A total of 103 cardiovascular disease patients were recruited. One patient was excluded from the data analysis, due to stopping the 6MWT prematurely for a medical reason (cramps in his/her legs). All patients that were included in the data analysis performed both the smartphone-measured, standardized 6MWT and the smartphone-measured, random walk 6MWT. Participants’ age ranged from 27 to 90 years (mean age = 65.9 years, standard deviation = 11.4 years) with 23 female and 79 male participants. Included patients were participating in a cardiac rehabilitation program due to recent coronary artery disease, heart failure, recent ablation, recent pacemaker, or a cardiac implantable electronic device implantation.
3.1. Smartphone-Measured, Standardized 6MWT
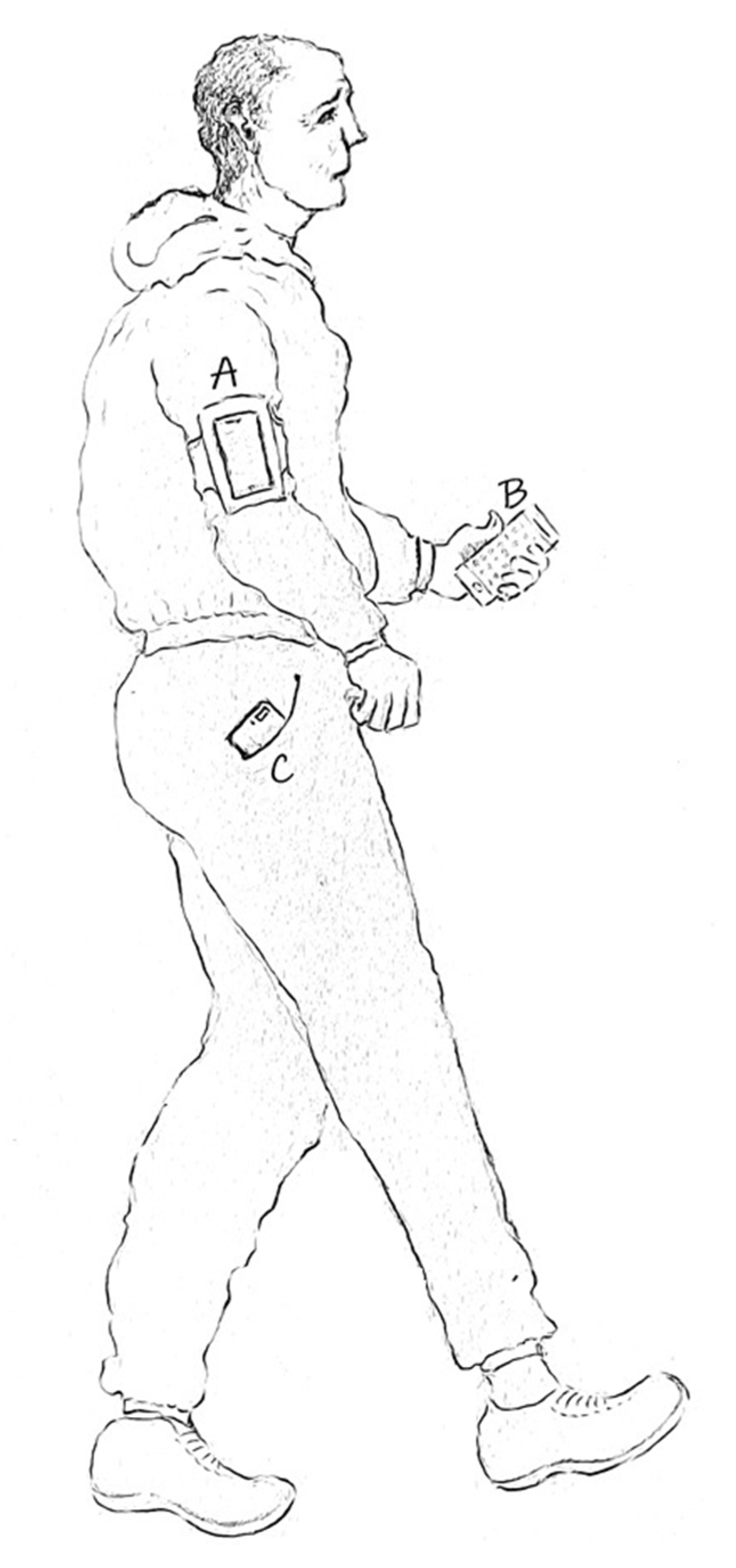
The results of 102 standardized 6MWTs running the four algorithms in parallel (
Google Fit Raw, Google Fit Processed, GPS, GPS and Google Fit) in the three smartphone positions (
pocket, hand, arm) were used to determine the accuracy and reliability of the smartphone-measured, standardized 6MWT.
Table 1 depicts the analysis of the personalized-threshold, outlier-filtered data set.
As depicted in
Table 1, the algorithm
Google Fit Processed with the smartphone mounted on the patient’s
arm yielded for the personalized-threshold, outlier-filtered data set the smallest mean absolute error, the best median error, the minimum standard deviation, and the minimum error rate. Therefore, we can conclude that among the algorithms that we included in this study, the algorithm
Google Fit Processed with the smartphone mounted on the patient’s
arm is the best combination for a smartphone-measured, standardized six-minute walk test.
The mean absolute error for the algorithm
Google Fit Processed with the smartphone worn in a strap around the
arm is 20.16 m, which is lower than the MCID suggested by Bohannon and Crouch [
9]. Furthermore, the maximal absolute error for this algorithm–smartphone position combination is 66 m. This indicates that this algorithm–smartphone position combination can be used to detect changes in cardiovascular disease patients’ functional capacity.
In
Figure 2, the 6MWDs, as measured by the smartphone with the
Google Fit Processed–
arm combination, and as measured by the healthcare professional manually, are depicted for each participant. For the majority of the patients, the 6MWD measured by the healthcare professional and the 6MWD measured by the algorithm
Google Fit Processed in the
arm position are overlapping or extremely close to each other, indicating that the smartphone-measured 6MWD is fairly accurate. For this algorithm–smartphone position combination, the number of outliers is limited (only two outliers). Missing values for this algorithm–smartphone position combination are indicated by no value/dot for the participant (e.g., participant 5). Possible reasons for missing values include the smartphone going into sleep mode during the 6MWT and the patient pressing a button in the 6MWT application while the test is ongoing.
The Bland–Altman plot (
Figure 3) shows the difference between the 6MWD measured manually by the healthcare professional, and the 6MWD measured by the algorithm
Google Fit Processed in the
arm position. The difference in meters between the healthcare professional-measured and smartphone-measured 6MWD for this algorithm–smartphone position combination is at most 66 m. Relative to the total distance walked during the 6MWT, which is minimally 228 m and maximally 657 m, this difference is acceptable. Furthermore, for most participants, the difference is significantly smaller.
Next, using the same metrics (i.e., minimum mean absolute error, best median, minimum standard deviation, and minimum error rate), we analyzed which algorithm performs best in each position for a smartphone-measured, standardized 6MWT. The algorithm
Google Fit Processed outperformed all other algorithms in all positions (i.e.,
pocket, hand, arm) by recording the minimum mean absolute error, the best median, the minimum standard deviation, and the minimum error rate (
Table 1), indicating that the best algorithm to use for a smartphone-measured, standardized 6MWT is
Google Fit Processed, independent of the position of the smartphone.
Similarly, we inspected our evaluation metrics (i.e., minimum mean absolute error, best median, minimum standard deviation, and minimum error rate) for each algorithm separately in all positions to find the best position to wear the smartphone for each algorithm for a smartphone-measured, standardized six-minute walk test (
Table 1).
The algorithm
Google Fit Raw obtained the best results with the smartphone in the front
pocket of the patient’s pants. Since the accuracy of this algorithm heavily depends on an accurate detection of steps, it is logical that a position that allows accurate step detection (such as the pocket of your pants) yields the best results. The algorithm
Google Fit Processed produced the most accurate results when the smartphone was mounted in a strap around the
arm. This is surprising, since similar to the algorithm
Google Fit Raw, the accuracy of this algorithm heavily depends on the accurate detection of steps. However, the algorithm
Google Fit Processed uses Google Fit’s preprocessing of steps, which gives a more accurate step count than using the raw
Google Fit step count data [
10] (as in the
algorithm Google Fit Raw). This might have an influence on the recognition of steps in the different smartphone positions and thus the best position to wear the smartphone for the two algorithms that are based on
Google Fit data.
The algorithm GPS achieved the best results with the smartphone in the hand. We think this could be caused by the localization data being more accurate when the smartphone is held in the hand (no interference from other material surrounding the smartphone, such as the arm strap or the patient’s pants), in comparison with the smartphone worn in a strap around the arm or in the pocket of the patient’s pants. The algorithm GPS and Google Fit performed best with the smartphone carried in the hand. It is reasonable to expect that the best results for both the algorithms GPS and GPS and Google Fit are the same, since both rely mostly on the localization information provided by the smartphone’s built-in GPS sensors to measure the distance walked during the six-minute walk test.
In addition to the accuracy of the measured six-minute walk distance, it is important to consider the reliability of the algorithm–smartphone position combination to evaluate which combination is best for a smartphone-measured, standardized 6MWT.
Table 2 provides for each algorithm–smartphone position combination an overview of the number of missing values (i.e., the algorithm provides no result for the 6MWD) and the number of outliers (i.e., the algorithm provides an unrealistic 6MWD). It is remarkable that there are no outliers detected for the algorithm
Google Fit Raw. Most outliers were detected for the combination
GPS and Google Fit–pocket, indicating that this is the least reliable algorithm–smartphone position combination in terms of outliers.
When considering the algorithm that performed best in each smartphone position, i.e., Google Fit Processed, we can conclude that for this algorithm the number of outliers is quite limited, ranging from zero to two outliers dependent on the smartphone position. In terms of reliability, the best algorithm–smartphone position combinations are the algorithm Google Fit Raw in the hand position and the algorithm GPS in the hand position. For all algorithms, the number of missing values and number of outliers are lowest when the smartphone is carried in the hand. However, it must be noted that the difference in the number of missing values and outliers is small for most algorithm–smartphone position combinations, with the exception of the combination GPS and Google Fit–pocket.
3.2. Smartphone-Measured, Random Walk 6MWT
The results of 102 random walk six-minute walk tests (6MWTs) running in parallel the four algorithms (
Google Fit Raw, Google Fit Processed, GPS, GPS and Google Fit) in the three smartphone positions (
pocket, hand, arm) were used to determine the best algorithm–smartphone position combination for a smartphone-measured, random walk 6MWT. We considered both the reliability and the accuracy of the six-minute walk distance (6MWD) to determine the best algorithm–smartphone position combination. We used the 6MWD as measured by the healthcare professional during the standardized 6MWT as a reference to determine the accuracy.
Table 3 shows the analysis of the 6MWD for a random walk six-minute walk test for the personalized-threshold, outlier-filtered data set.
The algorithm Google Fit Processed with the smartphone worn in a strap around the patient’s arm produced the smallest mean absolute error, the best median error, the minimum standard deviation, and the minimum error rate. As a result, we can conclude that among the algorithms that we included in this study, the algorithm Google Fit Processed with the smartphone mounted on the patient’s arm provides the most accurate 6MWD for a smartphone-measured, random walk six-minute walk test.
When comparing the mean absolute error for the algorithm
Google Fit Processed with the smartphone worn in a strap around the patient’s
arm (i.e., 20.6 m), with the minimal clinically important difference (i.e., 30.5 meters [
9]), we can conclude that this algorithm–smartphone position combination can be used to detect changes in cardiovascular disease patients’ functional capacity. Furthermore, the maximal absolute error for this algorithm–smartphone combination is 111.2 m.
In
Figure 4, the six-minute walk distances (6MWDs), as measured during the random walk 6MWT by the smartphone with the algorithm
Google Fit Processed with the smartphone mounted in a strap around the patient’s
arm, and as measured during the standardized 6MWT manually by the healthcare professional, are depicted for each participant. For most participants, the 6MWD measured by the healthcare professional during the standardized 6MWT and the 6MWD measured by the algorithm
Google Fit Processed in the
arm position during the random walk 6MWT are extremely close to each other or even overlapping, indicating that the smartphone-measured 6MWD is fairly accurate. For this algorithm–smartphone position combination, there are only two outliers. Missing values for this combination of algorithm–smartphone position are indicated by no dot for the participant (e.g., participant 5).
Figure 5 depicts the Bland–Altman plot, showing the difference between the 6MWD measured by the algorithm
Google Fit Processed in the
arm position during the random walk 6MWT, and the 6MWD measured manually by the healthcare professional during the standardized 6MWT. The difference in meters between the healthcare professional-measured, standardized 6MWD and smartphone-measured, random walk 6MWD for this algorithm–smartphone position combination is at most 111.2 m. Relative to the total distance walked during the random walk 6MWT, which is minimally 262.1 m and maximally 635 m, this difference is acceptable. Furthermore, for most participants, the difference is significantly smaller, indicated by the dots in the Bland–Altman plot (
Figure 5) being close to 0.
Using the same metrics (i.e., minimum mean absolute error, best median, minimum standard deviation, and minimum error rate), we determined which algorithm performs best in each position for a smartphone-measured, random walk 6MWT. The algorithm
Google Fit Processed surpassed all other algorithms in all three smartphone positions (
pocket, hand, arm) by recording the minimum mean absolute error, the best median, the minimum standard deviation, and the minimum error rate (
Table 3).
Likewise, we inspected our evaluation metrics (i.e., minimum mean absolute error, best median, minimum standard deviation, and minimum error rate) for each algorithm separately in all positions to find the best position to wear the smartphone for each algorithm for a smartphone-measured, random walk 6MWT (
Table 3).
The algorithm Google Fit Raw obtained the best results with the smartphone in the front pocket of the patient’s pants, whereas the algorithm Google Fit Processed performed best with the smartphone mounted in a strap around the patient’s arm. The result for the algorithm Google Fit Processed is surprising, since we expected that a position in which steps can be accurately detected is favorable for these two algorithms that heavily depend on accurate step count detection (i.e., Google Fit Raw and Google Fit Processed).
The algorithms GPS and GPS and Google Fit produced the best results with the smartphone in the pocket position. As expected, the position to wear the smartphone for both algorithms that depend on the localization information provided by the built-in GPS sensors (i.e., GPS and GPS and Google Fit) is the same. However, we do not have a direct indication of why the pocket position performs better than the other two smartphone positions.
Similar to the smartphone-measured, standardized 6MWT, we investigated the reliability of the different algorithm–smartphone position combinations to evaluate which combination is best for a smartphone-measured, random walk 6MWT.
Table 4 provides for each investigated algorithm–smartphone position combination an overview of the number of missing values and the number of outliers. It is noteworthy that no outliers were detected for the algorithm
Google Fit Raw in any of the smartphone positions. Furthermore, several other algorithm–smartphone position combinations did not have any outliers:
Google Fit Processed–pocket,
GPS–pocket,
GPS–arm, and
GPS and Google Fit–arm). Most outliers were detected for the algorithm
GPS and Google Fit with the smartphone worn in the front
pocket of the patient’s pants, indicating that this is the least reliable algorithm–smartphone position combination in terms of outliers.
When considering the algorithm that performed best in each smartphone position, i.e.,
Google Fit Processed (
Table 3), we can conclude that for this algorithm the number of outliers is quite low, ranging from zero (for the
pocket position) to two outliers (for the
arm position) dependent on the smartphone position. In terms of reliability, the best algorithm–smartphone position combinations are
GPS–arm and
GPS and Google Fit–arm. For all algorithms, the total number of missing values and outliers is lowest when the smartphone is carried in the
arm position and highest when the smartphone is carried in the front
pocket of the patient’s pants. A possible explanation is that missing values might be caused by accidentally pressing a button while the 6MWT is ongoing, which happens easily when the smartphone is carried in the pocket of the patient’s pants.
3.3. Comparison of the Smartphone-Measured Standardized 6MWT and the Smartphone-Measured Random Walk 6MWT
For both trajectories, the most accurate algorithm–smartphone combination for a smartphone-measured 6MWT is the algorithm Google Fit Processed with the smartphone mounted in a strap around the patient’s arm. As a result, this is the most accurate algorithm–smartphone position combination, independent of the walking trajectory. In addition, our analysis demonstrated that for a smartphone-measured 6MWT the algorithm Google Fit Processed outperforms all other algorithms for all smartphone positions, independent of the walking trajectory.
Figure 6 presents the six-minute walk distance (6MWD) as measured by the algorithm
Google Fit Processed in the
arm position for both the standardized 6MWT and the random walk 6MWT. In addition, the reference distance, i.e., the 6MWD as measured manually by the healthcare professional during the standardized 6MWT, is depicted. For most participants, both smartphone-measured 6MWDs are very close to or even overlapping with the healthcare professional-measured 6MWD. With respect to the outliers, we can see that for participant 56 the smartphone-measured 6MWD is considered an outlier for both walking trajectories, whereas the second outlier is unique for each walking trajectory (i.e., 6MWD value of participant 13 for the standardized 6MWT and 6MWD value of participant 81 for the random walk 6MWT).
The smartphone-measured, standardized 6MWT is slightly more accurate than the smartphone-measured, random walk 6MWT, indicated by a lower mean absolute error, a lower standard deviation of the absolute error, and a lower error rate. However, when considering this with respect to the minimal clinically important difference, we can conclude that this difference in accuracy is not significant. We see that the smartphone-measured random walk 6MWT rather underestimates the 6MWD, whereas the smartphone-measured standardized 6MWT rather overestimates the 6MWD. As already mentioned, the 6MWD gives an indication of a patient’s functional capacity. Therefore, it can be used as an information source when prescribing physical exercise training to cardiac patients. For physical exercise training, it is safer to underestimate a person’s functional capacity and thus give a lower training, rather than overestimate a person’s functional capacity and thus prescribe a too intense exercise program. However, it must be noted that the difference is only very small.
For both walking trajectories (standardized and random walk), the reliability turns out to be similar when considering the most accurate algorithm–smartphone position combination. Indeed, the number of outliers is exactly the same for both walking trajectories. On the contrary, the number of missing values is higher for the smartphone-measured standardized 6MWT (15 missing values) than for the smartphone-measured random walk 6MWT (four missing values). However, it is unclear if these outliers are due to the walking trajectory, since missing values were often caused by patients accidentally pressing a button on the smartphone while the 6MWT was ongoing. Furthermore, the best algorithm–smartphone position combinations in terms of reliability are different for the two walking trajectories.
3.4. Patients’ Opinion about a Self-Administered 6MWT
In our study, the 6MWT application was controlled by the healthcare professional. Patients’ opinion about performing a self-administered, smartphone-measured 6MWT alone at home was assessed with a survey. After the participants performed both the standardized 6MWT and the random walk 6MWT, they filled in a custom-made questionnaire consisting of several Likert scale, multiple choice, rating, and open questions. The questionnaire was completed by all 102 patients that performed the two 6MWTs. It is important to note that 10% of the participants clearly indicated that they are not using a smartphone regularly.
First, we assessed patients’ impressions and feelings about the 6MWT in general by asking them to indicate their opinion for a number of statements on a 5-point Likert scale, ranging from strongly disagree to strongly agree (
Figure 7). The majority of the patients do not consider the 6MWT a tool that is only useful for healthcare professionals. The 6MWT is rather perceived as a tool that triggers reflection on their physical fitness, and thus could contribute to the motivation of the patient. Only three patients indicated that they do not like to perform the 6MWT to follow up on their progress themselves. Interpreting the result of their 6MWT is a challenge for some patients, indicated by a higher number of (strongly) disagree and neutral responses. This highlights the importance of education and guidance when patients perform the 6MWT in their home environment, without the supervision of a healthcare professional.
Next, we assessed patients’ opinion about using a smartphone application to perform a self-administered 6MWT at home (e.g., do they find it reliable to use a smartphone app to perform the 6MWT). Again, we used 5-point Likert scale questions, ranging from strongly disagree to strongly agree (
Figure 8). It is notable that only five out of the 102 participants did not want to use a smartphone application to perform a 6MWT. Most patients think it is reliable and are not afraid to perform a self-administered, smartphone-based 6MWT without the supervision of a healthcare professional. We observed no clear difference in the moment (during or after finishing the rehabilitation program in the rehabilitation center) at which patients would find it more useful to perform a home-based 6MWT to follow up on their physical fitness. Patients would like that their healthcare professionals (e.g., cardiologist or physiotherapist) follow up the results of the 6MWTs that they perform at home. Lastly, we want to note that the negative and neutral responses regarding the usage of a smartphone application to do a 6MWT might be due to patients’ unfamiliarity with technology and smartphones in particular, or their unwillingness to follow up their physical fitness using a smartphone application.
As a next step, we investigated patients’ preferences for the location to perform a 6MWT, i.e., in the hospital/rehabilitation center under the supervision of a healthcare professional or at home using a smartphone application. Twenty-seven percent of the patients preferred to do the 6MWT in the rehabilitation center under the supervision of a healthcare professional, whereas 29 percent of the patients preferred to do the 6MWT at home with the smartphone application. Eighteen percent of the patients wanted to perform the 6MWT in both settings (in the rehabilitation center and at home). The remaining 25 percent did not have a preference for the location to perform the 6MWT. This indicates that only 27 percent of the participants do not want to perform a self-administered, smartphone-based 6MWT at home. We believe that this is due to the patients’ unfamiliarity with smartphones.
Currently, in the rehabilitation center, patients perform maximal cardiopulmonary exercise testing (CPET) three times during their rehabilitation trajectory. However, as mentioned in the Introduction, we investigated if the 6MWT could be used as an alternative to the CPET to follow up on the patient’s functional exercise capacity. In the questionnaire, we assessed patients’ preferences for the CPET versus the 6MWT. Out of the 98 participants that answered this question, 46 participants (i.e., 47%) preferred the 6MWT, 39 participants (i.e., 40%) preferred the CPET, and 13 participants (i.e., 13%) did not have a preference. Reasons for preferring the 6MWT included the easiness and pleasantness of the test. Reasons for preferring the CPET included preferring cycling over walking and the greater amount information that is available from the CPET.
As a main contribution of this paper, we investigated the influence of the walking trajectory (i.e., standardized or random walk) on the 6MWT results. To complement these analyses, we assessed patients’ preferences for the walking trajectory. The majority of the patients (66 out of the 102 participants, 65%) preferred the random walk 6MWT, whereas only 16 patients (16%) preferred the standardized 6MWT. Fourteen patients (14%) thought both walking trajectories were equally convenient. From these findings, we can conclude that most participants prefer the random walk trajectory over the standardized trajectory for a 6MWT.
To gather insight into patients’ preferences for the position to wear the smartphone (pocket, hand, arm), we included in the questionnaire some questions that asked the participants to rate the different options. For both walking trajectories, the results were quite similar. Most patients preferred to wear the smartphone in a strap around the arm (59 participants for the standardized 6MWT and 54 participants for the random walk 6MWT), followed by the front pocket of the patients’ pants, and lastly the hand position. Only a few patients did not have any preference. Some reasons for participants’ preferences for the arm position were that this was the least disturbing, distracting, or hindering position, there was less chance of dropping the smartphone, they still had freedom to move easily, and they did not have to carry the device in their hand. Arguments against the arm position included needing an extra accessory (i.e., arm strap) and that the arm strap could be inconvenient when wearing a pullover or a jacket.