The Hemodynamic Parameters Values Prediction on the Non-Invasive Hydrocuff Technology Basis with a Neural Network Applying
Abstract
:1. Introduction
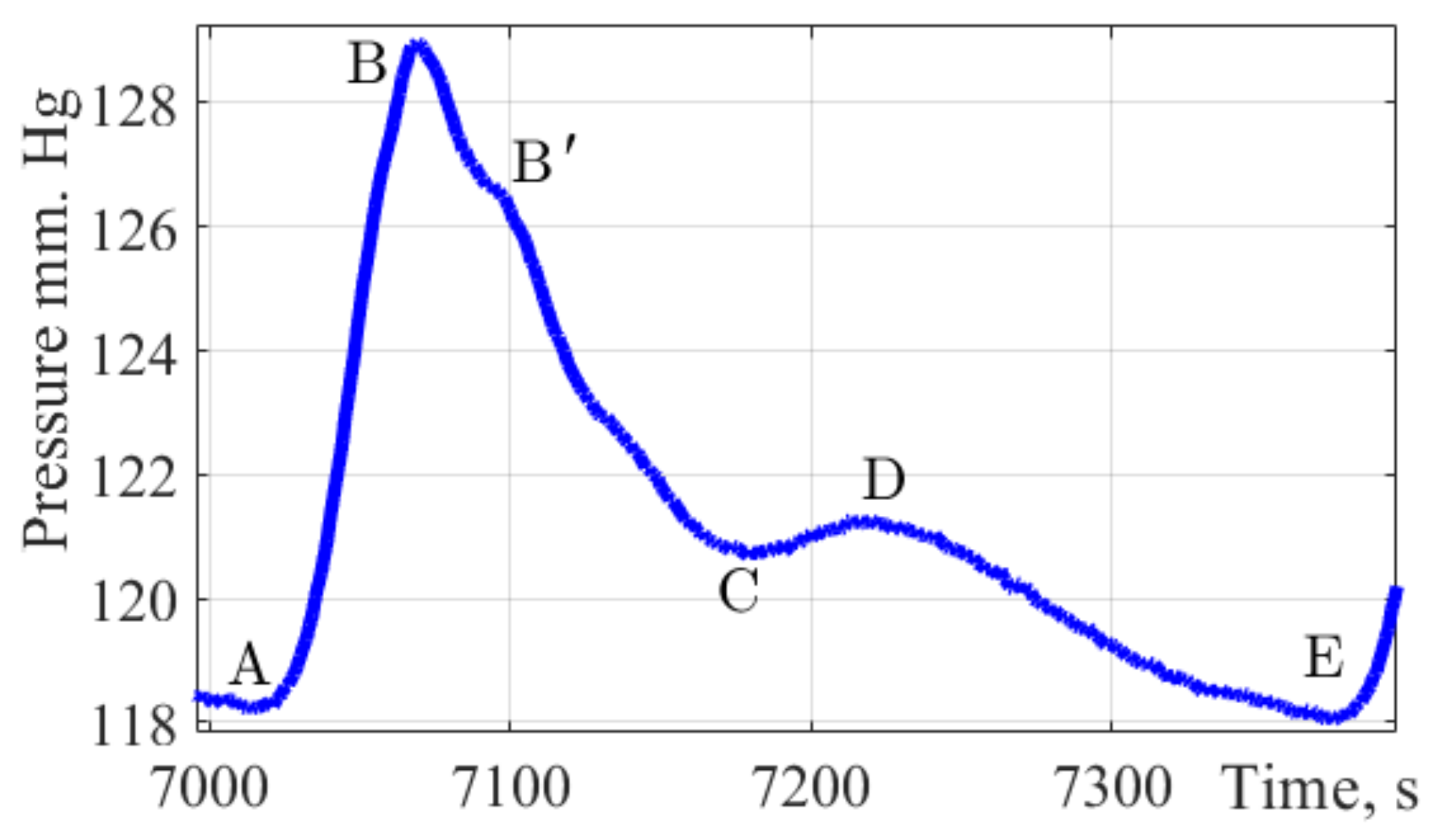
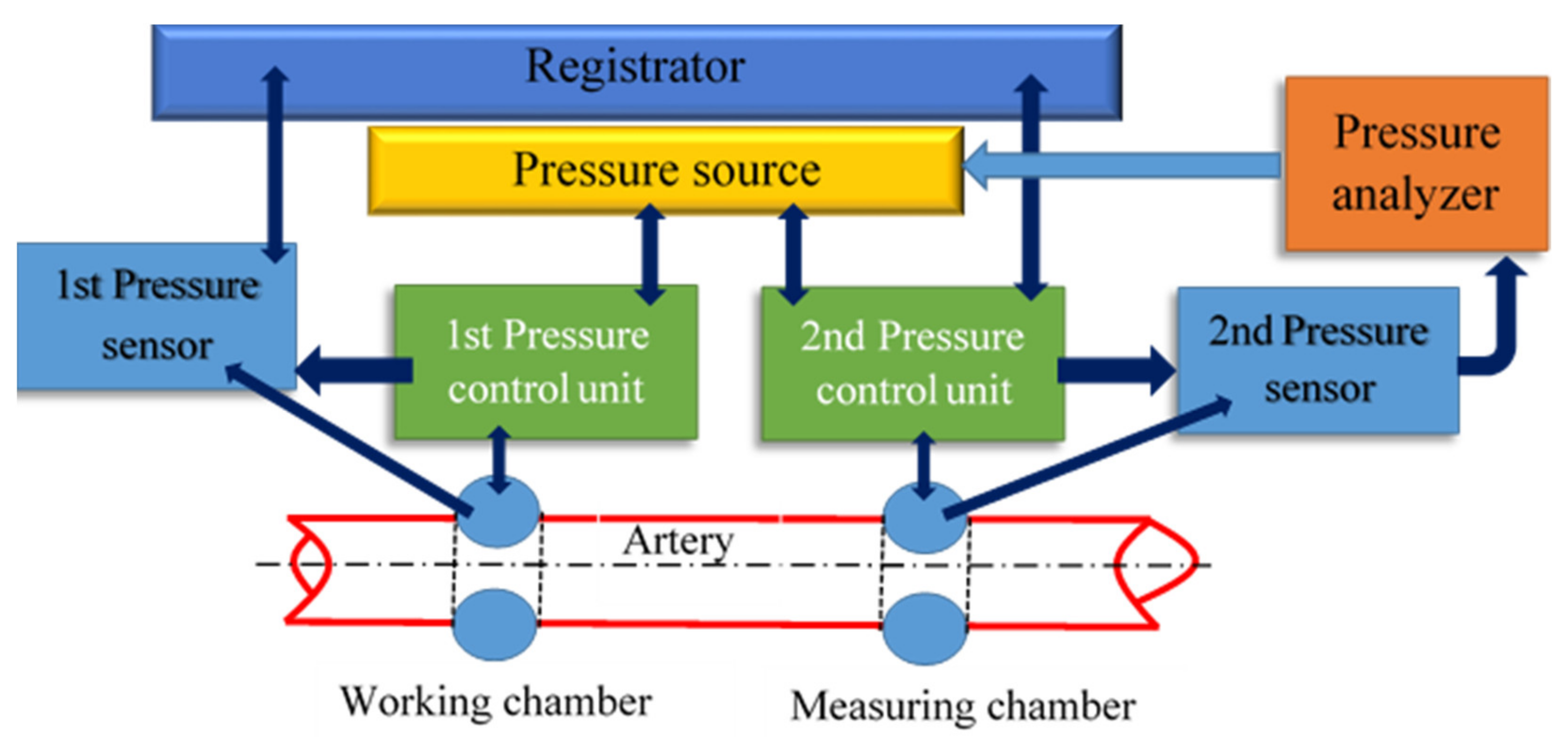
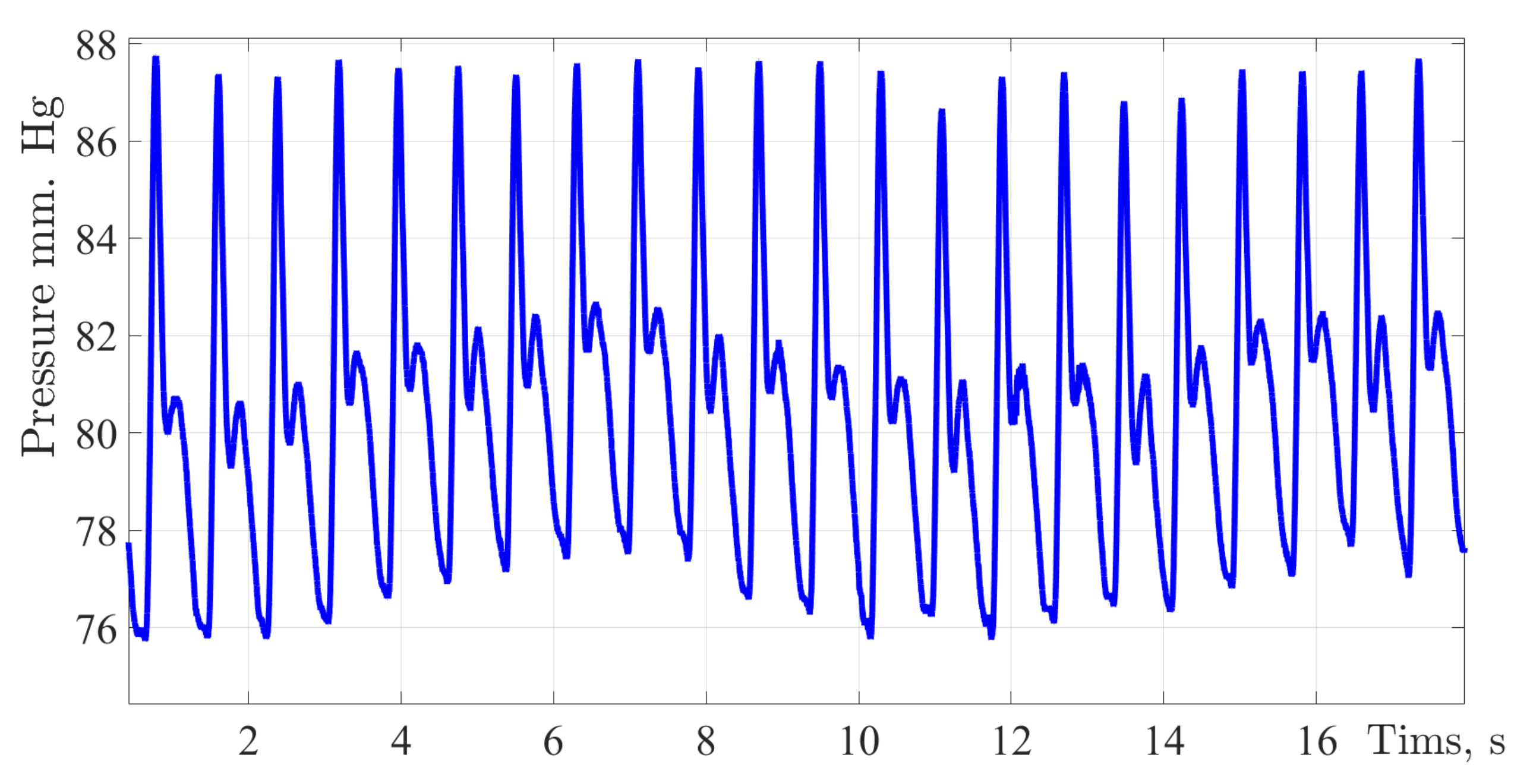
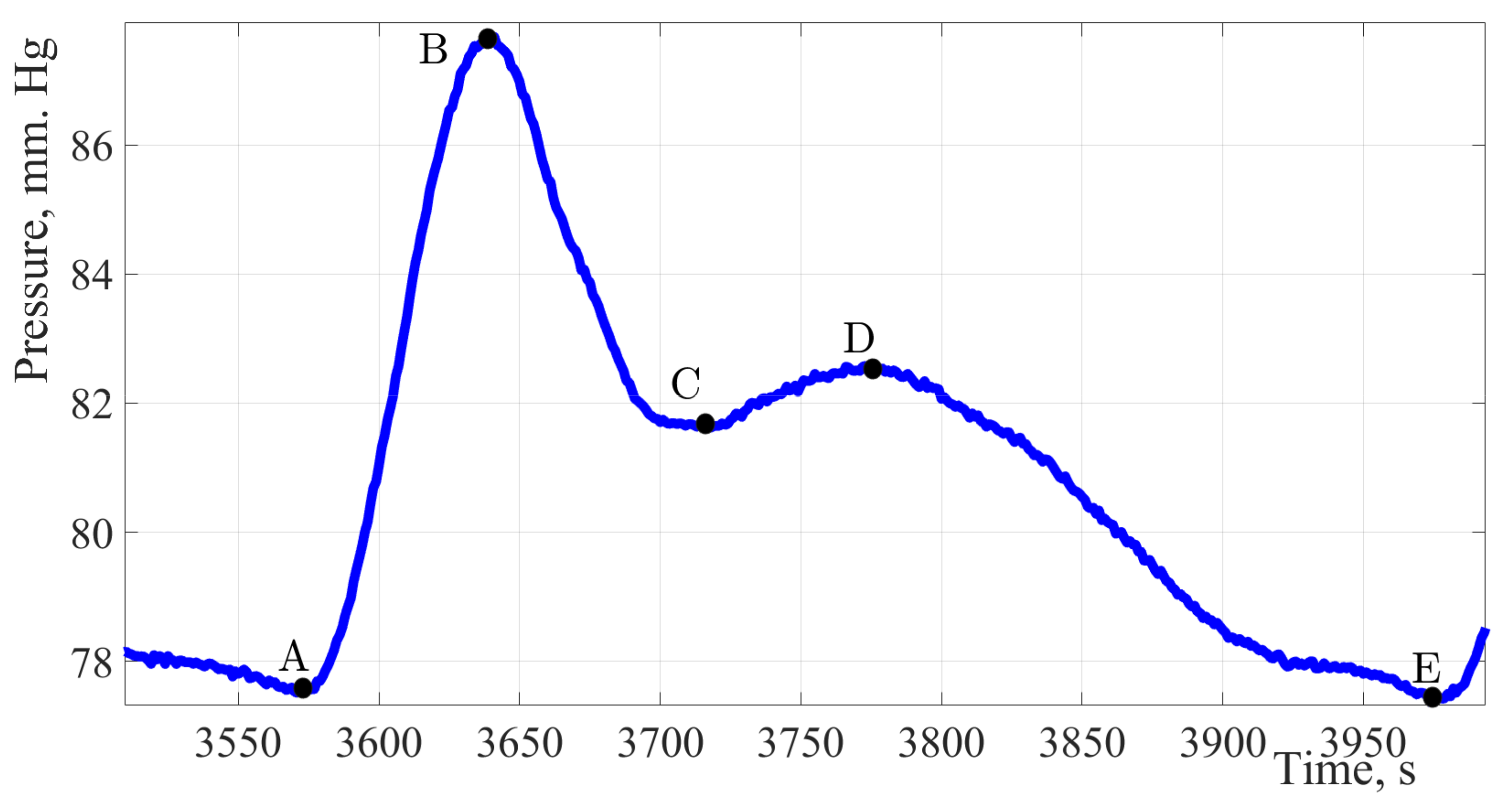
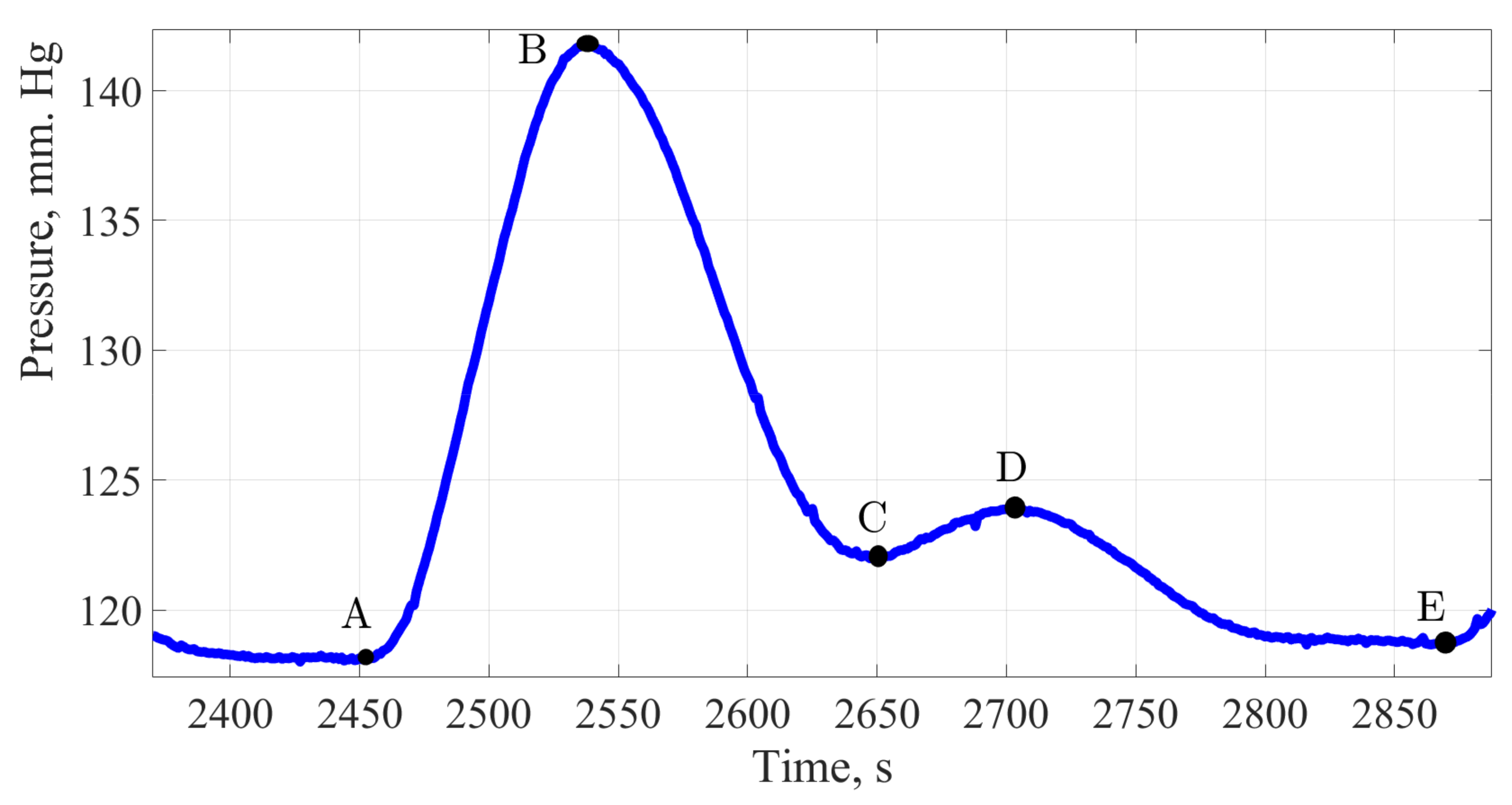
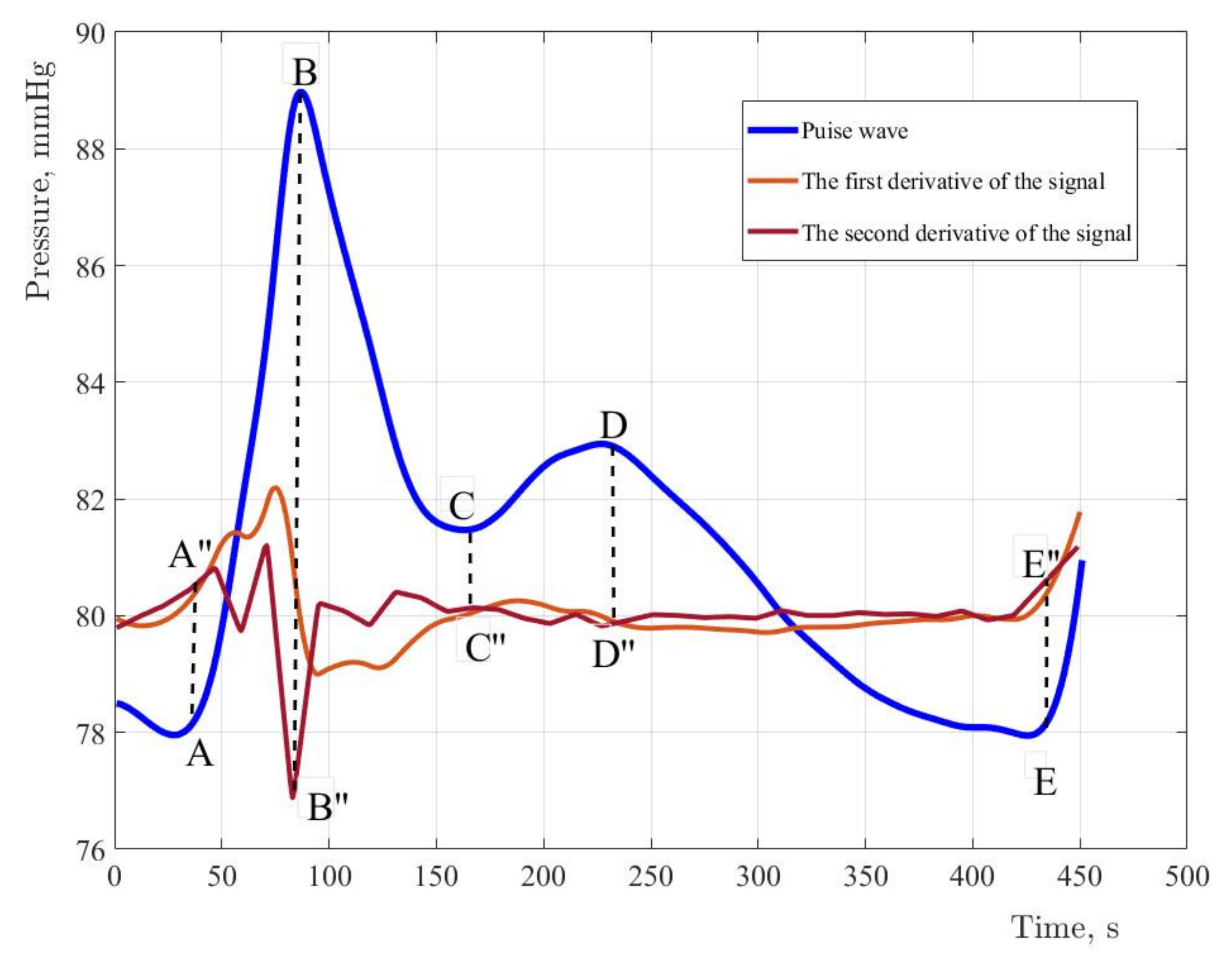
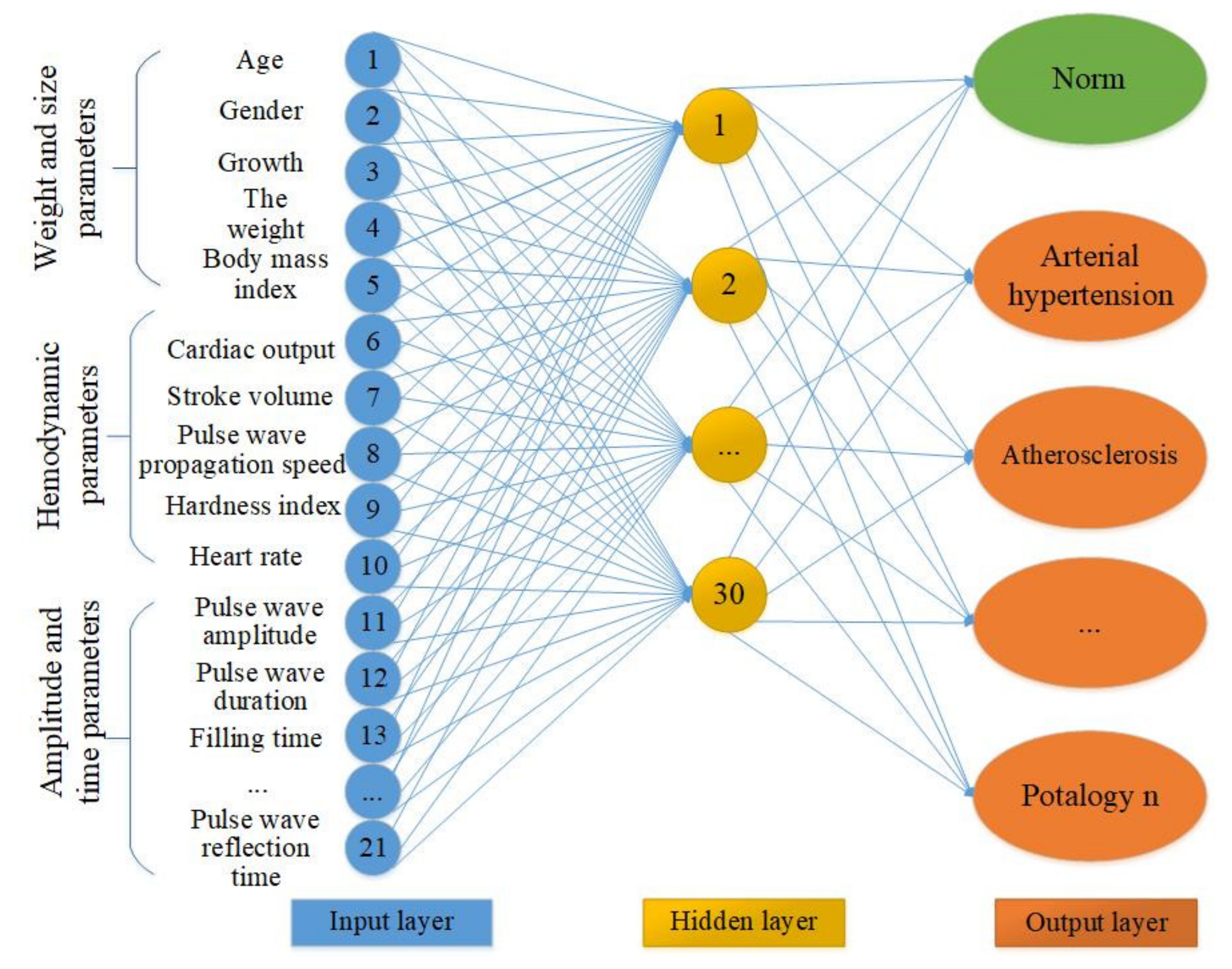
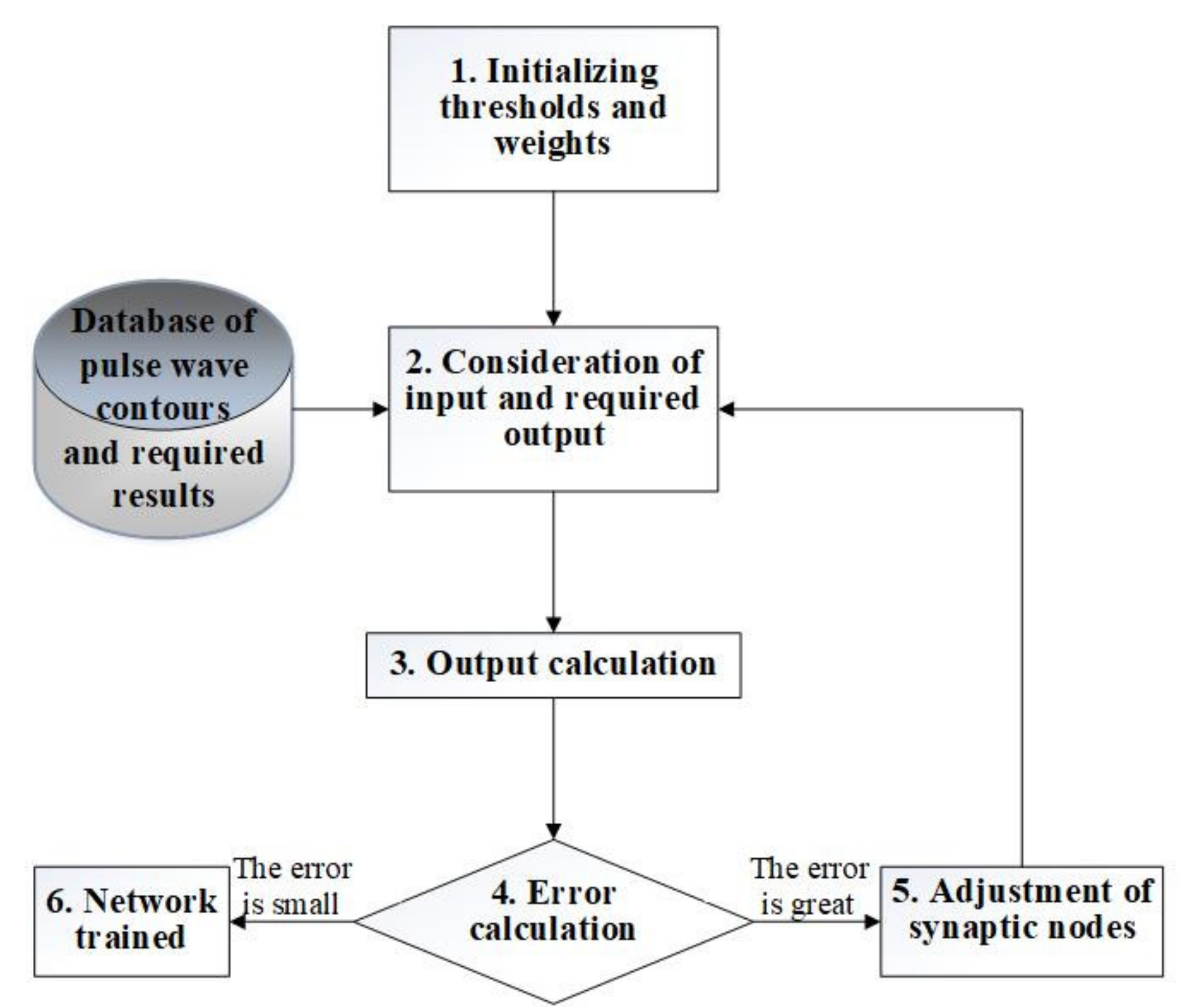
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Alhashemi, J.A.; Cecconi, M.; Hofer, C.K. Cardiac output monitoring: An integrative perspective. In Annual Update in Intensive Care and Emergency Medicine; Vincent, J.-L., Ed.; Springer: Berlin/Heidelberg, Germany, 2011; pp. 443–456. [Google Scholar]
- Naik, K.; Bhathawala, P.H. Mathematical Modeling of Human Cardiovascular System: A Lumped Parameter Approach and Simulation. Int. J. Math. Comput. Phys. Electr. Comput. Eng. 2017, 11, 73–84. [Google Scholar]
- Quarteroni, A.; Manzoni, A.; Vergara, C. The cardiovascular system: Mathematical modelling, numerical algorithms and clinical applications. Acta Numer. 2017, 26, 365–590. [Google Scholar] [CrossRef] [Green Version]
- Karavaev, A.S.; Ishbulatov, Y.M.; Ponomarenko, V.I.; Prokhorov, M.D.; Gridnev, V.I.; Bezruchko, B.P.; Kiselev, A.R. Model of human cardiovascular system with a loop of autonomic regulation of the mean arterial pressure. J. Am. Soc. Hypertens. 2016, 10, 235–243. [Google Scholar] [CrossRef] [PubMed]
- Gerashchenko, M.S.; Markuleva, M.V.; Gerashchenko, S.I.; Polosin, V.G. Hydrocuff Oscillations Formation Process Modeling. In Proceedings of the 2019 International Multi-Conference on Engineering, Computer and Information Sciences (SIBIRCON), Novosibirsk, Russia, 21–27 October 2019; pp. 442–445. [Google Scholar] [CrossRef]
- Yadav, S.S.; Jadhav, S.M. Deep convolutional neural network based medical image classification for disease diagnosis. J. Big Data 2019, 6, 113. [Google Scholar] [CrossRef] [Green Version]
- Anwar, S.M.; Majid, M.; Qayyum, A.; Awais, M.; Alnowami, M.; Khan, M.K. Medical Image Analysis using Convolutional Neural Networks: A Review. J. Med. Syst. 2018, 42, 226. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Markuleva, M.V.; Gerashchenko, M.S.; Voronin, S.V.; Gerashchenko, S.I.; Mitroshin, A.N. The neuronet method for pulse wave analysis by hydro-cuff technology at cardiovascular system diagnosis. J. Phys. Conf. Ser. 2020, 1679, 022081. [Google Scholar] [CrossRef]
- Harjai, S.; Khatri, S.K. An Intelligent Clinical Decision Support System Based on Artificial Neural Network for Early Diagnosis of Cardiovascular Diseases in Rural Areas. In Proceedings of the 2019 Amity International Conference on Artificial Intelligence (AICAI), Dubai, United Arab Emirates, 4–6 February 2019; pp. 729–736. [Google Scholar] [CrossRef]
- Konnova, N.; Basarab, M.; Khachatryan, M.; Domracheva, A.; Ivanov, I. Convolutional neural networks application in cardiovascular decision support systems. In Proceedings of the 2019 International Conference on Image and Video Processing, and Artificial Intelligence, Shanghai, China, 23–25 August 2019; Volume 11321, p. 113212D. [Google Scholar] [CrossRef]
- Shah, S.R.; Kumar, R. Mathematical Modeling of Blood Flow with the Suspension of Nanoparticles through a Tapered Artery with a Blood Clot. Front. Nanotechnol. 2020, 2, 596475. [Google Scholar] [CrossRef]
- Sankar, D.S.; Yatim, Y. Comparative Analysis of Mathematical Models for Blood Flow in Tapered Constricted Arteries. Abstr. Appl. Anal. 2012, 2012, 235960. [Google Scholar] [CrossRef]
- Avgerinos, N.A.; Neofytou, P. Mathematical Modelling and Simulation of Atherosclerosis Formation and Progress: A Review. Ann. Biomed. Eng. 2019, 47, 1764–1785. [Google Scholar] [CrossRef]
- Ford, S.; Birmingham, E.; King, A.; Lim, J.; Ansermino, J.M. At-a-Glance Monitoring: Covert Observations of Anesthesiologists in the Operating Room. Anesth. Analg. 2010, 111, 653–658. [Google Scholar] [CrossRef]
- Xiao, H.; Zhang, Y.; Yin, H.; Liu, P.; Liu, D. Early Diagnosis of Carotid Stenosis by Ultrasound Doppler Investigations: A Classification Method for the Hemodynamic Parameter. Information 2020, 11, 493. [Google Scholar] [CrossRef]
- Wüst, R.C.; Calcagno, C.; Daal, M.R.; Nederveen, A.J.; Coolen, B.; Strijkers, G. Emerging Magnetic Resonance Imaging Techniques for Atherosclerosis Imaging. Arterioscler. Thromb. Vasc. Biol. 2019, 39, 841–849. [Google Scholar] [CrossRef]
- Drzewiecki, G.; Hood, R.; Apple, H. Theory of the oscillometric maximum and the systolic and diastolic detection ratios. Ann. Biomed. Eng. 1994, 22, 88–96. [Google Scholar] [CrossRef]
- El-Hajj, C.; Kyriacou, P. A review of machine learning techniques in photoplethysmography for the non-invasive cuff-less measurement of blood pressure. Biomed. Signal Process. Control 2020, 58, 101870. [Google Scholar] [CrossRef]
- Elgendi, M.; Fletcher, R.; Liang, Y.; Howard, N.; Lovell, N.H.; Abbott, D.; Lim, K.; Ward, R. The use of photoplethysmography for assessing hypertension. NPJ Digit. Med. 2019, 2, 60. [Google Scholar] [CrossRef] [Green Version]
- Hellbrück, H.; Ardelt, G.; Wegerich, P.; Gehring, H. Brachialis Pulse Wave Measurements with Ultra-Wide Band and Continuous Wave Radar, Photoplethysmography and Ultrasonic Doppler Sensors. Sensors 2021, 21, 165. [Google Scholar] [CrossRef]
- Roh, D.; Shin, H. Recurrence Plot and Machine Learning for Signal Quality Assessment of Photoplethysmogram in Mobile Environment. Sensors 2021, 21, 2188. [Google Scholar] [CrossRef]
- Schrumpf, F.; Frenzel, P.; Aust, C.; Osterhoff, G.; Fuchs, M. Assessment of Non-Invasive Blood Pressure Prediction from PPG and rPPG Signals Using Deep Learning. Sensors 2021, 21, 6022. [Google Scholar] [CrossRef]
- Slapničar, G.; Mlakar, N.; Luštrek, M. Blood Pressure Estimation from Photoplethysmogram Using a Spectro-Temporal Deep Neural Network. Sensors 2019, 19, 3420. [Google Scholar] [CrossRef] [Green Version]
- Aguirre, N.; Grall-Maës, E.; Cymberknop, L.; Armentano, R. Blood Pressure Morphology Assessment from Photoplethysmogram and Demographic Information Using Deep Learning with Attention Mechanism. Sensors 2021, 21, 2167. [Google Scholar] [CrossRef]
- Su, P.; Ding, X.-R.; Zhang, Y.-T.; Liu, J.; Miao, F.; Zhao, N. Long-term blood pressure prediction with deep recurrent neural networks. In Proceedings of the 2018 IEEE EMBS International Conference on Biomedical & Health Informatics (BHI), Las Vegas, NV, USA, 4–7 March 2018; pp. 323–328. [Google Scholar] [CrossRef] [Green Version]
- Chowdhury, M.H.; Shuzan, N.I.; Chowdhury, M.E.; Mahbub, Z.B.; Uddin, M.M.; Khandakar, A.; Reaz, M.B.I. Estimating Blood Pressure from the Photoplethysmogram Signal and Demographic Features Using Machine Learning Techniques. Sensors 2020, 20, 3127. [Google Scholar] [CrossRef]
- Markuleva, M.V.; Gerashchenko, M.S.; Gerashchenko, S.I. The Hydrocuff Sensor Position Analysis for Assessing Therespiration Effect in Measuring Hemodynamics and Blood Pressure. In Proceedings of the 2020 International Russian Automation Conference (RusAutoCon), Sochi, Russia, 6–12 September 2020; pp. 810–814. [Google Scholar] [CrossRef]
- Markuleva, M.V.; Gerashchenko, M.S.; Gerashchenko, S.I.; Polosin, V.G.; Mitroshin, A.N.; Astafyev, A.N. The Respiratory Organs Effect on Hemodynamics Evaluating Method Based on Hydro-Cuff Technology. In Proceedings of the 2020 4th Scientific School on Dynamics of Complex Networks and their Application in Intellectual Robotics (DCNAIR), Innopolis, Russia, 7–9 September 2020; pp. 165–168. [Google Scholar] [CrossRef]
- Gerashchenko, M.S.; Markuleva, M.V.; Gerashchenko, S.I.; Semenov, A.D.; Mitroshin, A.N. Nonlinear SVD–filtration in hemodynamic parameters evaluation hydrocuff systems. J. Phys. Conf. Ser. 2020, 1515, 052041. [Google Scholar] [CrossRef]
- Volkova, N.A.; Gerashchenko, S.; Vasiliev, V.S. Algorithm for Estimating Arterial Pressure Based on Spectral Analysis of the Pulse Wave Form. In Proceedings of the 2020 Moscow Workshop on Electronic and Networking Technologies (MWENT), Moscow, Russia, 11–13 March 2020; pp. 1–4. [Google Scholar] [CrossRef]
- Papaioannou, T.G.; Xanthis, D.; Argyris, A.; Vernikos, P.; Mastakoura, G.; Samara, S.; Floros, I.T.; Protogerou, A.D.; Tousoulis, D. Accuracy and precision of cardiac output estimation by an automated, brachial cuff-based oscillometric device in patients with shock. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2020, 234, 1330–1336. [Google Scholar] [CrossRef]
- Barroso, W.K.S.; Gonçalves, C.F.; Berigó, J.A.C.; Melo, M.A.; Arantes, A.C.; Lelis, E.D.S.; Sousa, W.M.; Rezende, J.M.; Jardim, T.; Jardim, P.C.; et al. Tonometric and Oscillometric Methods for Measurement of Central Blood Pressure Parameters: A Comparison in Patients with Borderline Hypertension or Stage 1 Hypertension. Int. J. Cardiovasc. Sci. 2020, 33, 145–150. [Google Scholar] [CrossRef] [Green Version]
- Padwal, R.; Jalali, A.; McLean, D.; Anwar, S.; Smith, K.; Raggi, P.; Ringrose, J.S. Accuracy of oscillometric blood pressure algorithms in healthy adults and in adults with cardiovascular risk factors. Blood Press. Monit. 2019, 24, 33–37. [Google Scholar] [CrossRef]
- Zhang, Z.; Xi, W.; Wang, B.; Chu, G.; Wang, F. A convenient method to verify the accuracy of oscillometric blood pressure monitors by the auscultatory method: A smartphone-based app. J. Clin. Hypertens. 2019, 21, 173–180. [Google Scholar] [CrossRef] [Green Version]
- Rizfan, A.F.; Ghosh, K.; Mustaqir, A.; Mona, R.; Firdous, J.; Muhamad, N. Comparison between Auscultatory and Oscillometric Reading of Blood Pressure Measurement While in Sitting and Supine Position. Biomed. Pharmacol. J. 2019, 12, 775–781. [Google Scholar] [CrossRef]
- Kallioinen, N.; Hill, A.; Horswill, M.S.; Ward, H.E.; Watson, M.O. Sources of inaccuracy in the measurement of adult patients’ resting blood pressure in clinical settings: A systematic review. J. Hypertens. 2017, 35, 421–441. [Google Scholar] [CrossRef] [Green Version]
- Gerashchenko, M.S.; Gerashchenko, S.I. Electronic Tonometer. Patent of the Russian Federation 2652070, 16 May 2017. (In Russian). [Google Scholar]
- Yen, C.-T.; Chang, S.-N.; Liao, C.-H. Deep learning algorithm evaluation of hypertension classification in less photoplethysmography signals conditions. Meas. Control 2021, 54, 439–445. [Google Scholar] [CrossRef]
- Buscema, M. Theory: Foundations of Artificial Neural Networks. Subst. Use Misuse 1998, 33, 17–199. [Google Scholar] [CrossRef]
- Hartmann, V.; Liu, H.; Chen, F.; Hong, W.; Hughes, S.; Zheng, D. Toward Accurate Extraction of Respiratory Frequency from the Photoplethysmogram: Effect of Measurement Site. Front. Physiol. 2019, 10, 732. [Google Scholar] [CrossRef] [PubMed]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Markuleva, M.; Gerashchenko, M.; Gerashchenko, S.; Khizbullin, R.; Ivshin, I. The Hemodynamic Parameters Values Prediction on the Non-Invasive Hydrocuff Technology Basis with a Neural Network Applying. Sensors 2022, 22, 4229. https://doi.org/10.3390/s22114229
Markuleva M, Gerashchenko M, Gerashchenko S, Khizbullin R, Ivshin I. The Hemodynamic Parameters Values Prediction on the Non-Invasive Hydrocuff Technology Basis with a Neural Network Applying. Sensors. 2022; 22(11):4229. https://doi.org/10.3390/s22114229
Chicago/Turabian StyleMarkuleva, Marina, Mikhail Gerashchenko, Sergey Gerashchenko, Robert Khizbullin, and Igor Ivshin. 2022. "The Hemodynamic Parameters Values Prediction on the Non-Invasive Hydrocuff Technology Basis with a Neural Network Applying" Sensors 22, no. 11: 4229. https://doi.org/10.3390/s22114229
APA StyleMarkuleva, M., Gerashchenko, M., Gerashchenko, S., Khizbullin, R., & Ivshin, I. (2022). The Hemodynamic Parameters Values Prediction on the Non-Invasive Hydrocuff Technology Basis with a Neural Network Applying. Sensors, 22(11), 4229. https://doi.org/10.3390/s22114229





