Directed Functional Coordination Analysis of Swallowing Muscles in Healthy and Dysphagic Subjects by Surface Electromyography
Abstract
:1. Introduction
2. Materials and Methods
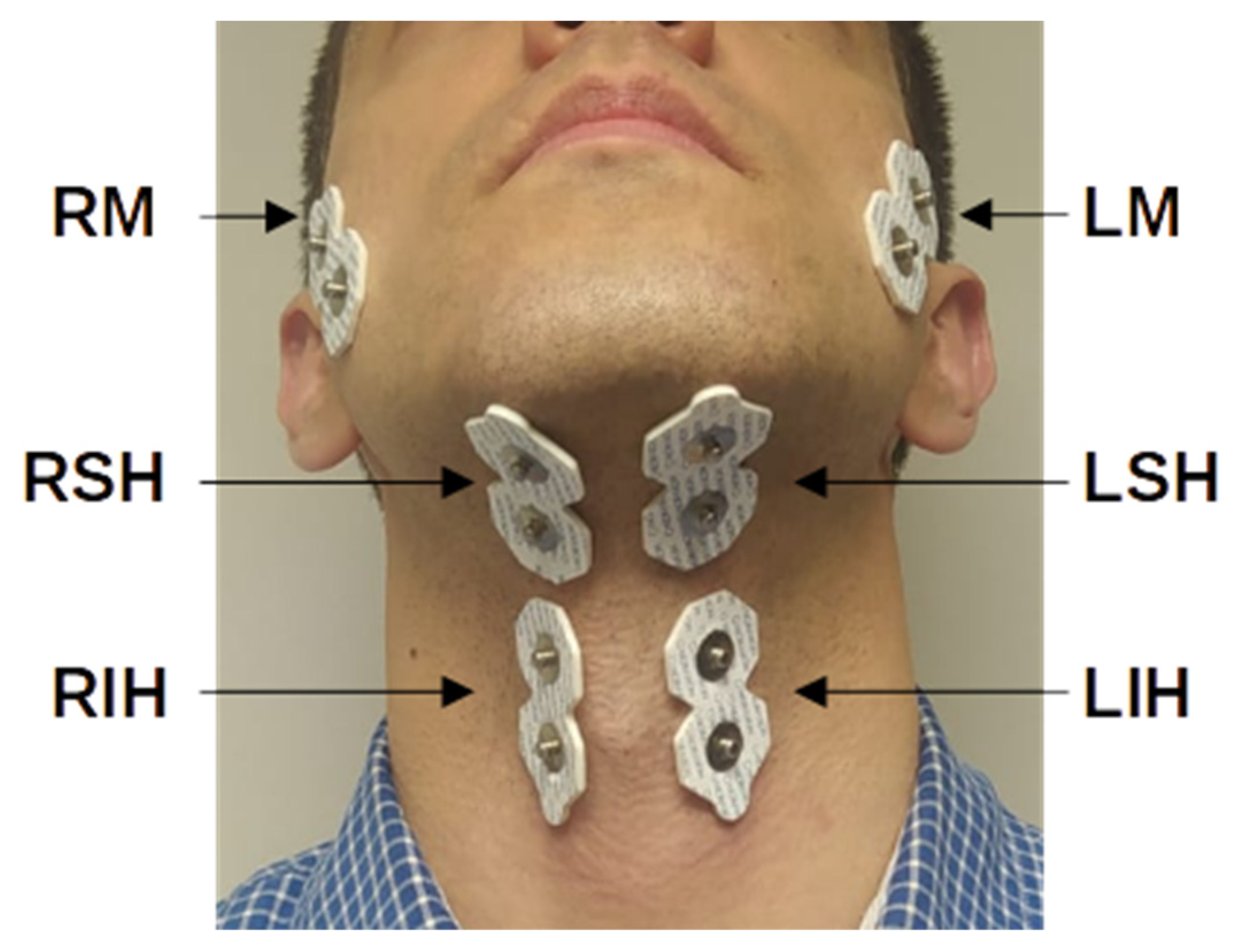
2.1. Data Acquisition
2.2. Conditional Granger Causality
2.3. Data Analysis
3. Results
3.1. Assessment of Muscle Interactions
3.2. Statistical Analysis
4. Discussion
4.1. Relevant Muscle Interactions during Swallowing
4.2. Alterations of Muscle Interactions in Dysphagia
4.3. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhu, M.; Yu, B.; Yang, W.; Jiang, Y.; Lu, L.; Huang, Z.; Chen, S.; Li, G. Evaluation of normal swallowing functions by using dynamic high-density surface electromyography maps. Biomed. Eng. Online 2017, 16, 1–18. [Google Scholar] [CrossRef] [Green Version]
- Bhattacharyya, N. The Prevalence of Dysphagia among Adults in the United States. Otolaryngol. Neck Surg. 2014, 151, 765–769. [Google Scholar] [CrossRef] [PubMed]
- Chen, D.F. Dysphagia in the Hospitalized Patient. Hosp. Med. Clin. 2017, 6, 38–52. [Google Scholar] [CrossRef]
- Daroff, R.B.; Jankovic, J.; Mazziotta, J.C.; Pomeroy, S.L. Bradley’s Neurology in Clinical Practice, 7th ed.; Elsevier: Amsterdam, The Netherlands, 2016. [Google Scholar]
- Hoy, M.; Domer, A.; Plowman, E.K.; Loch, R.; Belafsky, P. Causes of dysphagia in a tertiary-care swallowing center. Ann. Otol. Rhinol. Laryngol. 2013, 122, 335–338. [Google Scholar] [CrossRef] [PubMed]
- Ekberg, O.; Hamdy, S.; Woisard, V.; Wuttge-Hannig, A.; Ortega, P. Social and Psychological Burden of Dysphagia: Its Impact on Diagnosis and Treatment. Dysphagia 2002, 17, 139–146. [Google Scholar] [CrossRef]
- Cichero, J.A.; Altman, K.W. Definition, Prevalence and Burden of Oropharyngeal Dysphagia: A Serious Problem among Older Adults Worldwide and the Impact on Prognosis and Hospital Resources. In Stepping Stones to Living Well with Dysphagia; Karger Publishers: Berlin, Germany, 2012; Volume 72, pp. 1–11. [Google Scholar] [CrossRef]
- A Patel, D.; Krishnaswami, S.; Steger, E.; Conover, E.; Vaezi, M.F.; Ciucci, M.R.; O Francis, D. Economic and survival burden of dysphagia among inpatients in the United States. Dis. Esophagus 2017, 31, 1–7. [Google Scholar] [CrossRef]
- Attrill, S.; White, S.; Murray, J.; Hammond, S.; Doeltgen, S. Impact of oropharyngeal dysphagia on healthcare cost and length of stay in hospital: A systematic review. BMC Health Serv. Res. 2018, 18, 1–18. [Google Scholar] [CrossRef] [Green Version]
- Vaiman, M. Standardization of surface electromyography utilized to evaluate patients with dysphagia. Head Face Med. 2007, 3, 26. [Google Scholar] [CrossRef] [Green Version]
- Kang, C.H.; Hentz, J.G.; Lott, D.G. Muscle Tension Dysphagia: Symptomology and Theoretical Framework. Otolaryngol. Head. Neck Surg. 2016, 155, 837–842. [Google Scholar] [CrossRef]
- Krasnodębska, P.; Jarzyńska-Bućko, A.; Szkiełkowska, A.; Miaśkiewicz, B.; Skarżyński, H. Diagnosis in Muscle Tension Dysphagia. Otolaryngol. Polska 2020, 74, 1–5. [Google Scholar] [CrossRef]
- Wang, Y.-C.; Chou, W.; Lin, B.-S.; Wang, J.-J. The use of surface electromyography in dysphagia evaluation. Technol. Health Care 2017, 25, 1025–1028. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Casado, J.; Prats-Boluda, G.; Ye-Lin, Y.; Restrepo-Agudelo, S.; Perez-Giraldo, E.; Orozco-Duque, A. Evaluation of Swallowing Related Muscle Activity by Means of Concentric Ring Electrodes. Sensors 2020, 20, 5267. [Google Scholar] [CrossRef] [PubMed]
- Koyama, Y.; Ohmori, N.; Momose, H.; Kondo, E.; Yamada, S.-I.; Kurita, H. Detection of swallowing disorders using a multiple channel surface electromyography sheet: A preliminary study. J. Dent. Sci. 2020, 16, 160–167. [Google Scholar] [CrossRef] [PubMed]
- Mori, H.; Izumi, S.-I.; Kagaya, H.; Oyama, H.; Abe, G.; Yashima, K.; Takagi, T. Evaluation of the myoelectric potential of the infrahyoid muscles as a means of detecting muscle activity of the suprahyoid muscles. Jpn. J. Compr. Rehabilit. Sci. 2020, 11, 52–58. [Google Scholar] [CrossRef]
- Inokuchi, H.; González-Fernández, M.; Matsuo, K.; Brodsky, M.B.; Yoda, M.; Taniguchi, H.; Okazaki, H.; Hiraoka, T.; Palmer, J.B. Electromyography of Swallowing with Fine Wire Intramuscular Electrodes in Healthy Human: Activation Sequence of Selected Hyoid Muscles. Dysphagia 2014, 29, 713–721. [Google Scholar] [CrossRef]
- Restrepo-Agudelo, S.; Roldan-Vasco, S.; Ramirez-Arbelaez, L.; Cadavid-Arboleda, S.; Perez, E.; Orozco-Duque, A. Improving surface EMG burst detection in infrahyoid muscles during swallowing using digital filters and discrete wavelet analysis. J. Electromyogr. Kinesiol. 2017, 35, 1–8. [Google Scholar] [CrossRef]
- Roldan-Vasco, S.; Restrepo-Agudelo, S.; Valencia-Martinez, Y.; Orozco-Duque, A. Automatic detection of oral and pharyngeal phases in swallowing using classification algorithms and multichannel EMG. J. Electromyogr. Kinesiol. 2018, 43, 193–200. [Google Scholar] [CrossRef]
- Sebastian, R.V.; Estefania, P.G.; Andres, O.D. Orozco-Duque. Scalogram-energy based segmentation of surface electromyography signals from swallowing related muscles. Comput. Methods Programs Biomed. 2020, 194, 105480. [Google Scholar] [CrossRef]
- Mosier, K.; Bereznaya, I. Parallel cortical networks for volitional control of swallowing in humans. Exp. Brain Res. 2001, 140, 280–289. [Google Scholar] [CrossRef]
- Steele, C.M.; Van Lieshout, P.H.H.M. The Dynamics of Lingual-Mandibular Coordination During Liquid Swallowing. Dysphagia 2007, 23, 33–46. [Google Scholar] [CrossRef]
- Murakami, K.; Hirano, H.; Watanabe, Y.; Edahiro, A.; Ohara, Y.; Yoshida, H.; Kim, H.; Takagi, D.; Hironaka, S. Relationship between swallowing function and the skeletal muscle mass of older adults requiring long-term care. Geriatr. Gerontol. Int. 2015, 15, 1185–1192. [Google Scholar] [CrossRef] [PubMed]
- Matsuo, K.; Palmer, J.B. Anatomy and Physiology of Feeding and Swallowing: Normal and Abnormal. Phys. Med. Rehabil. Clin. N. Am. 2008, 19, 691–707. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spiro, J.; Rendell, J.K.; Gay, T. Activation and Coordination Patterns of the Suprahyoid Muscles During Swallowing. Laryngoscope 1994, 104, 1376–1382. [Google Scholar] [CrossRef] [PubMed]
- Gay, T.; Rendell, J.K.; Spiro, J. Oral and Laryngeal Muscle Coordination During Swallowing. Laryngoscope 1994, 104, 341–349. [Google Scholar] [CrossRef] [PubMed]
- Perlman, A.L.; Palmer, P.M.; McCulloch, T.M.; Vandaele, D.J. Electromyographic activity from human laryngeal, pharyngeal, and submental muscles during swallowing. J. Appl. Physiol. 1999, 86, 1663–1669. [Google Scholar] [CrossRef] [PubMed]
- McKeown, M.J.; Torpey, D.C.; Gehm, W.C. Non-invasive monitoring of functionally distinct muscle activations during swallowing. Clin. Neurophysiol. 2002, 113, 354–366. [Google Scholar] [CrossRef]
- Lee, H.-J.; Kim, K.-D. Analysis of the Correlation between Activity of the Suprahyoid Muscles, Infrahyoid Muscles and the New VFSS Scale in Stroke Patients with Dysphagia. J. Korean Soc. Phys. Med. 2018, 13, 19–25. [Google Scholar] [CrossRef] [Green Version]
- Green, J.R.; Wang, Y.-T. Tongue-surface movement patterns during speech and swallowing. J. Acoust. Soc. Am. 2003, 113, 2820–2833. [Google Scholar] [CrossRef] [Green Version]
- Ishii, T.; Narita, N.; Endo, H. Evaluation of jaw and neck muscle activities while chewing using EMG-EMG transfer function and EMG-EMG coherence function analyses in healthy subjects. Physiol. Behav. 2016, 160, 35–42. [Google Scholar] [CrossRef] [Green Version]
- Bastos, A.M.; Schoffelen, J.-M. A Tutorial Review of Functional Connectivity Analysis Methods and Their Interpretational Pitfalls. Front. Syst. Neurosci. 2016, 9, 175. [Google Scholar] [CrossRef] [Green Version]
- Hnazaee, M.F.; Khachatryan, E.; Chehrazad, S.; Kotarcic, A.; De Letter, M.; Van Hulle, M. Overlapping connectivity patterns during semantic processing of abstract and concrete words revealed with multivariate Granger Causality analysis. Sci. Rep. 2020, 10, 1–19. [Google Scholar] [CrossRef] [Green Version]
- Manomaisaowapak, P.; Nartkulpat, A.; Songsiri, J. Granger Causality Inference in EEG Source Connectivity Analysis: A State-Space Approach. IEEE Trans. Neural Networks Learn. Syst. 2021, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Shi, Q.; Chen, H.; Jia, Q.; Yuan, Z.; Wang, J.; Li, Y.; Han, Z.; Mo, D.; Zhang, Y. Altered Granger Causal Connectivity of Resting-State Neural Networks in Patients With Leukoaraiosis-Associated Cognitive Impairment—A Cross-Sectional Study. Front. Neurol. 2020, 11, 457. [Google Scholar] [CrossRef] [PubMed]
- Sitnikova, E.; Dikanev, T.; Smirnov, D.; Bezruchko, B.; van Luijtelaar, G. Granger causality: Cortico-thalamic interdependencies during absence seizures in WAG/Rij rats. J. Neurosci. Methods 2008, 170, 245–254. [Google Scholar] [CrossRef] [Green Version]
- Eichler, M. Causal inference with multiple time series: Principles and problems. Philos. Trans. R. Soc. Lond. Ser. A Math. Phys. Eng. Sci. 2013, 371, 20110613. [Google Scholar] [CrossRef] [Green Version]
- Clavé, P.; DE Kraa, M.; Arreola, V.; Girvent, M.; Farré, R.; Palomera, E.; Serra-Prat, M. The effect of bolus viscosity on swallowing function in neurogenic dysphagia. Aliment. Pharmacol. Ther. 2006, 24, 1385–1394. [Google Scholar] [CrossRef]
- Bozorgi, C.; Holleufer, C.; Wendin, K. Saliva Secretion and Swallowing—The Impact of Different Types of Food and Drink on Subsequent Intake. Nutrients 2020, 12, 256. [Google Scholar] [CrossRef] [Green Version]
- Barnett, L.; Seth, A.K. The MVGC multivariate Granger causality toolbox: A new approach to Granger-causal inference. J. Neurosci. Methods 2014, 223, 50–68. [Google Scholar] [CrossRef] [Green Version]
- Goen, A.; Tiwari, D.C. Review of Surface Electromyogram Signals: Its Analysis and Applications. Int. J. Electr. Electron. Sci. Eng. 2013, 7, 965–973. [Google Scholar]
- Dhamala, M.; Rangarajan, G.; Ding, M. Analyzing information flow in brain networks with nonparametric Granger causality. NeuroImage 2008, 41, 354–362. [Google Scholar] [CrossRef] [Green Version]
- Oommen, E.R.; Kim, Y.; McCullough, G. Stage Transition and Laryngeal Closure in Poststroke Patients with Dysphagia. Dysphagia 2010, 26, 318–323. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cohen, D.; Tsuchiya, N. The Effect of Common Signals on Power, Coherence and Granger Causality: Theoretical Review, Simulations, and Empirical Analysis of Fruit Fly LFPs Data. Front. Syst. Neurosci. 2018, 12, 30. [Google Scholar] [CrossRef] [PubMed]
- Alfonsi, E.; Cosentino, G.; Mainardi, L.; Schindler, A.; Fresia, M.; Brighina, F.; Benazzo, M.; Moglia, A.; Alvisi, E.; Fierro, B.; et al. Electrophysiological Investigations of Shape and Reproducibility of Oropharyngeal Swallowing: Interaction with Bolus Volume and Age. Dysphagia 2015, 30, 540–550. [Google Scholar] [CrossRef] [PubMed]
- Park, M.W.; Lee, D.; Gil Seo, H.; Han, T.R.; Lee, J.C.; Kim, H.C.; Oh, B.-M. Reliability of Suprahyoid and Infrahyoid Electromyographic Measurements during Swallowing in Healthy Subjects. J. Korean Dysphagia Soc. 2021, 11, 128–136. [Google Scholar] [CrossRef]
- Cosentino, G.; Alfonsi, E.; Mainardi, L.; Alvisi, E.; Brighina, F.; Valentino, F.; Fierro, B.; Sandrini, G.; Bertino, G.; Berlangieri, M.; et al. The importance of the reproducibility of oropharyngeal swallowing in amyotrophic lateral sclerosis. An electrophysiological study. Clin. Neurophysiol. 2017, 128, 792–798. [Google Scholar] [CrossRef] [PubMed]
- Hiraoka, K. Changes in masseter muscle activity associated with swallowing. J. Oral Rehabil. 2004, 31, 963–967. [Google Scholar] [CrossRef]
- Zanato, L.E.; Chiari, B.M.; Vieira, M.M.; Bommarito, S. Study of the electrical activity of muscles: Masseter, temporal and supra-hyoid during swallowing. Dent. Oral Craniofacial Res. 2016, 3, 1–4. [Google Scholar]
- Monaco, A.; Cattaneo, R.; Spadaro, A.; Giannoni, M. Surface electromyography pattern of human swallowing. BMC Oral Health 2008, 8, 6. [Google Scholar] [CrossRef] [Green Version]
- Ko, J.Y.; Kim, H.; Jang, J.; Lee, J.C.; Ryu, J.S. Electromyographic activation patterns during swallowing in older adults. Sci. Rep. 2021, 11, 1–10. [Google Scholar] [CrossRef]
- Leslie, P.; Carding, P.; Wilson, J. Investigation and management of chronic dysphagia. BMJ 2003, 326, 433–436. [Google Scholar] [CrossRef] [Green Version]
- Karnell, M.P.; Rogus, N.M. Comparison of Clinician Judgments and Measurements of Swallow Response Time. J. Speech Lang. Hear. Res. 2005, 48, 1269–1279. [Google Scholar] [CrossRef]
- Lin, C.-W.; Chang, Y.-C.; Chen, W.-S.; Chang, K.; Chang, H.-Y.; Wang, T.-G. Prolonged Swallowing Time in Dysphagic Parkinsonism Patients With Aspiration Pneumonia. Arch. Phys. Med. Rehabil. 2012, 93, 2080–2084. [Google Scholar] [CrossRef] [PubMed]
- Teismann, I.K.; Warnecke, T.; Suntrup, S.; Steinsträter, O.; Kronenberg, L.; Ringelstein, E.B.; Dengler, R.; Petri, S.; Pantev, C.; Dziewas, R. Cortical Processing of Swallowing in Als Patients with Progressive Dysphagia—A Magnetoencephalographic Study. PLoS ONE 2011, 6, e19987. [Google Scholar] [CrossRef] [Green Version]
- Ertekin, C.; Aydogdu, I.; Yuceyar, N.; Kiylioglu, N.; Tarlacı, S.; Uludag, B. Pathophysiological mechanisms of oropharyngeal dysphagia in amyotrophic lateral sclerosis. Brain 2000, 123, 125–140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ertekin, C.; Aydogdu, I.; Tarlaci, S.; Turman, A.B.; Kiylioglu, N. Mechanisms of dysphagia in suprabulbar palsy with lacunar infarct. Stroke 2000, 31, 1370–1376. [Google Scholar] [CrossRef] [Green Version]
- Krasnodębska, P.; Jarzyńska-Bućko, A.; Szkiełkowska, A.; Bartosik, J. Clinical and Electromyographic Assessment of Swallowing in Individuals with Functional Dysphonia Associated with Dysphagia Due to Muscle Tension or Atypical Swallowing. Audiol. Res. 2021, 11, 167–178. [Google Scholar] [CrossRef]
- Taniguchi, H.; Tsukada, T.; Ootaki, S.; Yamada, Y.; Inoue, M. Correspondence between food consistency and suprahyoid muscle activity, tongue pressure, and bolus transit times during the oropharyngeal phase of swallowing. J. Appl. Physiol. 2008, 105, 791–799. [Google Scholar] [CrossRef] [Green Version]
- Nascimento, W.; A Cassiani, R.; Santos, C.M.; O Dantas, R. Effect of Bolus Volume and Consistency on Swallowing Events Duration in Healthy Subjects. J. Neurogastroenterol. Motil. 2015, 21, 078–082. [Google Scholar] [CrossRef] [Green Version]
- Youmans, S.R.; Stierwalt, J.A.G. Normal swallowing acoustics across age, gender, bolus viscosity, and bolus volume. Dysphagia 2011, 26, 374–384. [Google Scholar] [CrossRef]
- Lee, J.; Sejdić, E.; Steele, C.M.; Chau, T. Effects of liquid stimuli on dual-axis swallowing accelerometry signals in a healthy population. Biomed. Eng. Online 2010, 9, 7. [Google Scholar] [CrossRef] [Green Version]
- Funami, T.; Ishihara, S.; Nakauma, M.; Kohyama, K.; Nishinari, K. Texture design for products using food hydrocolloids. Food Hydrocoll. 2012, 26, 412–420. [Google Scholar] [CrossRef]
- Igarashi, A.; Kawasaki, M.; Nomura, S.-I.; Sakai, Y.; Ueno, M.; Ashida, I.; Miyaoka, Y. Sensory and Motor Responses of Normal Young Adults During Swallowing of Foods with Different Properties and Volumes. Dysphagia 2009, 25, 198–206. [Google Scholar] [CrossRef] [PubMed]
- Sifrim, D.; Vilardell, N.; Clavé, P. Oropharyngeal Dysphagia and Swallowing Dysfunction. Front. Gastrointest. Res. 2014, 33, 1–13. [Google Scholar]
- Suzuki, M.; Sasaki, M.; Kamata, K.; Nakayama, A.; Shibamoto, I.; Tamada, Y. Swallowing Pattern Classification Method Using Multichannel Surface EMG Signals of Suprahyoid and Infrahyoid Muscles. Adv. Biomed. Eng. 2020, 9, 10–20. [Google Scholar] [CrossRef] [Green Version]
- Molfenter, S.M.; Steele, C. Physiological Variability in the Deglutition Literature: Hyoid and Laryngeal Kinematics. Dysphagia 2010, 26, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Archer, S.K.; Garrod, R.; Hart, N.; Miller, S. Dysphagia in Duchenne Muscular Dystrophy Assessed Objectively by Surface Electromyography. Dysphagia 2012, 28, 188–198. [Google Scholar] [CrossRef] [PubMed]






| From | |||||||
|---|---|---|---|---|---|---|---|
| RM | LM | RSH | LSH | RIH | LIH | ||
| To | RM | 78%|79% | 85%|79% | 66%|57% | 84%|75% | 65%|53% | |
| LM | 72%|77% | 73%|63% | 94%|69% | 59%|70% | 90%|72% | ||
| RSH | 83%|68% | 67%|63% | 100%|97% | 88%|96% | 71%|58% | ||
| LSH | 67%|62% | 76%|75% | 100%|91% | 69%|63% | 92%|85% | ||
| RIH | 78%|63% | 68%|65% | 96%|92% | 74%|75% | 98%|95% | ||
| LIH | 57%|55% | 82%|74% | 82%|78% | 94%|95% | 98%|97% | ||
| Average | Bilateral | 91%|89% | Ipsilateral | 87%|78% | Contralateral | 68%|64% | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ye-Lin, Y.; Prats-Boluda, G.; Galiano-Botella, M.; Roldan-Vasco, S.; Orozco-Duque, A.; Garcia-Casado, J. Directed Functional Coordination Analysis of Swallowing Muscles in Healthy and Dysphagic Subjects by Surface Electromyography. Sensors 2022, 22, 4513. https://doi.org/10.3390/s22124513
Ye-Lin Y, Prats-Boluda G, Galiano-Botella M, Roldan-Vasco S, Orozco-Duque A, Garcia-Casado J. Directed Functional Coordination Analysis of Swallowing Muscles in Healthy and Dysphagic Subjects by Surface Electromyography. Sensors. 2022; 22(12):4513. https://doi.org/10.3390/s22124513
Chicago/Turabian StyleYe-Lin, Yiyao, Gema Prats-Boluda, Marina Galiano-Botella, Sebastian Roldan-Vasco, Andres Orozco-Duque, and Javier Garcia-Casado. 2022. "Directed Functional Coordination Analysis of Swallowing Muscles in Healthy and Dysphagic Subjects by Surface Electromyography" Sensors 22, no. 12: 4513. https://doi.org/10.3390/s22124513
APA StyleYe-Lin, Y., Prats-Boluda, G., Galiano-Botella, M., Roldan-Vasco, S., Orozco-Duque, A., & Garcia-Casado, J. (2022). Directed Functional Coordination Analysis of Swallowing Muscles in Healthy and Dysphagic Subjects by Surface Electromyography. Sensors, 22(12), 4513. https://doi.org/10.3390/s22124513







