Changes in Electromyographic Activity of the Dominant Arm Muscles during Forehand Stroke Phases in Wheelchair Tennis
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
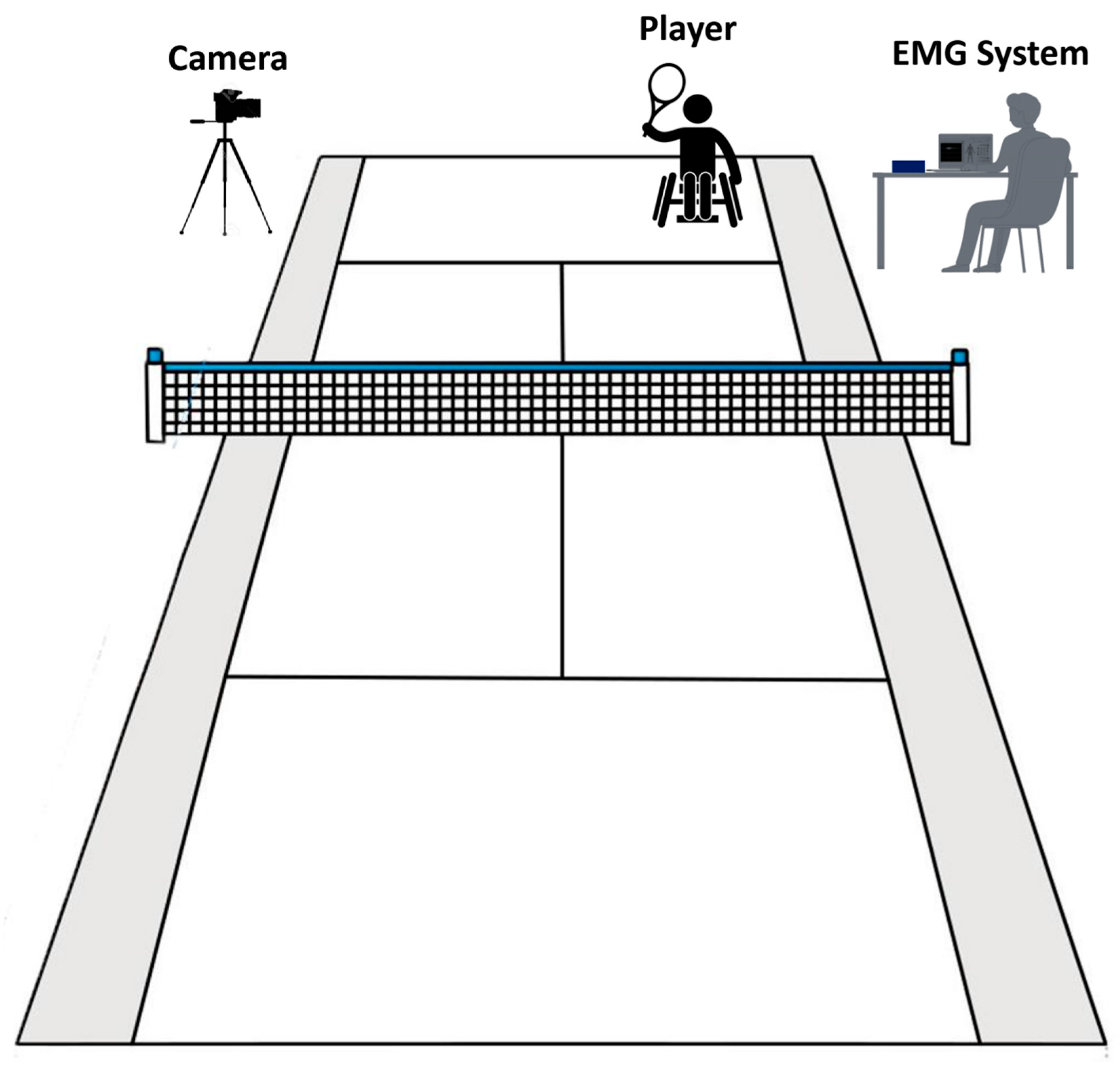
2.2. Study Design
2.3. Experiment Protocol
2.4. Data Recording
2.5. Statistical Analysis
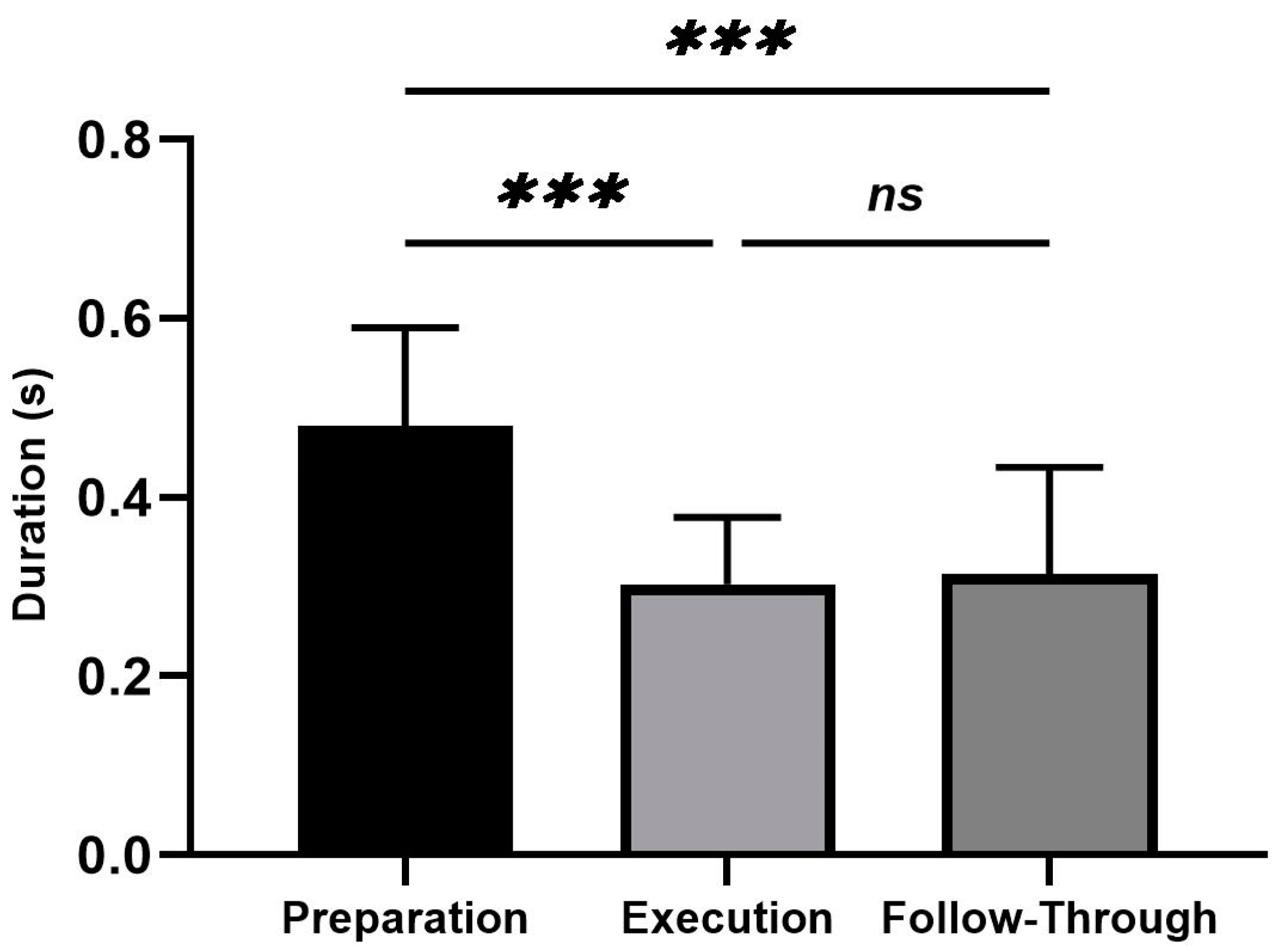
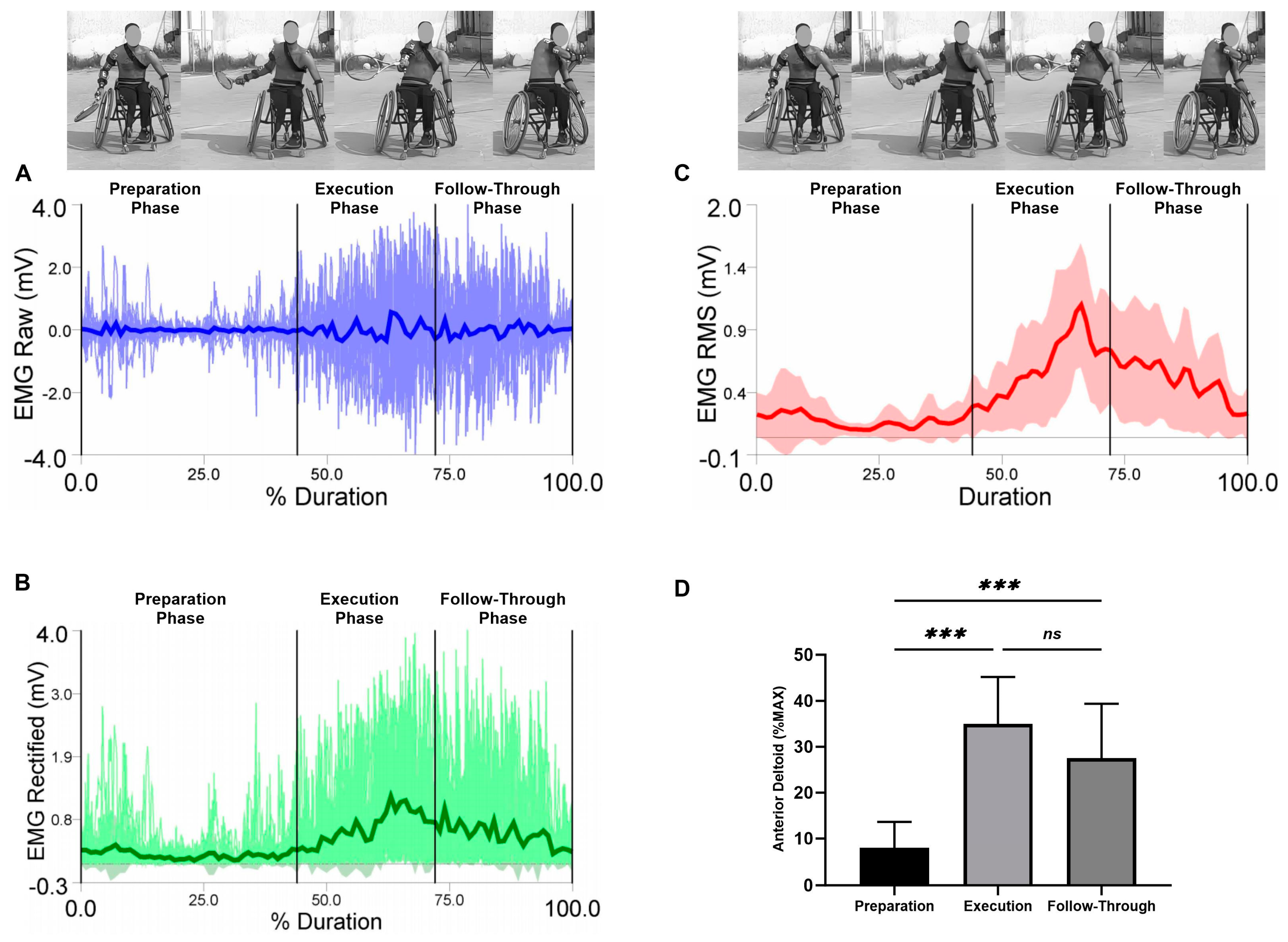
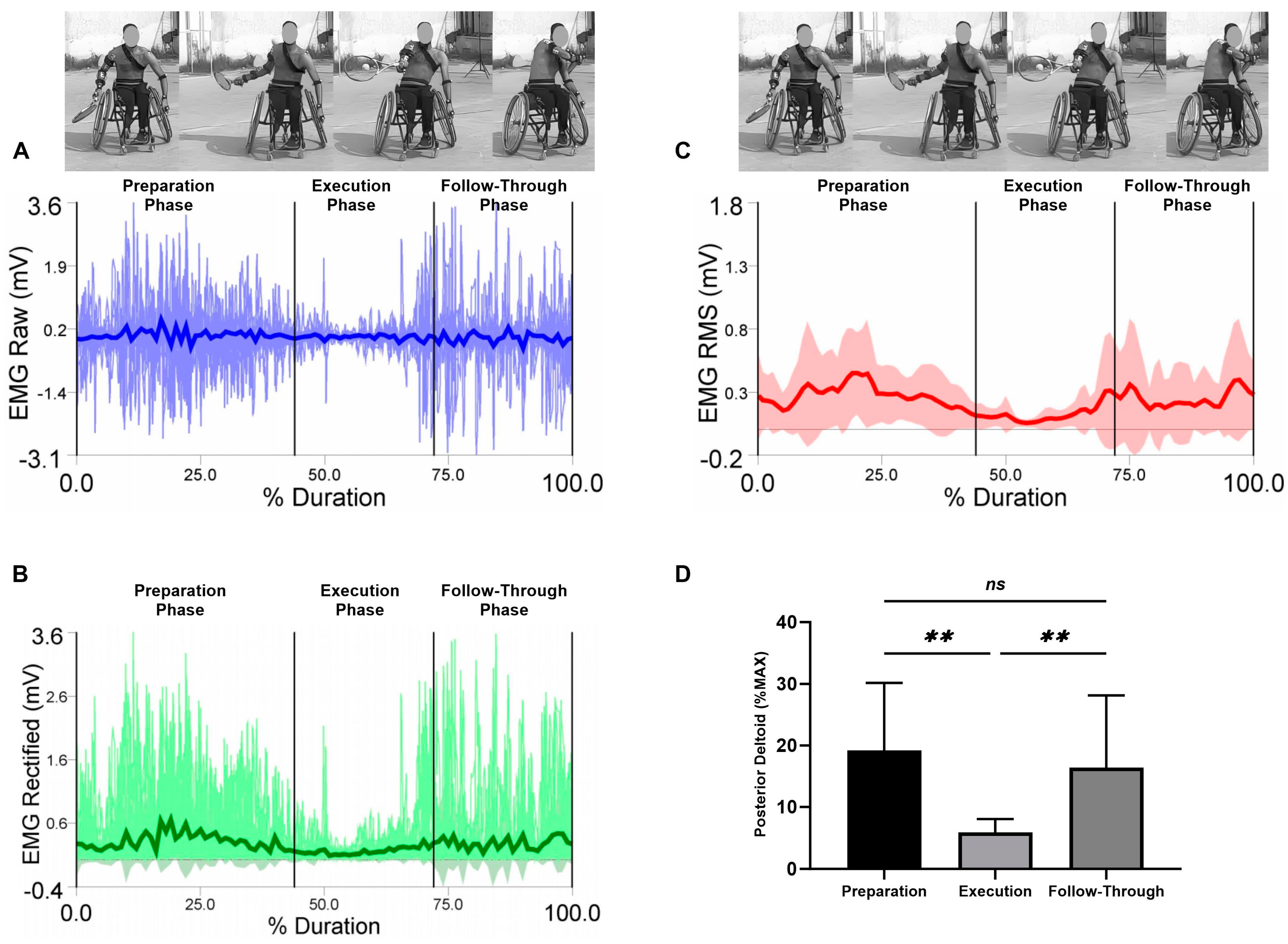
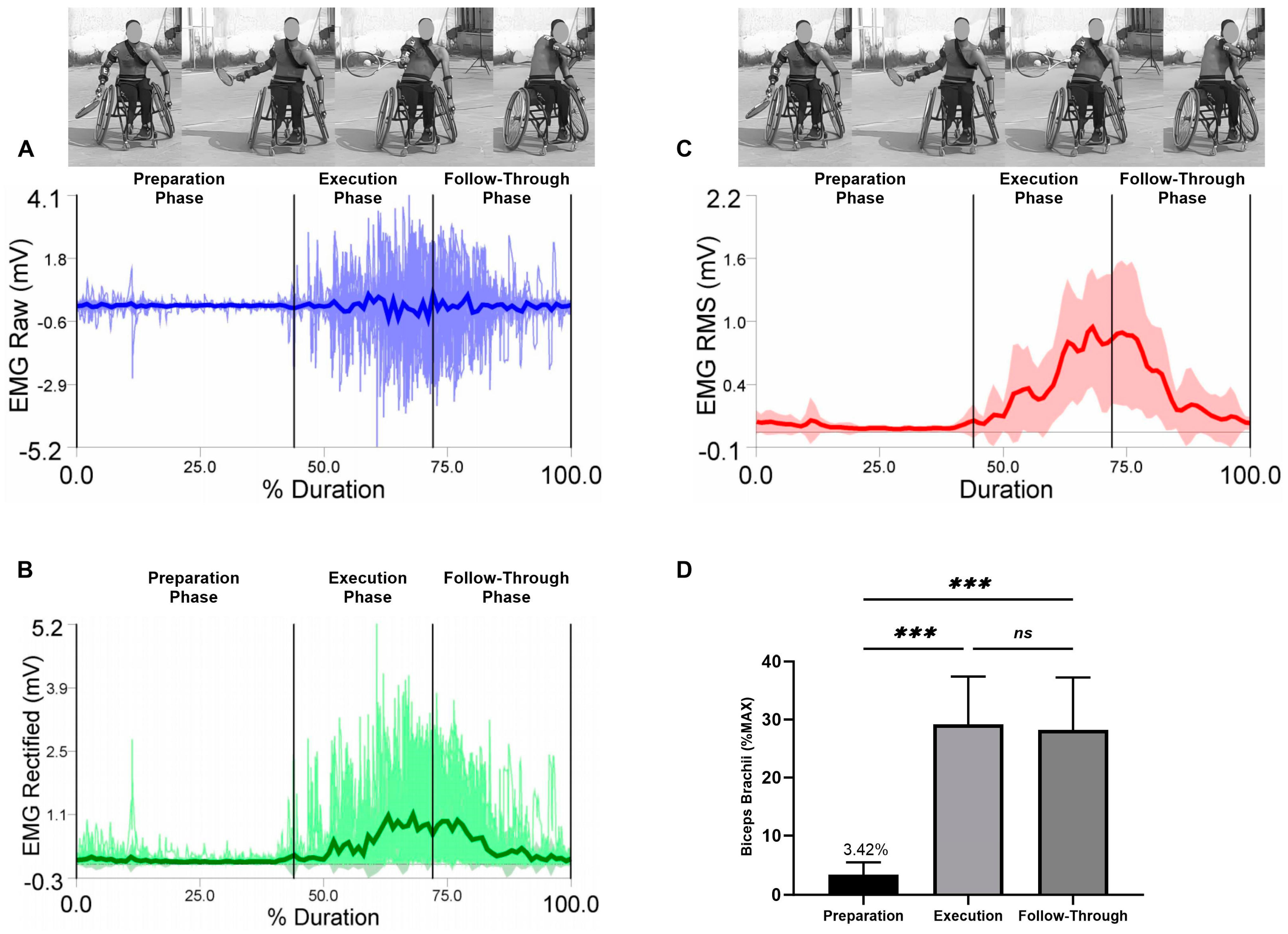
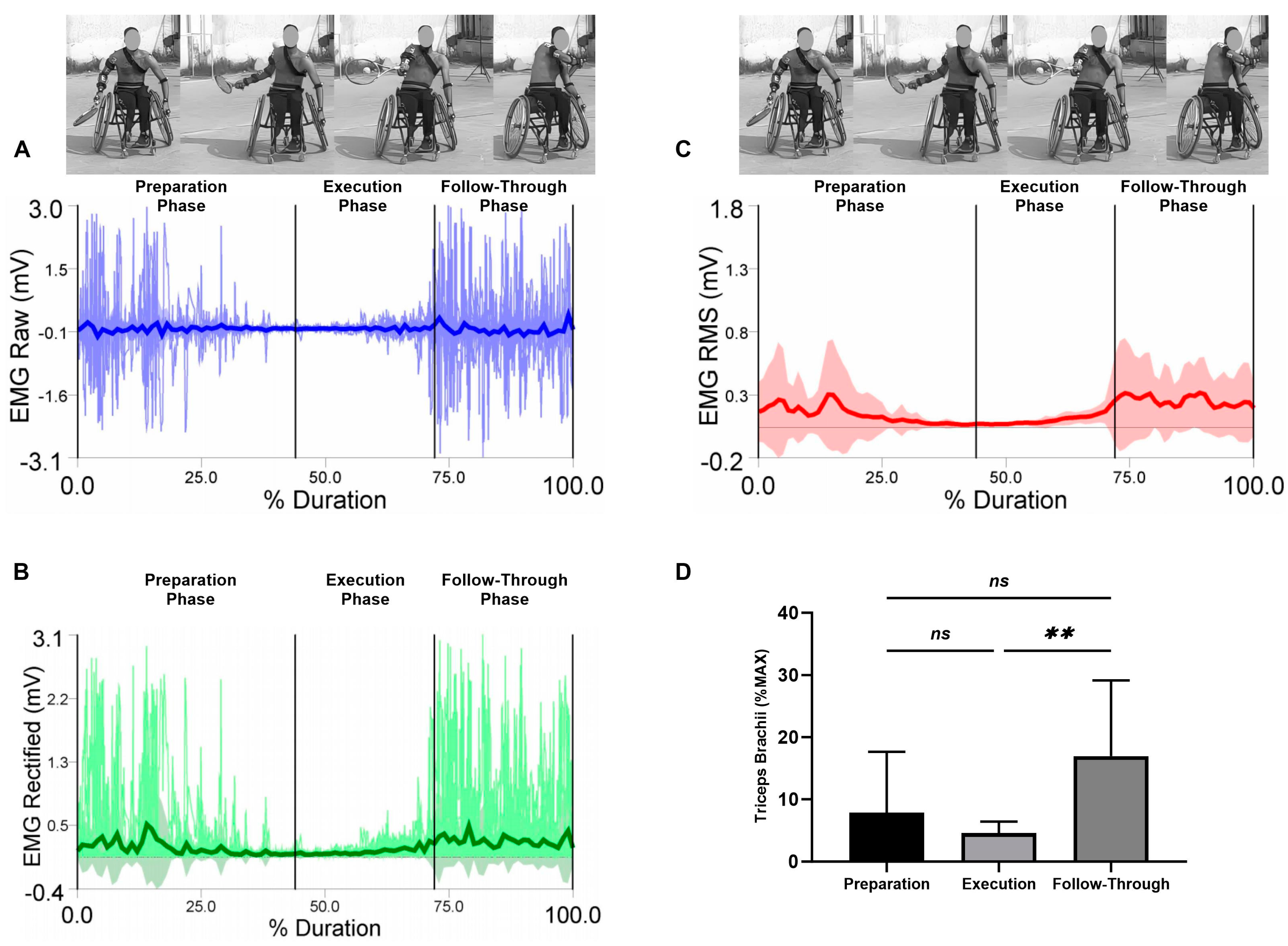
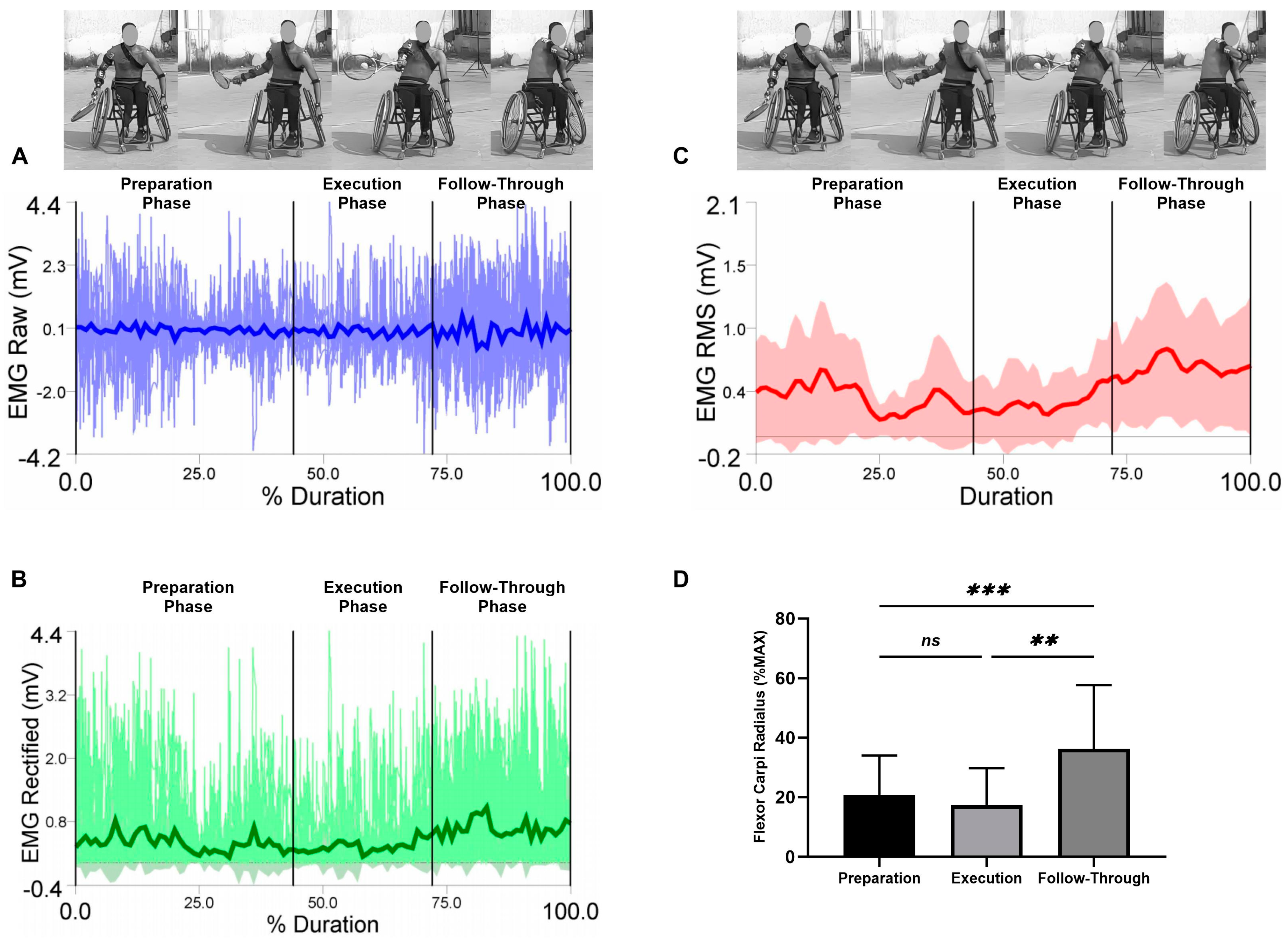
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sanchez-Pay, A.; Sanz-Rivas, D. Competitive Evolution of Professional Wheelchair Tennis from the Paralympic Games in Athens 2004 to Rio 2016: An Observational Study. Int. J. Environ. Res. Public Health 2021, 18, 3157. [Google Scholar] [CrossRef] [PubMed]
- Alberca, I.; Chenier, F.; Astier, M.; Watelain, E.; Vallier, J.M.; Pradon, D.; Faupin, A. Sprint performance and force application of tennis players during manual wheelchair propulsion with and without holding a tennis racket. PLoS ONE 2022, 17, e0263392. [Google Scholar] [CrossRef] [PubMed]
- Mayrhuber, L.; Rietveld, T.; de Vries, W.; van der Woude, L.H.V.; de Groot, S.; Vegter, R.J.K. A Scoping Review on Shoulder Injuries of Wheelchair Tennis Players: Potential Risk-Factors and Musculoskeletal Adaptations. Front. Rehabil. Sci. 2022, 3, 862233. [Google Scholar] [CrossRef] [PubMed]
- Rietveld, T.; Vegter, R.J.K.; der Woude, L.H.V.; de Groot, S. The interaction between wheelchair configuration and wheeling performance in wheelchair tennis: A narrative review. Sports Biomech./Int. Soc. Biomech. Sports 2021. [Google Scholar] [CrossRef] [PubMed]
- Goosey-Tolfrey, V.L.; Moss, A.D. Wheelchair velocity of tennis players during propulsion with and without the use of racquets. Adapt. Phys. Act. Q. 2005, 22, 291–301. [Google Scholar] [CrossRef]
- Blauwet, C.A.; Yang, H.Y.; Cruz, S.A.; Collins, J.E.; Smith, K.C.; Losina, E.; Katz, J.N. Functional and Environmental Factors Are Associated With Sustained Participation in Adaptive Sports. PM&R 2017, 9, 668–675. [Google Scholar] [CrossRef]
- Sakakibara, B.M.; Miller, W.C.; Eng, J.J.; Routhier, F.; Backman, C.L. Health, Personal, and Environmental Predictors of Wheelchair-Use Confidence in Adult Wheelchair Users. Phys. Ther. 2015, 95, 1365–1373. [Google Scholar] [CrossRef][Green Version]
- Veeger, H.; Rozendaal, L.; Van der Helm, F. Load on the shoulder in low intensity wheelchair propulsion. Clin. Biomech. 2002, 17, 211–218. [Google Scholar] [CrossRef]
- Van der Woude, L.; Veeger, H.; Dallmeijer, A.; Janssen, T.; Rozendaal, L. Biomechanics and physiology in active manual wheelchair propulsion. Med. Eng. Phys. 2001, 23, 713–733. [Google Scholar] [CrossRef]
- Medola, F.O.; Elui, V.M.C.; da Silva Santana, C.; Fortulan, C.A. Aspects of manual wheelchair configuration affecting mobility: A review. J. Phys. Ther. Sci. 2014, 26, 313–318. [Google Scholar] [CrossRef]
- Mason, B.S.; van der Woude, L.H.V.; Goosey-Tolfrey, V.L. The Ergonomics of Wheelchair Configuration for Optimal Performance in the Wheelchair Court Sports. Sports Med. 2013, 43, 23–38. [Google Scholar] [CrossRef] [PubMed]
- Matsuwaka, S.T.; Latzka, E.W. Summer adaptive sports technology, equipment, and injuries. Sports Med. Arthrosc. Rev. 2019, 27, 48–55. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Pay, A.; Torres-Luque, G.; Sanz-Rivas, D. Activity patterns in male and female wheelchair tennis matches. Kinesiology 2017, 49, 41–46. [Google Scholar] [CrossRef][Green Version]
- Chung, K.C.; Lark, M.E. Upper extremity injuries in tennis players: Diagnosis, treatment, and management. Hand Clin. 2017, 33, 175–186. [Google Scholar] [CrossRef] [PubMed]
- Jeon, I.-H.; Kochhar, H.; Lee, J.-M.; Kyung, H.-S.; Min, W.-K.; Cho, H.-S.; Wee, H.-W.; Shin, D.-J.; Kim, P.-T. Ultrasonographic evaluation of the shoulder in elite wheelchair tennis players. J. Sport Rehabil. 2010, 19, 161–172. [Google Scholar] [CrossRef]
- Heyward, O.W.; Vegter, R.J.; De Groot, S.; Van Der Woude, L.H. Shoulder complaints in wheelchair athletes: A systematic review. PLoS ONE 2017, 12, e0188410. [Google Scholar] [CrossRef]
- Aytar, A.; Zeybek, A.; Pekyavas, N.O.; Tigli, A.A.; Ergun, N. Scapular resting position, shoulder pain and function in disabled athletes. Prosthet. Orthot. Int. 2015, 39, 390–396. [Google Scholar] [CrossRef]
- Aben, A.; De Wilde, L.; Hollevoet, N.; Henriquez, C.; Vandeweerdt, M.; Ponnet, K.; Van Tongel, A. Tennis elbow: Associated psychological factors. J. Shoulder Elb. Surg. 2018, 27, 387–392. [Google Scholar] [CrossRef]
- Kibler, W.B.; Sciascia, A. Kinetic chain contributions to elbow function and dysfunction in sports. Clin. Sports Med. 2004, 23, 545–552. [Google Scholar] [CrossRef]
- Willick, S.E.; Webborn, N.; Emery, C.; Blauwet, C.A.; Pit-Grosheide, P.; Stomphorst, J.; Vliet, P.V.d.; Marques, N.A.P.; Martinez-Ferrer, J.O.; Jordaan, E.; et al. The epidemiology of injuries at the London 2012 Paralympic Games. Br. J. Sports Med. 2013, 47, 426–432. [Google Scholar] [CrossRef]
- Caldwell, M.; De Luigi, A.J. Wheelchair Tennis and Para-table Tennis. In Adaptive Sports Medicine: A Clinical Guide; De Luigi, A.J., Ed.; Springer International Publishing: Cham, Switzerland, 2018; pp. 201–217. [Google Scholar]
- Verhagen, E.; Clarsen, B.; Capel-Davies, J.; Collins, C.; Derman, W.; de Winter, D.; Dunn, N.; Ellenbecker, T.S.; Forde, R.; Hainline, B.; et al. Tennis-specific extension of the International Olympic Committee consensus statement: Methods for recording and reporting of epidemiological data on injury and illness in sport 2020. Br. J. Sports Med. 2021, 55, 9–13. [Google Scholar] [CrossRef] [PubMed]
- Pallis, J.M.; McNitt-Gray, J.L.; Hung, G.K. Biomechanical Principles and Applications in Sports; Springer: Berlin/Heidelberg, Germany, 2019. [Google Scholar]
- Horobeanu, C.; Johnson, A.; Pullinger, S.A. The prevalence of musculoskeletal injuries in junior elite squash players. Asian J. Sports Med. 2019, 10, e84495. [Google Scholar] [CrossRef]
- Okhovatian, F.; Ezatolahi, A. Sport injuries in squash. Pak. J. Med. Sci. 2009, 25, 413–417. [Google Scholar]
- Finch, C.F.; Eime, R.M. The epidemiology of squash injuries. Int. Sport. J. 2001, 2, 48462. [Google Scholar]
- Tsai, C.; Pan, K.; Huang, K.; Chang, T.; Hsueh, Y.; Wang, L.; Chang, S. The surface EMG activity of the upper limb muscles in table tennis forehand drives. In Proceedings of the ISBS-Conference Proceedings Archive, Marquette, MI, USA, 19–23 July 2010. [Google Scholar]
- Rigozzi, C.; Cox, J.; Vio, G.A.; Martens, W.L.; Poronnik, P. The effect of spin level and ball exit speed on forearm muscle activity in the tennis forehand stroke. Int. J. Sports Sci. Coach. 2021, 17, 123–133. [Google Scholar] [CrossRef]
- Ikenaga, M.; Okuma, N.; Nishiyama, H.; Chiba, S.; Nishino, K.; Omori, G.; Nunome, H. Influence of Ball Impact Location on Racquet Kinematics, Forearm Muscle Activation and Shot Accuracy during the Forehand Groundstrokes in Tennis. Proceedings 2020, 49, 89. [Google Scholar] [CrossRef]
- Yeh, I.L.; Elangovan, N.; Feczer, R.; Khosravani, S.; Mahnan, A.; Konczak, J. Vibration-Damping technology in tennis racquets: Effects on vibration transfer to the arm, muscle fatigue and tennis performance. Sports Med. Health Sci. 2019, 1, 49–58. [Google Scholar] [CrossRef]
- Rogowski, I.; Creveaux, T.; Faucon, A.; Rota, S.; Champely, S.; Guillot, A.; Hautier, C. Relationship between muscle coordination and racket mass during forehand drive in tennis. Eur. J. Appl. Physiol. 2009, 107, 289–298. [Google Scholar] [CrossRef]
- Kibler, W.B.; Chandler, T.J.; Shapiro, R.; Conuel, M. Muscle activation in coupled scapulohumeral motions in the high performance tennis serve. Br. J. Sports Med. 2007, 41, 745–749. [Google Scholar] [CrossRef]
- Knudson, D.; Blackwell, J. Trunk muscle activation in open stance and square stance tennis forehands. Int. J. Sports Med. 2000, 21, 321–324. [Google Scholar] [CrossRef]
- Akl, A.-R.; Hassan, A.; Elgizawy, H.; Tilp, M. Quantifying Coordination between Agonist and Antagonist Elbow Muscles during Backhand Crosscourt Shots in Adult Female Squash Players. Int. J. Environ. Res. Public Health 2021, 18, 9825. [Google Scholar] [CrossRef] [PubMed]
- de Groot, S.; Bos, F.; Koopman, J.; Hoekstra, A.; Vegter, R. Effect of holding a racket on propulsion technique of wheelchair tennis players. Scand. J. Med. Sci. Sports 2017, 27, 918–924. [Google Scholar] [CrossRef]
- Boninger, M.L.; Koontz, A.M.; Sisto, S.A.; Dyson-Hudson, T.A.; Chang, M.; Price, R.; Cooper, R.A. Pushrim biomechanics and injury prevention in spinal cord injury: Recommendations based on CULP-SCI investigations. J. Rehabil. Res. Dev. 2005, 42, 9. [Google Scholar] [CrossRef]
- Pellegrini, N.; Guillon, B.; Prigent, H.; Pellegrini, M.; Orlikovski, D.; Raphael, J.-C.; Lofaso, F. Optimization of power wheelchair control for patients with severe Duchenne muscular dystrophy. Neuromuscul. Disord. 2004, 14, 297–300. [Google Scholar] [CrossRef] [PubMed]
- Boninger, M.L.; Baldwin, M.; Cooper, R.A.; Koontz, A.; Chan, L. Manual wheelchair pushrim biomechanics and axle position. Arch. Phys. Med. Rehabil. 2000, 81, 608–613. [Google Scholar] [CrossRef] [PubMed]
- Genevois, C.; Reid, M.; Creveaux, T.; Rogowski, I. Kinematic differences in upper limb joints between flat and topspin forehand drives in competitive male tennis players. Sports Biomech./Int. Soc. Biomech. Sports 2020, 19, 212–226. [Google Scholar] [CrossRef]
- Furuya, R.; Yokoyama, H.; Dimic, M.; Yanai, T.; Vogt, T.; Kanosue, K. Difference in racket head trajectory and muscle activity between the standard volley and the drop volley in tennis. PLoS ONE 2021, 16, e0257295. [Google Scholar] [CrossRef]
- Rota, S.; Hautier, C.; Creveaux, T.; Champely, S.; Guillot, A.; Rogowski, I. Relationship between muscle coordination and forehand drive velocity in tennis. J. Electromyogr. Kinesiol. 2012, 22, 294–300. [Google Scholar] [CrossRef]
- Hermens, H.J.; Freriks, B.; Disselhorst-Klug, C.; Rau, G. Development of recommendations for SEMG sensors and sensor placement procedures. J. Electromyogr. Kinesiol. 2000, 10, 361–374. [Google Scholar] [CrossRef]
- Quittmann, O.J.; Meskemper, J.; Albracht, K.; Abel, T.; Foitschik, T.; Struder, H.K. Normalising surface EMG of ten upper-extremity muscles in handcycling: Manual resistance vs. sport-specific MVICs. J. Electromyogr. Kinesiol. 2020, 51, 102402. [Google Scholar] [CrossRef]
- Ju, Y.Y.; Chu, W.T.; Shieh, W.Y.; Cheng, H.K. Sensors for Wheelchair Tennis: Measuring Trunk and Shoulder Biomechanics and Upper Extremity Vibration during Backhand Stroke. Sensors 2021, 21, 6576. [Google Scholar] [CrossRef]
- Lauer, J.; Figueiredo, P.; Vilas-Boas, J.P.; Fernandes, R.J.; Rouard, A.H. Phase-dependence of elbow muscle coactivation in front crawl swimming. J. Electromyogr. Kinesiol. 2013, 23, 820–825. [Google Scholar] [CrossRef] [PubMed]
- Rouard, A.H.; Clarys, J.P. Cocontraction in the elbow and shoulder muscles during rapid cyclic movements in an aquatic environment. J. Electromyogr. Kinesiol. 1995, 5, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Ju, Y.Y.; Chu, W.T.; Shieh, W.Y.; Cheng, H.K. Elbow, wrist kinematics and shock transmission of backhand stroke in wheelchair tennis players. Sports Biomech./Int. Soc. Biomech. Sports 2021. [Google Scholar] [CrossRef] [PubMed]
- Darainy, M.; Ostry, D.J. Muscle cocontraction following dynamics learning. Exp. Brain Res. 2008, 190, 153–163. [Google Scholar] [CrossRef]
- Bazzucchi, I.; Sbriccoli, P.; Marzattinocci, G.; Felici, F. Coactivation of the elbow antagonist muscles is not affected by the speed of movement in isokinetic exercise. Muscle Nerve 2006, 33, 191–199. [Google Scholar] [CrossRef]
- Giangarra, C.E.; Conroy, B.; Jobe, F.W.; Pink, M.; Perry, J. Electromyographic and cinematographic analysis of elbow function in tennis players using single-and double-handed backhand strokes. Am. J. Sports Med. 1993, 21, 394–399. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abuwarda, K.; Akl, A.-R. Changes in Electromyographic Activity of the Dominant Arm Muscles during Forehand Stroke Phases in Wheelchair Tennis. Sensors 2023, 23, 8623. https://doi.org/10.3390/s23208623
Abuwarda K, Akl A-R. Changes in Electromyographic Activity of the Dominant Arm Muscles during Forehand Stroke Phases in Wheelchair Tennis. Sensors. 2023; 23(20):8623. https://doi.org/10.3390/s23208623
Chicago/Turabian StyleAbuwarda, Khaled, and Abdel-Rahman Akl. 2023. "Changes in Electromyographic Activity of the Dominant Arm Muscles during Forehand Stroke Phases in Wheelchair Tennis" Sensors 23, no. 20: 8623. https://doi.org/10.3390/s23208623
APA StyleAbuwarda, K., & Akl, A.-R. (2023). Changes in Electromyographic Activity of the Dominant Arm Muscles during Forehand Stroke Phases in Wheelchair Tennis. Sensors, 23(20), 8623. https://doi.org/10.3390/s23208623







