [Google Scholar] [CrossRef] [PubMed]
- Kerst, A.; Zielasek, J.; Gaebel, W. Smartphone Applications for Depression: A Systematic Literature Review and a Survey of Health Care Professionals’ Attitudes towards Their Use in Clinical Practice. Eur. Arch. Psychiatry Clin. Neurosci. 2020, 270, 139–152. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, N.; Nguyen, C.; Thrul, J. Digital Health for Assessment and Intervention Targeting Tobacco and Cannabis Co-Use. Curr. Addict. Rep. 2020, 7, 268–279. [Google Scholar] [CrossRef]
- Konsolakis, K.; Hermens, H.; Villalonga, C.; Vollenbroek-Hutten, M.; Banos, O. Human Behaviour Analysis through Smartphones. Proceedings 2018, 2, 1243. [Google Scholar] [CrossRef] [Green Version]
- Straczkiewicz, M.; James, P.; Onnela, J.P. A Systematic Review of Smartphone-Based Human Activity Recognition Methods for Health Research. Npj Digit. Med. 2021, 4, 148. [Google Scholar] [CrossRef]
- Mendes, J.P.M.; Moura, I.R.; van de Ven, P.; Viana, D.; Silva, F.J.S.; Coutinho, L.R.; Teixeira, S.; Rodrigues, J.J.P.C.; Teles, A.S. Sensing Apps and Public Data Sets for Digital Phenotyping of Mental Health: Systematic Review. J. Med. Internet Res. 2022, 24, e28735. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferrari, R. Writing Narrative Style Literature Reviews. Eur. Med. Writ. Assoc. 2015, 24, 230–235. [Google Scholar] [CrossRef]
- Baethge, C.; Goldbeck-Wood, S.; Mertens, S. SANRA—A Scale for the Quality Assessment of Narrative Review Articles. Res. Integr. Peer Rev. 2019, 4, 5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Privacy in Android 11. Android Developers. Available online: https://developer.android.com/about/versions/11/privacy (accessed on 29 April 2022).
- Privacy Changes in Android 10. Android Developers. Available online: https://developer.android.com/about/versions/10/privacy/changes (accessed on 29 April 2022).
- Ibrahim, A.; Zhang, H.; Clinch, S.; Poliakoff, E.; Parsia, B.; Harper, S. Digital Phenotypes for Understanding Individuals’ Compliance With COVID-19 Policies and Personalized Nudges: Longitudinal Observational Study. JMIR Form. Res. 2021, 5, e23461. [Google Scholar] [CrossRef] [PubMed]
- Jones, S.L.; Hue, W.; Kelly, R.M.; Barnett, R.; Henderson, V.; Sengupta, R. Determinants of Longitudinal Adherence in Smartphone-Based Self-Tracking for Chronic Health Conditions. Proc. ACM Interact. Mob. Wearable Ubiquitous Technol. 2021, 5, 16. [Google Scholar] [CrossRef]
- Rahim, K.N.K.A.; Elamvazuthi, I.; Izhar, L.I.; Capi, G. Classification of Human Daily Activities Using Ensemble Methods Based on Smartphone Inertial Sensors. Sensors 2018, 18, 4132. [Google Scholar] [CrossRef] [Green Version]
- Chen, A.T.; Russell, S.; Wu, C.; Fritz, H.; Miller, M.; Craddock, C.; Kinney, K.; Castelli, D.; Schnyer, D. Exploring Post COVID-19 Outbreak Intradaily Mobility Pattern Change in College Students: A GPS-Focused Smartphone Sensing Study. Front. Digit. Health 2021, 3, 765972. [Google Scholar] [CrossRef]
- Vaghela, M.; Sasidhar, K. Analyzing the Human Behavior Using Pervasive Sensing System. In Proceedings of the 21st International Conference on Distributed Computing and Networking, Kolkata, India, 4–7 January 2020. [Google Scholar]
- Kelly, D.; Curran, K.; Caulfield, B. Automatic Prediction of Health Status Using Smartphone-Derived Behavior Profiles. IEEE J. Biomed. Health Inform. 2017, 21, 1750–1760. [Google Scholar] [CrossRef]
- di Mitri, D.; Asyraaf Mat Sanusi, K.; Trebing, K.; Bromuri, S. MOBIUS: Smart Mobility Tracking with Smartphone Sensors. In Science and Technologies for Smart Cities; Lecture Notes of the Institute for Computer Sciences, Social-Informatics and Telecommunications Engineering, LNICST; Springer: Cham, Switzerland, 2021; Volume 372. [Google Scholar] [CrossRef]
- Harari, G.M.; Müller, S.R.; Stachl, C.; Wang, R.; Wang, W.; Bühner, M.; Rentfrow, P.J.; Campbell, A.T.; Gosling, S.D. Sensing Sociability: Individual Differences in Young Adults’ Conversation, Calling, Texting, and App Use Behaviors in Daily Life. J. Personal. Soc. Psychol. 2020, 119, 204–228. [Google Scholar] [CrossRef]
- Wetzel, B.; Pryss, R.; Baumeister, H.; Edler, J.S.; Gonçalves, A.S.O.; Cohrdes, C. “How Come You Don’t Call Me?” Smartphone Communication App Usage as an Indicator of Loneliness and Social Well-Being across the Adult Lifespan during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 6212. [Google Scholar] [CrossRef]
- Schoedel, R.; Pargent, F.; Au, Q.; Völkel, S.T.; Schuwerk, T.; Bühner, M.; Stachl, C. To Challenge the Morning Lark and the Night Owl: Using Smartphone Sensing Data to Investigate Day–Night Behaviour Patterns. Eur. J. Personal. 2020, 34, 733–752. [Google Scholar] [CrossRef]
- Montanini, L.; Sabino, N.; Spinsante, S.; Gambi, E. Smartphone as Unobtrusive Sensor for Real-Time Sleep Recognition. In Proceedings of the 2018 IEEE International Conference on Consumer Electronics, Las Vegas, NV, USA, 12–14 January 2018; pp. 1–4. [Google Scholar] [CrossRef]
- ElBolock, A.; Amr, R.; Abdennadher, S. Non-Obtrusive Sleep Detection for Character Computing Profiling. Adv. Intell. Syst. Comput. 2018, 722, 249–254. [Google Scholar] [CrossRef]
- Lim, J.; Jeong, C.Y.; Lim, J.M.; Chung, S.; Kim, G.; Noh, K.J.; Jeong, H. Assessing Sleep Quality Using Mobile EMAs: Opportunities, Practical Consideration, and Challenges. IEEE Access 2022, 10, 2063–2076. [Google Scholar] [CrossRef]
- Phan, T.T.; Labhart, F.; Muralidhar, S.; Gatica-Perez, D. Understanding Heavy Drinking at Night through Smartphone Sensing and Active Human Engagement. In Proceedings of the PervasiveHealth: Pervasive Computing Technologies for Healthcare, Atlanta, GA, USA, 18–20 May 2020; Volume 12, pp. 211–222. [Google Scholar] [CrossRef]
- Meegahapola, L.; Labhart, F.; Phan, T.T.; Gatica-Perez, D. Examining the Social Context of Alcohol Drinking in Young Adults with Smartphone Sensing. Proc. ACM Interact. Mob. Wearable Ubiquitous Technol. 2021, 5, 26. [Google Scholar] [CrossRef]
- Bae, S.; Chung, T.; Ferreira, D.; Dey, A.K.; Suffoletto, B. Mobile Phone Sensors and Supervised Machine Learning to Identify Alcohol Use Events in Young Adults: Implications for Just-in-Time Adaptive Interventions. Addict. Behav. 2018, 83, 42–47. [Google Scholar] [CrossRef] [PubMed]
- Naughton, F.; Brown, C.; High, J.; Notley, C.; Mascolo, C.; Coleman, T.; Barton, G.; Shepstone, L.; Sutton, S.; Prevost, A.T.; et al. Randomised Controlled Trial of a Just-in-Time Adaptive Intervention (JITAI) Smoking Cessation Smartphone App: The Quit Sense Feasibility Trial Protocol. BMJ Open 2021, 11, e048204. [Google Scholar] [CrossRef]
- Li, R.; Agu, E.; Balakrishnan, G.; Herman, D.; Abrantes, A.; Stein, M.; Metrik, J. WeedGait: Unobtrusive Smartphone Sensing of Marijuana-Induced Gait Impairment by Fusing Gait Cycle Segmentation and Neural Networks. In Proceedings of the 2019 IEEE Healthcare Innovations and Point of Care Technologies, HI-POCT 2019, Bethesda, MD, USA, 20–22 November 2019; pp. 91–94. [Google Scholar] [CrossRef]
- Meegahapola, L.; Ruiz-Correa, S.; Robledo-Valero, V.D.C.; Hernandez-Huerfano, E.E.; Alvarez-Rivera, L.; Chenu-Abente, R.; Gatica-Perez, D. One More Bite? Inferring Food Consumption Level of College Students Using Smartphone Sensing and Self-Reports. Proc. ACM Interact. Mob. Wearable Ubiquitous Technol. 2021, 5, 26. [Google Scholar] [CrossRef]
- About Chronic Diseases. CDC. Available online: https://www.cdc.gov/chronicdisease/about/index.htm (accessed on 6 April 2022).
- Sarda, A.; Munuswamy, S.; Sarda, S.; Subramanian, V. Using Passive Smartphone Sensing for Improved Risk Stratification of Patients with Depression and Diabetes: Cross-Sectional Observational Study. JMIR Mhealth Uhealth 2019, 7, e11041. [Google Scholar] [CrossRef] [Green Version]
- Singh, V.K.; Long, T. Automatic Assessment of Mental Health Using Phone Metadata. Proc. Assoc. Inf. Sci. Technol. 2018, 55, 450–459. [Google Scholar] [CrossRef]
- Servia-Rodríguez, S.; Rachuri, K.K.; Mascolo, C.; Rentfrow, P.J.; Lathia, N.; Sandstrom, G.M. Mobile Sensing at the Service of Mental Well-Being: A Large-Scale Longitudinal Study. In Proceedings of the 26th International World Wide Web Conference, WWW 2017, Perth, Australia, 3–7 April 2017; pp. 103–112. [Google Scholar] [CrossRef] [Green Version]
- Messner, E.M.; Sariyska, R.; Mayer, B.; Montag, C.; Kannen, C.; Schwerdtfeger, A.; Baumeister, H. Insights—Future Implications of Passive Smartphone Sensing in the Therapeutic Context. Verhaltenstherapie 2019, 1–10. [Google Scholar] [CrossRef]
- Kalogirou, I.P.; Kallipolitis, A.; Maglogiannis, I. Passive Emotion Recognition Using Smartphone Sensing Data. Stud. Comput. Intell. 2020, 891, 17–28. [Google Scholar] [CrossRef]
- Buda, T.S.; Khwaja, M.; Matic, A. Outliers in Smartphone Sensor Data Reveal Outliers in Daily Happiness. Proc. ACM Interact. Mob. Wearable Ubiquitous Technol. 2021, 5, 19. [Google Scholar] [CrossRef]
- Piskioulis, O.; Tzafilkou, K.; Economides, A.A. Emotion Detection through Smartphone’s Accelerometer and Gyroscope Sensors. In Proceedings of the 29th ACM Conference on User Modeling, Adaptation and Personalization, Utrecht, The Netherlands, 21–25 June 2021; Volume 8, pp. 130–137. [Google Scholar] [CrossRef]
- Ruensuk, M.; Cheon, E.; Hong, H.; Oakley, I. How Do You Feel Online. Proc. ACM Interact. Mob. Wearable Ubiquitous Technol. 2020, 4, 1–32. [Google Scholar] [CrossRef]
- Wen, H.; Sobolev, M.; Vitale, R.; Kizer, J.; Pollak, J.P.; Muench, F.; Estrin, D. MPulse Mobile Sensing Model for Passive Detection of Impulsive Behavior: Exploratory Prediction Study. JMIR Ment. Health 2021, 8, e25019. [Google Scholar] [CrossRef]
- Wang, F.; Wang, Y.; Wang, J.; Xiong, H.; Zhao, J.; Zhang, D. Assessing Mental Stress Based on Smartphone Sensing Data: An Empirical Study. In Proceedings of the 2019 IEEE SmartWorld, Ubiquitous Intelligence and Computing, Advanced and Trusted Computing, Scalable Computing and Communications, Internet of People and Smart City Innovation (SmartWorld/UIC/ATC/SCALCOM/IOP/SCI), Leicester, UK, 19–23 August 2019; pp. 1031–1038. [Google Scholar] [CrossRef]
- Etienne, N.; Agu, E. Investigating Transfer Learning of Smartphone-Sensed Stress in University Populations. In Proceedings of the 2020 IEEE International Conference on Big Data (Big Data), Atlanta, GA, USA, 10–13 December 2020; pp. 4850–4858. [Google Scholar] [CrossRef]
- Byrne, M.L.; Lind, M.N.; Horn, S.R.; Mills, K.L.; Nelson, B.W.; Barnes, M.L.; Slavich, G.M.; Allen, N.B. Using Mobile Sensing Data to Assess Stress: Associations with Perceived and Lifetime Stress, Mental Health, Sleep, and Inflammation. Digit. Health 2021, 7. [Google Scholar] [CrossRef]
- Asare, K.O.; Visuri, A.; Ferreira, D.S.T. Towards Early Detection of Depression through Smartphone Sens-Ing. In Proceedings of the 2019 ACM International Joint Conference on Pervasive and Ubiquitous Computing and 2019 ACM International Symposium on Wearable Computers, London, UK, 9–13 September 2019; pp. 1158–1161. [Google Scholar] [CrossRef] [Green Version]
- Nguyen, B.; Kolappan, S.; Bhat, V.; Krishnan, S. Clustering and Feature Analysis of Smartphone Data for Depression Monitoring. In Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society, EMBS, Mexico, 1–5 November 2021; pp. 113–116. [Google Scholar] [CrossRef]
- Asare, K.O.; Terhorst, Y.; Vega, J.; Peltonen, E.; Lagerspetz, E.; Ferreira, D. Predicting Depression From Smartphone Behavioral Markers Using Machine Learning Methods, Hyperparameter Optimization, and Feature Importance Analysis: Exploratory Study. JMIR Mhealth Uhealth 2021, 9, e26540. [Google Scholar] [CrossRef]
- Müller, S.R.; Chen, X.; Peters, H.; Chaintreau, A.; Matz, S.C. Depression Predictions from GPS-Based Mobility Do Not Generalize Well to Large Demographically Heterogeneous Samples. Sci. Rep. 2021, 11, 14007. [Google Scholar] [CrossRef]
- Huckins, J.F.; DaSilva, A.W.; Hedlund, E.L.; Murphy, E.I.; Rogers, C.; Wang, W.; Obuchi, M.; Holtzheimer, P.E.; Wagner, D.D.; Campbell, A.T. Causal Factors of Anxiety and Depression in College Students: Longitudinal Ecological Momentary Assessment and Causal Analysis Using Peter and Clark Momentary Conditional Independence. JMIR Ment. Health 2020, 7, e16684. [Google Scholar] [CrossRef]
- di Matteo, D.; Fotinos, K.; Lokuge, S.; Mason, G.; Sternat, T.; Katzman, M.A.; Rose, J. Automated Screening for Social Anxiety, Generalized Anxiety, and Depression From Objective Smartphone-Collected Data: Cross-Sectional Study. J. Med. Internet Res. 2021, 23, e28918. [Google Scholar] [CrossRef]
- McIntyre, R.S.; Lee, Y.; Rong, C.; Rosenblat, J.D.; Brietzke, E.; Pan, Z.; Park, C.; Subramaniapillai, M.; Ragguett, R.M.; Mansur, R.B.; et al. Ecological Momentary Assessment of Depressive Symptoms Using the Mind.Me Application: Convergence with the Patient Health Questionnaire-9 (PHQ-9). J. Psychiatr. Res. 2021, 135, 311–317. [Google Scholar] [CrossRef]
- di Matteo, D.; Fotinos, K.; Lokuge, S.; Yu, J.; Sternat, T.; Katzman, M.A.; Rose, J. The Relationship Between Smartphone-Recorded Environmental Audio and Symptomatology of Anxiety and Depression: Exploratory Study. JMIR Form. Res. 2020, 4, e18751. [Google Scholar] [CrossRef] [PubMed]
- Yue, C.; Ware, S.; Morillo, R.; Lu, J.; Shang, C.; Bi, J.; Kamath, J.; Russell, A.; Bamis, A.; Wang, B. Automatic Depression Prediction Using Internet Traffic Characteristics on Smartphones. Smart Health 2020, 18, 100137. [Google Scholar] [CrossRef] [PubMed]
- Ware, S.; Yue, C.; Morillo, R.; Lu, J.; Shang, C.; Bi, J.; Kamath, J.; Russell, A.; Bamis, A.; Wang, B. Predicting Depressive Symptoms Using Smartphone Data. Smart Health 2020, 15, 100093. [Google Scholar] [CrossRef]
- Chow, P.I.; Fua, K.; Huang, Y.; Bonelli, W.; Xiong, H.; Barnes, L.E.; Teachman, B.A. Using Mobile Sensing to Test Clinical Models of Depression, Social Anxiety, State Affect, and Social Isolation Among College Students. J. Med. Internet Res. 2017, 19, e6820. [Google Scholar] [CrossRef]
- Fulford, D.; Mote, J.; Gonzalez, R.; Abplanalp, S.; Zhang, Y.; Luckenbaugh, J.; Onnela, J.P.; Busso, C.; Gard, D.E. Smartphone Sensing of Social Interactions in People with and without Schizophrenia. J. Psychiatr. Res. 2021, 137, 613–620. [Google Scholar] [CrossRef]
- Wang, R.; Wang, W.; Aung, M.S.H.; Ben-Zeev, D.; Brian, R.; Campbell, A.T.; Choudhury, T.; Hauser, M.; Kane, J.; Scherer, E.A.; et al. Predicting Symptom Trajectories of Schizophrenia Using Mobile Sensing. Proc. ACM Interact. Mob. Wearable Ubiquitous Technol. 2017, 1, 1–24. [Google Scholar] [CrossRef] [Green Version]
- Wang, W.; Mirjafari, S.; Harari, G.; Ben-Zeev, D.; Brian, R.; Choudhury, T.; Hauser, M.; Kane, J.; Masaba, K.; Nepal, S.; et al. Social Sensing: Assessing Social Functioning of Patients Living with Schizophrenia Using Mobile Phone Sensing. In Proceedings of the Conference on Human Factors in Computing Systems, Honolulu, HI, USA, 25–30 April 2020. [Google Scholar] [CrossRef]
- Jongs, N.; Jagesar, R.; van Haren, N.E.M.; Penninx, B.W.J.H.; Reus, L.; Visser, P.J.; van der Wee, N.J.A.; Koning, I.M.; Arango, C.; Sommer, I.E.C.; et al. A Framework for Assessing Neuropsychiatric Phenotypes by Using Smartphone-Based Location Data. Transl. Psychiatry 2020, 10, 211. [Google Scholar] [CrossRef]
- Ebner-Priemer, U.W.; Mühlbauer, E.; Neubauer, A.B.; Hill, H.; Beier, F.; Santangelo, P.S.; Ritter, P.; Kleindienst, N.; Bauer, M.; Schmiedek, F.; et al. Digital Phenotyping: Towards Replicable Findings with Comprehensive Assessments and Integrative Models in Bipolar Disorders. Int. J. Bipolar Disord. 2020, 8, 35. [Google Scholar] [CrossRef]
- Busk, J.; Faurholt-Jepsen, M.; Frost, M.; Bardram, J.E.; Kessing, L.V.; Winther, O. Forecasting Mood in Bipolar Disorder From Smartphone Self-Assessments: Hierarchical Bayesian Approach. JMIR Mhealth Uhealth 2020, 8, e15028. [Google Scholar] [CrossRef] [Green Version]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The PHQ-9: Validity of a Brief Depression Severity Measure. J. Gen. Intern. Med. 2001, 16, 606. [Google Scholar] [CrossRef]
- Russell, D.W. UCLA Loneliness Scale (Version 3): Reliability, Validity, and Factor Structure. J. Personal. Assess. 2010, 66, 20–40. [Google Scholar] [CrossRef] [PubMed]
- Shiffman, S.; Stone, A.A.; Hufford, M.R. Ecological Momentary Assessment. Annu. Rev. Clin. Psychol. 2008, 4, 1–32. [Google Scholar] [CrossRef] [PubMed]
- Rooksby, J.; Morrison, A.; Murray-Rust, D. Student Perspectives on Digital Phenotyping the Acceptability of Using Smartphone Data to Assess Mental Health. In Proceedings of the Conference on Human Factors in Computing Systems, Glasgow, UK, 4–9 May 2019; p. 14. [Google Scholar] [CrossRef] [Green Version]
- di Matteo, D.; Fine, A.; Fotinos, K.; Rose, J.; Katzman, M. Patient Willingness to Consent to Mobile Phone Data Collection for Mental Health Apps: Structured Questionnaire. JMIR Ment. Health 2018, 5, e9539. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- González-Pérez Ignacio Miralles, A.; Granell Sven Casteleyn, C.; González-Pérez, A.; Miralles, I.; Granell, C. Technical Challenges to Deliver Sensor-Based Psy-Chological Interventions Using Smartphones. In Proceedings of the 2019 ACM International Joint Conference on Pervasive and Ubiquitous Computing and 2019 ACM International Symposium on Wearable Computers, London, UK, 9–13 September 2019. [Google Scholar] [CrossRef]
- Tonti, S.; Marzolini, B.; Bulgheroni, M. Smartphone-Based Passive Sensing for Behavioral and Physical Monitoring in Free-Life Conditions: Technical Usability Study. JMIR Biomed. Eng. 2021, 6, e15417. [Google Scholar] [CrossRef]
- Keusch, F.; Wenz, A.; Conrad, F. Do You Have Your Smartphone with You? Behavioral Barriers for Measuring Everyday Activities with Smartphone Sensors. Comput. Hum. Behav. 2022, 127, 107054. [Google Scholar] [CrossRef]
- Harari, G.M. A Process-Oriented Approach to Respecting Privacy in the Context of Mobile Phone Tracking. Curr. Opin. Psychol. 2020, 31, 141–147. [Google Scholar] [CrossRef]
- Breslin, S.; Shareck, M.; Fuller, D. Research Ethics for Mobile Sensing Device Use by Vulnerable Populations. Soc. Sci. Med. 2019, 232, 50–57. [Google Scholar] [CrossRef]
- Delgado-Santos, P.; Stragapede, G.; Tolosana, R.; Guest, R.; Deravi, F.; Vera-Rodriguez, R. A Survey of Privacy Vulnerabilities of Mobile Device Sensors. ACM Comput. Surv. 2021. [Google Scholar] [CrossRef]
- Beierle, F.; Tran, V.T.; Allemand, M.; Neff, P.; Schlee, W.; Probst, T.; Zimmermann, J.; Pryss, R. What Data Are Smartphone Users Willing to Share with Researchers?: Designing and Evaluating a Privacy Model for Mobile Data Collection Apps. J. Ambient. Intell. Humaniz. Comput. 2020, 11, 2277–2289. [Google Scholar] [CrossRef]
- Mulvenna, M.D.; Bond, R.; Delaney, J.; Dawoodbhoy, F.M.; Boger, J.; Potts, C.; Turkington, R. Ethical Issues in Democratizing Digital Phenotypes and Machine Learning in the Next Generation of Digital Health Technologies. Philos. Technol. 2021, 34, 1945–1960. [Google Scholar] [CrossRef]
- Experience Sampling—MovisensXS—Movisens GmbH. Available online: https://www.movisens.com/en/products/movisensxs/ (accessed on 27 April 2022).
- Behapp—Digital Phenotyping. Available online: https://www.behapp.com/ (accessed on 27 April 2022).
- EARS—Ksana Health. Available online: https://ksanahealth.com/ears/ (accessed on 27 April 2022).
- Lathia, N.; Rachuri, K.K.; Mascolo, C.; Roussos, G. Open Source Smartphone Libraries for Computational Social Science. In Proceedings of the 2013 ACM Conference on Ubiquitous Computing, Zurich, Switzerland, 8–12 September 2013; pp. 911–919. [Google Scholar] [CrossRef] [Green Version]
- Ranjan, Y.; Rashid, Z.; Stewart, C.; Conde, P.; Begale, M.; Verbeeck, D.; Boettcher, S.; Dobson, R.; Folarin, A. RADAR-Base: Open Source Mobile Health Platform for Collecting, Monitoring, and Analyzing Data Using Sensors, Wearables, and Mobile Devices. JMIR Mhealth Uhealth 2019, 7, e11734. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bulling, A.; Blanke, U.; Schiele, B. A Tutorial on Human Activity Recognition Using Body-Worn Inertial Sensors. ACM Comput. Surv. 2014, 46, 1–33. [Google Scholar] [CrossRef]
- Parra, L.; Sendra, S.; Jiménez, J.M.; Lloret, J. Multimedia Sensors Embedded in Smartphones for Ambient Assisted Living and E-Health. Multimed. Tools Appl. 2016, 75, 13271–13297. [Google Scholar] [CrossRef] [Green Version]
- Mental Health. Available online: https://www.who.int/health-topics/mental-health#tab=tab_2 (accessed on 28 April 2022).
- Mental Health—Our World in Data. Available online: https://ourworldindata.org/mental-health (accessed on 28 April 2022).
- Schwenk, M.; Mohler, J.; Wendel, C.; D’Huyvetter, K.; Fain, M.; Taylor-Piliae, R.; Najafi, B. Wearable Sensor-Based In-Home Assessment of Gait, Balance, and Physical Activity for Discrimination of Frailty Status: Baseline Results of the Arizona Frailty Cohort Study. Gerontology 2015, 61, 258–267. [Google Scholar] [CrossRef] [Green Version]
- Wang, J.B.; Cadmus-Bertram, L.A.; Natarajan, L.; White, M.M.; Madanat, H.; Nichols, J.F.; Ayala, G.X.; Pierce, J.P. Wearable Sensor/Device (Fitbit One) and SMS Text-Messaging Prompts to Increase Physical Activity in Overweight and Obese Adults: A Randomized Controlled Trial. Telemed. E-Health 2015, 21, 782–792. [Google Scholar] [CrossRef] [Green Version]
- Papagiannaki, A.; Zacharaki, E.I.; Kalouris, G.; Kalogiannis, S.; Deltouzos, K.; Ellul, J.; Megalooikonomou, V. Recognizing Physical Activity of Older People from Wearable Sensors and Inconsistent Data. Sensors 2019, 19, 880. [Google Scholar] [CrossRef] [Green Version]
- Rao, A.K. Wearable Sensor Technology to Measure Physical Activity (PA) in the Elderly. Curr. Geriatr. Rep. 2019, 8, 55–66. [Google Scholar] [CrossRef]
- Luo, H.; Lee, P.A.; Clay, I.; Jaggi, M.; de Luca, V. Assessment of Fatigue Using Wearable Sensors: A Pilot Study. Digit. Biomark. 2020, 4, 59–72. [Google Scholar] [CrossRef]
- AWARE—Open-Source Context Instrumentation Framework for Everyone. Available online: https://awareframework.com/ (accessed on 30 April 2022).
- Home—RADAR-Base. Available online: https://radar-base.org/ (accessed on 30 April 2022).
- Ordóñez, F.J.; Roggen, D.; Liu, Y.; Xiao, W.; Chao, H.-C.; Chu, P. Deep Convolutional and LSTM Recurrent Neural Networks for Multimodal Wearable Activity Recognition. Sensors 2016, 16, 115. [Google Scholar] [CrossRef] [Green Version]
- Hammerla, N.Y.; Kirkham, R.; Andras, P.; Plötz, T. On Preserving Statistical Characteristics of Accelerometry Data Using Their Empirical Cumulative Distribution. In Proceedings of the 17th Annual International Symposium on International Symposium on Wearable Computers, Zurich, Switzerland, 8–12 September 2013. [Google Scholar] [CrossRef]
- Ben-Zeev, D.; Scherer, E.A.; Wang, R.; Xie, H. Next-Generation Psychiatric Assessment: Using Smartphone Sensors to Monitor Behavior and Mental Health. Psychiatr. Rehabil. J. 2015, 38, 218–226. [Google Scholar] [CrossRef] [Green Version]
- Harari, G.M.; Lane, N.D.; Wang, R.; Crosier, B.S.; Campbell, A.T.; Gosling, S.D. Using Smartphones to Collect Behavioral Data in Psychological Science: Opportunities, Practical Considerations, and Challenges. Perspect. Psychol. Sci. 2016, 11, 838–854. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, H.N.; Seo, K. Smartphone-Based Health Program for Improving Physical Activity and Tackling Obesity for Young Adults: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2019, 17, 15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- de Vries, L.P.; Baselmans, B.M.L.; Bartels, M. Smartphone-Based Ecological Momentary Assessment of Well-Being: A Systematic Review and Recommendations for Future Studies. J. Happiness Stud. 2021, 22, 2361–2408. [Google Scholar] [CrossRef] [PubMed]
- Trifan, A.; Oliveira, M.; Oliveira, J.L. Passive Sensing of Health Outcomes Through Smartphones: Systematic Review of Current Solutions and Possible Limitations. JMIR Mhealth Uhealth 2019, 7, e12649. [Google Scholar] [CrossRef]
- Bardram, J.E.; Matic, A. A Decade of Ubiquitous Computing Research in Mental Health. IEEE Pervasive Comput. 2020, 19, 62–72. [Google Scholar] [CrossRef]
- Antosik-Wójcińska, A.Z.; Dominiak, M.; Chojnacka, M.; Kaczmarek-Majer, K.; Opara, K.R.; Radziszewska, W.; Olwert, A.; Święcicki, Ł. Smartphone as a Monitoring Tool for Bipolar Disorder: A Systematic Review Including Data Analysis, Machine Learning Algorithms and Predictive Modelling. Int. J. Med. Inform. 2020, 138, 104131. [Google Scholar] [CrossRef]
- Bauer, M.; Glenn, T.; Geddes, J.; Gitlin, M.; Grof, P.; Kessing, L.V.; Monteith, S.; Faurholt-Jepsen, M.; Severus, E.; Whybrow, P.C. Smartphones in Mental Health: A Critical Review of Background Issues, Current Status and Future Concerns. Int. J. Bipolar Disord. 2020, 8, 2. [Google Scholar] [CrossRef]
- Binns, R.; Kirkham, R. How Could Equality and Data Protection Law Shape AI Fairness for People with Disabilities? ACM Trans. Access. Comput. 2021, 14, 1–32. [Google Scholar] [CrossRef]
- Ferguson, C.; Hickman, L.D.; Turkmani, S.; Breen, P.; Gargiulo, G.; Inglis, S.C. “Wearables Only Work on Patients That Wear Them”: Barriers and Facilitators to the Adoption of Wearable Cardiac Monitoring Technologies. Cardiovasc. Digit. Health J. 2021, 2, 137–147. [Google Scholar] [CrossRef]
- Sergueeva, K.; Shaw, N.; Lee, S.H. Understanding the Barriers and Factors Associated with Consumer Adoption of Wearable Technology Devices in Managing Personal Health. Can. J. Adm. Sci. Rev. Can. Sci. L’adm. 2020, 37, 45–60. [Google Scholar] [CrossRef]
- Loncar-Turukalo, T.; Zdravevski, E.; da Silva, J.M.; Chouvarda, I.; Trajkovik, V. Literature on Wearable Technology for Connected Health: Scoping Review of Research Trends, Advances, and Barriers. J. Med. Internet Res. 2019, 21, e14017. [Google Scholar] [CrossRef] [PubMed]
- Nolazco-Flores, J.A.; Faundez-Zanuy, M.; Velázquez-Flores, O.A.; Del-Valle-Soto, C.; Cordasco, G.; Esposito, A. Mood State Detection in Handwritten Tasks Using PCA–MFCBF and Automated Machine Learning. Sensors 2022, 22, 1686. [Google Scholar] [CrossRef] [PubMed]
- Baumeister, H.; Kraft, R.; Baumel, A.; Pryss, R.; Messner, E.-M. Persuasive E-Health Design for Behavior Change. In Digital Phenotyping and Mobile Sensing; Springer: Cham, Switzerland, 2019; pp. 261–276. [Google Scholar] [CrossRef]


| Advantages | Disadvantages |
|---|---|
| Highly customizable and can collect as much or as little data required [83] | Requires regular user input, places burden on the user. This may impact user acceptance, compliance, and retention [61,99]. |
| Ability to collect data about conditions that cannot be sensed directly, such as mental health [16,70,95] | Self-reported data can be subjective and susceptible to bias [2,20,100] |
| Ability to provide additional context or complementary data to passively sensed data [11,53,57,88] | Reliance on user memory and recall, which may not always be accurate [70,81]. |
| Sensor (S)/ Software Feature (SF) | What Does It Collect? | What Has It Been Used for? | Key Advantages (+)/Disadvantages (−) |
|---|---|---|---|
| Accelerometer (S) | Acceleration forces along x, y, and z axes of the device | It has been used to detect physical activity (such as standing, walking, running, etc.) and sedentary behavior [11,23,53]. Physical activity has also been used to infer mental wellbeing of individuals [15,67,92] (e.g., decline in physical activity impacting mental health) | + Relatively privacy-sensitive. + Low power − Accuracy impacted by sampling rate. − Performance negatively impacted by device placement. |
| Ambient Light (S) | Amount of light the device is exposed to | It has been used alongside other sensors to understand the user surroundings. Studies used the data to infer when the user was asleep [13,57,58] and infer the amount of spent in the dark, which could provide an indication of mood/mental health [15,26,80] | − Only able to make very limited inferences by itself, used in conjunction with other sensors − Potentially impacted by device placement |
| Application usage (SF) | Information about the applications used on the device | It has been used to infer the communication behavior of users. Information such as application use time and genres of applications (e.g., social media) used provided an insight into the user’s sociability and wellbeing [55,70,92]. | + Can be used to infer a wide range of user interactions − Privacy concerns depending on what information is captured. |
| Battery status (SF) | Indicates the phone charging status (on/off) | It was used as a proxy measure to infer phone-usage behavior. For example, studies monitoring sleep used it as an indicator of the person sleeping, assuming they charge their phone overnight [19,57]. | + Privacy-sensitive − Only able to make limited inferences by itself, used in conjunction with other sensors |
| Bluetooth (S) | Information about nearby Bluetooth-enabled devices | It has been used to infer the sociability of the user. By collecting information such as count of nearby Bluetooth devices, number of recurring devices etc., studies were able to infer the social context of users [9,61,76]. | − Not all nearby devices may have Bluetooth turned on |
| Camera (S) | Capture images and videos | It has been used to infer the user’s emotions by capturing facial images [71]. Another study used the camera to capture eye-movement data and checked if such features could provide an indication of the user emotions [74]. | + Ability to visually monitor user behavior − Higher impact on battery life − Relatively serious privacy concerns, due to video recording. |
| Global Positioning System (GPS) (S) | Latitudinal and longitudinal coordinates indicating physical location | It has been used to infer the mobility of a user (number of places visited, time spent outdoors, time spent at home) which has an impact on wellbeing [26,27,84] (e.g., too much time spent at home indicating a decline in sociability and in turn mental health [7]) | + Can use location to make a wide range of inferences about behavior and wellbeing. − Higher impact on battery life compared to other modes of sensing. − Privacy concerns, especially when used with a high degree of granularity. |
| Gyroscope (S) | Rotational forces along the x, y, and z axes of the device | It has been used in conjunction with the accelerometer for activity recognition. Assisted in detecting activities such as walking, standing, laying etc. [11,30,49] | + Can increase recognition accuracy compared to an accelerometer alone, due to the provision of additional rotational information. + Low power − Impacted by device placement |
| Microphone (S) | Collect audio recordings from the surroundings | It has been used to infer surrounding sound, which can provide information about the user’s context. Some studies used it to detect if the user was alone (i.e., sociability) by listening for conversation [3,54,84]. Some used it to detect if the user was sleeping if the surroundings were quiet (along with other sensor data such as light) [57,58]. | + Has utility in respect of social sensing. − Impacted by device placement − Relatively serious privacy concerns due to audio recording. |
| Phone lock/unlock status (SF) | Indicates whether the phone is locked or unlocked | It was used to infer phone usage behavior. By calculating the time between the unlock and lock states, studies estimated the phone usage time [24,25,91]. Additionally, this was also used as one of the factors to infer sleep (i.e., phone in locked state for long time during bedtime hours) [57,58,91] | + Privacy-sensitive. − Unreliable by itself, used in conjunction with other sensors |
| Phone-call and text-message logs (SF) | Logs/records of text messages and phone calls | It has been used to infer the communication patterns of users, which correlate to social wellbeing. For example, decreased frequency of such communication features could indicate decreased sociability of individuals [55,69,85] | − Privacy concerns depending on what information is captured. |
| Screen status (S) | Indicates screen on/off status | Similar to phone lock/unlock status, it was used to infer phone-user behavior. Screen on/off indicated when the device was being used, which could further indicate distracted/anxious behavior [84], or infer sleep [19,91] | − Unreliable by itself, used in conjunction with other sensors − Can be impacted by phone notifications (resulting in screen on state) |
| Wi-Fi (S) | Indicates nearby Wi-Fi connectivity | These types of data were used as a complimentary source to infer location and indicated indoor mobility [8,51,60,88] | + Can increase accuracy of location determination |
| Name [Original Ref] | Platforms Supported | Codebase | Last Updated (Year) | Cited by |
|---|---|---|---|---|
| AWARE [32] | Android, iOS | Android: https://github.com/denzilferreira/aware-client (accessed on 1 May 2022) iOS: https://github.com/tetujin/aware-client-ios-v2 (accessed on 1 May 2022) | Android: 2020 iOS: 2021 | [12,62,75,79] |
| Beiwe (Both open-source and Software-as-a-Service (SaaS) framework for data collection and analysis) [33] | Android, iOS | https://github.com/onnela-lab (accessed on 1 May 2022) | Android: 2021 iOS: 2022 | [9,50] |
| EARS (Initially open-source, now available as SaaS for data collection and analysis [34,111]) [34] | Android, iOS | https://github.com/C4DMH (accessed on 1 May 2022) | Android: 2020 iOS: 2020 | [78] |
| Emotion Sense [112] | Android | https://github.com/emotionsense (accessed on 1 May 2022) | 2017 Project is no longer maintained | [8,88] |
| RADAR—base [113] | Android, iOS | https://github.com/RADAR-base (accessed on 1 May 2022) | Android: 2022 iOS: 2021 | [7] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kulkarni, P.; Kirkham, R.; McNaney, R. Opportunities for Smartphone Sensing in E-Health Research: A Narrative Review. Sensors 2022, 22, 3893. https://doi.org/10.3390/s22103893
Kulkarni P, Kirkham R, McNaney R. Opportunities for Smartphone Sensing in E-Health Research: A Narrative Review. Sensors. 2022; 22(10):3893. https://doi.org/10.3390/s22103893
Chicago/Turabian StyleKulkarni, Pranav, Reuben Kirkham, and Roisin McNaney. 2022. "Opportunities for Smartphone Sensing in E-Health Research: A Narrative Review" Sensors 22, no. 10: 3893. https://doi.org/10.3390/s22103893
APA StyleKulkarni, P., Kirkham, R., & McNaney, R. (2022). Opportunities for Smartphone Sensing in E-Health Research: A Narrative Review. Sensors, 22(10), 3893. https://doi.org/10.3390/s22103893






