A Pilot Study Comparing the Effects of Concurrent and Terminal Visual Feedback on Standing Balance in Older Adults
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
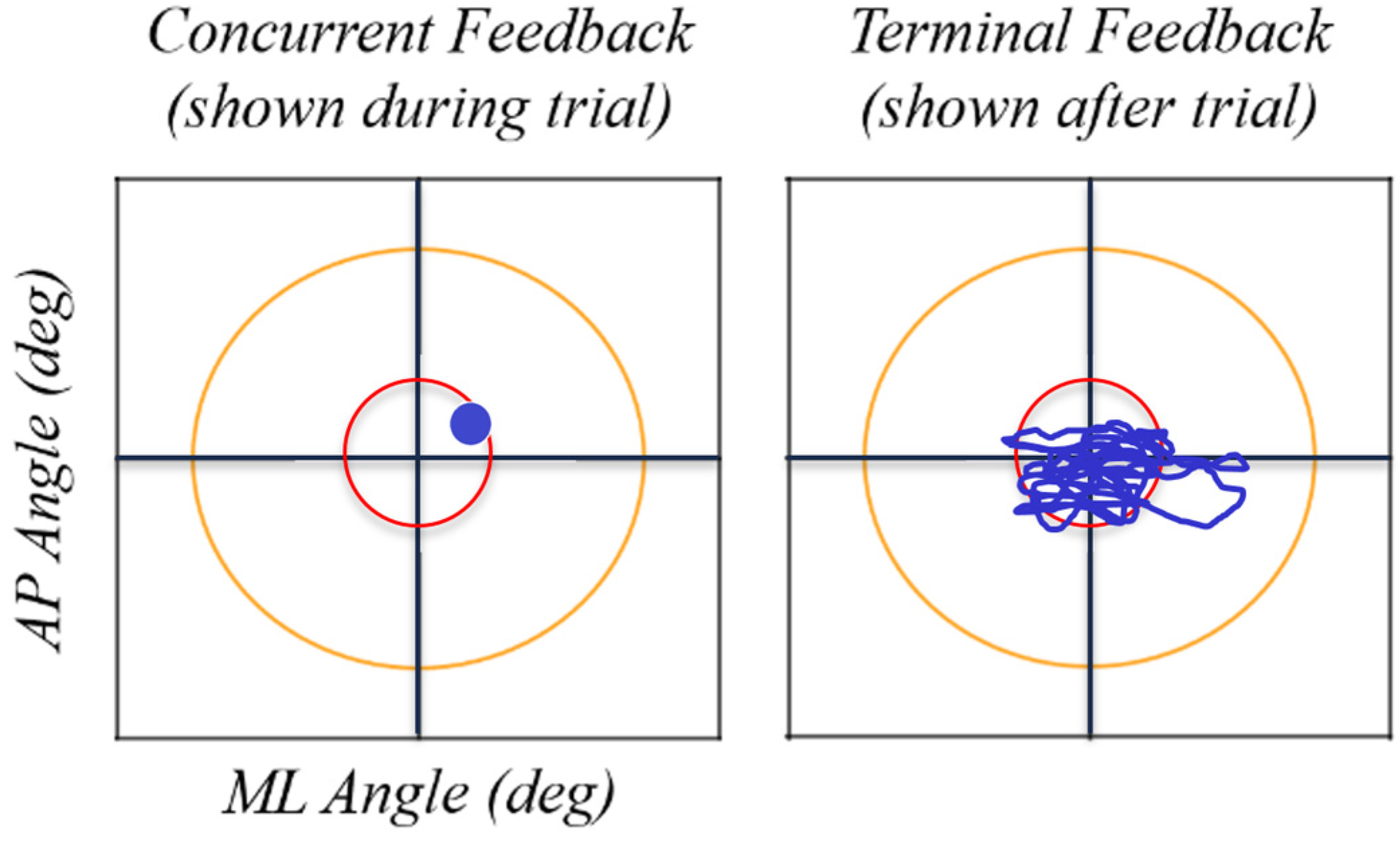
2.2. Protocol
2.3. Data Analysis
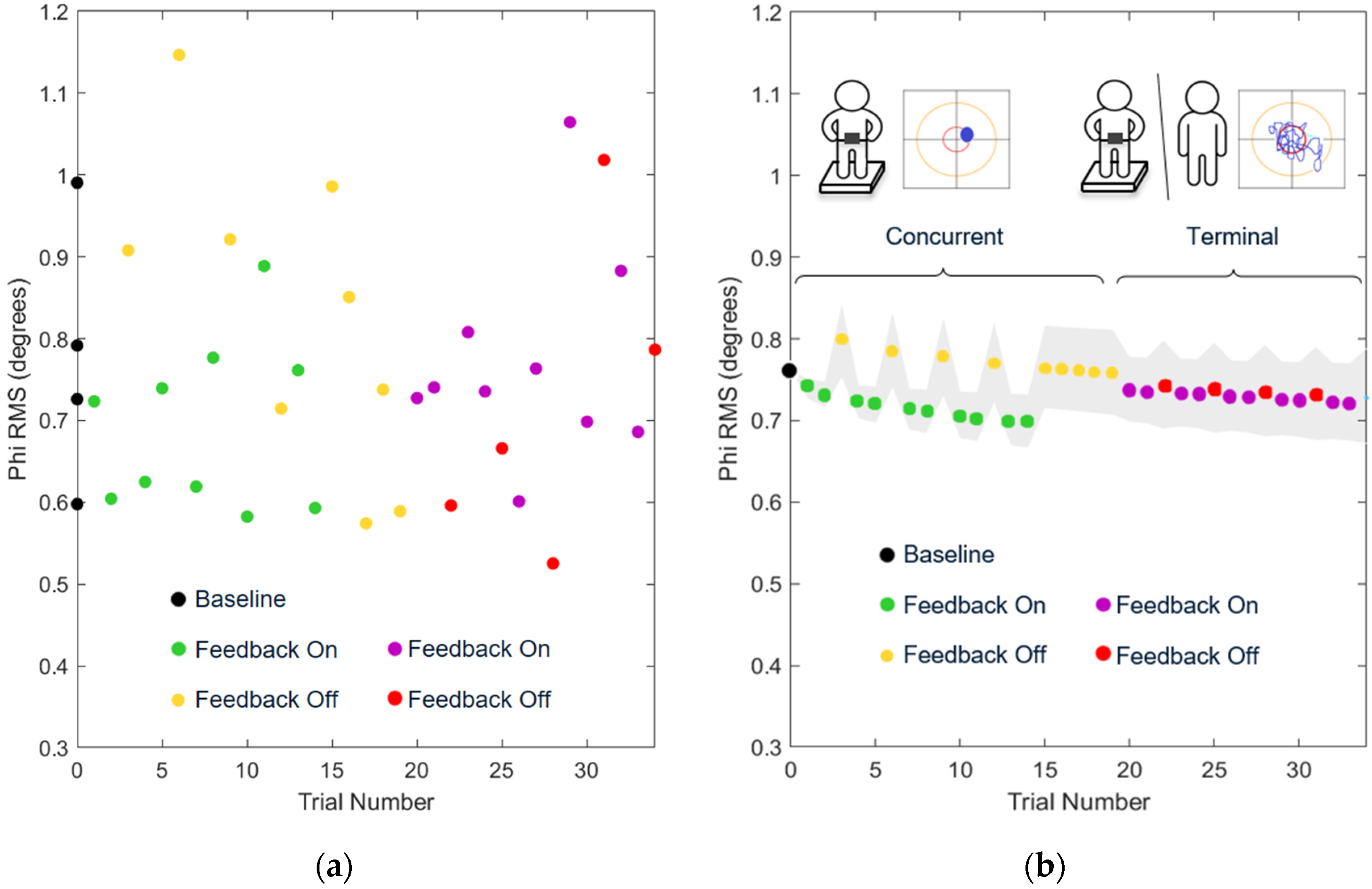
3. Results
4. Discussion
4.1. Effects of Balance Training with Feedback While Feedback Was Used
4.2. Effects of Balance Training with Feedback after Feedback Was Removed
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Falls. Available online: https://www.who.int/en/news-room/fact-sheets/detail/falls (accessed on 20 May 2021).
- Hull, S.L.; Kneebone, I.I.; Farquharson, L. Anxiety, depression, and fall-related psychological concerns in community-dwelling older people. Am. J. Geriatr. Psychiatry 2013, 21, 1287–1291. [Google Scholar] [CrossRef] [PubMed]
- Hughes, C.C.; Kneebone, I.I.; Jones, F.; Brady, B. A theoretical and empirical review of psychological factors associated with falls-related psychological concerns in community-dwelling older people. Int. Psychogeriatr. 2015, 27, 1071–1087. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Denkinger, M.D.; Lukas, A.; Nikolaus, T.; Hauer, K. Factors associated with fear of falling and associated activity restriction in community-dwelling older adults: A systematic review. Am. J. Geriatr. Psychiatry 2015, 23, 72–86. [Google Scholar] [CrossRef] [PubMed]
- Cumming, R.G.; Salkeld, G.; Thomas, M.; Szonyi, G. Prospective study of the impact of fear and falling on activities of daily living, SF-36 scores, and nursing home admission. J. Gerontol. 2000, 55, M299–M305. [Google Scholar] [CrossRef]
- Zijlstra, G.A.R.; Van Haastregt, J.C.M.; Van Eijk, J.T.M.; van Rossum, E.; Stalenhoef, P.A.; Kempen, G.I. Prevalence and correlates of fear of falling, and associated avoidance of activity in the general population of community-living older people. Age Ageing 2007, 36, 304–309. [Google Scholar] [CrossRef] [Green Version]
- Arfken, C.L.; Lach, H.W.; Birge, S.J.; Miller, J.P. The prevalence and correlates of fear of falling in elderly persons living in the community. Am. J. Public Health 1994, 84, 565–570. [Google Scholar] [CrossRef] [Green Version]
- Howland, J.; Peterson, E.W.; Levin, W.C.; Fried, L.; Pordon, D.; Bak, S. Fear of falling among the community-dwelling elderly. J. Aging Health 1993, 5, 229–243. [Google Scholar] [CrossRef]
- Lesinski, M.; Hortobagyi, T.; Muehlbauer, T.; Gollhofer, A.; Granacher, U. Effects of balance training on balance performance in healthy older adults: A systematic review and meta-analysis. Sports Med. 2015, 45, 1721–1738. [Google Scholar] [CrossRef] [Green Version]
- Gordt, K.; Gerhardy, T.; Najafi, B.; Schwenk, M. Effects of wearable sensor-based balance and gait training on balance, gait, and functional performance in healthy and patient populations: A systematic review and meta-analysis of randomized controlled trials. Gerontology 2018, 64, 74–89. [Google Scholar] [CrossRef]
- Kummel, J.; Kramer, A.; Giboin, L.S.; Gruber, M. Specificity of balance training in healthy individuals: A systematic review and meta-analysis. Sports Med. 2016, 46, 1261–1271. [Google Scholar] [CrossRef]
- Zimbelman, J.L.; Juraschek, S.P.; Zhang, X.; Lin, V.W.H. Physical therapy workforce in the United States: Forecasting nationwide shortages. Am. Acad. Phys. Med. Rehabil. 2010, 2, 1021–1029. [Google Scholar] [CrossRef] [PubMed]
- Landry, M.D.; Hack, L.M.; Coulson, E.; Freburger, J.; Johnson, M.P.; Katz, R.; Kerwin, J.; Smith, M.H.; Wessman, H.C.; Venskus, D.G.; et al. Workforce projections 2010-2020: Annual supply and demand forecasting models for physical therapists across the Unites States. Phsyical Ther. 2016, 96, 71–80. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lacroix, A.; Hortobágyi, T.; Beurskens, R.; Granacher, U. Effects of supervised vs. unsupervised training programs on balance and muscle strength in older adults: A systematic review and meta-analysis. Sports Med. 2017, 47, 2341–2361. [Google Scholar] [CrossRef]
- Sherrington, C.; Fairhall, N.; Wallbank, G.; Tiedemann, A.; Michaleff, Z.A.; Howard, K.; Clemson, L.; Hopewell, S.; Lamb, S. Exercise for preventing falls in older people living in the community: An abridged Cochrane systematic review. Br. J. Sports Med. 2020, 54, 885–891. [Google Scholar] [CrossRef] [PubMed]
- Sigrist, R.; Rauter, G.; Riener, R.; Wolf, P. Augmented visual, auditory, haptic, and multimodal feedback in motor learning: A review. Psychon. Bull. Rev. 2013, 20, 21–53. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mak, T.C.T.; Wong, T.W.L.; Ng, S.S.M. Visual-related training to improve balance and walking ability in older adults: A systematic review. Exp. Gerontol. 2021, 156, 111612. [Google Scholar] [CrossRef]
- De Angelis, S.; Princi, A.A.; Dal Farra, F.; Morone, G.; Galtagirone, C.; Tramontano, M. Vibrotactile-based rehabilitation on balance and gait in patients with neurological diseases: A systematic review and metanalysis. Brain Sci. 2021, 11, 518. [Google Scholar] [CrossRef]
- Bao, T.; Carender, W.J.; Kinnaird, C.; Barone, V.J.; Peethambaran, G.; Whitney, S.L.; Kabeto, M.; Seidler, R.D.; Sienko, K.H. Effects of long-term balance training with vibrotactile sensory augmentation among community-dwelling healthy older adults: A randomized preliminary study. J. NeuroEng. Rehabil. 2018, 15, 5. [Google Scholar] [CrossRef] [Green Version]
- Kinnaird, C.; Lee, J.; Carender, W.J.; Kabeto, M.; Martin, B.; Sienko, K.H. The effects of attractive vs. repulsive instructional cuing on balance performance. J. NeuroEng. Rehabil. 2016, 13, 29. [Google Scholar] [CrossRef] [Green Version]
- Halická, Z.; Lobotková, J.; Bučková, K.; Bzdúšková, D.; Hlavačka, F. Age-related effect of visual biofeedback on human balance control. Act. Nerv. Super. Rediviva 2011, 53, 67–71. [Google Scholar]
- Dozza, M.; Chiari, L.; Chan, B.; Rocchi, L.; Horak, F.B.; Cappello, A. Influence of a portable audio-biofeedback device on structural properties of postural sway. J. NeuroEng. Rehabil. 2005, 2, 2–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chiari, L.; Dozza, M.; Cappello, A.; Horak, F.B.; Macellari, V. Audio-biofeedback for balance improvement: An accelerometry-based system. IEEE Trans. Biomed. Eng. 2005, 52, 2108–2111. [Google Scholar] [CrossRef]
- Zijlstra, A.; Mancini, M.; Chiari, L.; Zijlstra, W. Biofeedback for training balance and mobility tasks in older populations: A systematic review. J. NeuroEng. Rehabil. 2010, 7, 58. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alhasan, H.; Hood, V.; Mainwaring, F. The effect of visual biofeedback on balance in elderly population: A systematic review. Clin. Interv. Aging 2017, 12, 487–497. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alhagbani, A.; Williams, A. Home-based exergames for older adults balance and falls risk: A systematic review. Phys. Occup. Ther. Geriatr. 2021, 39, 241–257. [Google Scholar] [CrossRef]
- Prieto, T.E.; Myklebust, J.B.; Hoffmann, R.G.; Lovett, E.G.; Myklebust, B.M. Measures of postural steadiness: Differences between healthy young and elderly adults. IEEE Trans. Biomed. Eng. 1996, 43, 956–966. [Google Scholar] [CrossRef] [PubMed]
- Sienko, K.H.; Balkwill, M.D.; Oddsson, L.I.E.; Wall, C. Effects of multi-directional vibrotactile feedback on vestibular-deficient postural performance during continuous multi-directional support surface perturbations. J. Vestib. Res. 2008, 18, 273–285. [Google Scholar] [CrossRef] [PubMed]
- Babadi, S.Y.; Daneshmandi, H. Effects of virtual reality versus conventional balance training on balance of the elderly. Exp. Gerontol. 2021, 153, 111498. [Google Scholar] [CrossRef]
- Yang, C.-M.; Hsieh, J.C.; Chen, Y.-C.; Yang, S.-Y.; Lin, H.-C.K. Effects of Kinect exergames on balance training among community older adults. Medicine 2020, 99, e21228. [Google Scholar] [CrossRef]
- Barry, G.; van Schaik, P.; MacSween, A.; Dixon, J.; Martin, D. Exergaming (XBOX KinectTM) versus traditional gym-based exercise for postural control, flow and technology acceptance in healthy adults: A randomized controlled trial. BMC Sports Sci. Med. Rehabil. 2016, 8, 25. [Google Scholar] [CrossRef] [Green Version]
- Sienko, K.H.; Seidler, R.D.; Carender, W.J.; Goodworth, A.D.; Whitney, S.L.; Peterka, R.J. Potential mechanisms of sensory augmentation systems on human balance control. Front. Neurol. 2018, 9, 944. [Google Scholar] [CrossRef] [PubMed]
- Dozza, M.; Chiari, L.; Peterka, R.J.; Wall, C.; Horak, F.B. What is the most effective type of audio-biofeedback for postural motor learning? Gait Posture 2011, 34, 313–319. [Google Scholar] [CrossRef] [PubMed]
- Taube, W.; Leukel, C.; Gollhofer, A. Influence of enhanced visual feedback on postural control and spinal reflex modulation during stance. Exp. Brain Res. 2008, 188, 353–361. [Google Scholar] [CrossRef] [PubMed]
- Davis, J.R.; Carpenter, M.G.; Tschanz, R.; Meyes, S.; Debrunner, D.; Burger, J.; Allum, J.H.J. Trunk sway reductions in young and older adults using multi-modal biofeedback. Gait Posture 2010, 31, 456–472. [Google Scholar] [CrossRef]
- Lee, B.-C.; Kim, J.; Chen, S.; Sienko, K.H. Cell phone based balance trainer. J. NeuroEng. Rehabil. 2012, 9, 10. [Google Scholar] [CrossRef] [Green Version]
- Bechly, K.E.; Carender, W.J.; Myles, J.D.; Sienko, K.H. Determining the preferred modality for real-time biofeedback during balance training. Gait Posture 2013, 37, 391–396. [Google Scholar] [CrossRef]
- Ma, C.Z.-H.; Lee, W.C.-C. A wearable vibrotactile biofeedback system improves balance control of healthy young adults following perturbations from quiet stance. Hum. Mov. Sci. 2017, 55, 54–60. [Google Scholar] [CrossRef]
- Grewal, G.S.; Schwenk, M.; Lee-Eng, J.; Parvaneh, S.; Bharara, M.; Menzies, R.A.; Talal, T.K.; Armstrong, D.G.; Najafi, B. Sensor-based interactive balance training with visual joint movement feedback for improving postural stability in diabetics with peripheral neuropathy: A randomized controlled trial. Gerontology 2015, 61, 567–574. [Google Scholar] [CrossRef]
- Basta, D.; Rossi-Izquierdo, M.; Soto-Varela, A.; Greters, M.E.; Bittar, R.S.; Steinhagen-Thiessen, E.; Eckardt, R.; Harada, T.; Goto, F.; Ogawa, K.; et al. Efficacy of a vibrotactile neurofeedback training in stance and gait conditions for the treatment of balance deficits: A double-blind, placebo-controlled multicenter study. Otol. Neurotol. 2011, 32, 1492–1499. [Google Scholar] [CrossRef] [Green Version]
- Rossi-Izquierdo, M.; Ernst, A.; Soto-Varela, A.; Santos-Pérez, S.; Faraldo-García, A.; Sesar-Ignacio, A.; Basta, D. Vibrotactile neurofeedback balance training in patients with Parkinson’s disease: Reducing the number of falls. Gait Posture 2013, 37, 195–200. [Google Scholar] [CrossRef]
- Brugnera, C.; Bittar, R.S.M.; Greters, M.E.; Basta, D. Effects of vibrotactile vestibular substitution on vestibular rehabilitation—preliminary study. Braz. J. Otorhinolaryngol. 2015, 81, 616–621. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, J.D.; Wickens, C.D.; Liu, Y.; Boyle, L.N. Designing for People: An Introduction to Human Factors Engineering, 3rd ed.; CreateSpace: Charleston, SC, USA, 2017. [Google Scholar]
- Ranganathan, R.; Newell, K.M. Influence of Augmented feedback on coordination strategies. J. Mot. Behav. 2009, 41, 317–330. [Google Scholar] [CrossRef] [PubMed]
- Sigrist, R.; Rauter, G.; Riener, R.; Wolf, P. Terminal feedback outperforms concurrent visual, auditory, and haptic feedback in learning a complex rowing-type task. J. Mot. Behav. 2013, 45, 455–472. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yamamoto, R.; Akizuki, K.; Kanai, Y.; Nakano, W.; Kobayashi, Y.; Ohashi, Y. Differences in skill level influence the effects of visual feedback on motor learning. J. Phys. Ther. Sci. 2019, 31, 939–945. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Winstein, C.J.; Pohl, P.S.; Lewthwaite, R. Effects of physical guidance and knowledge of results on motor learning: Support for the guidance hypothesis. Res. Q. Exerc. Sport 1994, 65, 316–323. [Google Scholar] [CrossRef]
- Goodwin, J.E.; Goggin, N.L. An older adult study of concurrent visual feedback in learning continuous balance. Percept. Mot. Ski. 2018, 125, 1160–1172. [Google Scholar] [CrossRef]
- Sullivan, K.J.; Kantak, S.S.; Burtner, P.A. Motor learning in children: Feedback effects on skill acquisition. Phys. Ther. 2008, 88, 720–732. [Google Scholar] [CrossRef]
- Wulf, G.; Schmidt, R.A. The learning of generalized motor programs: Reducing the relative frequency of knowledge of results enhances memory. J. Exp. Psychol. Learn. Mem. Cogn. 1989, 15, 748–757. [Google Scholar] [CrossRef]
- Thomas, M.D. The Effects of Relative Frequency of Knowledge of Results on Brain Injured and Neurologically Normal Individuals Learning a Linear Positioning Task. Master’s Thesis, Grand Valley State University, Allendale, MI, USA, 1995. [Google Scholar]
- Gandia, J.; Garcia-Masso, X.; Marco-Ahullo, A.; Estevan, I. Adolescents’ postural control learning according to the frequency of knowledge of process. J. Mot. Learn. Dev. 2019, 7, 204–214. [Google Scholar] [CrossRef]
- Marco-Ahullo, A.; Sandchez-Tormo, A.; Garcia-Perez, J.A.; Villarrasa-Sapina, I.; Gonzalez, L.M.; Garcia-Masso, X. Effect of concurrent visual feedback frequency on postural control learning in adolescents. J. Mot. Behav. 2019, 51, 193–198. [Google Scholar] [CrossRef]
- Huffman, J.L.; Norton, L.E.; Adkin, A.L.; Allum, J.H.J. Directional effects of biofeedback on trunk sway during stance tasks in healthy young adults. Gait Posture 2010, 32, 62–66. [Google Scholar] [CrossRef] [PubMed]
- Dos Anjos, F.; Lemos, T.; Imbiriba, L.A. Does the type of visual feedback information change the control of standing balance? Eur. J. Appl. Physiol. 2016, 116, 1771–1779. [Google Scholar] [CrossRef] [PubMed]
- Siqueira, C.M.; Moya, G.B.L.; Caffaro, R.R.; Fu, C.; Kohn, A.F.; Amorim, C.F.; Tanaka, C. Misalignment of the knees: Does it affect human stance stability. Posture Physiol. 2011, 15, 235–241. [Google Scholar] [CrossRef] [PubMed]
- Dault, M.C.; de Haart, M.; Geurts, A.C.H.; Arts, I.M.P.; Nienhuis, B. Effects of visual center of pressure feedback on postural control in young and elderly healthy adults and in stroke patients. Hum. Mov. Sci. 2003, 22, 221–236. [Google Scholar] [CrossRef]
- Wiesmeier, I.K.; Dalin, D.; Wehrle, A.; Granacher, U.; Muehlbauer, T.; Dietterle, J.; Weiller, C.; Gollhofer, A.; Maurer, C. Balance training enhances vestibular function and reduces overactive proprioceptive feedback in elderly. Front. Aging Neurosci. 2017, 9, 273. [Google Scholar] [CrossRef]
- Chang, J.-Y.; Chang, G.-L.; Chien, C.-J.C.; Chung, K.-C.; Hsu, A.-T. Effectiveness of two forms of feedback on training of a joint mobilization skill by using a joint translation simulator. Phys. Ther. J. 2007, 87, 418–430. [Google Scholar] [CrossRef] [Green Version]
- Vitale, R.V.; Barone, V.J.; Ferris, J.; Stirling, L.A.; Sienko, K.H. Effects of concurrent and terminal visual feedback on ankle co-contraction in older adults during standing balance. Sensors 2021, 21, 7305. [Google Scholar] [CrossRef]
- Krpič, A.; Savanović, A.; Cikajlo, I. Telerehabilitation remote multimedia-supported assistance and mobile monitoring of balance training outcomes can facilitate the clinical staff’s effort. Int. J. Rehabil. Res. 2013, 36, 162–171. [Google Scholar] [CrossRef]
- Walker, C.; Brouwer, B.J.; Culham, E.G. Use of visual feedback in retraining balance following acute stroke. Phys. Ther. 2000, 80, 886–895. [Google Scholar] [CrossRef] [Green Version]
- Yang, W.-C.; Wang, H.-K.; Wu, R.-M.; Lo, C.-S.; Lin, K.-H. Home-based virtual reality balance training and conventional balance training in Parkinson’s disease: A randomized controlled trial. J. Formos. Med. Assoc. 2016, 116, 734–743. [Google Scholar] [CrossRef] [Green Version]
- Yen, C.-Y.; Lin, K.-H.; Hu, M.-H.; Wu, R.-M.; Lu, T.-W.; Lin, C.-H. Effects of virtual reality—Augmented balance training on sensory organization and attentional demand for postural control in people with Parkinson Disease: A randomized controlled trial. Phys. Ther. 2011, 91, 862–874. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Age | Sex | Height (m) | Mass (kg) | |
|---|---|---|---|---|
| Group 1: Concurrent First (N = 10) | 70.4 (±3.0) | 7 Female | 1.64 (±0.10) | 72 (±16) |
| Group 2: Terminal First (N = 9) | 70.0 (±4.0) | 5 Female | 1.66 (±0.06) | 72 (±9) |
| Natural Log of Feature | Exponent on Trial Number (a) | Intercept (1) | Order | Block | TrialNumber a | Concurrent Feedback Removed | Terminal Feedback Removed |
|---|---|---|---|---|---|---|---|
| Phi RMS | 0.4 | Yes | No | Yes * | Yes * | Yes * | Yes |
| AP RMS | 0.5 | Yes * | No | Yes * | Yes * | Yes * | Yes |
| ML RMS | 0.1 | Yes * | No | No | Yes * | Yes * | Yes |
| MV | 0.1 | Yes | No | No | Yes * | Yes * | Yes |
| PL | 0.1 | Yes | No | No | Yes * | Yes * | Yes |
| EA | 0.3 | Yes * | No | Yes | Yes * | Yes * | Yes |
| Natural Log of Feature | Block: TrialNumber a | Block: Order | Concurrent Feedback Removed: Order | Terminal Feedback Removed: Order | Age | Sex | Participant |
| Phi RMS | No | No | No | No | No | Yes | Yes |
| AP RMS | No | No | No | No | No | Yes * | Yes |
| ML RMS | Yes * | Yes * | Yes | No | No | No | Yes |
| MV | Yes * | No | No | Yes | No | No | Yes |
| PL | Yes * | No | No | Yes | Yes | No | Yes |
| EA | No | No | No | No | No | Yes | Yes |
| Natural Log of Feature | Exponent on Trial Number (a) | Effect of Training with Concurrent Feedback | Difference in the Effects of Training with Terminal vs. Concurrent Feedback | ||
|---|---|---|---|---|---|
| p-Value | Estimate [95% CI] | p-Value | Estimate [95% CI] | ||
| Phi RMS | 0.4 | <0.001 * | −0.030 [−0.046, −0.014] | 0.975 | −0.000 [−0.047, 0.046] |
| AP RMS | 0.5 | <0.001 * | −0.038 [−0.052, −0.023] | 0.752 | 0.007 [−0.037, 0.052] |
| ML RMS | 0.1 | 0.004 * | −0.095 [−0.159, −0.031] | <0.001 * | 0.099 [0.049, 0.149] |
| MV | 0.1 | 0.012 * | 0.044 [0.010, 0.078] | <0.001 * | −0.116 [−0.142, −0.090] |
| PL | 0.1 | 0.004 | 0.052 [0.016, 0.087] | <0.001 * | −0.127 [−0.154, −0.010] |
| EA | 0.3 | <0.001 * | −0.073 [−0.115, −0.030] | 0.927 | 0.005 [−0.109, 0.120] |
| Effect of Removing Concurrent Feedback | Effect of Removing Terminal Feedback | ||||
| p-Value | Estimate [95% CI] | p-Value | Estimate [95% CI] | ||
| Phi RMS | 0.4 | <0.001 * | 0.092 [0.038, 0.146] | 0.711 | 0.011 [−0.045, 0.066] |
| AP RMS | 0.5 | <0.001 * | 0.121 [0.051, 0.192] | 0.526 | 0.024 [−0.049, 0.096] |
| ML RMS | 0.1 | 0.003 * | 0.106 [0.036, 0.175] | 0.573 | −0.016 [−0.072, 0.040] |
| MV | 0.1 | <0.001 * | −0.170 [−0.207, −0.132] | 0.251 | −0.027 [−0.074, 0.019] |
| PL | 0.1 | <0.001 * | −0.185 [−0.224, −0.146] | 0.209 | −0.031 [−0.080, 0.017] |
| EA | 0.3 | 0.003 | 0.149 [0.050, 0.248] | 0.944 | 0.004 [−0.098, 0.106] |
| Natural Log of Feature | After Training with Concurrent Feedback | After Training with Terminal Feedback | ||
|---|---|---|---|---|
| p-Value | Estimate [95% CI] | p-Value | Estimate [95% CI] | |
| Phi RMS | 0.910 | 0.004, [−0.062, 0.070] | 0.022 * | −0.07, [−0.145, −0.010] |
| AP RMS | 0.557 | 0.024, [−0.107, 0.059] | 0.005 * | 0.122, [−0.208, −0.037] |
| ML RMS | 0.732 | −0.014, [−0.097, 0.068] | 0.752 | −0.011, [−0.082, 0.059] |
| MV | <0.001 * | 0.111, [−0.159, −0.063] | <0.001 * | −0.122, [−0.179, −0.065] |
| PL | <0.001 * | −0.117, [−0.167, −0.068] | <0.001 * | −0.130, [−0.189, −0.071] |
| EA | 0.815 | −0.015, [−0.140, 0.110] | 0.013 * | −0.160, [−0.288, −0.031] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ferris, J.; Barone, V.J.; Perkins, N.C.; Sienko, K.H. A Pilot Study Comparing the Effects of Concurrent and Terminal Visual Feedback on Standing Balance in Older Adults. Sensors 2022, 22, 2826. https://doi.org/10.3390/s22082826
Ferris J, Barone VJ, Perkins NC, Sienko KH. A Pilot Study Comparing the Effects of Concurrent and Terminal Visual Feedback on Standing Balance in Older Adults. Sensors. 2022; 22(8):2826. https://doi.org/10.3390/s22082826
Chicago/Turabian StyleFerris, Jamie, Vincent J. Barone, Noel C. Perkins, and Kathleen H. Sienko. 2022. "A Pilot Study Comparing the Effects of Concurrent and Terminal Visual Feedback on Standing Balance in Older Adults" Sensors 22, no. 8: 2826. https://doi.org/10.3390/s22082826
APA StyleFerris, J., Barone, V. J., Perkins, N. C., & Sienko, K. H. (2022). A Pilot Study Comparing the Effects of Concurrent and Terminal Visual Feedback on Standing Balance in Older Adults. Sensors, 22(8), 2826. https://doi.org/10.3390/s22082826







