A Novel Non-Invasive Thermometer for Continuous Core Body Temperature: Comparison with Tympanic Temperature in an Acute Stroke Clinical Setting
Abstract
:1. Introduction
2. Materials and Methods
2.1. Novel Thermometer Characteristics
2.2. Tympanic and Forehead Temperature
2.3. Statistical Analyses
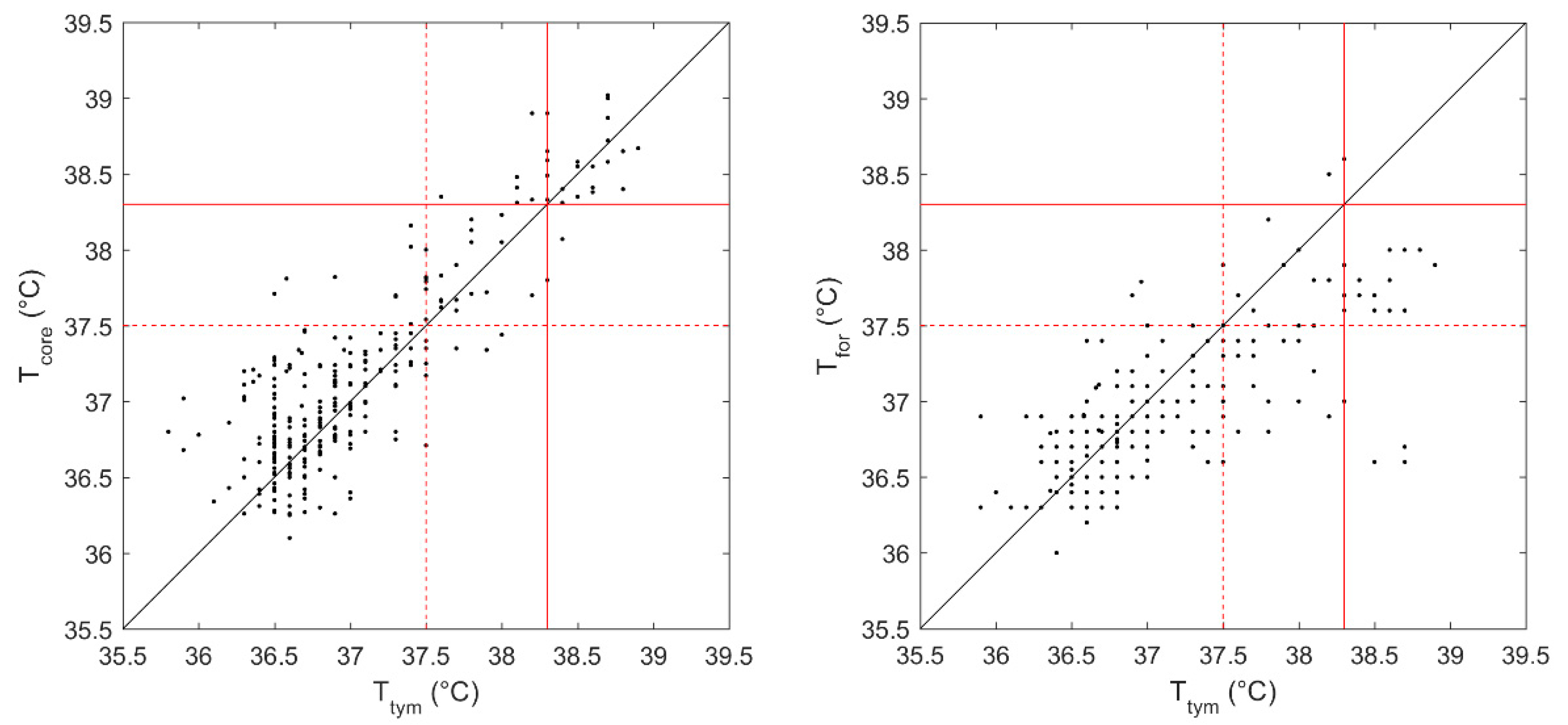
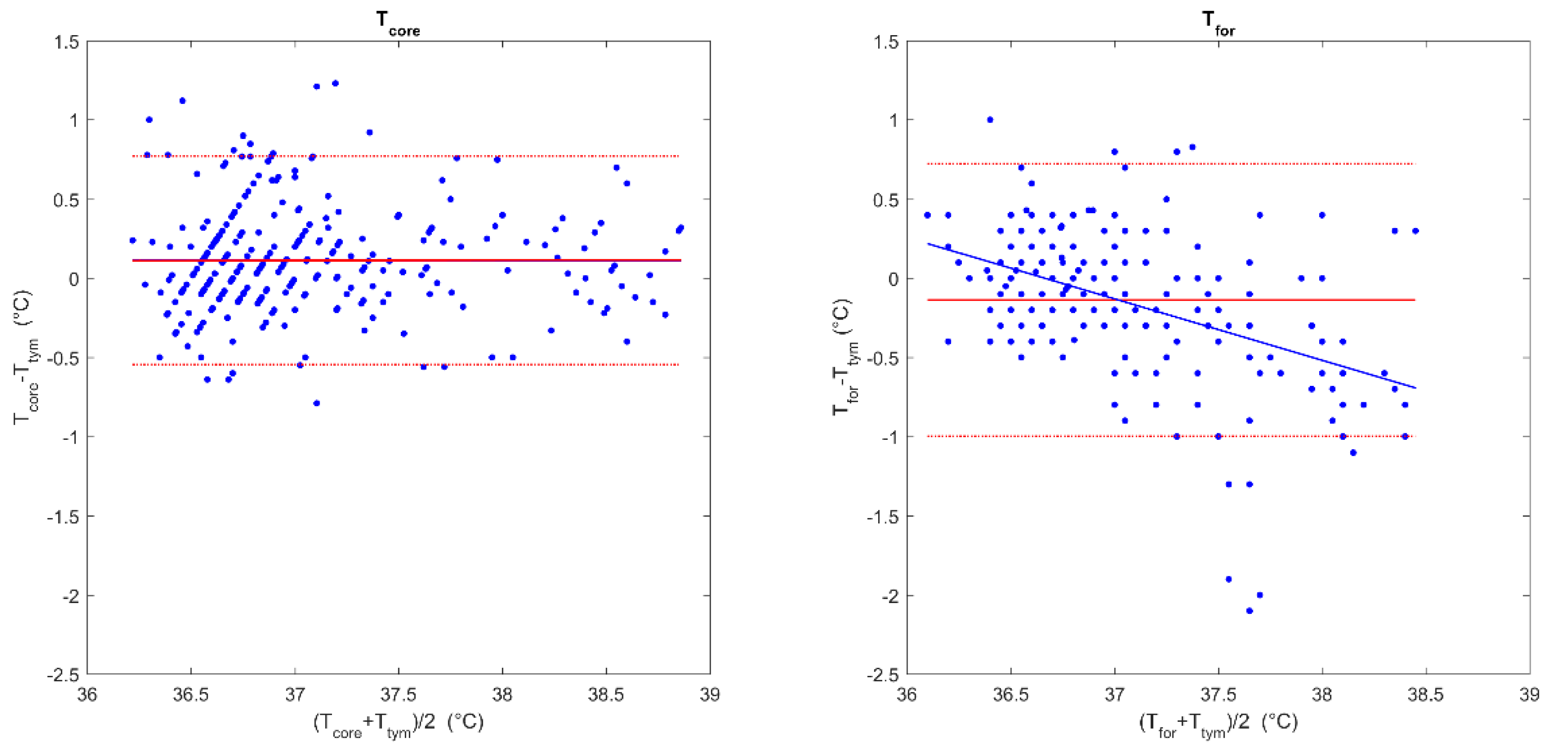
3. Results
Prediction Accuracy of the Presence or Absence of Hyperthermia and Fever
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Huang, F.; Magnin, C.; Brouqui, P. Ingestible Sensors Correlate Closely with Peripheral Temperature Measurements in Febrile Patients. J. Infect. 2020, 80, 161–166. [Google Scholar] [CrossRef] [Green Version]
- Vardasca, R.; Magalhaes, C.; Marques, D.; Moreira, J.; Frade, R.; Seixas, A.; Mendes, J.; Ring, F. Bilateral Assessment of Body Core Temperature through Axillar, Tympanic and Inner Canthi Thermometers in a Young Population. Physiol. Meas. 2019, 40, 094001. [Google Scholar] [CrossRef] [PubMed]
- Chen, W. Thermometry and Interpretation of Body Temperature. Biomed. Eng. Lett. 2019, 9, 3–17. [Google Scholar] [CrossRef] [PubMed]
- Childs, C. Body Temperature and Clinical Thermometry. Handb. Clin. Neurol. 2018, 157, 467–482. [Google Scholar] [CrossRef] [PubMed]
- Taylor, N.A.S.; Tipton, M.J.; Kenny, G.P. Considerations for the Measurement of Core, Skin and Mean Body Temperatures. J. Therm. Biol. 2014, 46, 72–101. [Google Scholar] [CrossRef] [Green Version]
- Kimberger, O.; Thell, R.; Schuh, M.; Koch, J.; Sessler, D.I.; Kurz, A. Accuracy and Precision of a Novel Non-Invasive Core Thermometer. Br. J. Anaesth. 2009, 103, 226–231. [Google Scholar] [CrossRef] [Green Version]
- Pecoraro, V.; Petri, D.; Costantino, G.; Squizzato, A.; Moja, L.; Virgili, G.; Lucenteforte, E. The Diagnostic Accuracy of Digital, Infrared and Mercury-in-Glass Thermometers in Measuring Body Temperature: A Systematic Review and Network Meta-Analysis. Intern. Emerg. Med. 2021, 16, 1071–1083. [Google Scholar] [CrossRef]
- Buoite Stella, A.; Manganotti, P.; Furlanis, G.; Accardo, A.; Ajčević, M. Return to School in the COVID-19 Era: Considerations for Temperature Measurement. J. Med. Eng. Technol. 2020, 44, 468–471. [Google Scholar] [CrossRef]
- Niven, D.J.; Gaudet, J.E.; Laupland, K.B.; Mrklas, K.J.; Roberts, D.J.; Stelfox, H.T. Accuracy of Peripheral Thermometers for Estimating Temperature: A Systematic Review and Meta-Analysis. Ann. Intern. Med. 2015, 163, 768–777. [Google Scholar] [CrossRef]
- Diamond, A.; Lye, C.T.; Prasad, D.; Abbott, D. One Size Does Not Fit All: Assuming the Same Normal Body Temperature for Everyone Is Not Justified. PLoS ONE 2021, 16, e0245257. [Google Scholar] [CrossRef]
- Geneva, I.I.; Cuzzo, B.; Fazili, T.; Javaid, W. Normal Body Temperature: A Systematic Review. Open Forum Infect. Dis. 2019, 6, ofz032. [Google Scholar] [CrossRef] [PubMed]
- O’Grady, N.P.; Barie, P.S.; Bartlett, J.G.; Bleck, T.; Carroll, K.; Kalil, A.C.; Linden, P.; Maki, D.G.; Nierman, D.; Pasculle, W.; et al. Guidelines for Evaluation of New Fever in Critically Ill Adult Patients: 2008 Update from the American College of Critical Care Medicine and the Infectious Diseases Society of America. Crit. Care Med. 2008, 36, 1330–1349. [Google Scholar] [CrossRef]
- Bindu, B.; Bindra, A.; Rath, G. Temperature Management under General Anesthesia: Compulsion or Option. J. Anaesthesiol. Clin. Pharmacol. 2017, 33, 306–316. [Google Scholar] [CrossRef]
- Robinson, J.L.; Seal, R.F.; Spady, D.W.; Joffres, M.R. Comparison of Esophageal, Rectal, Axillary, Bladder, Tympanic, and Pulmonary Artery Temperatures in Children. J. Pediatr. 1998, 133, 553–556. [Google Scholar] [CrossRef]
- Lefrant, J.-Y.; Muller, L.; de La Coussaye, J.E.; Benbabaali, M.; Lebris, C.; Zeitoun, N.; Mari, C.; Saïssi, G.; Ripart, J.; Eledjam, J.-J. Temperature Measurement in Intensive Care Patients: Comparison of Urinary Bladder, Oesophageal, Rectal, Axillary, and Inguinal Methods versus Pulmonary Artery Core Method. Intensive Care Med. 2003, 29, 414–418. [Google Scholar] [CrossRef] [PubMed]
- Laupland, K.B. Fever in the Critically Ill Medical Patient. Crit. Care Med. 2009, 37, S273-8. [Google Scholar] [CrossRef] [PubMed]
- Erkens, R.; Wernly, B.; Masyuk, M.; Muessig, J.M.; Franz, M.; Schulze, P.C.; Lichtenauer, M.; Kelm, M.; Jung, C. Admission Body Temperature in Critically Ill Patients as an Independent Risk Predictor for Overall Outcome. Med. Princ. Pract. Int. J. Kuwait Univ. Health Sci. Cent. 2020, 29, 389–395. [Google Scholar] [CrossRef] [PubMed]
- Wrotek, S.E.; Kozak, W.E.; Hess, D.C.; Fagan, S.C. Treatment of Fever after Stroke: Conflicting Evidence. Pharmacotherapy 2011, 31, 1085–1091. [Google Scholar] [CrossRef] [Green Version]
- Kenny, T.; Barr, C.; Laver, K. Management of Fever, Hyperglycemia, and Dysphagia in an Acute Stroke Unit. Rehabil. Nurs. Off. J. Assoc. Rehabil. Nurses 2016, 41, 313–319. [Google Scholar] [CrossRef]
- Leys, D.; Ringelstein, E.B.; Kaste, M.; Hacke, W. The Main Components of Stroke Unit Care: Results of a European Expert Survey. Cerebrovasc. Dis. 2007, 23, 344–352. [Google Scholar] [CrossRef]
- Conway, A.; Bittner, M.; Phan, D.; Chang, K.; Kamboj, N.; Tipton, E.; Parotto, M. Accuracy and Precision of Zero-Heat-Flux Temperature Measurements with the 3MTM Bair HuggerTM Temperature Monitoring System: A Systematic Review and Meta-Analysis. J. Clin. Monit. Comput. 2021, 35, 39–49. [Google Scholar] [CrossRef] [PubMed]
- Mazgaoker, S.; Ketko, I.; Yanovich, R.; Heled, Y.; Epstein, Y. Measuring Core Body Temperature with a Non-Invasive Sensor. J. Therm. Biol. 2017, 66, 17–20. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, S.; Rinaldi, J.E.; Hariharan, P.; Casamento, J.P.; Baek, S.; Seay, N.; Vesnovsky, O.; Topoleski, L. Clinical evaluation of non-contact infrared thermometers. Sci. Rep. 2021, 11, 22079. [Google Scholar] [CrossRef]
- Hussain, A.S.; Hussain, H.S.; Betcher, N.; Behm, R.; Cagir, B. Proper use of noncontact infrared thermometry for temperature screening during COVID-19. Sci. Rep. 2021, 11, 11832. [Google Scholar] [CrossRef]
- Lai, F.; Li, X.; Wang, Q.; Luo, Y.; Wang, X.; Huang, X.; Zhang, J.; Peng, J.; Wang, Q.; Fan, L.; et al. Reliability of Non-Contact Infrared Thermometers for Fever Screening Under COVID-19. Risk Manag. Healthc. Policy 2022, 15, 447–456. [Google Scholar] [CrossRef] [PubMed]
- Gunga, H.-C.; Werner, A.; Stahn, A.; Steinach, M.; Schlabs, T.; Koralewski, E.; Kunz, D.; Belavý, D.L.; Felsenberg, D.; Sattler, F.; et al. The Double Sensor-A Non-Invasive Device to Continuously Monitor Core Temperature in Humans on Earth and in Space. Respir. Physiol. Neurobiol. 2009, 169, S63–S68. [Google Scholar] [CrossRef]
- Yan, F.; Zhang, D.; Xu, H.; Guo, H. Risk Factors for Fever in Critically Ill Patients with Acute New-Onset Stroke. Neurol. Res. 2008, 30, 394–399. [Google Scholar] [CrossRef]
- Leira, R.; Rodríguez-Yáñez, M.; Castellanos, M.; Blanco, M.; Nombela, F.; Sobrino, T.; Lizasoain, I.; Dávalos, A.; Castillo, J. Hyperthermia Is a Surrogate Marker of Inflammation-Mediated Cause of Brain Damage in Acute Ischaemic Stroke. J. Intern. Med. 2006, 260, 343–349. [Google Scholar] [CrossRef]
- Khan, S.; Ali, S.; Khan, A.; Bermak, A. Wearable Printed Temperature Sensors: Short Review on Latest Advances for Biomedical Applications. IEEE Rev. Biomed. Eng. 2021. Early Access. [Google Scholar] [CrossRef]
- Shan, C.; Hu, J.; Zou, J.; Zhang, A. Wearable Personal Core Body Temperature Measurement Considering Individual Differences and Dynamic Tissue Blood Perfusion. IEEE J. Biomed. Health Inform. 2021, 26, 2158–2168. [Google Scholar] [CrossRef]
- Chaglla, E.J.S.; Celik, N.; Balachandran, W. Measurement of Core Body Temperature Using Graphene-Inked Infrared Thermopile Sensor. Sensors 2018, 18, 3315. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Suleman, M.I.; Doufas, A.G.; Akca, O.; Ducharme, M.; Sessler, D.I. Insufficiency in a new temporal-artery thermometer for adult and pediatric patients. Anesth. Analg. 2002, 95, 67–71. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kimberger, O.; Cohen, D.; Illievich, U.; Lenhardt, R. Temporal artery versus bladder thermometry during perioperative and intensive care unit monitoring. Anesth. Analg. 2007, 105, 1042–1047. [Google Scholar] [CrossRef] [PubMed]
- Moran, J.L.; Peter, J.V.; Solomon, P.J.; Grealy, B.; Smith, T.; Ashforth, W.; Wake, M.; Peake, S.L.; Peisach, A.R. Tympanic temperature measurements: Are they reliable in the critically ill? A clinical study of measures of agreement. Crit. Care Med. 2007, 35, 155–164. [Google Scholar] [CrossRef] [PubMed]
- Sessler, D.I.; Lee, K.A.; McGuire, J. Isoflurane anesthesia and circadian temperature cycles in humans. Anesthesiology 1991, 75, 985–989. [Google Scholar] [CrossRef] [PubMed]
- Tayefeh, F.; Plattner, O.; Sessler, D.I.; Ikeda, T.; Marder, D. Circadian changes in the sweating-to-vasoconstriction interthreshold range. Pflug. Archiv. Eur. J. Physiol. 1998, 435, 402–406. [Google Scholar] [CrossRef]
- Tsadok, I.; Scheinowitz, M.; Shpitzer, S.A.; Ketko, I.; Epstein, Y.; Yanovich, R. Assessing Rectal Temperature with a Novel Non-Invasive Sensor. J. Therm. Biol. 2021, 95, 102788. [Google Scholar] [CrossRef]
- Moyen, N.E.; Bapat, R.C.; Tan, B.; Hunt, L.A.; Jay, O.; Mündel, T. Accuracy of Algorithm to Non-Invasively Predict Core Body Temperature Using the Kenzen Wearable Device. Int. J. Environ. Res. Public Health 2021, 18, 3126. [Google Scholar] [CrossRef]
- Verdel, N.; Podlogar, T.; Ciuha, U.; Holmberg, H.-C.; Debevec, T.; Supej, M. Reliability and Validity of the CORE Sensor to Assess Core Body Temperature during Cycling Exercise. Sensors 2021, 21, 5932. [Google Scholar] [CrossRef]
- Dakappa, P.H.; Bhat, G.K.; Bolumbu, G.; Rao, S.B.; Adappa, S.; Mahabala, C. Comparison of Conventional Mercury Thermometer and Continuous TherCom(®) Temperature Recording in Hospitalized Patients. J. Clin. Diagn. Res. 2016, 10, OC43–OC46. [Google Scholar] [CrossRef]
- Liu, Y.; Liu, C.; Gao, M.; Wang, Y.; Bai, Y.; Xu, R.; Gong, R. Evaluation of a Wearable Wireless Device with Artificial Intelligence, IThermonitor WT705, for Continuous Temperature Monitoring for Patients in Surgical Wards: A Prospective Comparative Study. BMJ Open 2020, 10, e039474. [Google Scholar] [CrossRef] [PubMed]
- Verma, N.; Haji-Abolhassani, I.; Ganesh, S.; Vera-Aguilera, J.; Paludo, J.; Heitz, R.; Markovic, S.N.; Kulig, K.; Ghoreyshi, A. A Novel Wearable Device for Continuous Temperature Monitoring & Fever Detection. IEEE J. Transl. Eng. Health Med. 2021, 9, 2700407. [Google Scholar] [CrossRef] [PubMed]
- Buoite Stella, A.; Filingeri, D.; Ravanelli, N.; Morrison, S.A.; Ajčević, M.; Furlanis, G.; Manganotti, P. Heat Risk Exacerbation Potential for Neurology Patients during the COVID-19 Pandemic and Related Isolation. Int. J. Biometeorol. 2021, 65, 627–630. [Google Scholar] [CrossRef] [PubMed]
- Kagiyama, N.; Hiki, M.; Matsue, Y.; Dohi, T.; Matsuzawa, W.; Daida, H.; Minamino, T.; Kasai, T. Validation of Telemedicine-Based Self-Assessment of Vital Signs for Patients with COVID-19: A Pilot Study. J. Telemed. Telecare 2021, 1357633X211011825. [Google Scholar] [CrossRef]
- Ajčević, M.; Furlanis, G.; Naccarato, M.; Caruso, P.; Polverino, P.; Marsich, A.; Accardo, A.; Manganotti, P. E-Health Solution for Home Patient Telemonitoring in Early Post-Acute TIA/Minor Stroke during COVID-19 Pandemic. Int. J. Med. Inform. 2021, 152, 104442. [Google Scholar] [CrossRef] [PubMed]
- Polverino, P.; Ajčević, M.; Catalan, M.; Bertolotti, C.; Furlanis, G.; Marsich, A.; Buoite Stella, A.; Accardo, A.; Manganotti, P. Comprehensive Telemedicine Solution for Remote Monitoring of Parkinson’s Disease Patients with Orthostatic Hypotension during COVID-19 Pandemic. Neurol. Sci. Off. J. Ital. Neurol. Soc. Ital. Soc. Clin. Neurophysiol. 2022, 43, 3479–3487. [Google Scholar] [CrossRef]
- Summers, D.; Leonard, A.; Wentworth, D.; Saver, J.L.; Simpson, J.; Spilker, J.A.; Hock, N.; Miller, E.; Mitchell, P.H. Comprehensive Overview of Nursing and Interdisciplinary Care of the Acute Ischemic Stroke Patient: A Scientific Statement from the American Heart Association. Stroke 2009, 40, 2911–2944. [Google Scholar] [CrossRef] [Green Version]
- Thompson, H.J. Evidence-Base for Fever Interventions Following Stroke. Stroke 2015, 46, e98–e100. [Google Scholar] [CrossRef] [Green Version]
- Pusnik, I.; van der Ham, E.; Drnovsek, J. IR Ear Thermometers: What Do They Measure and How Do They Comply with the EU Technical Regulation? Physiol. Meas. 2004, 25, 699–708. [Google Scholar] [CrossRef] [Green Version]
- Dell’Isola, G.B.; Cosentini, E.; Canale, L.; Ficco, G.; Dell’Isola, M. Noncontact Body Temperature Measurement: Uncertainty Evaluation and Screening Decision Rule to Prevent the Spread of COVID-19. Sensors 2021, 21, 346. [Google Scholar] [CrossRef]
- Kameda, N. Clinical Accuracy of Non-Contact Forehead Infrared Thermometer and Infrared Tympanic Thermometer in Postoperative Adult Patients: A Comparative Study. J. Perioper. Pract. 2021, 32, 142–148. [Google Scholar] [CrossRef] [PubMed]
- Mekjavic, I.B.; Tipton, M.J. Myths and Methodologies: Degrees of Freedom—Limitations of Infrared Thermographic Screening for Covid-19 and Other Infections. Exp. Physiol. 2020. Early View. [Google Scholar] [CrossRef] [PubMed]
- Mogensen, C.B.; Wittenhoff, L.; Fruerhøj, G.; Hansen, S. Forehead or Ear Temperature Measurement Cannot Replace Rectal Measurements, except for Screening Purposes. BMC Pediatr. 2018, 18, 15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, H.Y.; Chen, A.; Chen, C. Investigation of the Impact of Infrared Sensors on Core Body Temperature Monitoring by Comparing Measurement Sites. Sensors 2020, 20, 2885. [Google Scholar] [CrossRef]
- Dwith Chenna, Y.N.; Ghassemi, P.; Pfefer, T.J.; Casamento, J.; Wang, Q. Free-Form Deformation Approach for Registration of Visible and Infrared Facial Images in Fever Screening. Sensors 2018, 18, 125. [Google Scholar] [CrossRef] [Green Version]
- Silawan, N.; Kusukame, K.; Kek, K.J.; Kuan, W.S. A Novel Environment-Invariant Core Body Temperature Estimation for High Sensitivity and Specificity Fever Screening. In Proceedings of the 2018 40th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Honolulu, HI, USA, 18–21 July 2018; pp. 1612–1615. [Google Scholar] [CrossRef]
- Atallah, L.; Ciuhu, C.; Paulussen, I.; Bongers, E.; Blom, A.; Idrissi, A.; Noordergraaf, G. Perioperative measurement of core body temperature using an unobtrusive passive heat flow sensor. J. Clin. Monit. Comput. 2020, 34, 1351–1359. [Google Scholar] [CrossRef]
- Teunissen, L.P.J.; Klewer, J.; de Haan, A.; de Koning, J.J.; Daanen, H.A.M. Non-Invasive Continuous Core Temperature Measurement by Zero Heat Flux. Physiol. Meas. 2011, 32, 559–570. [Google Scholar] [CrossRef]
- Sung, D.S.; Sim, S.Y.; Jin, H.W.; Kwon, W.Y.; Kim, K.S.; Kim, T.; Jung, Y.S.; Ko, J.-I.; Shin, S.M.; Suh, G.J.; et al. Validation of Non-Invasive Brain Temperature Estimation Models during Swine Therapeutic Hypothermia. Physiol. Meas. 2019, 40, 25004. [Google Scholar] [CrossRef]
- West, N.; Cooke, E.; Morse, D.; Merchant, R.N.; Görges, M. Zero-Heat-Flux Core Temperature Monitoring System: An Observational Secondary Analysis to Evaluate Agreement with Naso-/Oropharyngeal Probe during Anesthesia. J. Clin. Monit. Comput. 2020, 34, 1121–1129. [Google Scholar] [CrossRef]
- Fox, R.H.; Solman, A.J.; Isaacs, R.; Fry, A.J.; MacDonald, I.C. A new method for monitoring deep body temperature from the skin surface. Clin. Sci. 1973, 44, 81–86. [Google Scholar] [CrossRef] [Green Version]
- Bräuer, A.; Fazliu, A.; Perl, T.; Heise, D.; Meissner, K.; Brandes, I.F. Accuracy of zero-heat-flux thermometry and bladder temperature measurement in critically ill patients. Sci. Rep. 2020, 10, 21746. [Google Scholar] [CrossRef] [PubMed]
- Iden, T.; Horn, E.P.; Bein, B.; Böhm, R.; Beese, J.; Höcker, J. Intraoperative temperature monitoring with zero heat flux technology (3M SpotOn sensor) in comparison with sublingual and nasopharyngeal temperature: An observational study. Eur. J. Anaesthesiol. 2015, 32, 387–391. [Google Scholar] [CrossRef] [PubMed]
- Mäkinen, M.T.; Pesonen, A.; Jousela, I.; Päivärinta, J.; Poikajärvi, S.; Albäck, A.; Salminen, U.S.; Pesonen, E. Novel Zero-Heat-Flux Deep Body Temperature Measurement in Lower Extremity Vascular and Cardiac Surgery. J. Cardiothorac. Vasc. Anesth. 2016, 30, 973–978. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Atallah, L.; Bongers, E.; Lamichhane, B.; Bambang-Oetomo, S. Unobtrusive monitoring of neonatal brain temperature using a zero-heat-flux sensor matrix. IEEE J. Biomed. Health Inform. 2016, 20, 100–107. [Google Scholar] [CrossRef]
| Participants (n = 30) | |
|---|---|
| Demographics | |
| Age, y | 71.9 ± 18.9 |
| Females, n (%) | 6 (20) |
| Body mass, kg | 69.9 ± 14.9 |
| Body height, m | 1.71 ± 9.8 |
| BMI, kg/m2 | 26.3 ± 2.5 |
| Stroke characteristics | |
| NIHSS | 7 ± 6 |
| mRS ≤ 2, n (%) | 30 (100) |
| Ischemic stroke, n (%) | 30 (100) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ajčević, M.; Buoite Stella, A.; Furlanis, G.; Caruso, P.; Naccarato, M.; Accardo, A.; Manganotti, P. A Novel Non-Invasive Thermometer for Continuous Core Body Temperature: Comparison with Tympanic Temperature in an Acute Stroke Clinical Setting. Sensors 2022, 22, 4760. https://doi.org/10.3390/s22134760
Ajčević M, Buoite Stella A, Furlanis G, Caruso P, Naccarato M, Accardo A, Manganotti P. A Novel Non-Invasive Thermometer for Continuous Core Body Temperature: Comparison with Tympanic Temperature in an Acute Stroke Clinical Setting. Sensors. 2022; 22(13):4760. https://doi.org/10.3390/s22134760
Chicago/Turabian StyleAjčević, Miloš, Alex Buoite Stella, Giovanni Furlanis, Paola Caruso, Marcello Naccarato, Agostino Accardo, and Paolo Manganotti. 2022. "A Novel Non-Invasive Thermometer for Continuous Core Body Temperature: Comparison with Tympanic Temperature in an Acute Stroke Clinical Setting" Sensors 22, no. 13: 4760. https://doi.org/10.3390/s22134760






