Quantitative Gait Feature Assessment on Two-Dimensional Body Axis Projection Planes Converted from Three-Dimensional Coordinates Estimated with a Deep Learning Smartphone App
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethical Approvals
2.2. Study Population
2.3. Data Acquisition of Estimated Three-Dimensional Relative Coordinates
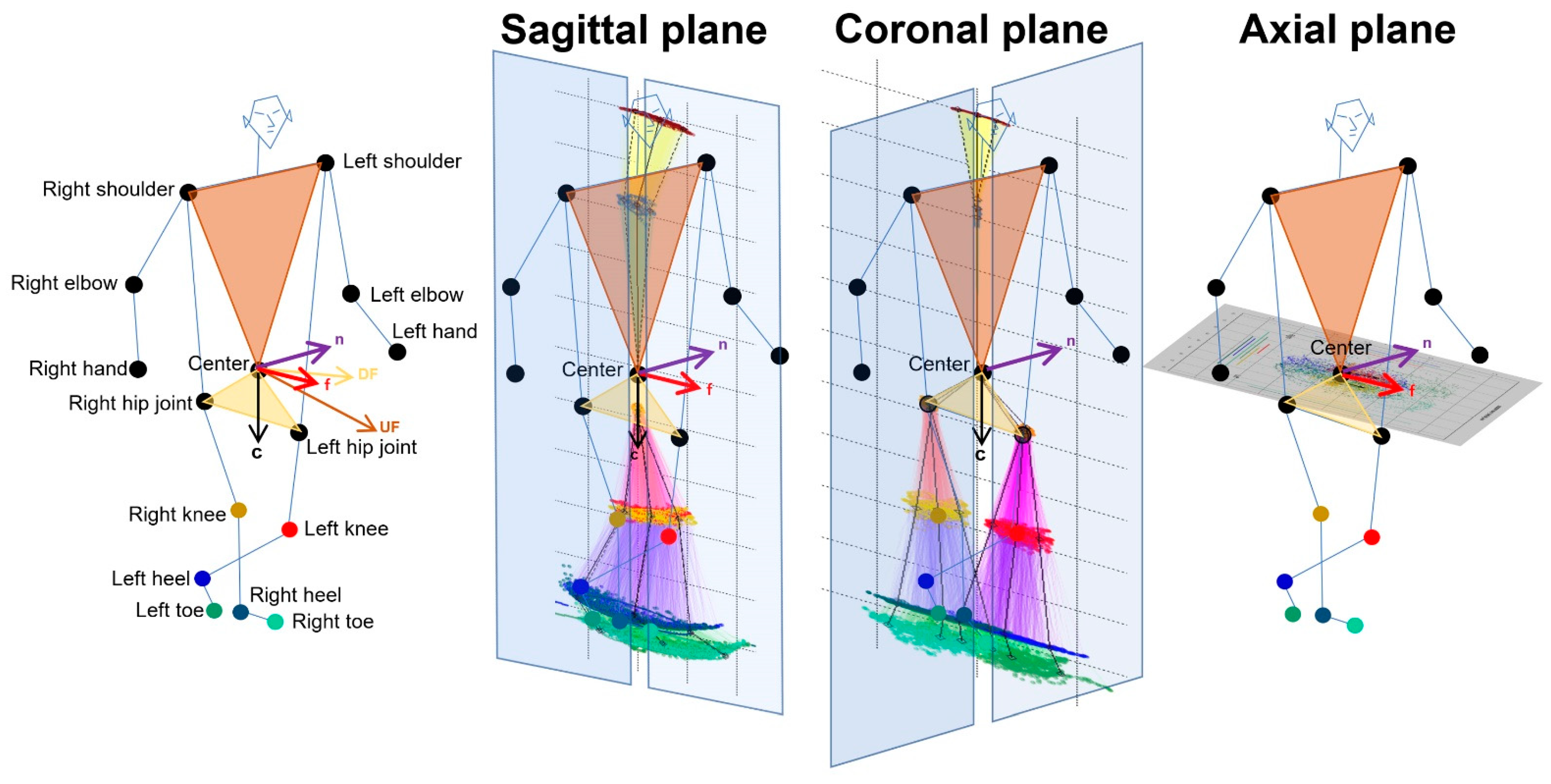
2.4. Projection of Relative Coordinates on the Body Axis Planes
2.5. Data Processing for Gait Analysis
2.6. Statistical Analysis
3. Results
3.1. Clinical Characteristics
3.2. Two-Dimensional Relative Coordinates on the Sagittal and Axial Projection Planes
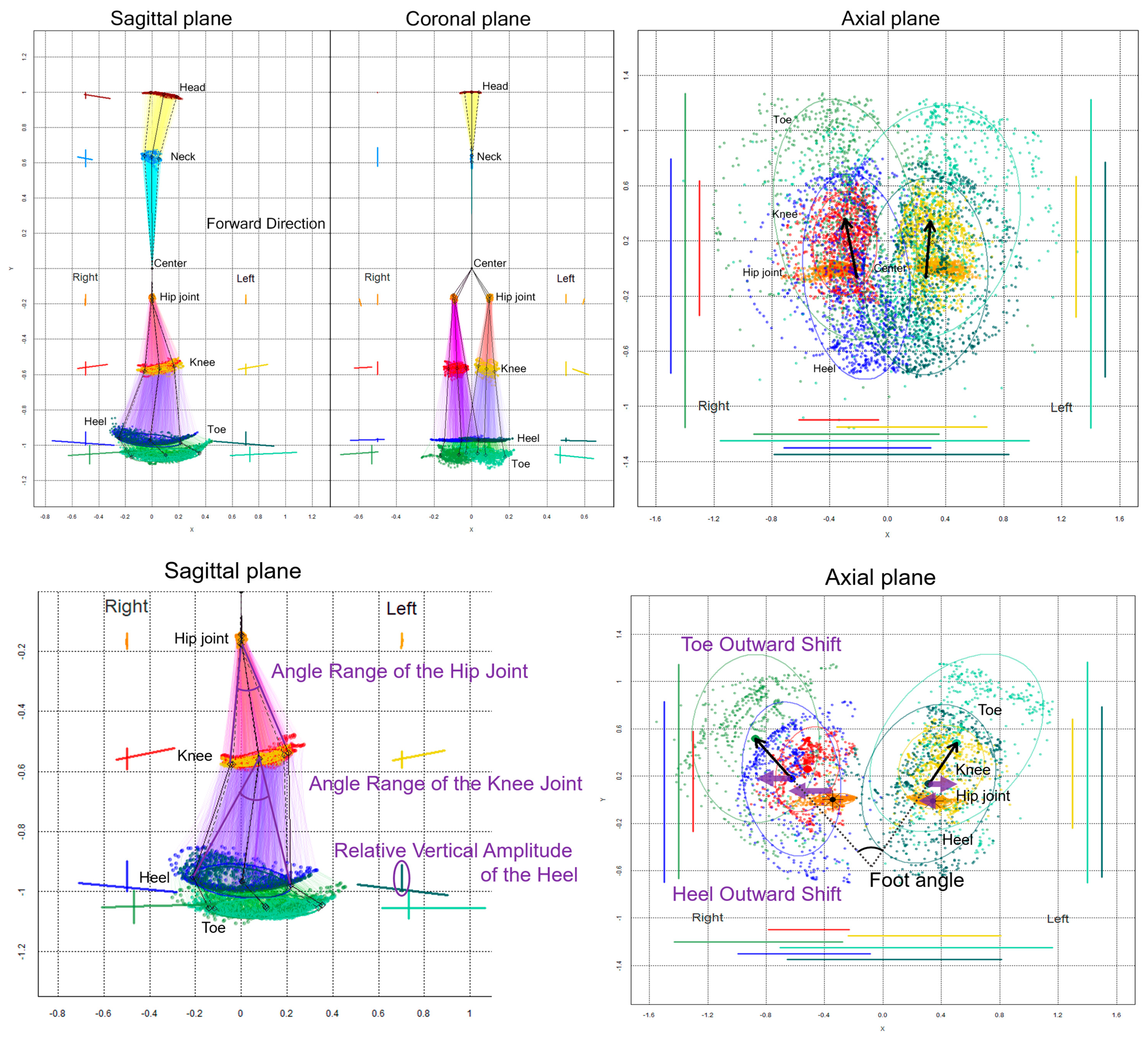
3.2.1. Sagittal Projection Plane
3.2.2. Axial Projection Plane
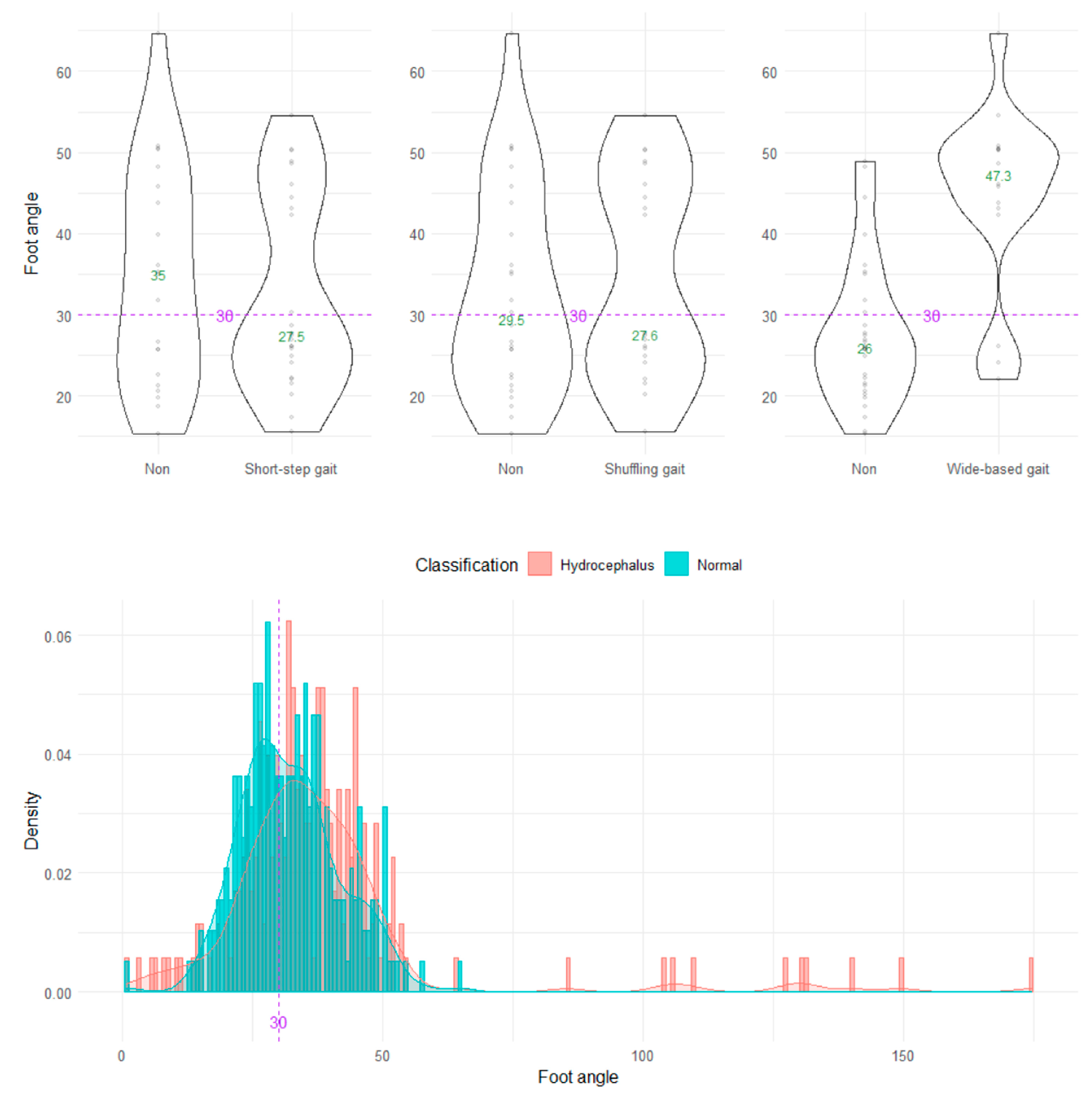
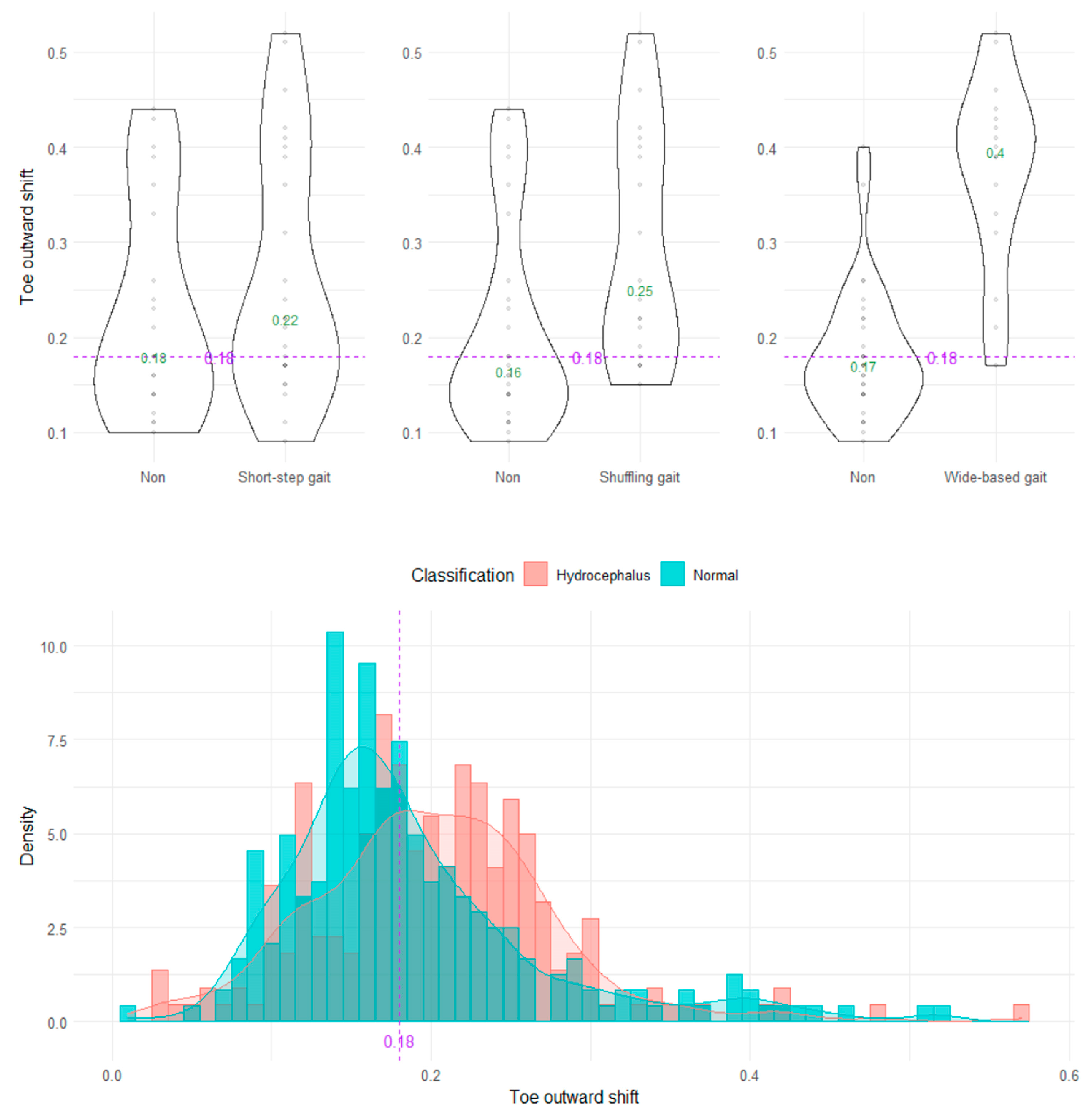
3.3. Discrimination of Pathological Gaits by Indices on 2D Projection Planes Using the TDPT-GT App
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gor-García-Fogeda, M.D.; Cano de la Cuerda, R.; Carratalá Tejada, M.; Alguacil-Diego, I.M.; Molina-Rueda, F. Observational gait assessments in people with neurological disorders: A systematic review. Arch. Phys. Med. Rehabil. 2016, 97, 131–140. [Google Scholar] [CrossRef]
- Ishikawa, M.; Yamada, S.; Yamamoto, K. Agreement study on gait assessment using a video-assisted rating method in patients with idiopathic normal-pressure hydrocephalus. PLoS ONE 2019, 14, e0224202. [Google Scholar] [CrossRef]
- Marmarou, A.; Bergsneider, M.; Relkin, N.; Klinge, P.; Black, P.M. Development of guidelines for idiopathic normal-pressure hydrocephalus: Introduction. Neurosurgery 2005, 57, S1–S3. [Google Scholar] [CrossRef] [Green Version]
- Nakajima, M.; Yamada, S.; Miyajima, M.; Ishii, K.; Kuriyama, N.; Kazui, H.; Kanemoto, H.; Suehiro, T.; Yoshiyama, K.; Kameda, M.; et al. Guidelines for Management of Idiopathic Normal Pressure Hydrocephalus (Third Edition): Endorsed by the Japanese Society of Normal Pressure Hydrocephalus. Neurol. Med.-Chir. 2021, 61, 63–97. [Google Scholar] [CrossRef] [PubMed]
- Scully, A.E.; Lim, E.C.W.; Teow, P.P.; Tan, D.M.L. A systematic review of the diagnostic utility of simple tests of change after trial removal of cerebrospinal fluid in adults with normal pressure hydrocephalus. Clin. Rehabil. 2018, 32, 942–953. [Google Scholar] [CrossRef] [PubMed]
- Stolze, H.; Kuhtz-Buschbeck, J.P.; Drücke, H.; Jöhnk, K.; Diercks, C.; Palmié, S.; Mehdorn, H.M.; Illert, M.; Deuschl, G. Gait analysis in idiopathic normal pressure hydrocephalus--Which parameters respond to the CSF tap test? Clin. Neurophysiol. 2000, 111, 1678–1686. [Google Scholar] [CrossRef] [PubMed]
- Hausdorff, J.M. Gait dynamics, fractals and falls: Finding meaning in the stride-to-stride fluctuations of human walking. Hum. Mov. Sci. 2007, 26, 555–589. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kitade, I.; Kitai, R.; Neishi, H.; Kikuta, K.I.; Shimada, S.; Matsumine, A. Relationship between gait parameters and MR imaging in idiopathic normal pressure hydrocephalus patients after shunt surgery. Gait Posture 2018, 61, 163–168. [Google Scholar] [CrossRef]
- Murray, M.P.; Sepic, S.B.; Gardner, G.M.; Downs, W.J. Walking patterns of men with parkinsonism. Am. J. Phys. Med. 1978, 57, 278–294. [Google Scholar]
- Panciani, P.P.; Migliorati, K.; Muratori, A.; Gelmini, M.; Padovani, A.; Fontanella, M. Computerized gait analysis with inertial sensor in the management of idiopathic normal pressure hydrocephalus. Eur. J. Phys. Rehabil. Med. 2018, 54, 724–729. [Google Scholar] [CrossRef]
- Williams, M.A.; Thomas, G.; de Lateur, B.; Imteyaz, H.; Rose, J.G.; Shore, W.S.; Kharkar, S.; Rigamonti, D. Objective assessment of gait in normal-pressure hydrocephalus. Am. J. Phys. Med. Rehabil. 2008, 87, 39–45. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Li, Y.; Xiong, F.; Zhang, W. Gait recognition using optical motion capture: A decision fusion based method. Sensors 2021, 21, 3496. [Google Scholar] [CrossRef] [PubMed]
- Hsu, A.L.; Tang, P.F.; Jan, M.H. Analysis of impairments influencing gait velocity and asymmetry of hemiplegic patients after mild to moderate stroke. Arch. Phys. Med. Rehabil. 2003, 84, 1185–1193. [Google Scholar] [CrossRef] [PubMed]
- Patterson, K.K.; Parafianowicz, I.; Danells, C.J.; Closson, V.; Verrier, M.C.; Staines, W.R.; Black, S.E.; McIlroy, W.E. Gait asymmetry in community-ambulating stroke survivors. Arch. Phys. Med. Rehabil. 2008, 89, 304–310. [Google Scholar] [CrossRef]
- Serrao, M.; Pierelli, F.; Ranavolo, A.; Draicchio, F.; Conte, C.; Don, R.; Di Fabio, R.; LeRose, M.; Padua, L.; Sandrini, G.; et al. Gait pattern in inherited cerebellar ataxias. Cerebellum 2012, 11, 194–211. [Google Scholar] [CrossRef]
- Yamada, S.; Aoyagi, Y.; Ishikawa, M.; Yamaguchi, M.; Yamamoto, K.; Nozaki, K. Gait assessment using three-dimensional acceleration of the trunk in idiopathic normal pressure hydrocephalus. Front. Aging Neurosci. 2021, 13, 653964. [Google Scholar] [CrossRef]
- Tsuchida, W.; Kobayashi, Y.; Inoue, K.; Horie, M.; Yoshihara, K.; Ooie, T. Kinematic characteristics during gait in frail older women identified by principal component analysis. Sci. Rep. 2022, 12, 1676. [Google Scholar] [CrossRef]
- Kobayashi, Y.; Hobara, H.; Matsushita, S.; Mochimaru, M. Key joint kinematic characteristics of the gait of fallers identified by principal component analysis. J. Biomech. 2014, 47, 2424–2429. [Google Scholar] [CrossRef]
- Kobayashi, Y.; Hobara, H.; Heldoorn, T.A.; Kouchi, M.; Mochimaru, M. Age-independent and age-dependent sex differences in gait pattern determined by principal component analysis. Gait Posture 2016, 46, 11–17. [Google Scholar] [CrossRef]
- Kobayashi, Y.; Ogata, T. Association between the gait pattern characteristics of older people and their two-step test scores. BMC Geriatr 2018, 18, 101. [Google Scholar] [CrossRef]
- Aoyagi, Y.; Yamada, S.; Ueda, S.; Iseki, C.; Kondo, T.; Mori, K.; Kobayashi, Y.; Fukami, T.; Hoshimaru, M.; Ishikawa, M.; et al. Development of smartphone application for markerless three-dimensional motion capture based on deep learning model. Sensors 2022, 22, 5282. [Google Scholar] [CrossRef] [PubMed]
- Iseki, C.; Kawanami, T.; Nagasawa, H.; Wada, M.; Koyama, S.; Kikuchi, K.; Arawaka, S.; Kurita, K.; Daimon, M.; Mori, E.; et al. Asymptomatic ventriculomegaly with features of idiopathic normal pressure hydrocephalus on MRI (AVIM) in the elderly: A prospective study in a Japanese population. J. Neurol. Sci. 2009, 277, 54–57. [Google Scholar] [CrossRef]
- Iseki, C.; Takahashi, Y.; Wada, M.; Kawanami, T.; Adachi, M.; Kato, T. Incidence of idiopathic normal pressure hydrocephalus (iNPH): A 10-year follow-up study of a rural community in Japan. J. Neurol. Sci. 2014, 339, 108–112. [Google Scholar] [CrossRef] [PubMed]
- Iseki, C.; Takahashi, Y.; Adachi, M.; Igari, R.; Sato, H.; Koyama, S.; Ishizawa, K.; Ohta, Y.; Kato, T. Prevalence and development of idiopathic normal pressure hydrocephalus: A 16-year longitudinal study in Japan. Acta Neurol. Scand. 2022, 146, 680–689. [Google Scholar] [CrossRef]
- Arvin, M.; Mazaheri, M.; Hoozemans, M.J.M.; Pijnappels, M.; Burger, B.J.; Verschueren, S.M.P.; van Dieën, J.H. Effects of narrow base gait on mediolateral balance control in young and older adults. J. Biomech. 2016, 49, 1264–1267. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hernández, A.; Silder, A.; Heiderscheit, B.C.; Thelen, D.G. Effect of age on center of mass motion during human walking. Gait Posture 2009, 30, 217–222. [Google Scholar] [CrossRef] [Green Version]
- Hurt, C.P.; Rosenblatt, N.; Crenshaw, J.R.; Grabiner, M.D. Variation in trunk kinematics influences variation in step width during treadmill walking by older and younger adults. Gait Posture 2010, 31, 461–464. [Google Scholar] [CrossRef]





| Primary Healthy Volunteer | Takahata Cohort | iNPH Patient | |
|---|---|---|---|
| Total Number | 15 | 92 | 47 |
| Sex (male:female) | 9:6 | 36:56 | 32:15 |
| Mean ± SD 1 of age (years) | 39.1 ± 20.1 | 73.0 ± 6.3 | 77.3 ± 6.3 |
| Range of age (years) | 22–78 | 60–91 | 61–87 |
| Shuffling gait | 0 | 0 | 26 |
| Short-stepped gait | 0 | 0 | 38 |
| Wide-based gait | 0 | 0 | 35 |
| Freezing gait | 0 | 0 | 8 |
| Spastic gait | 0 | 0 | 2 |
| Instability | 0 | 0 | 41 |
| Alzheimer’s disease | 0 | 0 | 4 |
| Fall history | 0 | 19 | 30 |
| Cutoff Value | AUC * (95% CI) ” | Sensitivity | Specificity | OD # (95% CI) ” | |
|---|---|---|---|---|---|
| Shuffling gait | |||||
| Angle range of the hip joint (°) | 30 | 77.1 (72.0–82.2) | 69.0 | 74.3 | 6.39 (3.90–10.64) |
| Angle range of the knee joint (°) | 45 | 78.6 (73.7–83.4) | 52.6 | 87.5 | 7.71 (4.54–13.28) |
| Relative vertical amplitude of the heel | 0.1 | 71.7 (66.3–77.2) | 59.5 | 76.0 | 4.64 (2.87–7.57) |
| Short-stepped gait | |||||
| Angle range of the knee joint (°) | 45 | 81.7 (77.4–86.0) | 43.0 | 93.4 | 10.55 (5.63–21.12) |
| Short-stepped gait | |||||
| Heel outward shift | −0.08 | 78.1 (73.6–82.5) | 81.4 | 60.9 | 3.36 (2.16–5.27) |
| Toe outward shift | 0.18 | 69.8 (64.6–75.0) | 70.2 | 58.8 | 6.77 (4.15–11.30) |
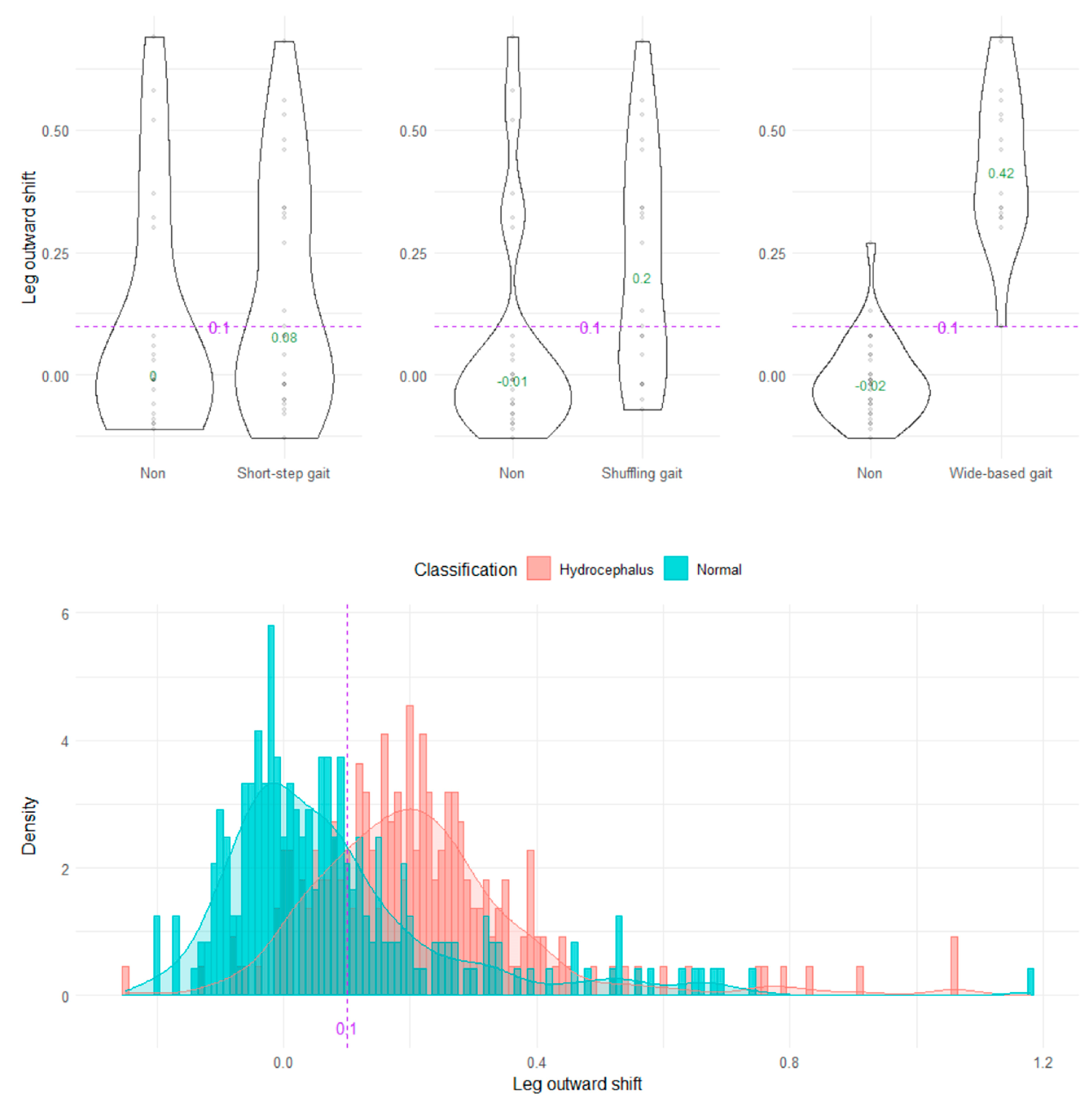
| Leg outward shift | 0.1 | 80.6 (76.4–84.8) | 81.4 | 63.8 | 7.65 (4.68–12.80) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yamada, S.; Aoyagi, Y.; Iseki, C.; Kondo, T.; Kobayashi, Y.; Ueda, S.; Mori, K.; Fukami, T.; Tanikawa, M.; Mase, M.; et al. Quantitative Gait Feature Assessment on Two-Dimensional Body Axis Projection Planes Converted from Three-Dimensional Coordinates Estimated with a Deep Learning Smartphone App. Sensors 2023, 23, 617. https://doi.org/10.3390/s23020617
Yamada S, Aoyagi Y, Iseki C, Kondo T, Kobayashi Y, Ueda S, Mori K, Fukami T, Tanikawa M, Mase M, et al. Quantitative Gait Feature Assessment on Two-Dimensional Body Axis Projection Planes Converted from Three-Dimensional Coordinates Estimated with a Deep Learning Smartphone App. Sensors. 2023; 23(2):617. https://doi.org/10.3390/s23020617
Chicago/Turabian StyleYamada, Shigeki, Yukihiko Aoyagi, Chifumi Iseki, Toshiyuki Kondo, Yoshiyuki Kobayashi, Shigeo Ueda, Keisuke Mori, Tadanori Fukami, Motoki Tanikawa, Mitsuhito Mase, and et al. 2023. "Quantitative Gait Feature Assessment on Two-Dimensional Body Axis Projection Planes Converted from Three-Dimensional Coordinates Estimated with a Deep Learning Smartphone App" Sensors 23, no. 2: 617. https://doi.org/10.3390/s23020617
APA StyleYamada, S., Aoyagi, Y., Iseki, C., Kondo, T., Kobayashi, Y., Ueda, S., Mori, K., Fukami, T., Tanikawa, M., Mase, M., Hoshimaru, M., Ishikawa, M., & Ohta, Y. (2023). Quantitative Gait Feature Assessment on Two-Dimensional Body Axis Projection Planes Converted from Three-Dimensional Coordinates Estimated with a Deep Learning Smartphone App. Sensors, 23(2), 617. https://doi.org/10.3390/s23020617










