Walk-IT: An Open-Source Modular Low-Cost Smart Rollator
Abstract
:1. Introduction
2. Gait Assessment Using a Smart Rollator
- Cadence (CAD): .
- Step time (SpT).
- Step length (SpL) m.
- Stride time (SdT).
- Stride length (Stance phase, SdL): m.
- Walking velocity (WV): .
- Weight-bearing (WB): .
- Step time (SpT): Average time between maximum–minimum (right) or minimum–maximum (left) in seconds.
- Stride time (SdT): Average time between maximum–maximum (right) and minimum–minimum (left) in seconds.
- Number of Step (NoS): Numbers of inflection points.
- Cadence (CAD): .
- Step length (SpL): Average length between maximum–minimum (right) or minimum–maximum (left) in seconds.
- Stride length (SdL): Average length between maximum–maximum (right) and minimum–minimum (left) in seconds.
- Distance(d): Distance walked by user in meters.
- Average walking velocity (WV): .
3. System Architecture
3.1. Hardware Modules
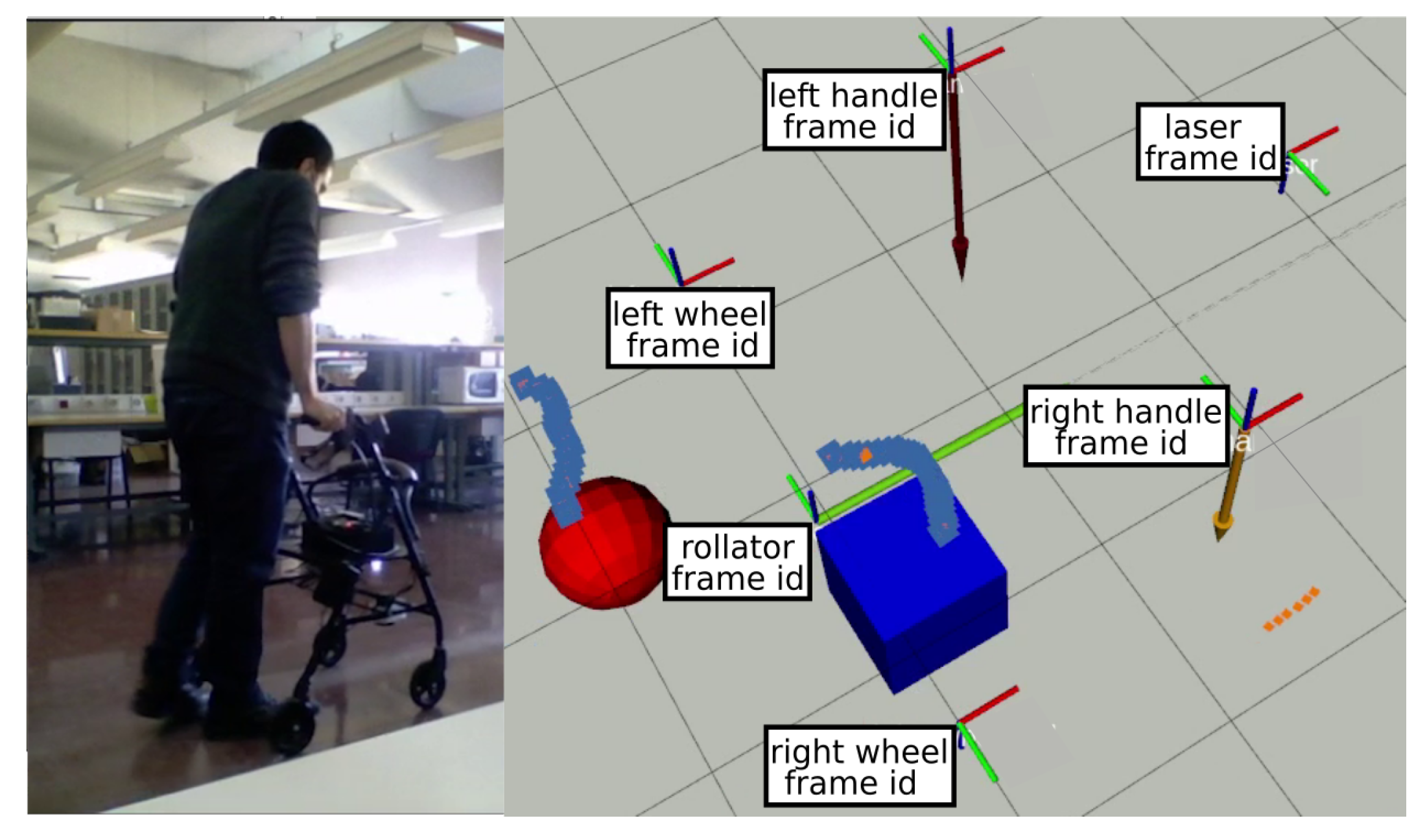
- Load sensors on the handlebars. Specifically, strain gauges are used in a Wheatstone bridge configuration to measure exerted support on each handle during the gait cycle. Gauges are adhered to the bars (Figure 3) and connected to an Arduino Nano using an HX711 24 bits Analog-to-Digital converter, specific for industrial control applications to interface directly with a bridge sensor such as the gauges. Figure 4 shows how load data is displayed under ROS2 with vertical arrows proportional to the applied force on their respective sensor.The Arduino board processes raw readings and makes them available through a serial-USB connection with a 2.5 Hz rate and a resolution of 5.5 gr. The whole circuit is protected with an adapted 3D-printed box attached to the bars. No modification of bar properties is performed, weight modification in the structure is minimal and symmetrical, and wiring is added to the brakes’ wiring harness. A basic Walk-IT includes one of these modules on each handlebar, to measure weight supported on each side of the rollator.
- Encoders on the wheels. User speed and step length are also required for gait analysis. Instead of modifying wheels in any way, encoders are attached to the rear wheels of the rollator, as shown in Figure 5. These encoders are built using an AS5601 magnetic rotary position sensor, protected with a plastic box and connected to an Arduino nano board via USB port. Encoders provide data at 600 Hz with an angular resolution of 0.1 mm per encoder tick. Again, no structure modification nor significant weight increase is required. The plastic box is positioned behind the frame to avoid interfering with patient’s movements while walking. Figure 4 presents odometry data as a green arrow displayed at the motion center. A basic Walk-IT includes one of these modules on each rear wheel, to provide right and left odometry.
- Light detection and ranging sensor. A Light Detection and Ranging (LiDaR) has been attached under the lower-front transversal pole. This sensor has a twofold purpose: (i) to detect feet movement and gait phases, and (ii) to detect nearby obstacles and help with robot localization. In this work, an RPLidar A1M8 LiDaR from SLAMTEC was chosen. A1M8 is a low-cost LiDaR with 360 degrees field of view, 6-meter range, and an average scan rate of 5.5 Hz. Although it is required for leg support estimation, it is not strictly necessary for the basic configuration of Walk-IT.
3.2. Software Modules
4. Tests and Results
4.1. Leg Speed Analysis
4.2. Partial Weight-Bearing
4.3. Spatiotemporal Gait Parameters Analysis
5. Discussion
6. Conclusions
- A system designed for easy replicability. Walk-IT relies on open software and off-the-shelf commercial components that can be easily replaced by similar ones, and it can be mounted on any standard rollator frame. In addition, hardware modules have been designed to be added to the base structure, so its original properties are not affected.
- A fully modular system. Walk-IT modules can be deployed/replaced on a need basis depending on the target application. In the present work, the Walk-IT basic configuration has been adapted for partial weight-bearing assessment, i.e., to measure how much weight a given user loads on each leg. Dynamic weight distribution is a very important parameter in clinical rehabilitation.
- An spatiotemporal analysis tool. Spatiotemporal gait parameters are reportedly linked to condition, so a spatiotemporal gait parameter capture algorithm based on leg detection has been implemented by including an additional node in the proposed ROS2 architecture.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tinetti, M.E. Performance-Oriented Assessment of Mobility Problems in Elderly Patients. J. Am. Geriatr. Soc. 1986, 34, 119–126. [Google Scholar] [CrossRef] [PubMed]
- Zeni, J.; Richards, J.; Higginson, J. Two simple methods for determining gait events during treadmill and overground walking using kinematic data. Gait Posture 2008, 27, 710–714. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Webster, K.; Wittwer, J.; Feller, J. Validity of the GAITRite (R) walkway system for the measurement of averaged and individual step parameters of gait. Gait Posture 2006, 22, 317–321. [Google Scholar] [CrossRef]
- Gomatam, A.N.M.; Sasi, S. Multimodal Gait Recognition Based on Stereo Vision and 3D Template Matching. In Proceedings of the International Conference on Imaging Science, Systems and Technology, CISST’04, Las Vegas, NV, USA, 21–24 June 2004; pp. 405–410. [Google Scholar]
- Mostayed, A.; Mynuddin, M.; Mazumder, G.; Kim, S.; Park, S.J. Abnormal Gait Detection Using Discrete Fourier Transform. In Proceedings of the 2008 International Conference on Multimedia and Ubiquitous Engineering (MUE 2008), Busan, Korea, 24–26 April 2008; pp. 36–40. [Google Scholar]
- Xue, Z.; Ming, D.; Song, W.; Wan, B.; Jin, S. Infrared Gait Recognition Based on Wavelet Transform and Support Vector Machine. Pattern Recogn. 2010, 43, 2904–2910. [Google Scholar] [CrossRef]
- Derawi, M.O.; Ali, H.; Cheikh, F.A. Gait recognition using time-of-flight sensor. In Proceedings of the BIOSIG 2011—Biometrics Special Interest Group, Darmstadt, Germany, 8–9 September 2011; Brömme, A., Busch, C., Eds.; Gesellschaft für Informatik e.V.: Bonn, Germany, 2011; pp. 187–194. [Google Scholar]
- Gabel, M.; Gilad-Bachrach, R.; Renshaw, E.; Schuster, A. Full body gait analysis with Kinect. In Proceedings of the 2012 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, San Diego, CA, USA, 28 August–1 September 2012; pp. 1964–1967. [Google Scholar]
- Bae, J.; Tomizuka, M. A tele-monitoring system for gait rehabilitation with an inertial measurement unit and a shoe-type ground reaction force sensor. Mechatronics 2013, 23, 646–651. [Google Scholar] [CrossRef]
- Ferrari, A.; Rocchi, L.; van den Noort, J.; Harlaar, J. Toward the Use of Wearable Inertial Sensors to Train Gait in Subjects with Movement Disorders. In Converging Clinical and Engineering Research on Neurorehabilitation; Number 1 in Biosystems & Biorobotics; Springer: Berlin/Heidelberg, Germany, 2013; pp. 937–940. [Google Scholar]
- Bruijn, S.; Kate, W.; Faber, G.; Meijer, O.; Beek, P.; Van Dieen, J. Estimating Dynamic Gait Stability Using Data from Non-aligned Inertial Sensors. Ann. Biomed. Eng. 2010, 38, 2588–2593. [Google Scholar] [CrossRef] [Green Version]
- Alves, J.; Seabra, E.; Caetano, I.; Santos, C.P. Overview of the ASBGo++ Smart Walker. In Proceedings of the 2017 IEEE 5th Portuguese Meeting on Bioengineering (ENBENG), Coimbra, Portugal, 16–18 February 2017; pp. 1–4. [Google Scholar]
- Ballesteros, J.; Urdiales, C.; Martinez, A.B.; Tirado, M. Automatic Assessment of a Rollator-User’s Condition During Rehabilitation Using the i-Walker Platform. IEEE Trans. Neural Syst. Rehabil. Eng. 2017, 25, 2009–2017. [Google Scholar] [CrossRef]
- Chalvatzaki, G.; Koutras, P.; Hadfield, J.; Papageorgiou, X.S.; Tzafestas, C.S.; Maragos, P. LSTM-based Network for Human Gait Stability Prediction in an Intelligent Robotic Rollator. In Proceedings of the 2019 International Conference on Robotics and Automation (ICRA), Montreal, QC, Canada, 20–24 May 2019; pp. 4225–4232. [Google Scholar]
- Watanabe, S.; Tsumugiwa, T.; Yokogawa, R. Gait Analysis of Walking Locomotion Enhanced by an Impedance-Controlled Gait-Aid Walker-Type Robot. In Proceedings of the 2020 IEEE/SICE International Symposium on System Integration (SII), Honolulu, HI, USA, 12–15 January 2020; pp. 1187–1192. [Google Scholar]
- Costamagna, E.; Thies, S.B.; Kenney, L.P.J.; Howard, D.; Lindemann, U.; Klenk, J.; Baker, R. Objective measures of rollator user stability and device loading during different walking scenarios. PLoS ONE 2019, 14, e0210960. [Google Scholar] [CrossRef]
- Wentink, E.; Schut, V.; Prinsen, E.; Rietman, J.; Veltink, P. Detection of the onset of gait initiation using kinematic sensors and EMG in transfemoral amputees. Gait Posture 2014, 39, 391–396. [Google Scholar] [CrossRef]
- Joly, C.; Dune, C.; Gorce, P.; Rives, P. Feet and legs tracking using a smart rollator equipped with a Kinect. Workshop on Assistance and Service Robotics in a Human Environment. In Proceedings of the Conjonction with IEEE/RSJ International Conference on Intelligent Robots and Systems (IROS), Tokyo, Japan, 7 November 2013. [Google Scholar]
- Abellanas, A.; Neto, A.F.; Ruiz, R.C.; Raya, R.; Estévez, L.C. Ultrasonic time of flight estimation in assistive mobility: Improvement of the model-echo fitting. In Proceedings of the Eurosensors XXII, Dresden, Germany, 7–10 September 2008; pp. 464–467. [Google Scholar]
- Alwan, M.; Ledoux, A.; Wasson, G.; Sheth, P.; Huang, C. Basic walker-assisted gait characteristics derived from forces and moments exerted on the walker’s handles: Results on normal subjects. Med. Eng. Phys. 2007, 29, 380–389. [Google Scholar] [CrossRef]
- Ballesteros, J.; Urdiales, C.; Martinez, A.B.; Tirado, M. Gait analysis for challenged users based on a rollator equipped with force sensors. In Proceedings of the 2015 IEEE/RSJ International Conference on Intelligent Robots and Systems (IROS), Hamburg, Germany, 28 September–2 October 2015; pp. 5587–5592. [Google Scholar]
- Davenport, R.D. Robotics. In Smart Technology for Aging, Disability, and Independence; Wiley–Interscience, Ltd.: New York, NY, USA, 2005; Chapter 3; pp. 67–109. [Google Scholar]
- Fernandez-Carmona, M.; Ballesteros, J.; Urdiales, C. Walk-IT Repository. Available online: https://github.com/TaISLab/WalKit/tree/foxy (accessed on 24 February 2022).
- Hustedt, J.W.; Blizzard, D.J.; Baumgaertner, M.R.; Leslie, M.P.; Grauer, J.N. Effect of age on partial weight-bearing training. Orthopedics 2012, 35, e1061–e1067. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ganse, B.; Yang, P.F.; Gardlo, J.; Gauger, P.; Kriechbaumer, A.; Pape, H.C.; Koy, T.; Müller, L.P.; Rittweger, J. Partial weight bearing of the tibia. Injury 2016, 47, 1777–1782. [Google Scholar] [CrossRef] [PubMed]
- Dabke, H.; Gupta, S.; Holt, C.A.; O’Callaghan, P.; Dent, C. How accurate is partial weightbearing? Clin. Orthop. Relat. Res. 2004, 421, 282–286. [Google Scholar] [CrossRef] [PubMed]
- Price, C.; Schmeltzpfenning, T.; Nester, C.J.; Brauner, T. Chapter 3—Foot and footwear biomechanics and gait. In Handbook of Footwear Design and Manufacture, 2nd ed.; Luximon, A., Ed.; The Textile Institute Book Series; Woodhead Publishing: Cambridge, UK, 2021; pp. 79–103. [Google Scholar]
- Snijders, A.H.; Van De Warrenburg, B.P.; Giladi, N.; Bloem, B.R. Neurological gait disorders in elderly people: Clinical approach and classification. Lancet Neurol. 2007, 6, 63–74. [Google Scholar] [CrossRef]
- Andersson, L.; Wesslau, A.; Bodén, H.; Dalén, N. Immediate or late weight bearing after uncemented total hip arthroplasty: A study of functional recovery. J. Arthroplast. 2001, 16, 1063–1065. [Google Scholar] [CrossRef]
- Hollman, J.H.; McDade, E.M.; Petersen, R.C. Normative spatiotemporal gait parameters in older adults. Gait Posture 2011, 34, 111–118. [Google Scholar] [CrossRef] [Green Version]
- Balaban, B.; Tok, F. Gait disturbances in patients with stroke. PM&R 2014, 6, 635–642. [Google Scholar]
- Ebersbach, G.; Sojer, M.; Valldeoriola, F.; Wissel, J.; Müller, J.; Tolosa, E.A.; Poewe, W. Comparative analysis of gait in Parkinson’s disease, cerebellar ataxia and subcortical arteriosclerotic encephalopathy. Brain 1999, 122, 1349–1355. [Google Scholar] [CrossRef] [Green Version]
- Jahn, K.; Zwergal, A.; Schniepp, R. Gait disturbances in old age: Classification, diagnosis, and treatment from a neurological perspective. Dtsch. Ärzteblatt Int. 2010, 107, 306–316. [Google Scholar]
- Lang, J.; Ishikawa, K.; Hatakeyama, K.; Wong, W.H.; Yin, M.; Saito, T.; Sibata, Y. 3D body segment oscillation and gait analysis for vestibular disorders. Auris Nasus Larynx 2013, 40, 18–24. [Google Scholar] [CrossRef]
- Woolley, S.M. Characteristics of gait in hemiplegia. Top. Stroke Rehabil. 2001, 7, 1–18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Annicchiarico, R.; Barrué, C.; Benedico, T.; Campana, F.; Cortés, U.; Martínez-Velasco, A. The I-Walker: An Intelligent Pedestrian Mobility Aid. In Proceedings of the 2008 Conference on ECAI 2008: 18th European Conference on Artificial Intelligence, Patras, Greece, 21–25 July 2008; IOS Press: Amsterdam, The Netherlands, 2008; pp. 708–712. [Google Scholar]
- Ballesteros, J.; Urdiales, C.; Martinez, A.B.; Van Dieën, J.H. On Gait Analysis Estimation Errors Using Force Sensors on a Smart Rollator. Sensors 2016, 16, 1896. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- KMINA. KMINA Rollator Comfort. Available online: https://kmina.com/en/black-rollator-cable-brake/ (accessed on 24 February 2022).
- Thomas, D.; Woodall, W.; Fernandez, E. Next-Generation ROS: Building on DDS; ROSCon Chicago 2014; Open Robotics: Mountain View, CA, USA, 2014. [Google Scholar]
- Maruyama, Y.; Kato, S.; Azumi, T. Exploring the performance of ROS2. In Proceedings of the 13th ACM SIGBED International Conference on Embedded Software (EMSOFT), Pittsburgh, PN, USA, 1–7 October 2016; pp. 1–10. [Google Scholar]











| Age | Weight | Height | Preexisting Conditions | Gender | Experience Using Rollators | |
|---|---|---|---|---|---|---|
| User 1 | 42 | 94 | 1.74 | None | Male | No |
| User 2 | 38 | 110 | 1.84 | Right leg polytraumatism | Male | Yes |
| User 3 | 39 | 112 | 1.75 | None | Female | No |
| User 4 | 70 | 79 | 1.80 | None | Male | No |
| User 5 | 69 | 58 | 1.65 | None | Female | No |
| User 6 | 75 | 56 | 1.63 | Rheumatoid arthritis | Female | No |
| User 7 | 90 | 51 | 1.55 | Osteoarthritis | Female | Yes |
| User 8 | 39 | 74 | 1.80 | None | Male | No |
| User 9 | 31 | 60 | 1.80 | None | Male | No |
| User 10 | 42 | 83 | 1.75 | None | Male | No |
| User 11 | 35 | 54 | 1.69 | Arthritis | Female | Yes |
| User | CAD | SdT | SdL | rSpT | lSpT | rSpL | lSpL | WV | UrS |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 58.41 | 1.05 (0.14) | 0.55 (0.03) | 0.75 (0.18) | 0.83 (0.26) | 0.28 (0.01) | 0.27 (0.02) | 0.53 | 22.68 |
| 2 | 99.01 | 0.61 (0.01) | 0.35 (0.01) | 0.48 (0.02) | 0.43 (0.01) | 0.18 (0.00) | 0.17 (0.00) | 0.57 | 35.17 |
| 3 | 106.62 | 1.17 (0.19) | 1.01 (0.21) | 0.58 (0.19) | 0.59 (0.07) | 0.51 (0.21) | 0.51 (0.11) | 0.86 | <1 |
| 4 | 80.91 | 0.75 (0.20) | 0.47 (0.09) | 0.53 (0.17) | 0.61 (0.31) | 0.19 (0.02) | 0.27 (0.05) | 0.62 | 24.49 |
| 5 | 89.36 | 0.67 (0.13) | 0.38 (0.05) | 0.55 (0.19) | 0.46 (0.18) | 0.22 (0.02) | 0.16 (0.01) | 0.56 | 8.37 |
| 6 | 95.17 | 0.64 (0.19) | 0.83 (0.25) | 0.52 (0.42) | 0.44 (0.13) | 0.46 (0.14) | 0.37 (0.08) | 0.72 | 5.83 |
| 7 | 89.67 | 0.68 (0.26) | 0.45 (0.08) | 0.53 (0.31) | 0.48 (0.27) | 0.27 (0.04) | 0.19 (0.03) | 0.66 | 6.56 |
| 8 | 119.42 | 0.51 (0.03) | 0.85 (0.19) | 0.39 (0.08) | 0.38 (0.03) | 0.44 (0.11) | 0.4 (0.08) | 0.96 | 11.56 |
| 9 | 106.15 | 0.57 (0.02) | 0.71 (0.04) | 0.44 (0.04) | 0.42 (0.02) | 0.39 (0.02) | 0.32 (0.02) | 0.91 | 17.05 |
| 10 | 96.91 | 0.62 (0.03) | 0.78 (0.05) | 0.46 (0.04) | 0.46 (0.05) | 0.40 (0.03) | 0.37 (0.02) | 0.75 | 23.01 |
| 11 | 85.94 | 0.71 (0.20) | 0.56 (0.07) | 0.47 (0.11) | 0.61 (0.35) | 0.23 (0.02) | 0.34 (0.04) | 0.79 | 12.66 |
| Av. | 93.41 | 0.72 | 0.63 | 0.51 | 0.52 | 0.32 | 0.31 | 0.72 | 15.21 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fernandez-Carmona, M.; Ballesteros, J.; Díaz-Boladeras, M.; Parra-Llanas, X.; Urdiales, C.; Gómez-de-Gabriel, J.M. Walk-IT: An Open-Source Modular Low-Cost Smart Rollator. Sensors 2022, 22, 2086. https://doi.org/10.3390/s22062086
Fernandez-Carmona M, Ballesteros J, Díaz-Boladeras M, Parra-Llanas X, Urdiales C, Gómez-de-Gabriel JM. Walk-IT: An Open-Source Modular Low-Cost Smart Rollator. Sensors. 2022; 22(6):2086. https://doi.org/10.3390/s22062086
Chicago/Turabian StyleFernandez-Carmona, Manuel, Joaquin Ballesteros, Marta Díaz-Boladeras, Xavier Parra-Llanas, Cristina Urdiales, and Jesús Manuel Gómez-de-Gabriel. 2022. "Walk-IT: An Open-Source Modular Low-Cost Smart Rollator" Sensors 22, no. 6: 2086. https://doi.org/10.3390/s22062086
APA StyleFernandez-Carmona, M., Ballesteros, J., Díaz-Boladeras, M., Parra-Llanas, X., Urdiales, C., & Gómez-de-Gabriel, J. M. (2022). Walk-IT: An Open-Source Modular Low-Cost Smart Rollator. Sensors, 22(6), 2086. https://doi.org/10.3390/s22062086








