Armband Sensors Location Assessment for Left Arm-ECG Bipolar Leads Waveform Components Discovery Tendencies around the MUAC Line
Abstract
1. Introduction
2. Materials and Methods
2.1. Extracted Data Set

2.2. Data Acquisition and Sensor System
2.2.1. Front-End Data Acquisition System and Signal Characteristics
2.2.2. Pre-Filtering
2.3. Bipolar Arm Leads Definitions
2.4. Data Processing Approach
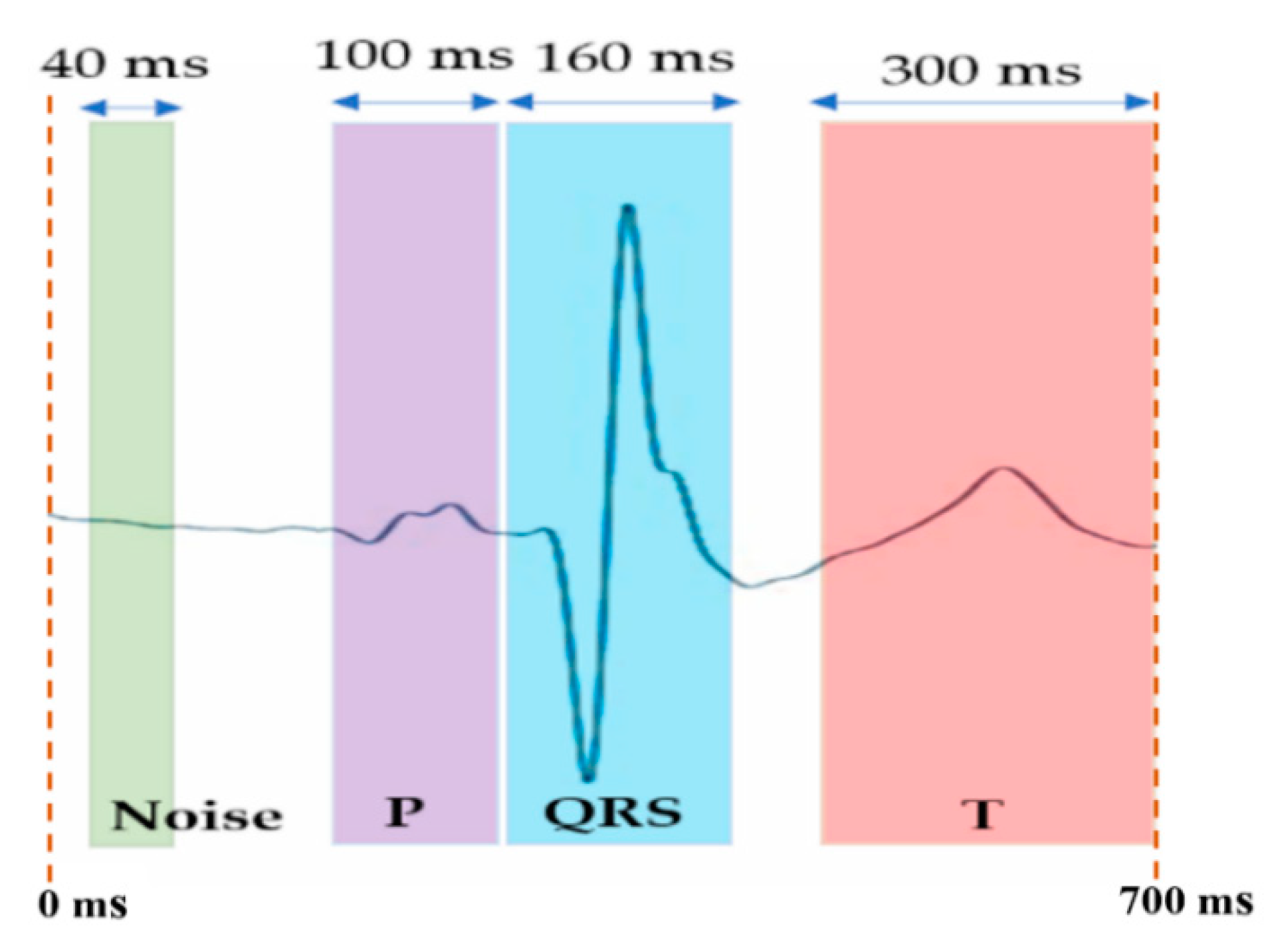
2.4.1. Signal-Averaged ECG Algorithm
2.4.2. Bipolar Arm-Lead ECG Event Discovery Quality Assessment Metrics
2.4.3. QRS Event Detection Performance
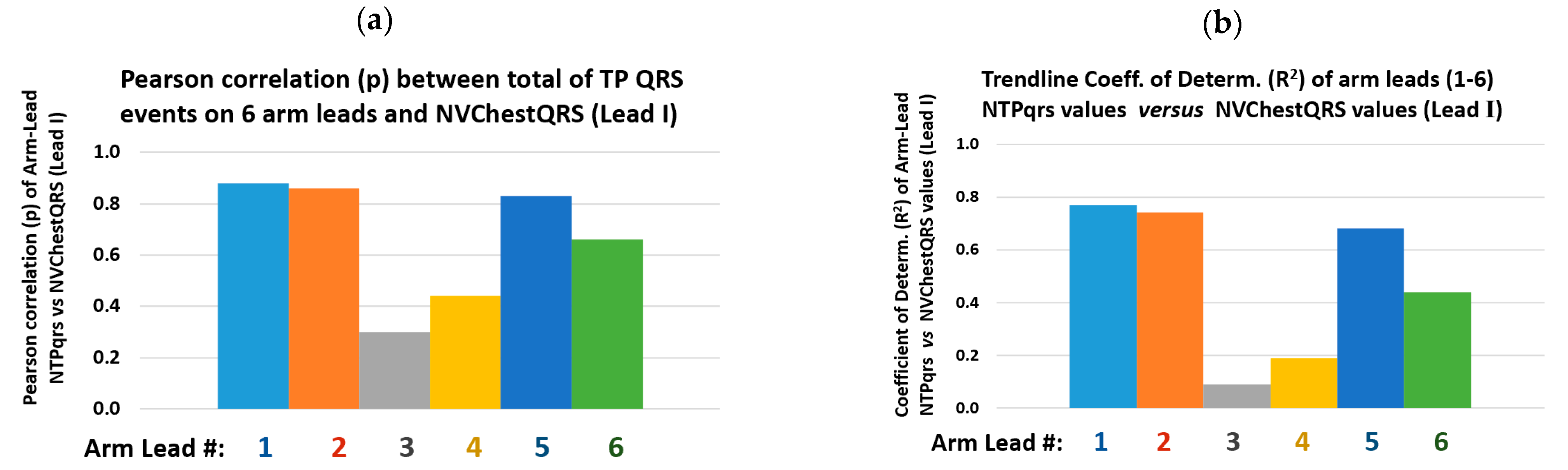
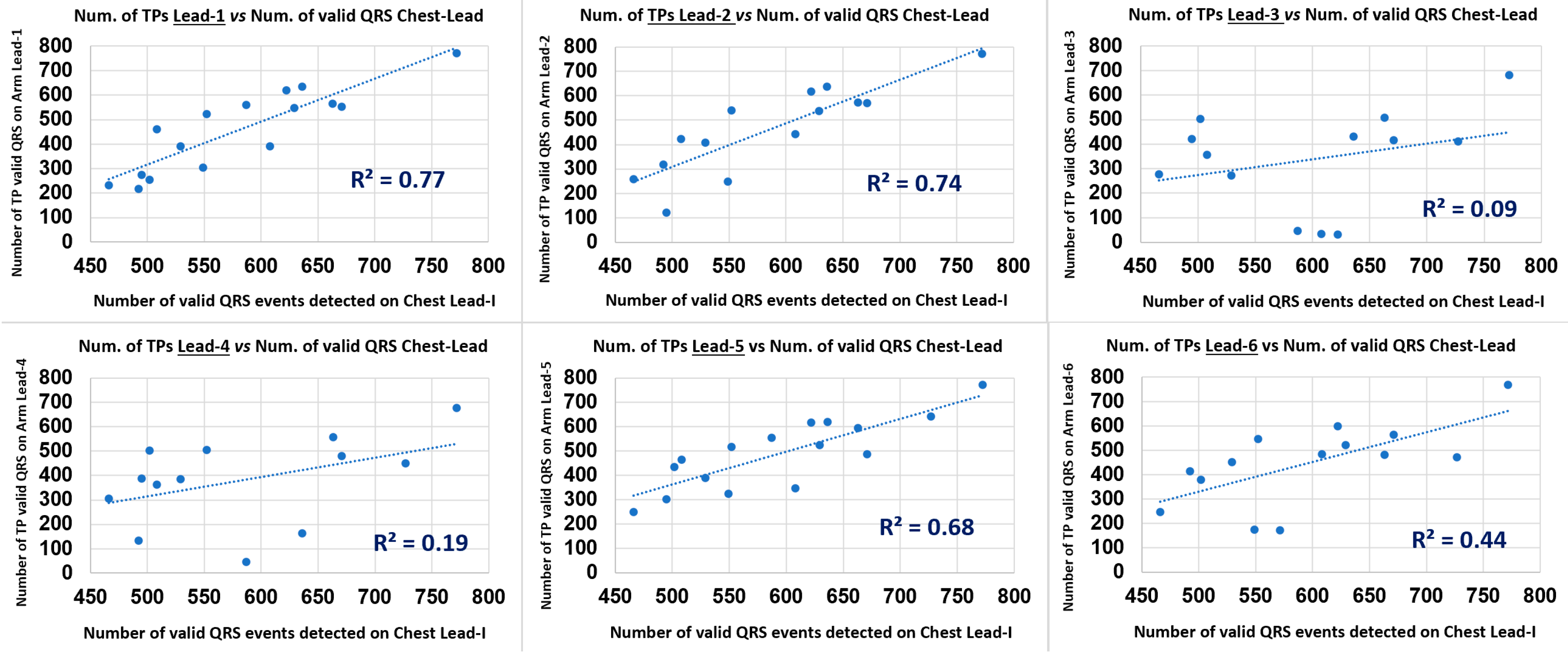
2.4.4. Arm Leads QRS Detection Performance Analysis
2.4.5. HRV Performance Metrics
2.5. Removing Outliers
3. Results
3.1. SAECG Bipolar Arm Lead Signal Enhancement Output
3.2. Bipolar Arm Leads ECG Waveform Events Discovery Quality (EDQ) Analysis
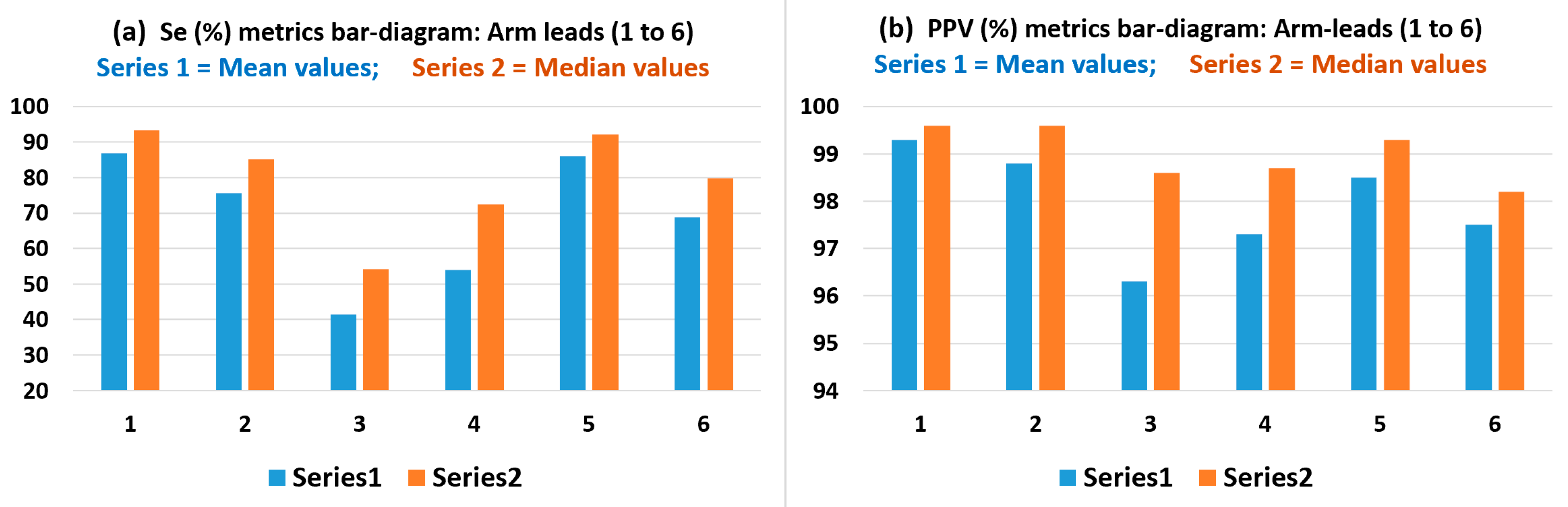
3.3. Arm Leads QRS Detection Sensitivity (Se) and Precision (PPV) Performance Analysis
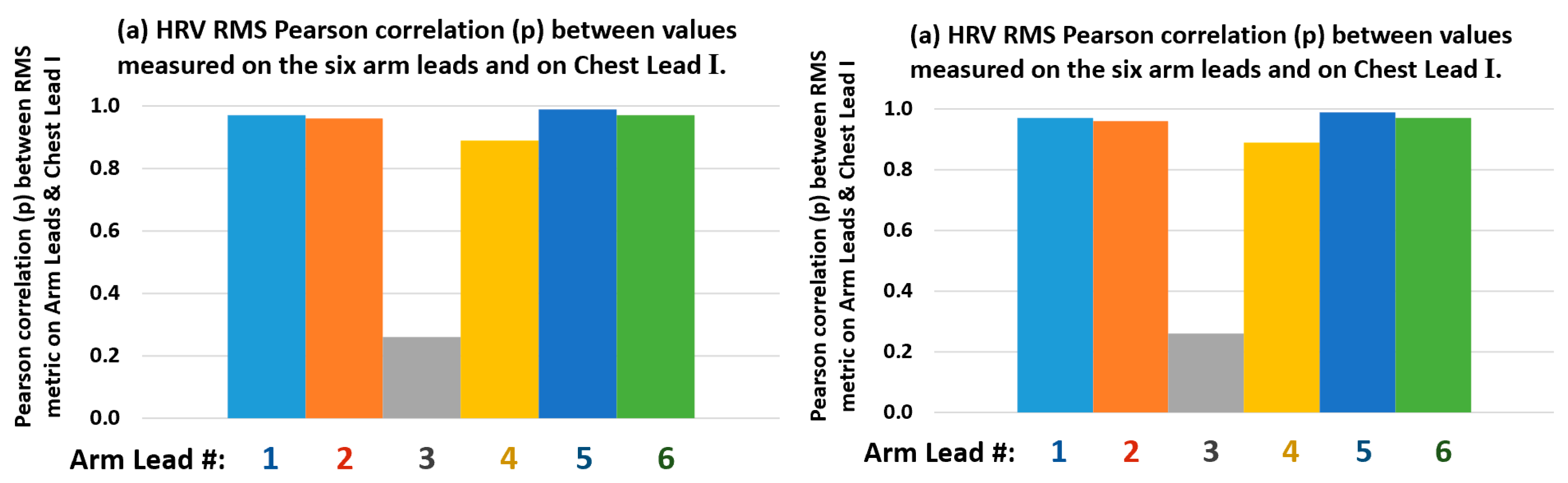
3.4. Arm Leads Comparative HRV Metrics Measurement Performance Analysis
3.5. Overall Results Summary
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Virani, S.S.; Alonso, A.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.M.; Cheng, S.; Delling, F.N.; et al. Heart Disease and Stroke Statistics—2020 Update: A Report from the American Heart Association. Circulation 2020, 141, e139–e596. [Google Scholar] [PubMed]
- Benjamin, E.J.; Muntner, P.; Alonso, A.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Das, S.R.; et al. Heart disease and stroke statistics—2019. Update: A report from the American Heart Association. Circulation 2019, 139, e56–e528. [Google Scholar] [CrossRef]
- Mann, I.; Sandler, B.; Linton, N.; Kanagaratnam, P. Drivers of Atrial Fibrillation: Theoretical Considerations and Practical Concerns. Arrhythmia Electrophysiol. Rev. 2018, 7, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Xi, Y.; Cheng, J. Dysfunction of the autonomic nervous system in atrial fibrillation. J. Thorac. Dis. 2015, 7, 193–198. [Google Scholar] [PubMed]
- Khan, A.A.; Lip, G.Y.H.; Shantsila, A. Heart rate variability in atrial fibrillation: The balance between sympathetic and parasympathetic nervous system. Eur. J. Clin. Investig. 2019, 49, e13174. [Google Scholar] [CrossRef]
- Shoushan, M.M.; Reyes, B.A.; Rodriguez, A.R.M.; Chong, J.W. Contactless Monitoring of Heart Rate Variability During Respiratory Maneuvers. IEEE Sens. J. 2022, 22, 14563–14573. [Google Scholar] [CrossRef]
- Lynn, W.D.; Escalona, O.J.; McEneaney, D.J. Arm and wrist surface potential mapping for wearable ECG rhythm recording devices: A pilot clinical study. J. Phys. Conf. Ser. 2013, 450, 012026. [Google Scholar] [CrossRef]
- Lazaro, J.; Reljin, N.; Hossain, M.-B.; Noh, Y.; Laguna, P.; Chon, K. Wearable Armband Device for Daily Life Electrocardiogram Monitoring. IEEE Trans. Biomed. Eng. 2020, 67, 3464–3473. [Google Scholar] [CrossRef]
- Lee, D.; Kwon, H.; Lee, H.; Seo, C.; Park, K. Optimal Lead Position in Patch-Type Monitoring Sensors for Reconstructing 12-Lead ECG Signals with Universal Transformation Coefficient. Sensors 2020, 20, 963. [Google Scholar] [CrossRef]
- Cosoli, G.; Spinsante, S.; Scardulla, F.; D’Acquisto, L.; Scalise, L. Wireless ECG and cardiac monitoring systems: State of the art, available commercial devices and useful electronic components. Meas. J. Int. Meas. Confed. 2021, 177, 109243. [Google Scholar] [CrossRef]
- Bae, T.W.; Kwon, K.K.; Kim, K.H. Vital Block and Vital Sign Server for ECG and Vital Sign Monitoring in a Portable u-Vital System. Sensors 2020, 20, 1089. [Google Scholar] [CrossRef] [PubMed]
- Escalona, O.J.; McFrederick, L.; Borge, M.; Perpiñan, G.; McLaughlin, J.; McEneaney, D. Wrist and Arm Body Surface Cardiac Electrogram Mapping Techniques Study for Long-Term Rhythm Monitoring. Comput. Cardiol. 2017, 44, 1–4. Available online: https://www.cinc.org/archives/2017/pdf/071-458.pdf (accessed on 20 August 2022).
- Mukhopadhyay, S.C. Wearable Sensors for Human Activity Monitoring: A Review. IEEE Sens. J. 2015, 15, 1321–1330. [Google Scholar] [CrossRef]
- Villegas, A.; McEneaney, D.; Escalona, O. Arm-ECG Wireless Sensor System for Wearable Long-Term Surveillance of Heart Arrhythmias. Electronics 2018, 8, 1300. [Google Scholar] [CrossRef]
- Vizcaya, P.; Perpiñan, G.; McEneaney, D.; Escalona, O.J. Standard ECG lead I prospective estimation study from far-field bipolar leads on the left upper arm: A neural network approach. Biomed. Signal Process. Control 2019, 51, 171–180. [Google Scholar] [CrossRef]
- Escalona, O.J.; Villegas, A.; Mukhtar, S.; Perpiñan, G.; McEneaney, D.J. Wireless Arm Wearable Sensor Band for Long-Term Heart Rhythms Surveillance Using a Bipolar Arm-ECG Lead. In Proceedings of the 2020 Computing in Cardiology, Rimini, Italy, 13–16 September 2020; pp. 1–4. [Google Scholar] [CrossRef]
- Escalona, O.J.; Lynn, W.D.; Perpiñan, G.; McFrederick, L.; McEneaney, D.J. Data-Driven ECG Denoising Techniques for Characterising Bipolar Lead Sets along the Left Arm in Wearable Long-Term Heart Rhythm Monitoring. Electronics 2017, 6, 84. [Google Scholar] [CrossRef]
- Lynn, W.D.; Escalona, O.J.; Vizcaya, P.; McEneaney, D. Arm-ECG Bipolar Leads Signal Recovery Methods for Wearable Long-term Heart Rate and Rhythm Monitoring. Comput. Cardiol. 2017, 44, 1–4. Available online: https://www.cinc.org/archives/2017/pdf/072-464.pdf (accessed on 20 August 2022).
- Pan, J.; Tompkins, W.J. A Real-Time QRS Detection Algorithm. IEEE Trans. Biomed. Eng. 1985, 32, 230–236. [Google Scholar] [CrossRef]
- Brito, N.B.; Llanos, J.P.S.; Ferrer, M.F.; García, J.G.O.; Brito, I.D.; Castro, F.P.-G.; Castellanos, N.C.; Rodríguez, C.X.A.; Abizanda, E.P. Relationship between Mid-Upper Arm Circumference and Body Mass Index in Inpatients. PLoS ONE 2016, 11, e0160480. [Google Scholar] [CrossRef]
- Kamiya, K.; Masuda, T.; Matsue, Y.; Inomata, T.; Hamazaki, N.; Matsuzawa, R.; Tanaka, S.; Nozaki, K.; Maekawa, E.; Noda, C.; et al. Complementary Role of Arm Circumference to Body Mass Index in Risk Stratification in Heart Failure. JACC Heart Fail. 2016, 4, 265–273. [Google Scholar] [CrossRef] [PubMed]
- MathWorks—Makers of MATLAB and Simulink, Mathworks.com. 2020. Available online: https://www.mathworks.com/ (accessed on 20 August 2022).
- Escalona, O.J.; Mitchell, R.H. Frequency bandwidth limitations in the signa--averaged ECG by the maximum coherence matching technique. Automedica 1991, 13, 177–187. [Google Scholar]
- Escalona, O.J.; Mitchell, R.; Balderson, D.; Harron, D. A fast and reliable QRS alignment technique for high-frequency analysis of the signal-averaged ECG. Med Biol. Eng. Comput. 1993, 3, S137–S146. [Google Scholar] [CrossRef] [PubMed]
- Ali, A.M.S. Pan Tompkins Algorithm based ECG Signal Classification. Res. J. Pharm. Technol. 2017, 10, 4365. [Google Scholar] [CrossRef]
- Fariha, M.A.Z.; Ikeura, R.; Hayakawa, S.; Tsutsumi, S. Analysis of Pan-Tompkins Algorithm Performance with Noisy ECG Signals. J. Phys. Conf. Ser. 2020, 1532, 012022. [Google Scholar] [CrossRef]
- McCallan, N.; Finlay, D.; Biglarbeigi, P.; Perpinan, G.; Jenning, M.; Ng, K.Y.; McLaughlin, J.; Escalona, O.J. Wearable Technology: Signal Recovery of Electrocardiogram from Short Spaced Leads in the Far-Field Using Discrete Wavelet Transform Based Techniques. Comput. Cardiol. 2019, 46, 1. [Google Scholar] [CrossRef]
- Nasir, I.M.; Khan, M.A.; Yasmin, M.; Shah, J.H.; Gabryel, M.; Scherer, R.; Damaševičius, R. Pearson Correlation-Based Feature Selection for Document Classification Using Balanced Training. Sensors 2020, 20, 6793. [Google Scholar] [CrossRef]
- Detect and Remove Outliers in Data—MATLAB Rmoutliers—MathWorks United Kingdom. Available online: https://uk.mathworks.com/help/matlab/ref/rmoutliers.html (accessed on 14 July 2022).
- Carlitz, L. The inverse of the error function. Pac. J. Math. 1963, 13, 459–470. [Google Scholar] [CrossRef][Green Version]
- Inverse complementary error function—MATLAB erfcinv—MathWorks United Kingdom. Available online: https://uk.mathworks.com/help/matlab/ref/erfcinv.html (accessed on 14 July 2022).
- Addison, P.S. Wavelet transforms and the ECG: A review. Physiol. Meas. 2005, 26, R155. [Google Scholar] [CrossRef]




| Bipolar Arm-Lead Definition | Bipolar Arm-Lead Axis Rotation Angle |
|---|---|
| Lead-1:(Ch8 − Ch10) | 0° |
| Lead-2:[Ch10 − {(Ch8 + Ch9)/2}] | 30° |
| Lead-3:[Ch9 − {(Ch8 + Ch10)/2}] | −60° |
| Lead-4:[Ch9 − {(Ch8 + Ch9 + 2 × Ch10)/3}] | −90° |
| Lead-5:(Ch8 − GND) | −30° |
| Lead-6:(Ch9 − Ch10) | 60° |
| Characteristics | Mean | SD | Median | IQR |
|---|---|---|---|---|
| Age (y): both genders | 40.3 | 15.3 | 37.0 | 21.8 |
| Age (y): females (77%) | 50.6 | 14.1 | 52.0 | 22.5 |
| Age (y): males (33%) | 27.3 | 4.7 | 29.0 | 4.5 |
| Height (m) | 1.68 | 0.12 | 1.68 | 0.17 |
| Weight (Kg) | 70.9 | 10.2 | 69.0 | 14.1 |
| BMI (Kg/m2) | 24.9 | 0.43 | 24.9 | 0.66 |
| MUAC (cm) | 28.6 | 0.50 | 28.5 | 0.76 |
| Pulse (bpm) | 73.0 | 9.1 | 72.0 | 12.5 |
| Lead # | QRS SNR | PqrsR [%] | TqrsR [%] | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Median | IQR | Mean | SD | Median | IQR | Mean | SD | Median | IQR | |
| Chest | 996 | 735 | 741 | 1050 | 12.80 | 4.85 | 12.37 | 9.01 | 29.3 | 13.9 | 22.7 | 18.8 |
| Lead 1 | 230 | 197 | 144 | 297 | 5.98 | 2.04 | 6.26 | 2.43 | 43.6 | 25.1 | 35.1 | 25.5 |
| Lead 2 | 212 | 198 | 145 | 225 | 6.70 | 2.48 | 6.51 | 3.04 | 46.7 | 26.7 | 41.9 | 35.0 |
| Lead 3 | 120 | 90 | 106 | 81 | 8.35 | 4.65 | 6.72 | 5.16 | 29.9 | 22.9 | 23.9 | 6.1 |
| Lead 4 | 130 | 90 | 113 | 102 | 7.79 | 4.11 | 6.50 | 5.29 | 27.9 | 20.7 | 24.8 | 23.4 |
| Lead 5 | 244 | 203 | 171 | 312 | 6.20 | 2.45 | 6.73 | 3.95 | 38.4 | 21.5 | 37.0 | 24.5 |
| Lead 6 | 218 | 233 | 117 | 134 | 7.03 | 3.01 | 6.75 | 3.38 | 43.6 | 24.1 | 33.9 | 25.9 |
| Lead # | Mean | SD | Median | IQR | ||||
|---|---|---|---|---|---|---|---|---|
| Se% | PPV% | Se% | PPV% | Se% | PPV% | Se% | PPV% | |
| Lead 1 | 86.8 | 99.3 | 15.7 | 0.8 | 93.3 | 99.6 | 15.7 | 0.6 |
| Lead 2 | 75.6 | 98.8 | 27.9 | 1.7 | 85.1 | 99.6 | 32.3 | 1.1 |
| Lead 3 | 41.5 | 96.3 | 36.5 | 4.6 | 54.1 | 98.6 | 65.7 | 6.3 |
| Lead 4 | 53.9 | 97.3 | 37.1 | 3.9 | 72.3 | 98.7 | 73.0 | 2.2 |
| Lead 5 | 86.1 | 98.5 | 15.5 | 1.9 | 92.2 | 99.3 | 11.9 | 2.4 |
| Lead 6 | 68.8 | 97.5 | 29.1 | 2.9 | 79.8 | 98.2 | 27.5 | 3.2 |
| Lead-1 | Lead-2 | Lead-3 | Lead-4 | Lead-5 | Lead-6 | |
|---|---|---|---|---|---|---|
| Pearson correlation (p) between: NVChestQRS vs. Arm leads NTPqrs | 0.88 | 0.86 | 0.30 | 0.44 | 0.83 | 0.66 |
| Scatter plot (Figure 6) trendline related Coefficient of Determination (R2) | 0.77 | 0.74 | 0.09 | 0.19 | 0.68 | 0.44 |
| Lead-1 | Lead-2 | Lead-3 | Lead-4 | Lead-5 | Lead-6 | |
|---|---|---|---|---|---|---|
| Pearson correlation (p) between: Chest RMS (HRV) vs. Arm-Lead RMS | 0.97 | 0.96 | 0.26 | 0.89 | 0.99 | 0.97 |
| Scatter plot ( Figure 9) trendline related Coefficient of Determination (R2) | 0.95 | 0.93 | 0.07 | 0.80 | 0.98 | 0.93 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Escalona, O.; Mukhtar, S.; McEneaney, D.; Finlay, D. Armband Sensors Location Assessment for Left Arm-ECG Bipolar Leads Waveform Components Discovery Tendencies around the MUAC Line. Sensors 2022, 22, 7240. https://doi.org/10.3390/s22197240
Escalona O, Mukhtar S, McEneaney D, Finlay D. Armband Sensors Location Assessment for Left Arm-ECG Bipolar Leads Waveform Components Discovery Tendencies around the MUAC Line. Sensors. 2022; 22(19):7240. https://doi.org/10.3390/s22197240
Chicago/Turabian StyleEscalona, Omar, Sephorah Mukhtar, David McEneaney, and Dewar Finlay. 2022. "Armband Sensors Location Assessment for Left Arm-ECG Bipolar Leads Waveform Components Discovery Tendencies around the MUAC Line" Sensors 22, no. 19: 7240. https://doi.org/10.3390/s22197240
APA StyleEscalona, O., Mukhtar, S., McEneaney, D., & Finlay, D. (2022). Armband Sensors Location Assessment for Left Arm-ECG Bipolar Leads Waveform Components Discovery Tendencies around the MUAC Line. Sensors, 22(19), 7240. https://doi.org/10.3390/s22197240









