Slotted Monopole Patch Antenna for Microwave-Based Head Imaging Applications
Abstract
:1. Introduction
2. Materials and Methods
2.1. Initial Antenna Design
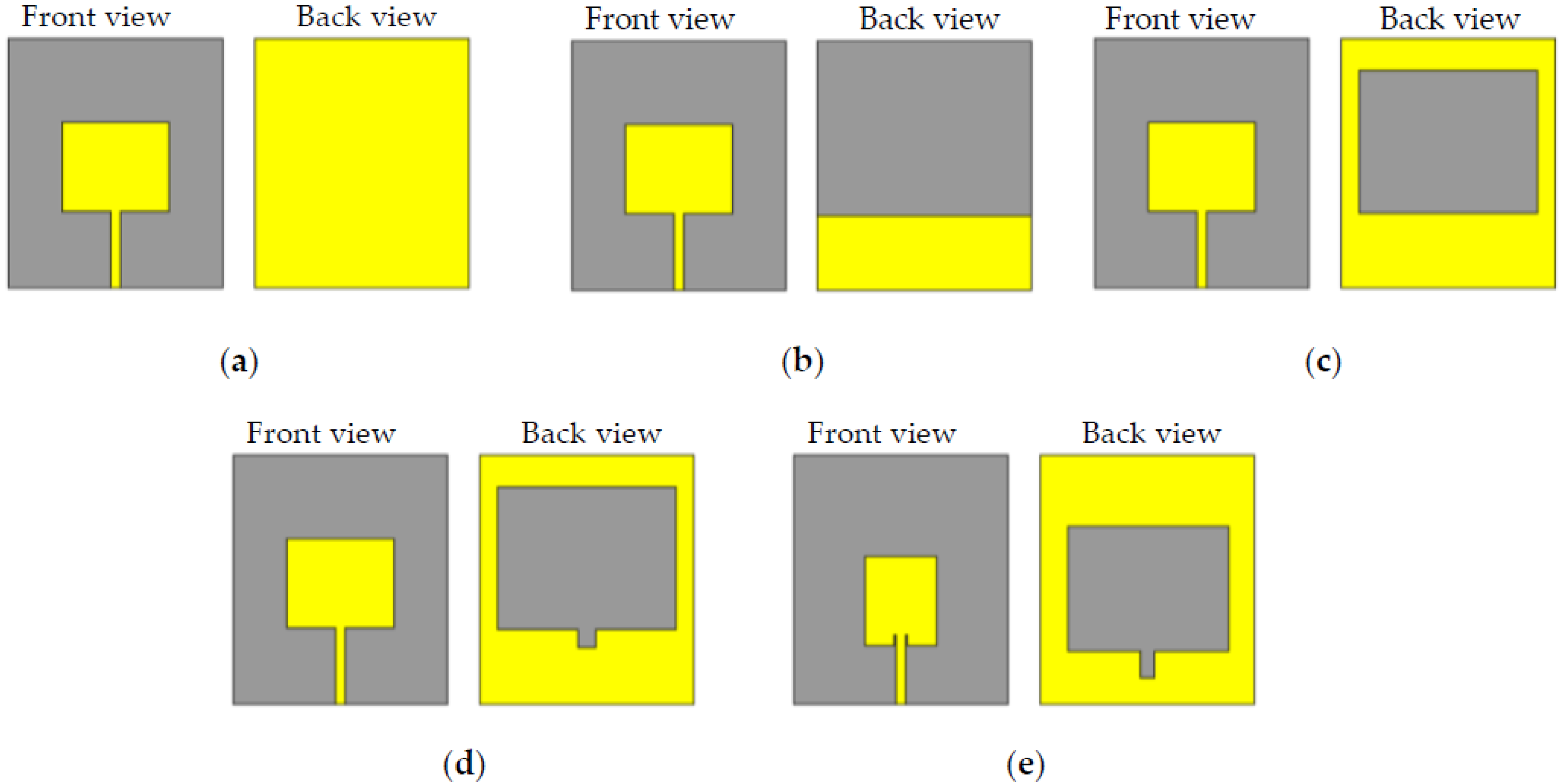
2.2. Parametric Study
2.3. The Proposed Antenna Design
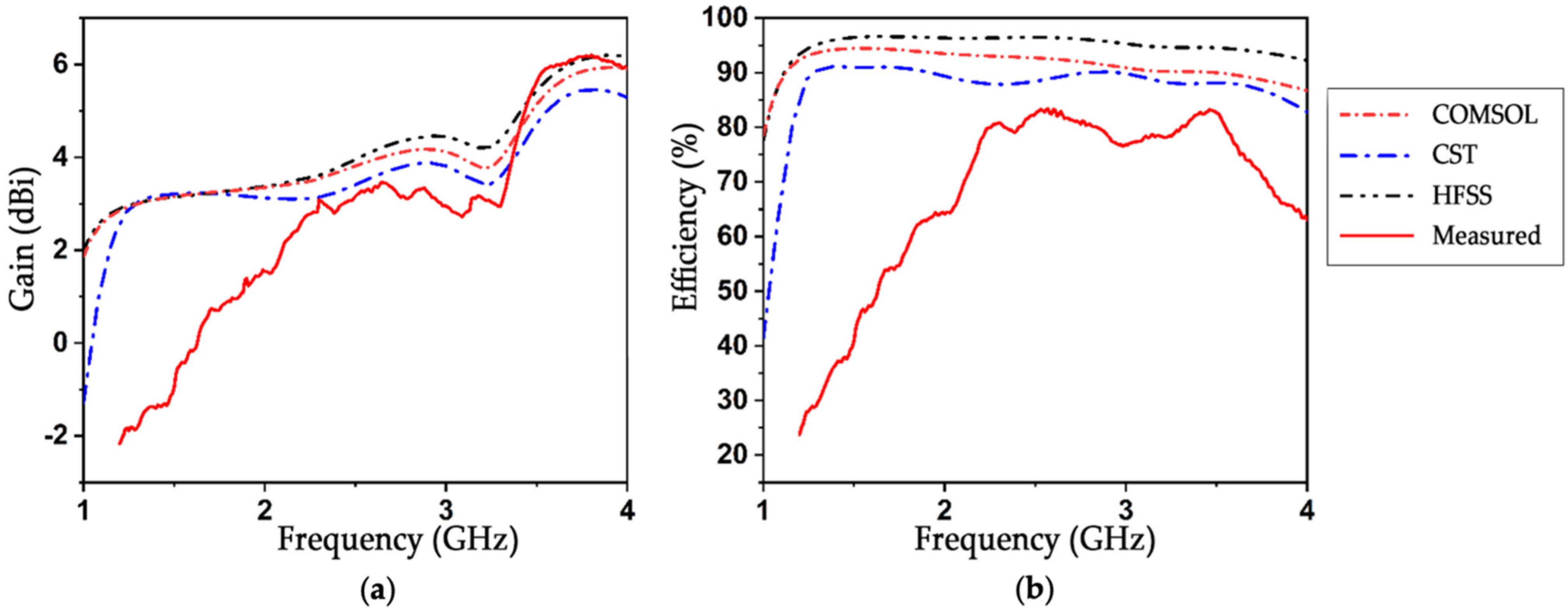
3. Results and Discussion
3.1. Surface Current Analysis
3.2. Antenna Fabrication and Frequency Domain Measurements
3.3. Time-Domain Analysis
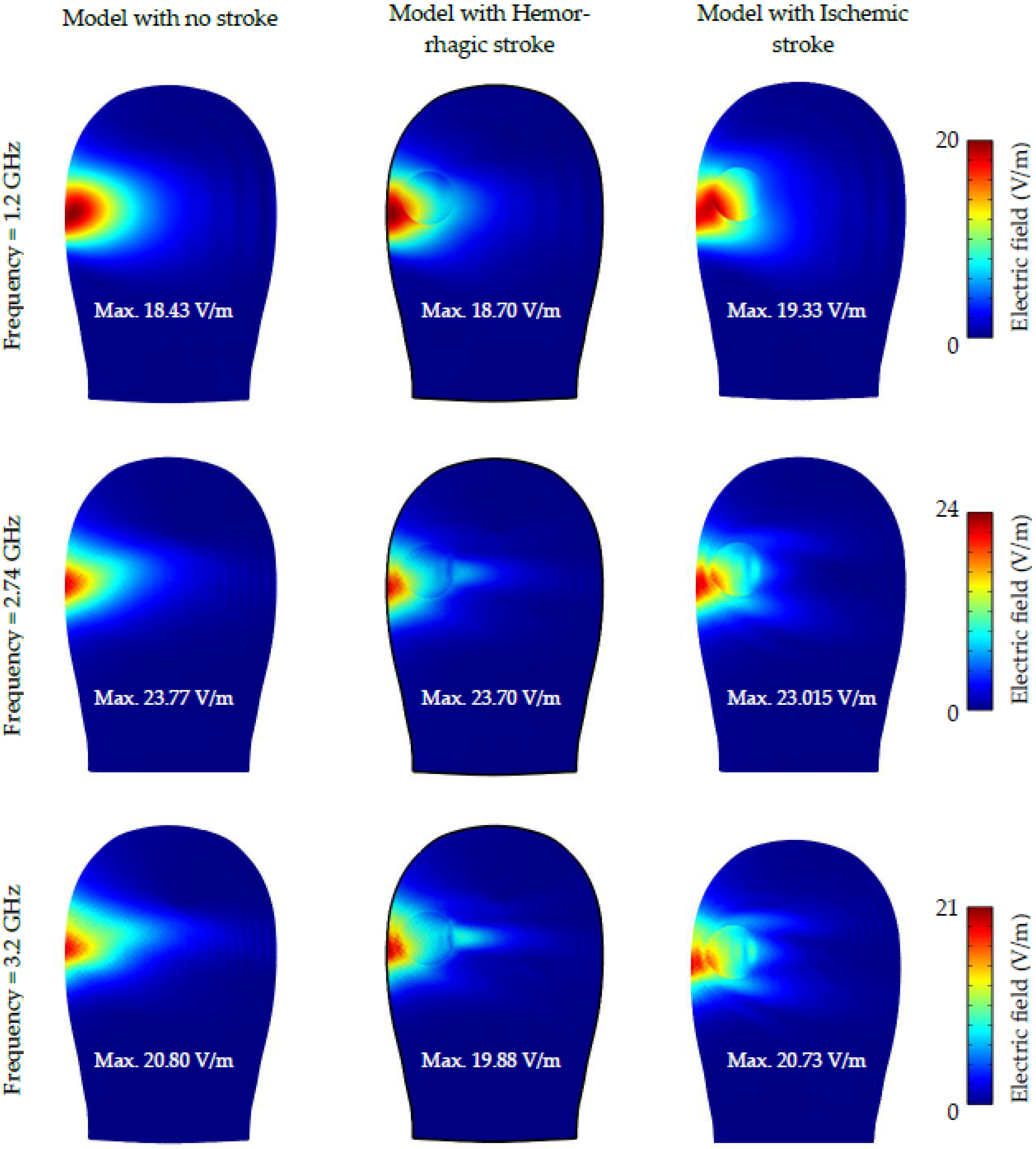
3.4. The Proposed Antenna for Head Imaging
3.5. Comparative Analysis
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Persson, M.; Fhager, A.; Trefna, H.D.; Yu, Y.; McKelvey, T.; Pegenius, G.; Karlsson, J.-E.; Elam, M. Microwave-Based Stroke Diagnosis Making Global Prehospital Thrombolytic Treatment Possible. IEEE Trans. Biomed. Eng. 2014, 61, 2806–2817. [Google Scholar] [CrossRef]
- Vasquez, J.A.T.; Scapaticci, R.; Turvani, G.; Bellizzi, G.; Rodriguez-Duarte, D.O.; Joachimowicz, N.; Duchêne, B.; Tedeschi, E.; Casu, M.R.; Crocco, L.; et al. A Prototype Microwave System for 3D Brain Stroke Imaging. Sensors 2020, 20, 2607. [Google Scholar] [CrossRef]
- Ireland, D.; Bialkowski, M. Feasibility study on microwave stroke detection using a realistic phantom and the FDTD method. In Proceedings of the 2010 Asia-Pacific Microwave Conference, Yokohama, Japan, 7–10 December 2010; IEEE: New York, NY, USA, 2010; pp. 1360–1363. [Google Scholar]
- Fhager, A.; Candefjord, S.; Elam, M.; Persson, M. Microwave Diagnostics Ahead: Saving Time and the Lives of Trauma and Stroke Patients. IEEE Microw. Mag. 2018, 19, 78–90. [Google Scholar] [CrossRef]
- Xu, J.; Chen, J.; Yu, W.; Zhang, H.; Wang, F.; Zhuang, W.; Yang, J.; Bai, Z.; Xu, L.; Sun, J.; et al. Noninvasive and portable stroke type discrimination and progress monitoring based on a multichannel microwave transmitting–receiving system. Sci. Rep. 2020, 10, 21647. [Google Scholar] [CrossRef]
- Mobashsher, A.T.; Mahmoud, A.; Abbosh, A.M. Portable Wideband Microwave Imaging System for Intracranial Hemorrhage Detection Using Improved Back-projection Algorithm with Model of Effective Head Permittivity. Sci. Rep. 2016, 6, 20459. [Google Scholar] [CrossRef]
- Qureshi, A.M.; Mustansar, Z.; Mustafa, S. Finite-element analysis of microwave scattering from a three-dimensional human head model for brain stroke detection. R. Soc. Open Sci. 2018, 5, 180319. [Google Scholar] [CrossRef]
- Stancombe, A.E.; Bialkowski, K.S.; Abbosh, A.M. Portable Microwave Head Imaging System Using Software-Defined Radio and Switching Network. IEEE J. Electromagn. RF Microwaves Med. Biol. 2019, 3, 284–291. [Google Scholar] [CrossRef]
- Rodriguez-Duarte, D.; Vasquez, J.T.; Scapaticci, R.; Turvani, G.; Cavagnaro, M.; Casu, M.; Crocco, L.; Vipiana, F. Experimental Validation of a Microwave System for Brain Stroke 3-D Imaging. Diagnostics 2021, 11, 1232. [Google Scholar] [CrossRef] [PubMed]
- Alqadami, A.S.M.; Nguyen-Trong, N.; Mohammed, B.; Stancombe, A.E.; Heitzmann, M.T.; Abbosh, A. Compact Unidirectional Conformal Antenna Based on Flexible High-Permittivity Custom-Made Substrate for Wearable Wideband Electromagnetic Head Imaging System. IEEE Trans. Antennas Propag. 2019, 68, 183–194. [Google Scholar] [CrossRef]
- Porter, E.; Kirshin, E.; Santorelli, A.; Coates, M.; Popovic, M. Time-Domain Multistatic Radar System for Microwave Breast Screening. IEEE Antennas Wirel. Propag. Lett. 2013, 12, 229–232. [Google Scholar] [CrossRef]
- Li, X.; Bond, E.; Van Veen, B.; Hagness, S. An overview of ultra-wideband microwave imaging via space-time beamforming for early-stage breast-cancer detection. IEEE Antennas Propag. Mag. 2005, 47, 19–34. [Google Scholar] [CrossRef]
- Hor, M.; Hikage, T.; Yamamoto, M. Linear Array of Leaf-Shaped Bowtie Slot Antenna Electromagnetically Fed by Microstrip Line. In Proceedings of the 2021 International Symposium on Antennas and Propagation (ISAP), Taipei, Taiwan, 19–22 October 2021; IEEE: New York, NY, USA, 2021; pp. 1–2. [Google Scholar]
- Mathur, P.; Kumar, G. Waveguide fed microstrip antenna array using i-shaped slots at ka-band. In Proceedings of the 2017 IEEE International Symposium on Antennas and Propagation & USNC/URSI National Radio Science Meeting, San Diego, CA, USA, 9–14 July 2017; IEEE: New York, NY, USA, 2017; pp. 2155–2156. [Google Scholar]
- Rafii, V.; Nourinia, J.; Ghobadi, C.; Pourahmadazar, J.; Virdee, B.S. Broadband circularly polarized slot antenna array using sequentially rotated technique for C -Band Applications. IEEE Antennas Wirel. Propag. Lett. 2013, 12, 128–131. [Google Scholar] [CrossRef]
- Rokunuzzaman, M.; Samsuzzaman, M.; Islam, M.T. Unidirectional Wideband 3-D Antenna for Human Head-Imaging Application. IEEE Antennas Wirel. Propag. Lett. 2016, 16, 169–172. [Google Scholar] [CrossRef]
- Zamani, A.; Abbosh, A.; Mobashsher, A.T. Fast Frequency-Based Multistatic Microwave Imaging Algorithm with Application to Brain Injury Detection. IEEE Trans. Microw. Theory Tech. 2016, 64, 653–662. [Google Scholar] [CrossRef]
- Dayo, Z.A.; Aamir, M.; Dayo, S.A.; Rahman, Z.; Khoso, I.A.; Shah, G.; Soothar, P.; Hu, Z.; Guan, Y. A Compact CPW-fed Multiband Bow-tie Slot Antenna for IoT Smart Healthcare Wireless Communication Applications. In Proceedings of the 2022 IEEE 95th Vehicular Technology Conference:(VTC2022-Spring), Helsinki, Finland, 19–22 June 2022; IEEE: New York, NY, USA, 2022; pp. 1–5. [Google Scholar]
- Hopfer, M.; Planas, R.; Hamidipour, A.; Henriksson, T.; Semenov, S. Electromagnetic Tomography for Detection, Differentiation, and Monitoring of Brain Stroke: A Virtual Data and Human Head Phantom Study. IEEE Antennas Propag. Mag. 2017, 59, 86–97. [Google Scholar] [CrossRef]
- Semenov, S.Y.; Svenson, R.H.; Bulyshev, A.E.; Souvorov, A.E.; Nazarov, A.G.; Sizov, Y.E.; Posukh, V.G.; Pavlovsky, A.; Repin, P.N.; Starostin, A.N.; et al. Three-dimensional microwave tomography: Initial experimental imaging of animals. IEEE Trans. Biomed. Eng. 2002, 49, 55–63. [Google Scholar] [CrossRef]
- Ahsan, S.; Guo, Z.; Miao, Z.; Sotiriou, I.; Koutsoupidou, M.; Kallos, E.; Palikaras, G.; Kosmas, P. Design and Experimental Validation of a Multiple-Frequency Microwave Tomography System Employing the DBIM-TwIST Algorithm. Sensors 2018, 18, 3491. [Google Scholar] [CrossRef]
- Mobashsher, A.T.; Abbosh, A.M. Compact 3-D Slot-Loaded Folded Dipole Antenna with Unidirectional Radiation and Low Impulse Distortion for Head Imaging Applications. IEEE Trans. Antennas Propag. 2016, 64, 3245–3250. [Google Scholar] [CrossRef]
- Samsuzzaman, M.; Fakeeh, K.A.; Talukder, S.; Hasan, M.; Rahman, H.; Alam, M.; Shaik, M.S.; Islam, M.T. A double hollow rectangular-shaped patch and with the slotted ground plane monopole wideband antenna for microwave head imaging applications. Int. J. Commun. Syst. 2021, 34, e4958. [Google Scholar] [CrossRef]
- Talukder, S.; Samsuzzaman; Islam, T.; Azim, R.; Mahmud, Z.; Islam, M.T. Compact ellipse shaped patch with ground slotted broadband monopole patch antenna for head imaging applications. Chin. J. Phys. 2021, 72, 310–326. [Google Scholar] [CrossRef]
- Alqadami, A.S.M.; Bialkowski, K.S.; Mobashsher, A.T.; Abbosh, A.M. Wearable Electromagnetic Head Imaging System Using Flexible Wideband Antenna Array Based on Polymer Technology for Brain Stroke Diagnosis. IEEE Trans. Biomed. Circuits Syst. 2018, 13, 124–134. [Google Scholar] [CrossRef]
- Hossain, A.; Islam, M.T.; Chowdhury, M.E.H. Samsuzzaman A Grounded Coplanar Waveguide-Based Slotted Inverted Delta-Shaped Wideband Antenna for Microwave Head Imaging. IEEE Access 2020, 8, 185698–185724. [Google Scholar] [CrossRef]
- Islam, M.S.; Hoque, A.; Islam, T.; Amin, N.; Chowdhury, M.E.H. A Portable Electromagnetic Head Imaging System Using Metamaterial Loaded Compact Directional 3D Antenna. IEEE Access 2021, 9, 50893–50906. [Google Scholar] [CrossRef]
- Sohani, B.; Khalesi, B.; Ghavami, N.; Ghavami, M.; Dudley, S.; Rahmani, A.; Tiberi, G. Detection of haemorrhagic stroke in simulation and realistic 3-D human head phantom using microwave imaging. Biomed. Signal Process. Control 2020, 61, 102001. [Google Scholar] [CrossRef]
- Sohani, B.; Tiberi, G.; Ghavami, N.; Ghavami, M.; Dudley, S.; Rahmani, A. Microwave imaging for stroke detection: Validation on head-mimicking phantom. In Proceedings of the 2019 PhotonIcs & Electromagnetics Research Symposium-Spring (PIERS-Spring), Rome, Italy, 17–20 June 2019; IEEE: New York, NY, USA, 2019; pp. 940–948. [Google Scholar]
- Talukder, M.S.; Samsuzzaman, M.; Hasan, M.M.; Islam, M.T.; Islam, M.T.; Rahman, M.N. Square Enclosed Circle Microstrip Patch Antenna for Microwave Head Imaging. In Proceedings of the 2020 23rd International Conference on Computer and Information Technology (ICCIT), Dhaka, Bangladesh, 19–21 December 2020; IEEE: New York, NY, USA, 2020; pp. 1–5. [Google Scholar]
- Yin, B.; Ye, M.; Yu, Y. A Novel Compact Wearable Antenna Design for ISM Band. Prog. Electromagn. Res. C 2021, 107, 97–111. [Google Scholar] [CrossRef]
- Rokunuzzaman, M.; Ahmed, A.; Baum, T.C.; Rowe, W.S.T. Compact 3-D Antenna for Medical Diagnosis of the Human Head. IEEE Trans. Antennas Propag. 2019, 67, 5093–5103. [Google Scholar] [CrossRef]
- everythingRF. “RF & Microwave Community”. Available online: https://www.everythingrf.com/community/what-is-antenna-efficiency (accessed on 1 September 2022).
- Tang, M.-C.; Ziolkowski, R.W.; Xiao, S. Compact Hyper-Band Printed Slot Antenna with Stable Radiation Properties. IEEE Trans. Antennas Propag. 2014, 62, 2962–2969. [Google Scholar] [CrossRef]
- IEEE Recommended Practice for Determining the Peak Spatial-Average Specific Absorption Rate (SAR) in the Human Head from Wireless Communications Devices: Measurement Techniques; IEEE Std 1528-2013; Institute of Electrical and Electronic Engineers: Piscataway, NJ, USA, 2013; pp. 1–246. [CrossRef]
- Razzicchia, E.; Lu, P.; Guo, W.; Kosmas, P. A New Metasurface-Enhanced Microstrip Patch Antenna for Haemorrhagic Stroke Detection. In Proceedings of the 2021 15th European Conference on Antennas and Propagation (EuCAP), Düsseldorf, Germany, 22–26 March 2021; IEEE: New York, NY, USA, 2021; pp. 1–4. [Google Scholar]
- Qureshi, A.M.; Mustansar, Z. Levels of detail analysis of microwave scattering from human head models for brain stroke detection. PeerJ 2017, 5, e4061. [Google Scholar] [CrossRef]
- Mohammed, B.; Abbosh, A.; Ireland, D. Stroke detection based on variations in reflection coefficients of wideband antennas. In Proceedings of the 2012 IEEE International Symposium on Antennas and Propagation, Chicago, IL, USA, 8–14 July 2012; IEEE: New York, NY, USA, 2012; pp. 1–2. [Google Scholar]
- Zolgharni, M.; Ledger, P.; Griffiths, H. Forward modelling of magnetic induction tomography: A sensitivity study for detecting haemorrhagic cerebral stroke. Med. Biol. Eng. Comput. 2009, 47, 1301–1313. [Google Scholar] [CrossRef] [PubMed]
- Zolgharni, M.; Ledger, P.; Armitage, D.W.; Holder, D.; Griffiths, H. Imaging cerebral haemorrhage with magnetic induction tomography: Numerical modelling. Physiol. Meas. 2009, 30, S187–S200. [Google Scholar] [CrossRef]
- Rahman, M.A.; Hossain, M.F.; Riheen, M.A.; Sekhar, P.K. Early brain stroke detection using flexible monopole antenna. Prog. Electromagn. Res. C 2020, 99, 99–110. [Google Scholar] [CrossRef]
- Li, X.; Jalilvand, M.; Sit, Y.L.; Zwick, T. A Compact Double-Layer On-Body Matched Bowtie Antenna for Medical Diagnosis. IEEE Trans. Antennas Propag. 2014, 62, 1808–1816. [Google Scholar] [CrossRef]

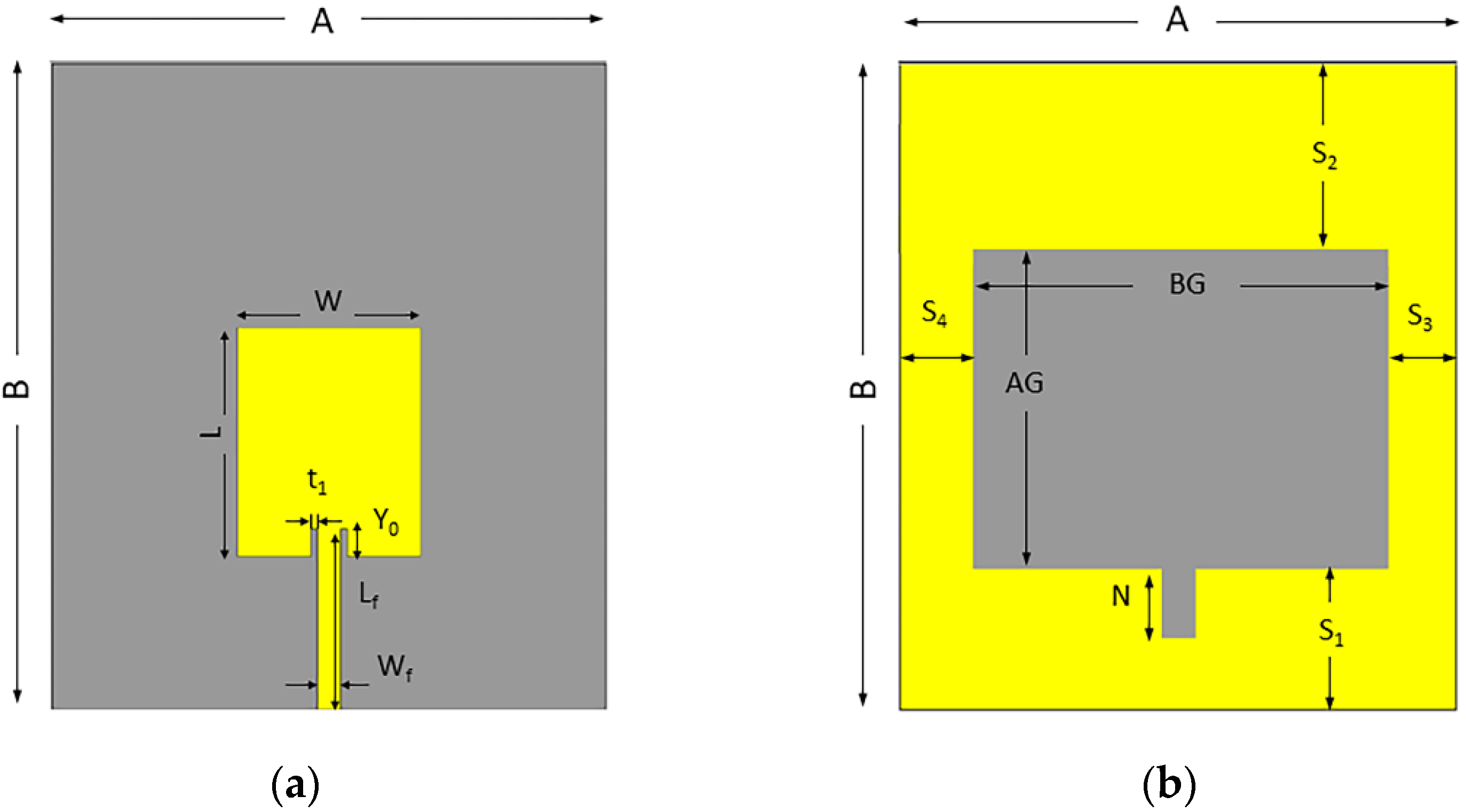









| Parameter | Value (mm) | Parameter | Value (mm) |
|---|---|---|---|
| A | 70 | AG | 35 |
| B | 60 | BG | 45 |
| L | 25 | N | 7.5 |
| W | 20 | S1 | 15 |
| Lf | 19.5 | S2 | 20 |
| Wf | 2.72 | S3 | 7.2 |
| Y0 | 3 | S4 | 7.8 |
| t1 | 0.5 |
| Modification | Operational Frequency (GHz) | Bandwidth (GHz) | Maximum Gain (dBi) |
|---|---|---|---|
| Full patch with full ground | No band | No band | N/A |
| Full patch with partial ground | 2.2–3.3 | 1.1 | 3.3101 |
| Full patch with slotted ground | 1.2–3 | 1.8 | 5.4508 |
| Full patch with full ground and notch | 1.2–3.1 | 1.9 | 5.118 |
| Proposed design | 1.3–3.7 | 2.4 | 6.15 |
| Year | Reference | Dimension (λ3) | Bandwidth (GHz) | Fractional Bandwidth (%) | Gain (dBi) | Efficiency (%) | Maximum SAR (W/kg) |
|---|---|---|---|---|---|---|---|
| 2019 | [10] | 0.083 × 0.09 × 0.018 | 1.00–2.00 | 66.6% | N/R | N/R | N/R |
| 2016 | [22] | 0.30 × 0.08 × 0.02 | 1.10–2.20 | 66.67% | 4.60 | >70 | N/R |
| 2018 | [25] | 0.33 × 0.23 × 0.015 | 1.16–1.94 | 50% | N/R | 83 | 0.500 |
| 2020 | [29] | 0.26 × 0.22 × 0.04 | 1.00–2.00 | 66.6% | Avg. 3.00 | N/R | N/R |
| 2021 | [24] | 0.277 × 0.238 × 0.006 | 1.19–3.56 | 100% | 5.95 | 85 | 0.927 |
| 2020 | [30] | 0.253 × 0.19 × 0.010 | 1.9–3.6 | 61.81% | 3.5 | <90 | N/R |
| 2020 | [28] | 0.263 × 0.227 × 0.004 | 1.0–2.0 | 66.6% | N/R | N/R | 0.45 |
| 2021 | [27] | 0.261 × 0.111 × 0.052 | 1.12–2.50 | 76.24% | >4 | >70 | >0.05 |
| 2020 | [26] | 0.283 × 0.250 × 0.009 | 1.70–3.71 | 74.4% | 5.6 | 90 | 0.0023 |
| 2021 | [31] | 0.49 × 0.49 × 0.02 | 2.20–2.80 | 24% | 4.7 | <90 | 0.24 |
| 2022 | Proposed | 0.32 × 0.28 × 0.007 | 1.3–3.7 | 94.34% | 6.15 | >90 | 0.1409 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alqahtani, A.; Islam, M.T.; Talukder, M.S.; Samsuzzaman, M.; Bakouri, M.; Mansouri, S.; Almoneef, T.; Dokos, S.; Alharbi, Y. Slotted Monopole Patch Antenna for Microwave-Based Head Imaging Applications. Sensors 2022, 22, 7235. https://doi.org/10.3390/s22197235
Alqahtani A, Islam MT, Talukder MS, Samsuzzaman M, Bakouri M, Mansouri S, Almoneef T, Dokos S, Alharbi Y. Slotted Monopole Patch Antenna for Microwave-Based Head Imaging Applications. Sensors. 2022; 22(19):7235. https://doi.org/10.3390/s22197235
Chicago/Turabian StyleAlqahtani, Abdulrahman, Mohammad Tariqul Islam, Md Siam Talukder, Md Samsuzzaman, Mohsen Bakouri, Sofiene Mansouri, Thamer Almoneef, Socrates Dokos, and Yousef Alharbi. 2022. "Slotted Monopole Patch Antenna for Microwave-Based Head Imaging Applications" Sensors 22, no. 19: 7235. https://doi.org/10.3390/s22197235







