Monitoring Scapular Kinematics through Wearable Magneto-Inertial Measurement Units: State of the Art and New Frontiers
Abstract
:1. Introduction
2. Methods
2.1. Literature Search Strategy and Eligibility Criteria
- Papers are published in a journal or presented at a conference.
- The studies used wearable M-IMUs to track scapular kinematics.
- Sensors are placed directly on the human skin via an adhesive, embedded within pockets, straps, or integrated into fabrics.
- Upper limb functional tasks are investigated.
- Reviews, books.
- Use of exoskeleton or robotic systems.
- Scapular kinematics is not included in the upper limb motion analysis.
- Wearable devices are not directly tested on humans.
2.2. Data Collection Process
3. Results
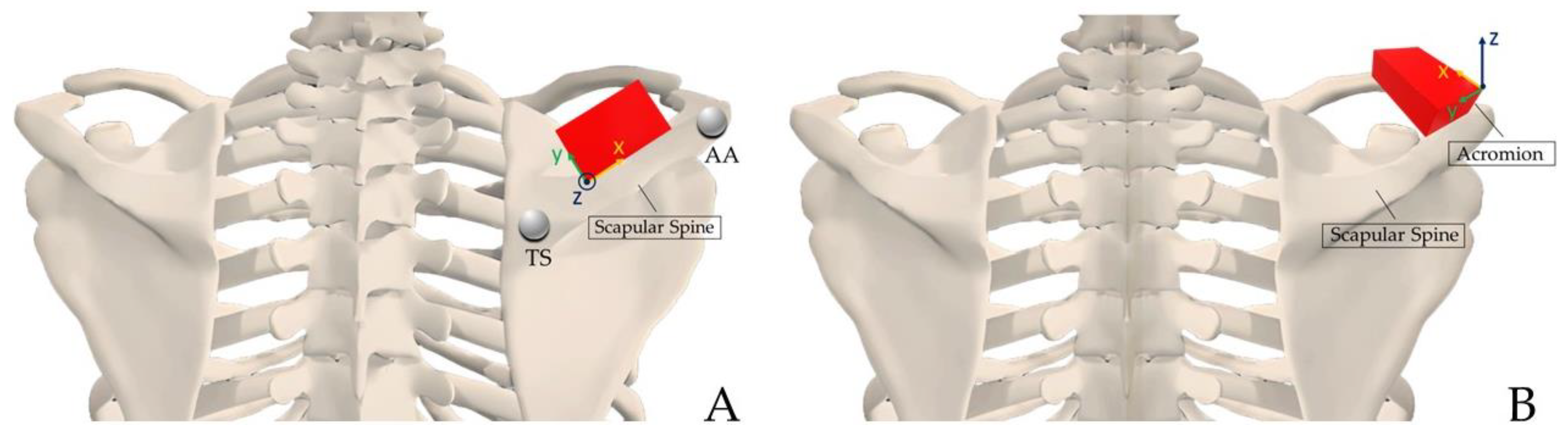
3.1. Sensors Positioning
3.2. Gold Standard
3.3. Calibration
3.4. Tasks Executed
| First Author, Year | M-IMUs: Brand Numbers and Placements | Gold Standard | Calibration Method | Participants | Tasks Executed | Aim |
|---|---|---|---|---|---|---|
| Cutti et al., 2008 [35] | MT9B (Xsens Technologies, NL) Unilateral (n = 3): thorax, scapulae (aligning with the scapular spine), and humerus | MOCAP (Vicon 460, Oxford Metrics, UK) | SC: the subject is instructed to stand still, with his back straight and with both arms alongside the body, perpendicular to the ground for 10 s | HS (n = 1) 1M 23.3 Y | Elbow FE, elbow PS, shoulder FE, IR, and ER shoulder-girdle elevation depression, PR, shoulder IR and ER with the arm abducted 90°, a shoulder AB-AD in the frontal plane, hand-to-nape task in the sagittal plane, and a hand-to-top-of-head task in the frontal plane | Develop a protocol to measure ST, HT joint angles, and elbow kinematics in ambulatory settings using M-IMUs |
| Parel et al., 2012 [36] | MTx sensor units (Xsens Technologies, NL) Unilateral (n = 3): thorax, scapulae (aligning with the scapular spine), and humerus | - | SC (static posture): upright position, elbow flexed at 90°, neutral forearm rotation, humerus perpendicular to the ground and in neutral rotation | P with MSDs (n = 20) 8F, 12M 28.3 ± 5.5 Y BMI 22.4 ± 1.8 HS (n = 20) 7F, 13M 43.9 ± 19.9 Y BMI 23.9 ± 4.8 | Humeral elevation in the sagittal (FE) and scapular (AB-AD) plane | Intra- and inter-operator agreement of ISEO protocol (INAIL Shoulder and Elbow Outpatient protocol based on inertial and magnetic sensors). |
| Parel et al., 2014 [41] | MTx sensor units (Xsens Technologies, NL) Unilateral (n = 3): thorax, scapulae (aligning with the scapular spine), and humerus | MOCAP (Motion Analysis Corporation; Santa Rosa, CA USA) | SC (static posture): upright position, elbow flexed at 90°, neutral forearm rotation, humerus perpendicular to the ground and in neutral rotation | HS (n = 23) 10F, 13M 29 ± 8 Y | Humeral elevation in the sagittal (FE) and scapular (AB-AD) plane | Comparison of two shoulder kinematic protocols. |
| van den Noort et al., 2014 [42] | MTw wireless sensor units (Xsens Technologies, NL) Unilateral (n = 4): thorax, scapulae (aligning with the scapular spine), upper arm, and lower arm | - | SC (static posture for few seconds): trunk upright, the upper arm along the trunk for neutral humerus internal/external rotation, and the elbow in 90° flexion | HS (n = 20) 17F, 3M 36 ± 11 Y BMI: 22 ± 2 Physical therapists (n = 2) | Elbow FE and shoulder PS | Intra- and inter-operator reliability and precision of the scapular kinematics using M-IMU. |
| Roldán-Jiménez et al., 2015 [43] | InertiaCube3™ (Intersense Inc., Billerica, MA, USA) Unilateral (n = 4): thorax, scapulae (along the scapular spine), humerus, and distal surface of the ulna and radius | - | - | Young HS (n = 11) 3F, 8M | Subject performed 180° right shoulder AB-AD and 180° right shoulder FE with the elbow extended, the wrist in neutral position, and the palmar area of the hand toward the midline at the beginning and end of the movement | Analyse upper-limb motions in the three anatomical axes. |
| van den Noort et al., 2015 [44] | MTw wireless sensor units (Xsens Technologies, NL) Unilateral (n = 4): thorax, scapulae (aligning with the scapular spine), upper arm, and lower arm | - | SC (static posture with trunk upright, upper arm along the trunk, elbow in 90° flexion, elbow FE and PS); DC (measurements were performed at 0° HT elevation, and at 30°, 60°, 90°, and 120° of active static HT elevation with elbow fully extended and thumb pointing lateral or up) | P with scapular dyskinesis (n = 10) | Bilateral active FE in the sagittal plane, bilateral, active AB-AD in the frontal plane (elbow fully extended and thumb pointing up) | Evaluate the change in 3D scapular kinematics caused by SC and DC with a scapular locator versus ISEO-protocol; assess the difference in 3D scapular kinematics between static posture and dynamic humeral elevation. |
| Roldán Jiménez et al., 2016 [45] | InertiaCube3™ (Intersense Inc., Billerica, MA, USA) Unilateral (n = 4): thorax, scapulae (along the scapular spine), humerus, and distal surface of the ulna and radius | - | - | Young HS (n = 11) 8F, 3M Older HS (n = 14) 9F, 5M | Shoulder abduction in the coronal plane and shoulder flexion in the sagittal plane | Analyse age-related differences in shoulder kinematics between young and older asymptomatic adults. |
| Carbonaro et al., 2018 [49] | MTw wireless sensor units (Xsens Technologies, NL) Unilateral (n = 3): thorax, scapulae (along the scapular spine), and humerus | - | - | Physiotherapists (n = 2) HS (n = 5) | ER arm AB-AD | Define a new set of WS capable of evaluating the shoulder angles to characterize classic shoulder rehabilitation tasks and discriminate correct and incorrect movements. |
| Ajčević et al., 2020 [46] | MTw wireless sensor units (Xsens Technologies, NL) Unilateral (n = 3): thorax, scapulae (along the scapular spine), and humerus | - | SC: upright position, elbow flexed at 90° | P with AC (n = 6) 3F, 3M 53.8 ± 4.3 Y HS (n = 7) 3F, 4M 41.3 ± 4.3 Y | Micro-mobilization of accessory clavicula, AC and SCl joints, scapula, cervical and dorsal rachis. Dynamic mobilizations: anterior flexion, abduction, ER, and IR and postural active exercises | Investigate the possibility to quantitatively evaluate patients who suffer from capsulate-related deficit versus healthy controls and assess treatment efficacy. |
| Iban et al., 2020 [47] | Bilateral (n = 5): one at the manubrium sterni, two on each suprascapular fossae and two over the lateral aspect of both arms | - | SC: subject standing upright, the humerus positioned alongside the body and the elbow flexed at 90° | HS (n = 25) 12F, 13M 37 ± 11.1 Y | FE and AB-AD movements | Evaluate the intra- and interobserver reproducibility for assessing the 3D shoulder kinematics in an outpatient setting. |
| Höglund et al., 2021 [50] | Unilateral (n = 7): one sensor on thorax, two on the scapula (the first on the flat surface of acromion and the second aligned with the scapular spine), two on the upper arm, and two on the forearm | MOCAP | SC: the arms hanging vertically, alongside the participant, with the palm of the hand pointing medially | HS (n = 11) 5F, 6M 28 ± 6.5 Y | Nine arm-movement tasks based on the Modified Mallet Scale [54] | Evaluate how sensor placement affects kinematic outputs in the assessment of motion of the arm, shoulder, and scapula. |
| Grip et al., 2022 [38] | Bilateral (n = 7): thorax, scapula sensors (cranially on the middle part of spina scapulae), upper arm, and forearm sensors | MOCAP (Oqus, Qualisys AB, Gothenburg, Sweden) | SC: the arms alongside the body with palms facing the body | BPBI group (n = 6) 8–22 Y 4F, 2M Control group (n = 9) 7–25 Y 6F, 3M | Shoulder FE in the sagittal plane, elbow FE in the sagittal plane, forearm PS, maximal AB-AD, ER, IR, hand to neck, hand to spine, and hand to mouth | Evaluate the validity of a wearable M-IMUs-based system in healthy individuals; assess the test–retest and inter-rater reliability in a group of BPBI patients and non-asymptomatic individuals. |
| Friesen et al., 2023 [37] | XSens Awinda (Xsens Technologies, NL) Bilateral (n = 5): sternum, bilateral posterior, and distal end of the humeri on scapulae (with the x-axis of the sensor perpendicular to the scapular spine or aligned with mid-scapular spine) | MOCAP (Vicon, Oxford, UK) | DC: at neutral position and at maximum humeral elevation | HS (n = 30) 15F, 15M 24 ± 4 Y Height 1.7 ± 0.1 m Weight 78.6 ± 16.9 kg | AB-AD in the frontal plane, FE in the sagittal plane, and eight tasks of the WRAFT protocol [55] | Assess the reliability of scapular motion M-IMU measurements compared to the gold standard; compare scapular M-IMU placement to assess which location (acromion or spine) was the best for the validity and reliability of scapular kinematics. |
| Reina et al., 2023 [48] | ShowMotion (NCS Lab srl, Modena, Italy) Bilateral (n = 7): thorax, scapula sensors (on suprascapular fossae), upper arm, and forearm sensors | - | - | P with RTSA (n = 14) 7F, 7M | FE, AB-AD in the scapular plane, IR/ER with elbow abducted to the thorax, and IR/ER with shoulder abduction at 90° and elbow flexed to 90° | Assess upper extremity kinematics and active ROM in patients who underwent RTSA compared with the contralateral side and quantify the ST motion. |
| Study, Year | Tasks Executed | Scapular Parameters and Performance Coefficients | ||
|---|---|---|---|---|
| Tilt | MLR | IER | ||
| Parel et al., 2012 [36] | FE Ab-Ad | CMC (SD) = 0.95° (0.05°), SEM = 3.1°, SDD = 8.5° CMC (SD) = 0.94° (0.06°), SEM = 2.7°, SDD = 7.4° | CMC (SD) = 0.96° (0.04°), SEM = 2.2°, SDD = 6.2° CMC (SD) = 0.95° (0.06°), SEM = 1.8°, SDD = 4.9° | CMC (SD) = 0.85° (0.11°), SEM = 2.6°, SDD = 7.1° CMC (SD) = 0.87° (0.11°), SEM = 3.0°, SDD = 8.3° |
| Parel et al., 2014 [41] | FE (max HT) Ab-Ad (max HT) | SEM = 1.7°, RMSE = 1.5° SEM = 2.2°, RMSE = 2.15° | SEM = 2.6°, RMSE = 2.75° SEM = 3.3°, RMSE = 3.42° | SEM = 2.2°, RMSE = 1.96° SEM = 2.2°, RMSE = 2.3° |
| van den Noort et al., 2014 [42] | Flexion (max HT) Abduction (max HT) | ICC = 0.67, SEM = 5, SDD = 13 ICC = 0.71, SEM = 5, SDD = 13 | ICC = 0.88, SEM = 3, SDD = 9 ICC = 0.84, SEM = 4, SDD = 10 | ICC = 0.80, SEM = 5, SDD = 14 ICC = 0.78, SEM = 5, SDD = 14 |
| Roldán Jiménez et al., 2015 [43] | Flexion Abduction | Mean ROM (SD) = 4.1° (16.9°) Mean ROM (SD) = −5.5° (12.3°) | Mean ROM (SD) = −7.7° (48.6°) Mean ROM (SD) = −5.9° (9.5°) | Mean ROM (SD) = 37.8° (6.3°) Mean ROM (SD) = 36.6° (10.2°) |
| van den Noort et al., 2015 [44] | Humeral abduction (max = 150°) | Mean difference = −8.4° Standard Error = 8.8° | Mean difference = 14.4° Standard Error = 10.1° | Mean difference = −12.1° Standard Error = 24.8° |
| Roldán-Jiménez et al., 2016 [45] | FE (young group) FE (older group) Ab-Ad (young group) Ab-Ad (older group) | Mean ROM = 17.8° (8.9°–26.7°) Mean ROM = 23.2° (18.7°–27.7°) Mean ROM = 10.7° (5.6°–15.8°) Mean ROM = 15.6° (11.2°–19.9°) | Mean ROM = 19° (9.3°–28.6°) Mean ROM = 5.4° (3.5°–7.4°) Mean ROM = 10.1° (6.14°–14.2°) Mean ROM = 5.73° (2.52°–8.95°) | Mean ROM = 44° (39.2°–48.8°) Mean ROM = 29° (25°–33.1°) Mean ROM = 42.1° (36.3°–47.9°) Mean ROM = 33.8° (27.5°–40.1°) |
| Ajčević et al., 2020 [46] | Ab-Ad (pre-treatment) Ab-Ad (post-treatments) | Mean ROM (SD) = 21° ± 7.1° Mean ROM (SD) = 34.6° ± 7.7° | ||
| Iban et al., 2020 [47] | Flexion (max HT) Abduction (max HT) | Mean ROM (SD) = 12.9° (6.65°) Mean ROM (SD) = 10.3° (6.1°) | Mean ROM (SD) = 25.2° (5.44°) Mean ROM (SD) = 24.0° (5.29°) | Mean ROM (SD) = −4.57° (5.20°) Mean ROM (SD) = −3.53° (5.66°) |
| Grip et al., 2022 [38] | FE Ab-Ad ER Hand-to-mouth IR | ICC = 0.92 ICC = 0.88 ICC = 0.92 ICC = 0.93 ICC = 0.97 | ICC = 0.71 ICC = 0.80 ICC = 0.94 ICC = 0.84 ICC = 0.80 | ICC = 0.71 ICC = 0.71 ICC = 0.88 ICC = 0.85 ICC = 0.92 |
| Friesen et al., 2023 [37] * | Combining Hair (Acromion) Combining Hair (Spine) Overhead Reach (Acromion) Overhead Reach (Spine) Overhead Lift (Acromion) Overhead Lift (Spine) Abduction (Acromion) Abduction (Spine) Flexion (Acromion) Flexion (Spine) | ICC = 0.504, RMSE = 14.7° ICC = −0.029, RMSE = 15.8° ICC = 0.209, RMSE = 14.1° ICC = −0.478, RMSE = 24.5° ICC = 0.267, RMSE = 14.7° ICC = −0.611, RMSE = 27.7° ICC = 0.426, RMSE = 15.0° ICC = 0.180, RMSE = 24.7° ICC = 0.446, RMSE = 18.8° ICC = −0.006, RMSE = 23.0° | ICC = 0.740, RMSE = 7.0° ICC = 0.606, RMSE = 11.3° ICC = 0.504, RMSE = 11.8° ICC = 0.720, RMSE = 8.8° ICC = 0.638, RMSE = 12.8° ICC = 0.523, RMSE = 12.1° ICC = 0.646, RMSE = 9.8° ICC = 0.652, RMSE = 10.6° ICC = 0.664, RMSE = 9.4° ICC = 0.312, RMSE = 12.7° | ICC = 0.855, RMSE = 9.9° ICC = 0.651, RMSE = 10.9° ICC = 0.677, RMSE = 13.4° ICC = 0.22, RMSE = 15.0° ICC = 0.670, RMSE = 17.9° ICC = −1.069, RMSE = 25.6° ICC = 0.849, RMSE = 12.2° ICC = 0.207, RMSE = 20.8° ICC = 0.914, RMSE = 10.8° ICC = 0.433, RMSE = 15.9° |
| Reina et al., 2023 [48] | FE (path. − max HT) FE (healthy − max HT) Ab-Ad (path. − max HT) Ab-Ad (healthy − max HT) | Mean ROM (SD) = 28.9° (7.5°) Mean ROM (SD) = 22.0° (8.9°) Mean ROM (SD) = 20.3° (6.7°) Mean ROM (SD) = 19.0° (6.1°) | Mean ROM (SD) = 34.1° (9.9°) Mean ROM (SD) = 31.4° (13.0°) Mean ROM (SD) = 27.10° (6.7) Mean ROM (SD) = 23.8° (5.6) | Mean ROM (SD) = −12.7° (9.0°) Mean ROM (SD) = −8.7° (8.6°) Mean ROM (SD) = −12.9° (7.8°) Mean ROM (SD) = −12.4° (6.8°) |
3.5. Scapular Kinematics and Systems’ Performance
4. Discussion
4.1. Application in a Clinical Scenario
4.2. Recommendations and New Frontiers
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Matsuki, K.; Matsuki, K.O.; Mu, S.; Yamaguchi, S.; Ochiai, N.; Sasho, T.; Sugaya, H.; Toyone, T.; Wada, Y.; Takahashi, K.; et al. In vivo 3-dimensional analysis of scapular kinematics: Comparison of dominant and nondominant shoulders. J. Shoulder Elb. Surg. 2011, 20, 659–665. [Google Scholar] [CrossRef] [PubMed]
- Rockwood, C.A. The Shoulder; Elsevier Health Sciences: Amsterdam, The Netherlands, 2009; Volume 1. [Google Scholar]
- Shuai, Z.; Dong, A.; Liu, H.; Cui, Y. Reliability and Validity of an Inertial Measurement System to Quantify Lower Extremity Joint Angle in Functional Movements. Sensors 2022, 22, 863. [Google Scholar] [CrossRef]
- Chapman, R.M.; Torchia, M.T.; Bell, J.E.; Van Citters, D.W. Assessing Shoulder Biomechanics of Healthy Elderly Individuals During Activities of Daily Living Using Inertial Measurement Units: High Maximum Elevation Is Achievable but Rarely Used. J. Biomech. Eng. 2019, 141, 0410011–0410017. [Google Scholar] [CrossRef]
- Carnevale, A.; Longo, U.G.; Schena, E.; Massaroni, C.; Lo Presti, D.; Berton, A.; Candela, V.; Denaro, V. Wearable systems for shoulder kinematics assessment: A systematic review. BMC Musculoskelet. Disord. 2019, 20, 546. [Google Scholar] [CrossRef]
- Longo, U.G.; Carnevale, A.; Massaroni, C.; Lo Presti, D.; Berton, A.; Candela, V.; Schena, E.; Denaro, V. Personalized, Predictive, Participatory, Precision, and Preventive (P5) Medicine in Rotator Cuff Tears. J. Pers. Med. 2021, 11, 255. [Google Scholar] [CrossRef] [PubMed]
- Cook, G.; Burton, L.; Hoogenboom, B.J.; Voight, M. Functional movement screening: The use of fundamental movements as an assessment of function—Part 1. Int. J. Sports Phys. Ther. 2014, 9, 396–409. [Google Scholar] [PubMed]
- Carnevale, A.; Massaroni, C.; Presti, D.L.; Formica, D.; Longo, U.G.; Schena, E.; Denaro, V. Wearable stretchable sensor based on conductive textile fabric for shoulder motion monitoring. In Proceedings of the 2020 IEEE International Workshop on Metrology for Industry 4.0 & IoT, Rome, Italy, 3–5 June 2020; pp. 106–110. [Google Scholar]
- Longo, U.G.; Risi Ambrogioni, L.; Berton, A.; Candela, V.; Massaroni, C.; Carnevale, A.; Stelitano, G.; Schena, E.; Nazarian, A.; DeAngelis, J.; et al. Scapular Dyskinesis: From Basic Science to Ultimate Treatment. Int. J. Environ. Res. Public Health 2020, 17, 2974. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carnevale, A.; Schena, E.; Formica, D.; Massaroni, C.; Longo, U.G.; Denaro, V. Skin Strain Analysis of the Scapular Region and Wearables Design. Sensors 2021, 21, 5761. [Google Scholar] [CrossRef] [PubMed]
- Crowe, M.M.; Elhassan, B.T. Scapular and Shoulder Girdle Muscular Anatomy: Its Role in Periscapular Tendon Transfers. J. Hand Surg. 2016, 41, 306–314; quiz 315. [Google Scholar] [CrossRef]
- Mattson, J.M.; Russo, S.A.; Rose, W.C.; Rowley, K.M.; Richards, J.G. Identification of scapular kinematics using surface mapping: A validation study. J. Biomech. 2012, 45, 2176–2179. [Google Scholar] [CrossRef] [Green Version]
- Wu, G.; van der Helm, F.C.; Veeger, H.E.; Makhsous, M.; Van Roy, P.; Anglin, C.; Nagels, J.; Karduna, A.R.; McQuade, K.; Wang, X.; et al. ISB recommendation on definitions of joint coordinate systems of various joints for the reporting of human joint motion--Part II: Shoulder, elbow, wrist and hand. J. Biomech. 2005, 38, 981–992. [Google Scholar] [CrossRef]
- Roche, S.J.; Funk, L.; Sciascia, A.; Kibler, W.B. Scapular dyskinesis: The surgeon’s perspective. Shoulder Elb. 2015, 7, 289–297. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lawrence, R.L.; Roseni, K.; Bey, M.J. Correspondence between scapular anatomical coordinate systems and the 3D axis of motion: A new perspective on an old challenge. J. Biomech. 2022, 145, 111385. [Google Scholar] [CrossRef] [PubMed]
- Rundquist, P.J.; Obrecht, C.; Woodruff, L. Three-dimensional shoulder kinematics to complete activities of daily living. Am. J. Phys. Med. Rehabil. 2009, 88, 623–629. [Google Scholar] [CrossRef]
- Faisal, A.I.; Majumder, S.; Mondal, T.; Cowan, D.; Naseh, S.; Deen, M.J. Monitoring Methods of Human Body Joints: State-of-the-Art and Research Challenges. Sensors 2019, 19, 2629. [Google Scholar] [CrossRef] [Green Version]
- Longo, U.G.; De Salvatore, S.; Carnevale, A.; Tecce, S.M.; Bandini, B.; Lalli, A.; Schena, E.; Denaro, V. Optical Motion Capture Systems for 3D Kinematic Analysis in Patients with Shoulder Disorders. Int. J. Environ. Res. Public Health 2022, 19, 12033. [Google Scholar] [CrossRef]
- Medina-Mirapeix, F.; Martín-San Agustín, R.; Cánovas-Ambit, G.; García-Vidal, J.A.; Gacto-Sánchez, M.; Escolar-Reina, P. An Optoelectronic System for Measuring the Range of Motion in Healthy Volunteers: A Cross-Sectional Study. Medicina 2019, 55, 516. [Google Scholar] [CrossRef] [Green Version]
- Chan, L.Y.T.; Chua, C.S.; Chou, S.M.; Seah, R.Y.B.; Huang, Y.; Luo, Y.; Dacy, L.; Bin Abd Razak, H.R. Assessment of shoulder range of motion using a commercially available wearable sensor-a validation study. Mhealth 2022, 8, 30. [Google Scholar] [CrossRef]
- Patel, S.; Park, H.; Bonato, P.; Chan, L.; Rodgers, M. A review of wearable sensors and systems with application in rehabilitation. J. Neuroeng. Rehabil. 2012, 9, 21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johnson, G.R.; Stuart, P.R.; Mitchell, S. A method for the measurement of three-dimensional scapular movement. Clin. Biomech. 1993, 8, 269–273. [Google Scholar] [CrossRef]
- Meskers, C.G.; Vermeulen, H.M.; de Groot, J.H.; van Der Helm, F.C.; Rozing, P.M. 3D shoulder position measurements using a six-degree-of-freedom electromagnetic tracking device. Clin. Biomech. 1998, 13, 280–292. [Google Scholar] [CrossRef] [PubMed]
- Warner, M.B.; Chappell, P.H.; Stokes, M.J. Measurement of dynamic scapular kinematics using an acromion marker cluster to minimize skin movement artifact. J. Vis. Exp. 2015, 96, e51717. [Google Scholar] [CrossRef] [Green Version]
- Leardini, A.; Chiari, L.; Della Croce, U.; Cappozzo, A. Human movement analysis using stereophotogrammetry. Part 3. Soft tissue artifact assessment and compensation. Gait Posture 2005, 21, 212–225. [Google Scholar] [CrossRef] [PubMed]
- Lempereur, M.; Brochard, S.; Leboeuf, F.; Rémy-Néris, O. Validity and reliability of 3D marker based scapular motion analysis: A systematic review. J. Biomech. 2014, 47, 2219–2230. [Google Scholar] [CrossRef]
- Jafarian Tangrood, Z.; Sole, G.; Cury Ribeiro, D. Between-Day Reliability of Scapular Locator for Measuring Scapular Position During Arm Elevation in Asymptomatic Participants. J. Manip. Physiol. Ther. 2020, 43, 276–283. [Google Scholar] [CrossRef]
- van Andel, C.; van Hutten, K.; Eversdijk, M.; Veeger, D.; Harlaar, J. Recording scapular motion using an acromion marker cluster. Gait Posture 2009, 29, 123–128. [Google Scholar] [CrossRef]
- Kirking, B.; El-Gohary, M.; Kwon, Y. The feasibility of shoulder motion tracking during activities of daily living using inertial measurement units. Gait Posture 2016, 49, 47–53. [Google Scholar] [CrossRef]
- Gini, G.; Mazzon, L.; Pontiggia, S.; Paolo, B. A Classifier of Shoulder Movements for a Wearable EMG-Based Device. J. Med. Robot. Res. 2017, 2, 1740003. [Google Scholar] [CrossRef]
- Rivela, D.; Scanella, A.; Pavan, E.E.; Frigo, C.A.; Bellucco, P.; Gino, G. Analysis and Comparison of Features and Algorithms to Classify Shoulder Movements From sEMG Signals. IEEE Sens. J. 2018, 18, 3714–3721. [Google Scholar] [CrossRef]
- Tigrini, A.; Pettinari, L.A.; Verdino, F.; Fioretti, S.; Mengarelli, A. Shoulder Motion Intention Detection Through Myoelectric Pattern Recognition. IEEE Sens. Lett. 2021, 5, 1–4. [Google Scholar] [CrossRef]
- Nsugbe, E.; Al-Timemy, A.H. Shoulder girdle recognition using electrophysiological and low frequency anatomical contraction signals for prosthesis control. CAAI Trans. Intell. Technol. 2021, 7, 81–94. [Google Scholar] [CrossRef]
- Tigrini, A.; Al-Timemy, A.H.; Verdini, F.; Fioretti, S.; Morettini, M.; Burattini, L.; Mengarelli, A. Decoding transient sEMG data for intent motion recognition in transhumeral amputees. Biomed. Signal Process. Control 2023, 85, 104936. [Google Scholar] [CrossRef]
- Cutti, A.G.; Giovanardi, A.; Rocchi, L.; Davalli, A.; Sacchetti, R. Ambulatory measurement of shoulder and elbow kinematics through inertial and magnetic sensors. Med. Biol. Eng. Comput. 2008, 46, 169–178. [Google Scholar] [CrossRef]
- Parel, I.; Cutti, A.G.; Fiumana, G.; Porcellini, G.; Verni, G.; Accardo, A.P. Ambulatory measurement of the scapulohumeral rhythm: Intra- and inter-operator agreement of a protocol based on inertial and magnetic sensors. Gait Posture 2012, 35, 636–640. [Google Scholar] [CrossRef] [PubMed]
- Friesen, K.B.; Sigurdson, A.; Lang, A.E. Comparison of scapular kinematics from optical motion capture and inertial measurement units during a work-related and functional task protocol. Med. Biol. Eng. Comput. 2023, 61, 1521–1531. [Google Scholar] [CrossRef] [PubMed]
- Grip, H.; Källströmer, A.; Öhberg, F. Validity and Reliability of Wearable Motion Sensors for Clinical Assessment of Shoulder Function in Brachial Plexus Birth Injury. Sensors 2022, 22, 9557. [Google Scholar] [CrossRef]
- Foxlin, E. Motion Tracking Requirements and Technologies. In Handbook of Virtual Environments; Stanney, K., Ed.; Erlbaum (Lawrence) Associates Ltd.: Mahwah, NJ, USA, 2015; pp. 163–210. [Google Scholar]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef]
- Parel, I.; Cutti, A.G.; Kraszewski, A.; Verni, G.; Hillstrom, H.; Kontaxis, A. Intra-protocol repeatability and inter-protocol agreement for the analysis of scapulo-humeral coordination. Med. Biol. Eng. Comput. 2014, 52, 271–282. [Google Scholar] [CrossRef]
- van den Noort, J.C.; Wiertsema, S.H.; Hekman, K.M.C.; Schönhuth, C.P.; Dekker, J.; Harlaar, J. Reliability and precision of 3D wireless measurement of scapular kinematics. Med. Biol. Eng. Comput. 2014, 52, 921–931. [Google Scholar] [CrossRef]
- Roldán-Jiménez, C.; Cuesta-Vargas, A.I. Studying upper-limb kinematics using inertial sensors: A cross-sectional study. BMC Res. Notes 2015, 8, 532. [Google Scholar] [CrossRef] [Green Version]
- van den Noort, J.C.; Wiertsema, S.H.; Hekman, K.M.; Schönhuth, C.P.; Dekker, J.; Harlaar, J. Measurement of scapular dyskinesis using wireless inertial and magnetic sensors: Importance of scapula calibration. J. Biomech. 2015, 48, 3460–3468. [Google Scholar] [CrossRef]
- Roldán-Jiménez, C.; Cuesta-Vargas, A.I. Age-related changes analyzing shoulder kinematics by means of inertial sensors. Clin. Biomech. 2016, 37, 70–76. [Google Scholar] [CrossRef]
- Ajčević, M.; Deodato, M.; Murena, L.; Miladinović, A.; Mezzarobba, S.; Accardo, A. Assessment of mobility deficit and treatment efficacy in adhesive capsulitis by measurement of kinematic parameters using IMU sensors. In Proceedings of the 2020 IEEE International Symposium on Medical Measurements and Applications (MeMeA), Bari, Italy, 1 June–1 July 2020. [Google Scholar]
- Ruiz Ibán, M.A.; Paniagua Gonzalez, A.; Muraccini, M.; Asenjo Gismero, C.; Varini, A.; Berardi, A.; Mantovani, M. Evaluation of a novel portable three-dimensional scapular kinematics assessment system with inter and intraobserver reproducibility and normative data for healthy adults. J. Exp. Orthop. 2020, 7, 31. [Google Scholar] [CrossRef] [PubMed]
- Reina, M.; Fiumana, G.; Mantovani, M.; D’Antonio, L.; Porcellini, G. Scapulohumeral rhythm in shoulders with reverse shoulder arthroplasty measured with a new portable three-dimensional scapular kinematics assessment system. J. Shoulder Elb. Surg. 2023, 32, 729–737. [Google Scholar] [CrossRef]
- Carbonaro, N.; Lucchesi, I.; Lorusssi, F.; Tognetti, A. Tele-monitoring and tele-rehabilitation of the shoulder muscular-skeletal diseases through wearable systems. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2018, 2018, 4410–4413. [Google Scholar] [CrossRef] [PubMed]
- Höglund, G.; Grip, H.; Öhberg, F. The importance of inertial measurement unit placement in assessing upper limb motion. Med. Eng. Phys. 2021, 92, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Feng, X.; Kim, J.H.; Rajulu, S. Review of biomechanical models for human shoulder complex. Int. J. Hum. Factors Model. Simul. 2010, 1, 271–293. [Google Scholar] [CrossRef]
- Brochard, S.; Lempereur, M.; Rémy-Néris, O. Double calibration: An accurate, reliable and easy-to-use method for 3D scapular motion analysis. J. Biomech. 2011, 44, 751–754. [Google Scholar] [CrossRef]
- Richardson, R.T.; Russo, S.A.; Topley, M.T.; Chafetz, R.S.; Kozin, S.H.; Zlotolow, D.A.; Richards, J.G. Assessment of approaches to estimate scapular orientation in children with brachial plexus birth injury. Gait Posture 2022, 98, 17–23. [Google Scholar] [CrossRef]
- Abzug, J.M.; Chafetz, R.S.; Gaughan, J.P.; Ashworth, S.; Kozin, S.H. Shoulder function after medial approach and derotational humeral osteotomy in patients with brachial plexus birth palsy. J. Pediatr. Orthop. 2010, 30, 469–474. [Google Scholar] [CrossRef]
- Friesen, K.B.; Wu, L.Z.; Waslen, A.; Lang, A.E. Defining repeatability for scapulothoracic and thoracohumeral motion during the novel work-related activities and functional task (WRAFT) protocol. J. Biomech. 2023, 153, 111596. [Google Scholar] [CrossRef] [PubMed]
- Bouvier, B.; Duprey, S.; Claudon, L.; Dumas, R.; Savescu, A. Upper Limb Kinematics Using Inertial and Magnetic Sensors: Comparison of Sensor-to-Segment Calibrations. Sensors 2015, 15, 18813–18833. [Google Scholar] [CrossRef] [PubMed]
- Neer, C.S.; Craig, E.V.; Fukuda, H. Cuff-tear arthropathy. J. Bone Jt. Surg. Am. 1983, 65, 1232–1244. [Google Scholar] [CrossRef] [Green Version]
- Valevicius, A.M.; Jun, P.Y.; Hebert, J.S.; Vette, A.H. Use of optical motion capture for the analysis of normative upper body kinematics during functional upper limb tasks: A systematic review. J. Electromyogr. Kinesiol. 2018, 40, 1–15. [Google Scholar] [CrossRef]
- Bruttel, H.; Spranz, D.M.; Bülhoff, M.; Aljohani, N.; Wolf, S.I.; Maier, M.W. Comparison of glenohumeral and humerothoracical range of motion in healthy controls, osteoarthritic patients and patients after total shoulder arthroplasty performing different activities of daily living. Gait Posture 2019, 71, 20–25. [Google Scholar] [CrossRef]
- Ludewig, P.M.; Reynolds, J.F. The association of scapular kinematics and glenohumeral joint pathologies. J. Orthop. Sports Phys. Ther. 2009, 39, 90–104. [Google Scholar] [CrossRef] [Green Version]
- Longo, U.G.; Vasta, S.; Maffulli, N.; Denaro, V. Scoring systems for the functional assessment of patients with rotator cuff pathology. Sports Med. Arthrosc. Rev. 2011, 19, 310–320. [Google Scholar] [CrossRef]
- Plancher, K.D.; Lipnick, S.L. Analysis of evidence-based medicine for shoulder instability. Arthroscopy 2009, 25, 897–908. [Google Scholar] [CrossRef]
- Kirkley, A.; Griffin, S.; Dainty, K. Scoring systems for the functional assessment of the shoulder. Arthroscopy 2003, 19, 1109–1120. [Google Scholar] [CrossRef]
- Booker, S.; Alfahad, N.; Scott, M.; Gooding, B.; Wallace, W.A. Use of scoring systems for assessing and reporting the outcome results from shoulder surgery and arthroplasty. World J. Orthop. 2015, 6, 244–251. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Antonacci, C.; Longo, U.G.; Nazarian, A.; Schena, E.; Carnevale, A. Monitoring Scapular Kinematics through Wearable Magneto-Inertial Measurement Units: State of the Art and New Frontiers. Sensors 2023, 23, 6940. https://doi.org/10.3390/s23156940
Antonacci C, Longo UG, Nazarian A, Schena E, Carnevale A. Monitoring Scapular Kinematics through Wearable Magneto-Inertial Measurement Units: State of the Art and New Frontiers. Sensors. 2023; 23(15):6940. https://doi.org/10.3390/s23156940
Chicago/Turabian StyleAntonacci, Carla, Umile Giuseppe Longo, Ara Nazarian, Emiliano Schena, and Arianna Carnevale. 2023. "Monitoring Scapular Kinematics through Wearable Magneto-Inertial Measurement Units: State of the Art and New Frontiers" Sensors 23, no. 15: 6940. https://doi.org/10.3390/s23156940





