Deep Learning-Based Evaluation of Ultrasound Images for Benign Skin Tumors
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Subjects
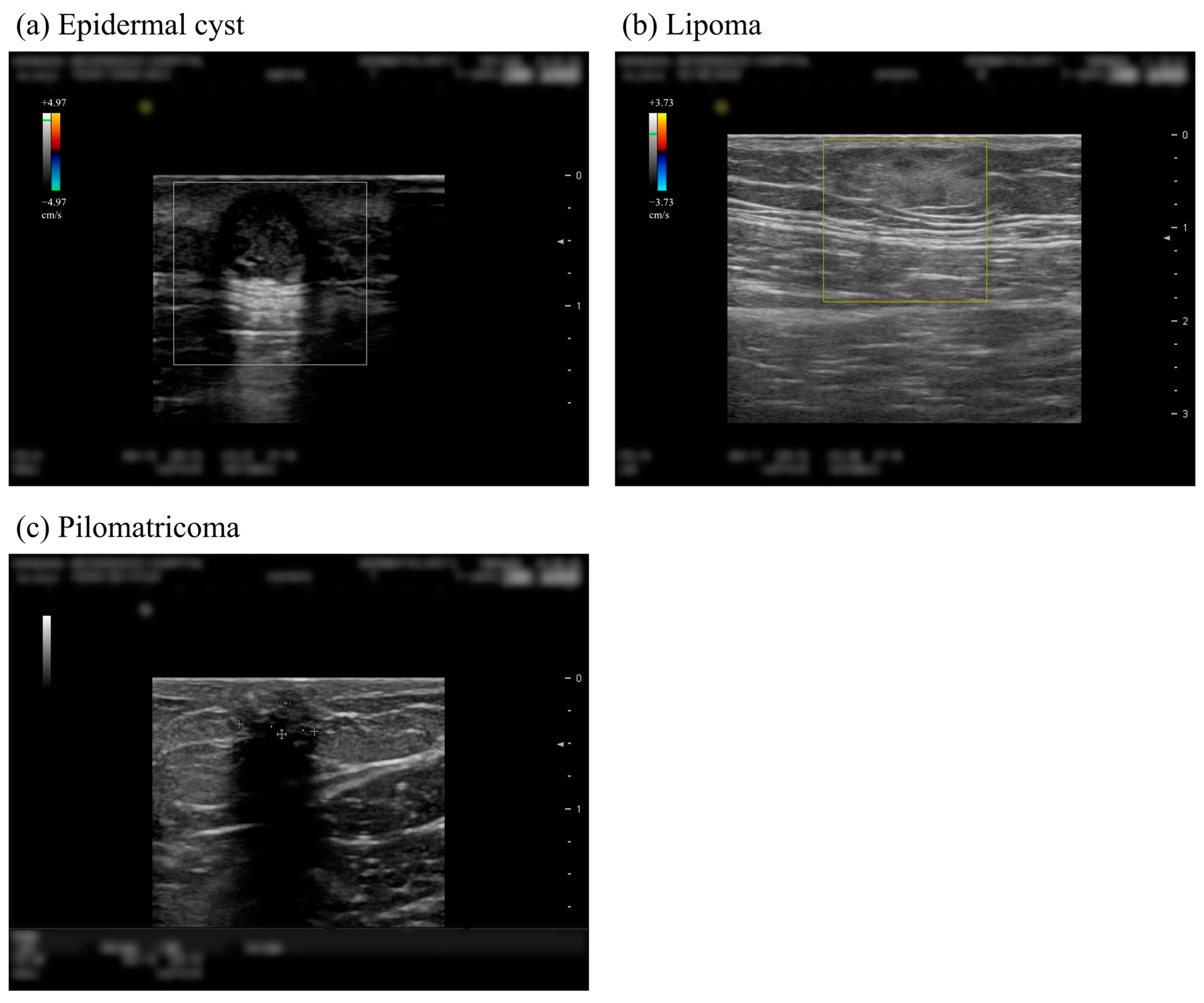
2.2. Data Preprocessing
2.3. Combined CNN Structure
2.3.1. Residual Structures
2.3.2. Attention-Gated Structures

2.4. Optimizing Combined CNN
2.4.1. Data Preparation
2.4.2. Training Details
2.5. Statistical Analysis
3. Results
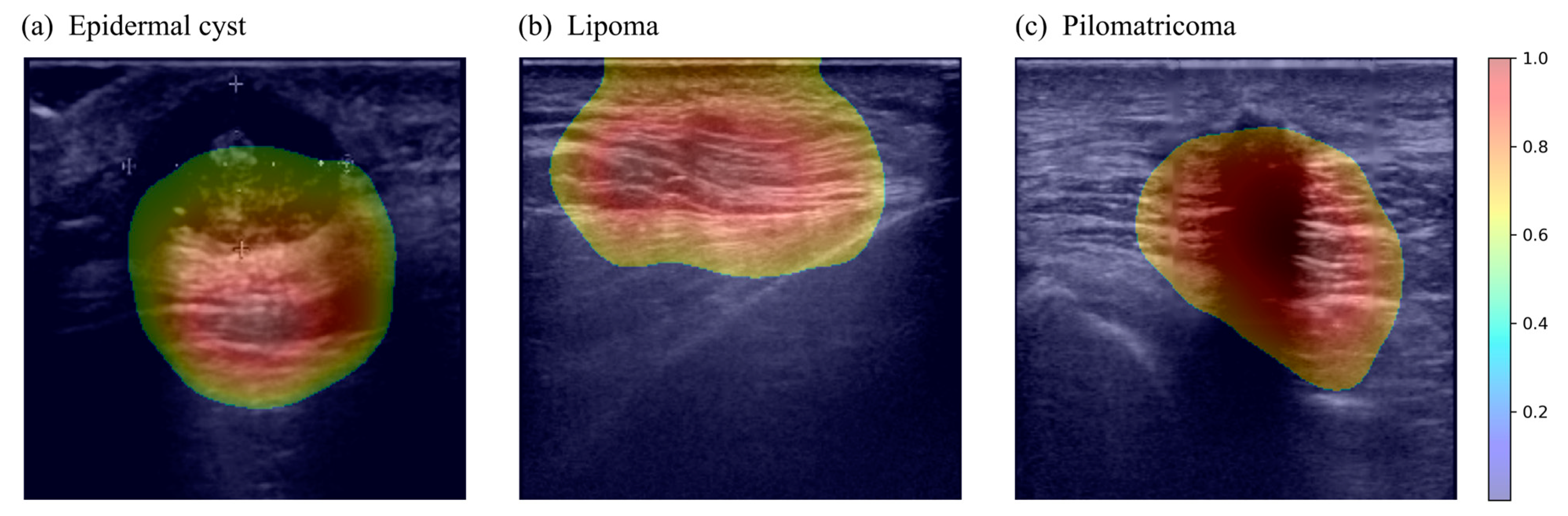
3.1. Quantitative Evaluation
3.2. Statistical Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wagner, J.M.; Lee, K.S.; Rosas, H.; Kliewer, M.A. Accuracy of sonographic diagnosis of superficial masses. J. Ultrasound Med. 2013, 32, 1443–1450. [Google Scholar] [CrossRef]
- Hwang, E.J.; Yoon, H.S.; Cho, S.; Park, H.S. The diagnostic value of ultrasonography with 5-15-MHz probes in benign subcutaneous lesions. Int. J. Dermatol. 2015, 54, e469–e475. [Google Scholar] [CrossRef]
- Levy, J.; Barrett, D.L.; Harris, N.; Jeong, J.J.; Yang, X.; Chen, S.C. High-frequency ultrasound in clinical dermatology: A review. Ultrasound J. 2021, 13, 24. [Google Scholar] [CrossRef]
- Wortsman, X. Practical applications of ultrasound in dermatology. Clin. Dermatol. 2021, 39, 605–623. [Google Scholar] [CrossRef]
- Wortsman, X. Top advances in dermatologic ultrasound. J. Ultrasound Med. 2023, 42, 521–545. [Google Scholar] [CrossRef]
- Almuhanna, N.; Wortsman, X.; Wohlmuth-Wieser, I.; Kinoshita-Ise, M.; Alhusayen, R. Overview of ultrasound imaging applications in dermatology. J. Cutan. Med. Surg. 2021, 25, 521–529. [Google Scholar] [CrossRef]
- Oh, B.H.; Kim, K.H.; Chung, K.Y. Skin imaging using ultrasound imaging, optical coherence tomography, confocal microscopy, and two-photon microscopy in cutaneous oncology. Front. Med. 2019, 6, 274. [Google Scholar] [CrossRef]
- Quien, M.M.; Saric, M. Ultrasound imaging artifacts: How to recognize them and how to avoid them. Echocardiography 2018, 35, 1388–1401. [Google Scholar] [CrossRef]
- Hoskins, P.R.; Martin, K.; Thrush, A. Diagnostic Ultrasound: Physics and Equipment; CRC Press: Boca Raton, FL, USA, 2019. [Google Scholar]
- Litjens, G.; Kooi, T.; Bejnordi, B.E.; Setio, A.A.A.; Ciompi, F.; Ghafoorian, M.; Van Der Laak, J.A.; Van Ginneken, B.; Sánchez, C.I. A survey on deep learning in medical image analysis. Med. Image Anal. 2017, 42, 60–88. [Google Scholar] [CrossRef]
- Yap, J.; Yolland, W.; Tschandl, P. Multimodal skin lesion classification using deep learning. Exp. Dermatol. 2018, 27, 1261–1267. [Google Scholar] [CrossRef]
- Li, Y.; Shen, L. Skin lesion analysis towards melanoma detection using deep learning network. Sensors 2018, 18, 556. [Google Scholar] [CrossRef]
- Harangi, B. Skin lesion classification with ensembles of deep convolutional neural networks. J. Biomed. Inform. 2018, 86, 25–32. [Google Scholar] [CrossRef]
- Majtner, T.; Yildirim-Yayilgan, S.; Hardeberg, J.Y. Combining deep learning and hand-crafted features for skin lesion classification. In Proceedings of the 2016 Sixth International Conference on Image Processing Theory, Tools and Applications (IPTA), Oulu, Finland, 12–15 December 2016; pp. 1–6. [Google Scholar]
- Yang, X.; Zeng, Z.; Yeo, S.Y.; Tan, C.; Tey, H.L.; Su, Y. A novel multi-task deep learning model for skin lesion segmentation and classification. arXiv 2017, arXiv:1703.01025. [Google Scholar]
- Premaladha, J.; Ravichandran, K. Novel approaches for diagnosing melanoma skin lesions through supervised and deep learning algorithms. J. Med. Syst. 2016, 40, 96. [Google Scholar] [CrossRef]
- Czajkowska, J.; Juszczyk, J.; Piejko, L.; Glenc-Ambroży, M. High-frequency ultrasound dataset for deep learning-based image quality assessment. Sensors 2022, 22, 1478. [Google Scholar] [CrossRef]
- Bandari, E.; Beuzen, T.; Habashy, L.; Raza, J.; Yang, X.; Kapeluto, J.; Meneilly, G.; Madden, K. Machine Learning Decision Support for Detecting Lipohypertrophy with Bedside Ultrasound: Proof-of-Concept Study. JMIR Form. Res. 2022, 6, e34830. [Google Scholar] [CrossRef]
- Kang, S. Fitzpatrick’s Dermatology, 2-Volume Set (Fitzpatricks Dermatology in General Medicine); McGraw Hill: New York, NY, USA, 2019. [Google Scholar]
- Oh, B.H.; Seo, J.; Chung, K.Y. Surgical treatment of 846 patients with benign skin tumors: Experience of a dermatologic surgeon in Korea. Korean J. Dermatol. 2015, 53, 202–208. [Google Scholar]
- Zhou, B.; Khosla, A.; Lapedriza, A.; Oliva, A.; Torralba, A. Learning deep features for discriminative localization. In Proceedings of the IEEE Conference on Computer Vision and Pattern Recognition, Las Vegas, NV, USA, 27–30 June 2016; pp. 2921–2929. [Google Scholar]
- Telea, A. An image inpainting technique based on the fast marching method. J. Graph. Tools 2004, 9, 23–34. [Google Scholar] [CrossRef]
- Lim, S.; Kim, I.; Kim, T.; Kim, C.; Kim, S. Fast autoaugment. arXiv 2019, arXiv:1905.00397. [Google Scholar]
- He, K.; Zhang, X.; Ren, S.; Sun, J. Deep residual learning for image recognition. In Proceedings of the IEEE Conference on Computer Vision and Pattern Recognition, Las Vegas, NV, USA, 27–30 June 2016; pp. 770–778. [Google Scholar]
- Schlemper, J.; Oktay, O.; Chen, L.; Matthew, J.; Knight, C.; Kainz, B.; Glocker, B.; Rueckert, D. Attention-gated networks for improving ultrasound scan plane detection. arXiv 2018, arXiv:1804.05338. [Google Scholar]
- Kingma, D.P.; Ba, J. Adam: A method for stochastic optimization. arXiv 2014, arXiv:1412.6980. [Google Scholar]
- Wortsman, X. Common applications of dermatologic sonography. J. Ultrasound Med. 2012, 31, 97–111. [Google Scholar] [CrossRef]
- Lee, H.S.; Joo, K.B.; Song, H.T.; Kim, Y.S.; Park, D.W.; Park, C.K.; Lee, W.M.; Park, Y.W.; Koo, J.H.; Song, S.Y. Relationship between sonographic and pathologic findings in epidermal inclusion cysts. J. Clin. Ultrasound 2001, 29, 374–383. [Google Scholar] [CrossRef] [PubMed]
- Wortsman, X.; Jemec, G. Dermatologic Ultrasound with Clinical and Histologic Correlations; Springer New York: New York, NY, USA, 2013. [Google Scholar]
- Chen, C.Y.; Chiou, H.J.; Chou, S.Y.; Chiou, S.Y.; Wang, H.K.; Chou, Y.H.; Chiang, H.K. Computer-aided diagnosis of soft-tissue tumors using sonographic morphologic and texture features. Acad. Radiol. 2009, 16, 1531–1538. [Google Scholar] [CrossRef] [PubMed]
- Chu, Y.S.; An, H.G.; Oh, B.H.; Yang, S. Artificial Intelligence in Cutaneous Oncology. Front. Med. 2020, 7, 318. [Google Scholar] [CrossRef] [PubMed]
- Cullell-Dalmau, M.; Noé, S.; Otero-Viñas, M.; Meić, I.; Manzo, C. Convolutional neural network for skin lesion classification: Understanding the fundamentals through hands-on learning. Front. Med. 2021, 8, 644327. [Google Scholar] [CrossRef]
- Wells, A.; Patel, S.; Lee, J.B.; Motaparthi, K. Artificial intelligence in dermatopathology: Diagnosis, education, and research. J. Cutan. Pathol. 2021, 48, 1061–1068. [Google Scholar] [CrossRef]
- Haggenmüller, S.; Maron, R.C.; Hekler, A.; Utikal, J.S.; Barata, C.; Barnhill, R.L.; Beltraminelli, H.; Berking, C.; Betz-Stablein, B.; Blum, A. Skin cancer classification via convolutional neural networks: Systematic review of studies involving human experts. Eur. J. Cancer 2021, 156, 202–216. [Google Scholar] [CrossRef]
- Ba, W.; Wu, H.; Chen, W.W.; Wang, S.H.; Zhang, Z.Y.; Wei, X.J.; Wang, W.J.; Yang, L.; Zhou, D.M.; Zhuang, Y.X. Convolutional neural network assistance significantly improves dermatologists’ diagnosis of cutaneous tumours using clinical images. Eur. J. Cancer 2022, 169, 156–165. [Google Scholar] [CrossRef]
- Aggarwal, P.; Choi, J.; Sutaria, N.; Roh, Y.; Wongvibulsin, S.; Williams, K.; Huang, A.; Boozalis, E.; Le, T.; Chavda, R. Clinical characteristics and disease burden in prurigo nodularis. Clin. Exp. Dermatol. 2021, 46, 1277–1284. [Google Scholar] [CrossRef]
- Jartarkar, S.R. Artificial intelligence: Its role in dermatopathology. Indian J. Dermatol. Venereol. Leprol. 2023, 89, 549–552. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Chu, Y.S.; Yoo, S.K.; Choi, S.; Choe, S.J.; Koh, S.B.; Chung, K.Y.; Xing, L.; Oh, B.; Yang, S. Augmented decision-making for acral lentiginous melanoma detection using deep convolutional neural networks. J. Eur. Acad. Dermatol. Venereol. 2020, 34, 1842–1850. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Wang, J.; Xie, F.; Liu, J.; Shu, C.; Wang, Y.; Zheng, Y.; Zhang, H. A convolutional neural network trained with dermoscopic images of psoriasis performed on par with 230 dermatologists. Comput. Biol. Med. 2021, 139, 104924. [Google Scholar] [CrossRef]
- Kwiatkowska, D.; Kluska, P.; Reich, A. Convolutional neural networks for the detection of malignant melanoma in dermoscopy images. Adv. Dermatol. Allergol. /Postępy Dermatol. I Alergol. 2021, 38, 412–420. [Google Scholar] [CrossRef] [PubMed]
- Zhao, W.; Kang, Q.; Qian, F.; Li, K.; Zhu, J.; Ma, B. Convolutional neural network-based computer-assisted diagnosis of Hashimoto’s thyroiditis on ultrasound. J. Clin. Endocrinol. Metab. 2022, 107, 953–963. [Google Scholar] [CrossRef]
- Hu, L.; Pei, C.; Xie, L.; Liu, Z.; He, N.; Lv, W. Convolutional Neural Network for predicting thyroid cancer based on ultrasound elastography image of perinodular region. Endocrinology 2022, 163, bqac135. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.N.; Podkowa, A.S.; Park, T.H.; Miller, R.J.; Do, M.N.; Oelze, M.L. Use of a convolutional neural network and quantitative ultrasound for diagnosis of fatty liver. Ultrasound Med. Biol. 2021, 47, 556–568. [Google Scholar] [CrossRef]
- Liu, J.; Li, W.; Zhao, N.; Cao, K.; Yin, Y.; Song, Q.; Chen, H.; Gong, X. Integrate domain knowledge in training CNN for ultrasonography breast cancer diagnosis. In Proceedings of the International Conference on Medical Image Computing and Computer-Assisted Intervention, Granada, Spain, 16–20 September 2018; pp. 868–875. [Google Scholar]
- Zhou, B.-Y.; Wang, L.-F.; Yin, H.-H.; Wu, T.-F.; Ren, T.-T.; Peng, C.; Li, D.-X.; Shi, H.; Sun, L.-P.; Zhao, C.-K. Decoding the molecular subtypes of breast cancer seen on multimodal ultrasound images using an assembled convolutional neural network model: A prospective and multicentre study. eBiomedicine 2021, 74, 103684. [Google Scholar] [CrossRef]
- Lee, J.H.; Baek, J.H.; Kim, J.H.; Shim, W.H.; Chung, S.R.; Choi, Y.J.; Lee, J.H. Deep Learning–Based Computer-Aided Diagnosis System for Localization and Diagnosis of Metastatic Lymph Nodes on Ultrasound: A Pilot Study. Thyroid 2018, 28, 1332–1338. [Google Scholar] [CrossRef]
- Xie, B.; Lei, T.; Wang, N.; Cai, H.; Xian, J.; He, M.; Zhang, L.; Xie, H. Computer-aided diagnosis for fetal brain ultrasound images using deep convolutional neural networks. Int. J. Comput. Assist. Radiol. Surg. 2020, 15, 1303–1312. [Google Scholar] [CrossRef]
- Born, J.; Wiedemann, N.; Brändle, G.; Buhre, C.; Rieck, B.; Borgwardt, K. Accelerating COVID-19 differential diagnosis with explainable ultrasound image analysis. arXiv 2020, arXiv:2009.06116. [Google Scholar]
- Schneider, S.L.; Kohli, I.; Hamzavi, I.H.; Council, M.L.; Rossi, A.M.; Ozog, D.M. Emerging imaging technologies in dermatology: Part II: Applications and limitations. J. Am. Acad. Dermatol. 2019, 80, 1121–1131. [Google Scholar] [CrossRef] [PubMed]


| Dataset | Total No. of Images | Images, No. (%) | ||
|---|---|---|---|---|
| (Augmented a) | Epidermal Cyst | Lipoma | Pilomatricoma | |
| 1st fold | ||||
| Training set | 548 (11,508) | 310 (56.6) | 183 (33.4) | 55 (10.0) |
| Test set | 150 | 76 (50.7) | 49 (32.7) | 25 (16.7) |
| 2nd fold | ||||
| Training set | 544 (11,424) | 311 (57.2) | 165 (30.3) | 68 (12.5) |
| Test set | 154 | 75 (48.7) | 67 (43.5) | 12 (7.8) |
| 3rd fold | ||||
| Training set | 579 (12,159) | 317 (54.7) | 198 (34.2) | 64 (11.1) |
| Test set | 119 | 69 (58.0) | 34 (28.6) | 16 (13.4) |
| 4th fold | ||||
| Training set | 558 (11,718) | 322 (57.7) | 177 (31.7) | 59 (10.6) |
| Test set | 140 | 64 (45.7) | 55 (39.2) | 21 (15.0) |
| 5th fold | ||||
| Training set | 558 (11,718) | 301 (53.9) | 207 (37.1) | 50 (9.0) |
| Test set | 140 | 85 (60.7) | 25 (17.9) | 30 (21.4) |
| Tumor Types | Accuracy, % Mean a (95% CI b) | AUROC, Mean a (95% CI b) | F1 Score, Mean a (95% CI b) | Sensitivity, Mean a (95% CI b) | Specificity, Mean a (95% CI b) |
|---|---|---|---|---|---|
| Epidermal cyst | 94.9 (91.3–98.5) | 0.962 (0.931–0.993) | 95.5 (93.2–97.9) | 97.9 (95.4–100.0) | 92.4 (84.5–100.0) |
| Lipoma | 98.2 (95.7–100.0) | 0.996 (0.986–1.000) | 97.6 (94.7–100.0) | 96.5 (91.7–100.0) | 98.9 (97.4–100.0) |
| Pilomatricoma | 94.5 (90.6–98.4) | 0.905 (0.804–1.000) | 78.8 (63.3–94.3) | 75.9 (50.6–100.0) | 97.4 (94.4–100.0) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, H.; Lee, Y.; Jung, S.-W.; Lee, S.; Oh, B.; Yang, S. Deep Learning-Based Evaluation of Ultrasound Images for Benign Skin Tumors. Sensors 2023, 23, 7374. https://doi.org/10.3390/s23177374
Lee H, Lee Y, Jung S-W, Lee S, Oh B, Yang S. Deep Learning-Based Evaluation of Ultrasound Images for Benign Skin Tumors. Sensors. 2023; 23(17):7374. https://doi.org/10.3390/s23177374
Chicago/Turabian StyleLee, Hyunwoo, Yerin Lee, Seung-Won Jung, Solam Lee, Byungho Oh, and Sejung Yang. 2023. "Deep Learning-Based Evaluation of Ultrasound Images for Benign Skin Tumors" Sensors 23, no. 17: 7374. https://doi.org/10.3390/s23177374






