Patients’ Self-Report and Handwriting Performance Features as Indicators for Suspected Mild Cognitive Impairment in Parkinson’s Disease
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Measures
2.3. Procedure
2.4. Statistical Analysis
3. Results
3.1. Participants’ Demographic and Medical Status
3.2. Comparison of PGF Ability
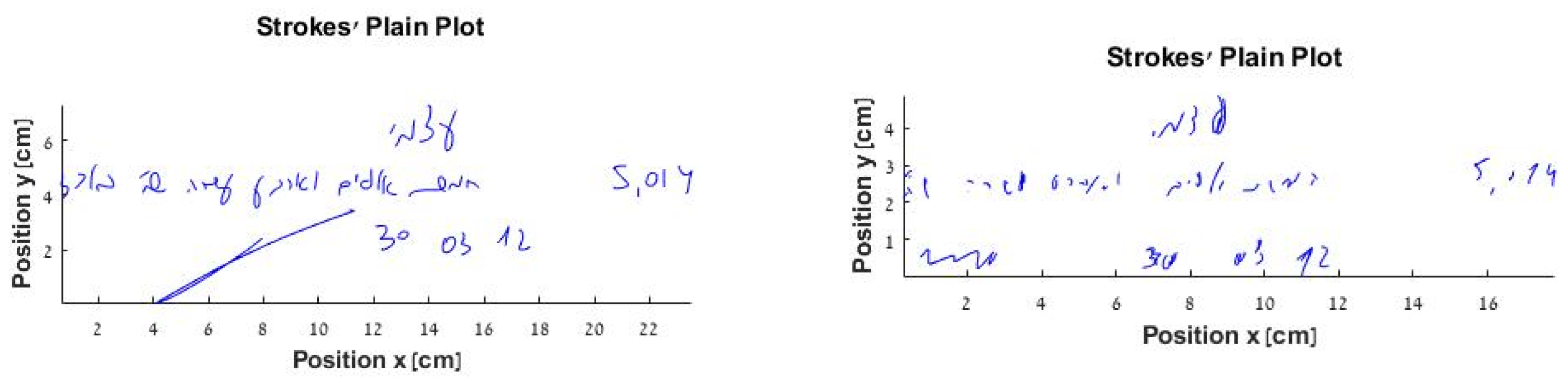
3.3. Comparison of Objective Handwriting Measure (Fill in a Check)
3.4. Correlations between Handwriting Process Measure, PGF Ability, and BDI and CF Score: All Samples
3.5. Prediction of CF Feature by Handwriting Process Measures, PGF Ability, and BDI Scores above Age
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Goldman, J.G.; Litvan, I. Mild Cognitive Impairment in Parkinson’s disease. Minerva Med. 2011, 102, 441–459. [Google Scholar] [PubMed]
- Wojtala, J.; Heber, I.A.; Neuser, P.; Heller, J.; Kalbe, E.; Rehberg, S.; Storch, A.; Linse, K.; Schneider, C.; Gräber, S.; et al. Cognitive Decline in Parkinson’s Disease: The Impact of the Motor Phenotype on Cognition. J. Neurol. Neurosurg. Psychiatry 2019, 90, 171–179. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rosenblum, S.; Meyer, S.; Gemerman, N.; Mentzer, L.; Richardson, A.; Israeli-Korn, S.; Livneh, V.; Fay Karmon, T.; Nevo, T.; Yahalom, G.; et al. The Montreal Cognitive Assessment: Is It Suitable for Identifying Mild Cognitive Impairment in Parkinson’s Disease? Mov. Disord. Clin. Pract. 2020, 7, 648–655. [Google Scholar] [CrossRef] [PubMed]
- Rosenblum, S.; Meyer, S.; Richardson, A.; Hassin-Baer, S. Capturing subjective Mild Cognitive Decline in Parkinson’s Disease. in process.
- Cammisuli, D.M.; Cammisuli, S.M.; Fusi, J.; Franzoni, F.; Pruneti, C. Parkinson’s Disease: Mild Cognitive Impairment (Pd-Mci): A Useful Summary of Update Knowledge with a Focus on Non-Pharmacological Interventions Including Physical Exercise. Front. Aging Neurosci. 2019, 11, 303. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giles, G.M.; Edwards, D.F.; Baum, C.; Furniss, J.; Skidmore, E.; Wolf, T.; Leland, N.E. Making Functional Cognition a Professional Priority. Am. J. Occup. Therap. 2020, 74, 7401090010p1–7401090010p6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wilson, R.S.; Boyle, P.A.; Segawa, E.; Yu, L.; Begeny, C.T.; Anagnos, S.E.; Bennett, D.A. The Influence of Cognitive Decline on Wellbeing in Old Age. Psychol. Aging. 2013, 28, 304–313. [Google Scholar] [CrossRef] [Green Version]
- Waldman-Levi, A.; Erez, A.B.H.; Katz, N. Healthy Aging Is Reflected in Well-Being, Participation, Playfulness, and Cognitive-Emotional Functioning. Healthy Aging Res. 2015, 4, 1–7. [Google Scholar]
- Zich, J.M.; Attkisson, C.C.; Greenfield, T.K. Screening for Depression in Primary Care Clinics: The CES-D and the BDI. Int. J. Psychiatry Med. 1990, 20, 259–277. [Google Scholar] [CrossRef]
- Harvey, P.D.; Stone, L.; Lowenstein, D.; Czaja, S.J.; Heaton, R.K.; Patterson, T.L. The Convergence between Self-Reports and Observer Ratings of Financial Skills and Direct Assessment of Financial Capabilities in Patients with Schizophrenia: More Detail Is not always Better. Schizophr. Res. 2013, 147, 86–90. [Google Scholar] [CrossRef] [Green Version]
- Harvey, P.D.; Velligan, D.I.; Bellack, A.S. Performance-Based Measures of Functional Skills: Usefulness in Clinical Treatment Studies. Schizophr. Bull. 2007, 33, 1138–1148. [Google Scholar] [CrossRef]
- Goetz, C.G.; Tilley, B.C.; Shaftman, S.R.; Stebbins, G.T.; Fahn, S.; Martinez-Martin, P.; Poewe, W.; Sampaio, C.; Stern, M.B.; Dodel, R.; et al. Movement Disorder Society-Sponsored Revision of the Unified Parkinson’s Disease Rating Scale (MDS-UPDRS): Scale Presentation and Clinimetric Testing Results. Mov. Disord. 2008, 23, 2129–2170. [Google Scholar] [CrossRef]
- Rosenblum, S.; Josman, N.; Toglia, J. Development of the Daily Living Questionnaire (DLQ): A Factor Analysis Study. Open J. Occup. Ther. 2017, 5, 1–17. [Google Scholar] [CrossRef] [Green Version]
- Rosenblum, S. Reliability and validity of the Time Organization and Participation Scale (TOPS). Neuropsychol. Rehabil. 2012, 22, 65–84. [Google Scholar] [CrossRef] [PubMed]
- Carstensen, L.L.; Mikels, J.A.; Mather, M. Aging and the Intersection of Cognition, Motivation, and Emotion. In Handbook of the Psychology of Aging; Birren, J.E., Schaie, K.W., Stamma, P., Eds.; Academic Press: Cambridge, MA, USA, 2006; pp. 343–362. [Google Scholar]
- Stievano, P.; Michetti, S.; McClintock, S.M.; Levi, G.; Scalisi, T.G. Handwriting Fluency and Visuospatial Generativity at Primary School. Read. Writ. 2016, 29, 1497–1510. [Google Scholar] [CrossRef]
- Rosenblum, S.; Samuel, M.; Zlotnik, S.; Erikh, I.; Schlesinger, I. Handwriting as an Objective Tool for Parkinson’s Disease Diagnosis. J. Neurol. 2013, 260, 2357–2361. [Google Scholar] [CrossRef]
- Teulings, H.L.; Contreras-Vidal, J.L.; Stelmach, G.E.; Adler, C.H. Adaptation of Handwriting Size under Distorted Visual Feedback in Patients with Parkinson’s Disease and Elderly and Young Controls. J. Neurol. Neurosurg. Psychiatry 2002, 72, 315–324. [Google Scholar] [CrossRef] [Green Version]
- Tucha, O.; Mecklinger, L.; Thome, J.; Reiter, A.; Alders, G.L.; Sartor, H.; Naumann, M.; Lange, K.W. Kinematic Analysis of Dopaminergic Effects on Skilled Handwriting Movements in Parkinson’s Disease. J. Neural. Transm. 2006, 113, 609–623. [Google Scholar] [CrossRef]
- Oliveira, R.M.; Gurd, J.M.; Nixon, P.; Marshall, J.C.; Passingham, R.E. Micrographia in Parkinson’s Disease: The Effect of Providing External Cues. J. Neurol. Neurosurg. Psychiatry 1997, 63, 429–433. [Google Scholar] [CrossRef] [Green Version]
- Ondo, W.G.; Satija, P. Withdrawal of Visual Feedback Improves Micrographia in Parkinson’s Disease. Mov. Disord. 2007, 22, 2130–2131. [Google Scholar] [CrossRef]
- Eichhorn, T.E.; Gasser, T.; Mai, N.; Marquardt, C.; Arnold, G.; Schwarz, J.; Oertel, W.H. Computational Analysis of Open Loop Handwriting Movements in Parkinson’s Disease: A Rapid Method to Detect Dopamimetic Effects. Mov. Disord. 1996, 11, 289–297. [Google Scholar] [CrossRef]
- Poluha, P.C.; Teulings, H.L.; Brookshire, R.H. Handwriting and Speech Changes across the Levodopa Cycle in Parkinson’s Disease. Acta. Psycho. 1998, 100, 71–84. [Google Scholar] [CrossRef]
- Rosenblum, S.; Parush, S.; Weiss, P.L. Computerized Temporal Handwriting Characteristics of Proficient and Poor Handwriters. Am. J. Occup. Ther. 2003, 57, 129–138. [Google Scholar] [CrossRef] [Green Version]
- Vessio, G. Dynamic Handwriting Analysis for Neurodegenerative Disease Assessment: A Literary Review. Appl. Sci. 2019, 9, 4666. [Google Scholar] [CrossRef] [Green Version]
- San Luciano, M.; Wang, C.; Ortega, R.A.; Yu, Q.; Boschung, S.; Soto-Valencia, J.; Bressman, S.B.; Lipton, R.B.; Pullman, S.; Saunders-Pullman, R. Digitized Spiral Drawing: A Possible Biomarker for Early Parkinson’s Disease. PLoS ONE 2016, 11, e0162799. [Google Scholar] [CrossRef] [Green Version]
- Zham, P.; Arjunan, S.; Raghav, S.; Kumar, D.K. Efficacy of Guided Spiral Drawing in the Classification of Parkinson’s Disease. IEEE J. Biomed. Health Inform. 2017, 5, 1648–1652. [Google Scholar] [CrossRef] [PubMed]
- Rosenblum, S.; Werner, P.; Dekel, T.; Gurevitz, I.; Heinik, J. Handwriting Process Variables among Elderly People with Mild Major Depressive Disorder: A Preliminary Study. Aging Clin. Exp. Res. 2010, 22, 141–147. [Google Scholar] [CrossRef] [PubMed]
- Diaz, M.; Moetesum, M.; Siddiqi, I.; Vessio, G. Sequence-Based Dynamic Handwriting Analysis for Parkinson’s Disease Detection with One-Dimensional Convolutions and BiGRUs. Expert Syst. Appl. 2021, 168, 114405. [Google Scholar] [CrossRef]
- Drotár, P.; Mekyska, J.; Rektorová, I.; Masarová, L.; Smékal, Z.; Faundez-Zanuy, M. Decision Support Framework for Parkinson’s Disease Based on Novel Handwriting Markers. IEEE Trans. Neural Syst. Rehabil. Eng. 2015, 23, 508–516. [Google Scholar] [CrossRef] [PubMed]
- Rosenblum, S. Handwriting Measures as Reflectors of Executive Functions among Adults with Developmental Coordination Disorders (DCD). Front. Psychol. 2013, 4, 357–367. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Richardson, A.; Kraus, S.; Weiss, P.L.; Rosenblum, S. COACH: Cumulative Online Algorithm for Classification of Handwriting Deficiencies. In Proceedings of the Twentieth Innovative Applications of Artificial Intelligence Conference, Chicago, IL, USA, 13–17 July 2008; pp. 1725–1730. [Google Scholar]
- Aarsland, D.; Bronnick, K.; Williams-Gray, C.; Weintraub, D.; Marder, K.; Kulisevsky, J.; Burn, D.; Barone, P.; Pagonabarraga, J.; Allcock, L.; et al. Mild Cognitive Impairment in Parkinson Disease: A Multicenter Pooled Analysis. Neurology 2010, 75, 1062–1069. [Google Scholar] [CrossRef]
- Kliegel, M.; Altgassen, M.; Hering, A.; Rose, N.S. A Process-Model Based Approach to Prospective Memory Impairment in Parkinson’s Disease. Neuropsychologia 2011, 49, 2166–2177. [Google Scholar] [CrossRef]
- Williams-Gray, C.H.; Foltynie, T.; Brayne, C.E.G.; Robbins, T.W.; Barker, R.A. Evolution of Cognitive Dysfunction in an Incident Parkinson’s Disease Cohort. Brain 2007, 30, 1787–1798. [Google Scholar] [CrossRef] [Green Version]
- Dalrymple-Alford, J.C.; MacAskill, M.R.; Nakas, C.T.; Livingston, L.; Graham, C.; Crucian, G.P.; Melzer, T.R.; Kirwan, J.; Keenan, R.; Wells, S.; et al. The MoCA Well-Suited Screen for Cognitive Impairment in Parkinson Disease. Neurology 2010, 75, 1717–1725. [Google Scholar] [CrossRef]
- Hoops, S.; Nazem, S.; Siderowf, A.D.; Duda, J.E.; Xie, S.X.; Stern, M.B.; Weintraub, D. Validity of the MoCA and MMSE in the Detection of MCI and Dementia in Parkinson Disease. Neurology 2009, 73, 1738–1745. [Google Scholar] [CrossRef]
- Nasreddine, Z.S.; Phillips, N.A.; Bédirian, V.; Charbonneau, S.; Whitehead, V.; Collin, I.; Cummings, J.L.; Chertkow, H. The Montreal Cognitive Assessment, MoCA: A Brief Screening Tool for Mild Cognitive Impairment. J. Am. Geriatr. Soc. 2005, 53, 695–699. [Google Scholar] [CrossRef]
- Postuma, R.B.; Berg, D.; Stern, M.; Poewe, W.; Olanow, C.W.; Oertel, W.; Obeso, J.; Marek, K.; Litvan, I.; Lang, A.E.; et al. MDS Clinical Diagnostic Criteria for Parkinson’s Disease. Mov. Disord. 2015, 30, 1591–1601. [Google Scholar] [CrossRef]
- Hoehn, M.M.; Yahr, M.D. Parkinsonism: Onset, Progression and Mortality. Neurology 1967, 17, 427–442. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Toglia, J.; Foster, E. The Multicontext Approach: A Metacognitive Strategy Based Intervention to Optimize Functional Cognition; Gatekeeper Press: Grove City, OH, USA, 2022; in press. [Google Scholar]
- Tomlinson, C.L.; Stowe, R.; Patel, S.; Rick, C.; Gray, R.; Clarke, C.E. Systematic Review of Levodopa dose Equivalency Reporting in Parkinson’s Disease. Mov. Disord. 2010, 25, 2649–2653. [Google Scholar] [CrossRef] [PubMed]
- Heinik, J.; Wenre, P.; Dekel, T.; Gurevitz, I.; Rosenblum, S. Computerized Kinematic Analysis of the Clock Drawing Task in Elderly People with Mild Major Depressive-Disorder: An Exploratory Study. Int. Psychogeriatr. 2010, 22, 479–488. [Google Scholar] [CrossRef] [PubMed]
- Werner, P.; Rosenblum, S.; Bar-On, G.; Heinik, J.; Korczyn, A. Handwriting Process Variables Discriminating Mild Alzheimer’s Disease and Mild Cognitive Impairment. J. Gerontol. B Psychol. Sci. Soc. Sci. 2006, 61B, 228–236. [Google Scholar] [CrossRef] [PubMed]
- Al-Saffar, A.; Awang, S.; Al-Saiagh, W.; Al-Khaleefa, A.S.; Abed, S.A. A Sequential Handwriting Recognition Model Based on a Dynamically Configurable CRNN. Sensors 2021, 21, 7306. [Google Scholar] [CrossRef] [PubMed]
- Devillaine, L.; Lambert, R.; Boutet, J.; Aloui, S.; Brault, V.; Jolly, C.; Labyt, E. Analysis of Graphomotor Tests with Machine Learning Algorithms for an Early and Universal Pre-Diagnosis of Dysgraphia. Sensors 2021, 21, 7026. [Google Scholar] [CrossRef]
- Júnior, E.P.; Delmiro, I.L.D.; Magaia, N.; Maia, F.M.; Hassan, M.M.; Albuquerque, V.H.; Fortino, G. Intelligent Sensory Pen for Aiding in the Diagnosis of Parkinson’s Disease from Dynamic Handwriting Analysis. Sensors 2020, 20, 5840. [Google Scholar] [CrossRef] [PubMed]
- Kalbe, E.; Folkerts, A.-K.; Ophey, A.; Eggers, C.; Elben, S.; Dimenshteyn, K.; Sulzer, P.; Schulte, C.; Schmidt, N.; Schlenstedt, C.; et al. Enhancement of Executive Functions but Not Memory by Multidomain Group Cognitive Training in Patients with Parkinson’s Disease and Mild Cognitive Impairment: A Multicenter Randomized Controlled Trial. Parkinsons Dis. 2020, 2020, 4068706. [Google Scholar] [CrossRef] [PubMed]
- Lau, K.M.; Parikh, M.; Harvey, D.J.; Huang, C.J.; Farias, S.T. Early Cognitively Based Functional Limitations Predict Loss of Independence in Instrumental Activities of Daily Living in Older Adults. J. Int. Neuropsychol. Soc. 2015, 21, 688–698. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feenstra, H.E.; Vermeulen, I.E.; Murre, J.M.; Schagen, S.B. Online Self-Administered Cognitive Testing Using the Amsterdam Cognition Scan: Establishing Psychometric Properties and Normative Data. J. Med. Internet Res. 2018, 20, e9298. [Google Scholar] [CrossRef] [Green Version]
- Sciuto, G.L.; Russo, S.; Napoli, C. A Cloud-Based Flexible Solution for Psychometric Tests Validation, Administration and Evaluation. Proc. SYSTEM 2019, 2468, 16–21. [Google Scholar]
| Variable | M (SD) | |||
|---|---|---|---|---|
| s.PD-MCI (n = 25) | PD-n.MCI (n = 53) | t(76) | p | |
| 1. General thinking | 2.32 (0.99) | 2.21 (0.85) | 0.40 | 0.620 |
| 2. General functioning | 3.12 (1.05) | 2.63 (0.95) | 2.02 | 0.046 |
| 3. Role change: housekeeping | 3.20 (1.15) | 2.13 (1.13) | 3.83 | <0.001 |
| 4. Role change: community or work | 3.08 (1.17) | 2.10 (1.24) | 3.27 | 0.002 |
| 5. Satisfaction: doing things you need to do | 2.80 (1.12) | 2.06 (0.89) | 3.14 | 0.002 |
| 6. Satisfaction: doing things you want to do | 3.20 (1.19) | 2.10 (0.89) | 4.11 | <0.001 |
| 7. Change in your life due to the illness | 3.64 (0.86) | 2.62 (0.91) | 4.70 | <0.001 |
| Final mean score | 3.04 (0.78) | 2.26 (0.75) | 4.23 | <0.001 |
| Variable | M (SD) | |||
|---|---|---|---|---|
| s.PD-MCI (n = 25) | PD-n.MCI (n = 53) | t(76) | p | |
| Performance time | 44.130 (13.870) | 44.920 (14.000) | −0.226 | 0.822 |
| Mean pen-stroke width | 0.164 (0.050) | 0.054 (0.013) | −3.190 | 0.002 |
| Mean pen-stroke height | 0.285 (0.077) | 0.307 (0.066) | −1.250 | 0.214 |
| CF Feature | SWGM | BDI | PGF | |
|---|---|---|---|---|
| CF feature | −0.428 ** | 0.382 ** | 0.530 ** | |
| SWGM | −0.428 ** | −0.115 | −0.173 | |
| BDI | 0.382 ** | −0.115 | 0.502 ** | |
| PGF | 0.530 ** | −0.173 | 0.502 ** |
| Variable | Model 1 | Model 2 | Model 3 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| B | SE B | β | B | SE B | β | B | SE B | β | |
| Age | −0.024 | 0.007 | −0.368 *** | −0.015 | 0.007 | −0.229 * | −0.010 | 0.006 | −0.157 |
| PGF | 0.292 | 0.063 | 0.473 *** | 0.271 | 0.059 | 0.439 *** | |||
| SWGM | −0.230 | 0.690 | −0.315 *** | ||||||
| R2 | 0.13 | 0.33 | 0.43 | ||||||
| F | 11.080 *** | 17.95 *** | 17.41 *** | ||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rosenblum, S.; Meyer, S.; Richardson, A.; Hassin-Baer, S. Patients’ Self-Report and Handwriting Performance Features as Indicators for Suspected Mild Cognitive Impairment in Parkinson’s Disease. Sensors 2022, 22, 569. https://doi.org/10.3390/s22020569
Rosenblum S, Meyer S, Richardson A, Hassin-Baer S. Patients’ Self-Report and Handwriting Performance Features as Indicators for Suspected Mild Cognitive Impairment in Parkinson’s Disease. Sensors. 2022; 22(2):569. https://doi.org/10.3390/s22020569
Chicago/Turabian StyleRosenblum, Sara, Sonya Meyer, Ariella Richardson, and Sharon Hassin-Baer. 2022. "Patients’ Self-Report and Handwriting Performance Features as Indicators for Suspected Mild Cognitive Impairment in Parkinson’s Disease" Sensors 22, no. 2: 569. https://doi.org/10.3390/s22020569







