Multisensory System for Long-Term Activity Monitoring to Facilitate Aging-in-Place
Abstract
:1. Introduction
- An initial one monitoring mainly the activity data obtained from and initial system, counting number of steps during active periods of time and step frequency when walking, demonstrating the feasibility of the process for the subsequent generation of behavioural patterns;
- A second approach, where room-level location information is included to infer the type of activity. In addition to the inertial measurements, we would also include symbolic location based on WiFi and a barometer;
- Finally, we would consider precise positioning in selected areas. In this phase, an ad hoc wearable designed for DPA estimation would be introduced, adding precise adding precise positioning to the available inertial information.
2. Related Work
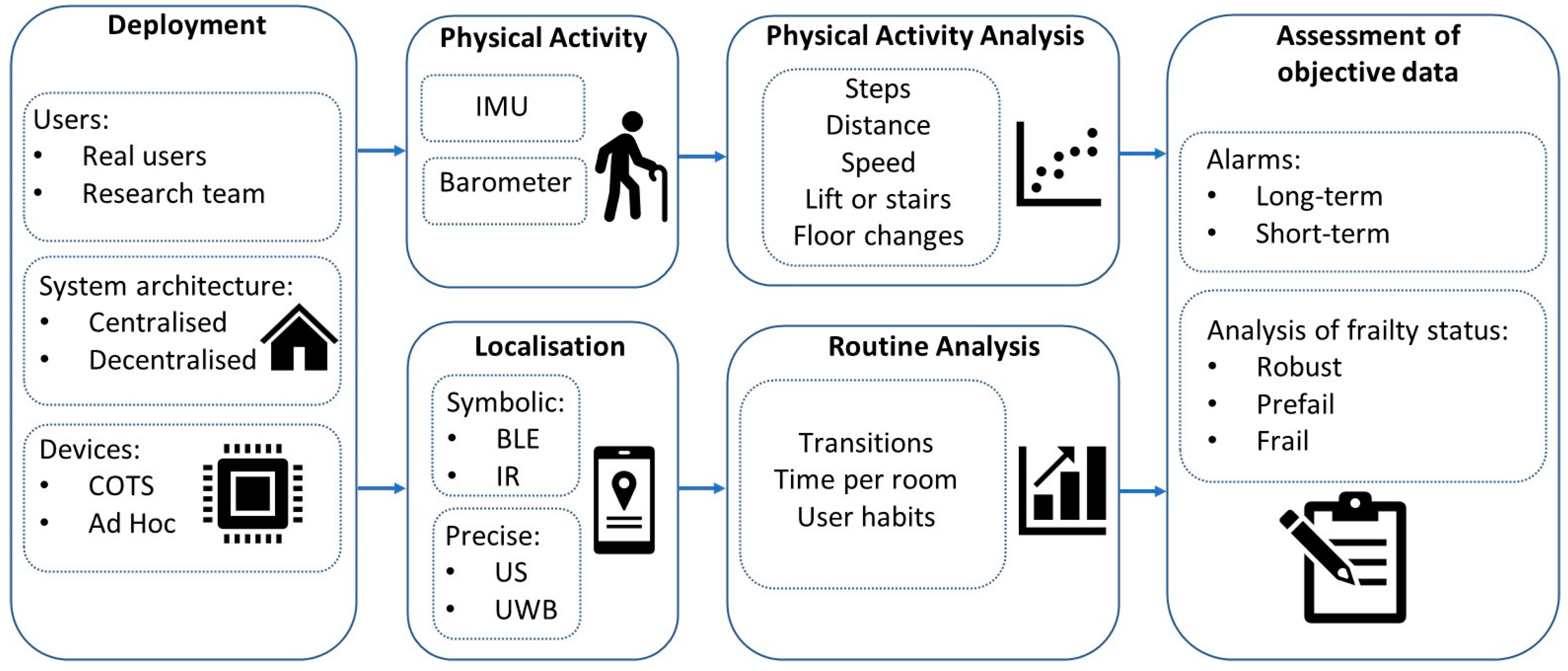
3. Experimental Approaches
3.1. Physical Activity Monitoring Approaches
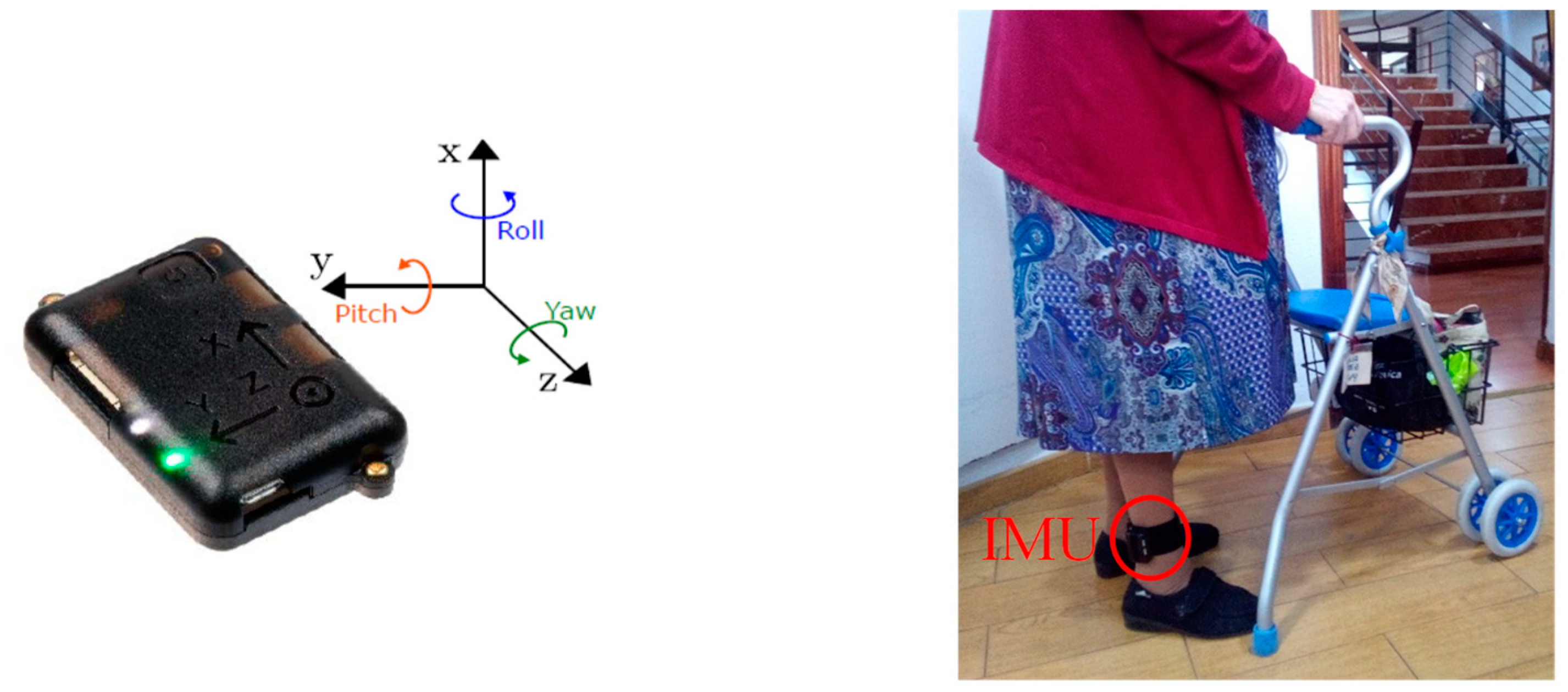
3.1.1. Inertial Sensor-Based Monitoring Approach
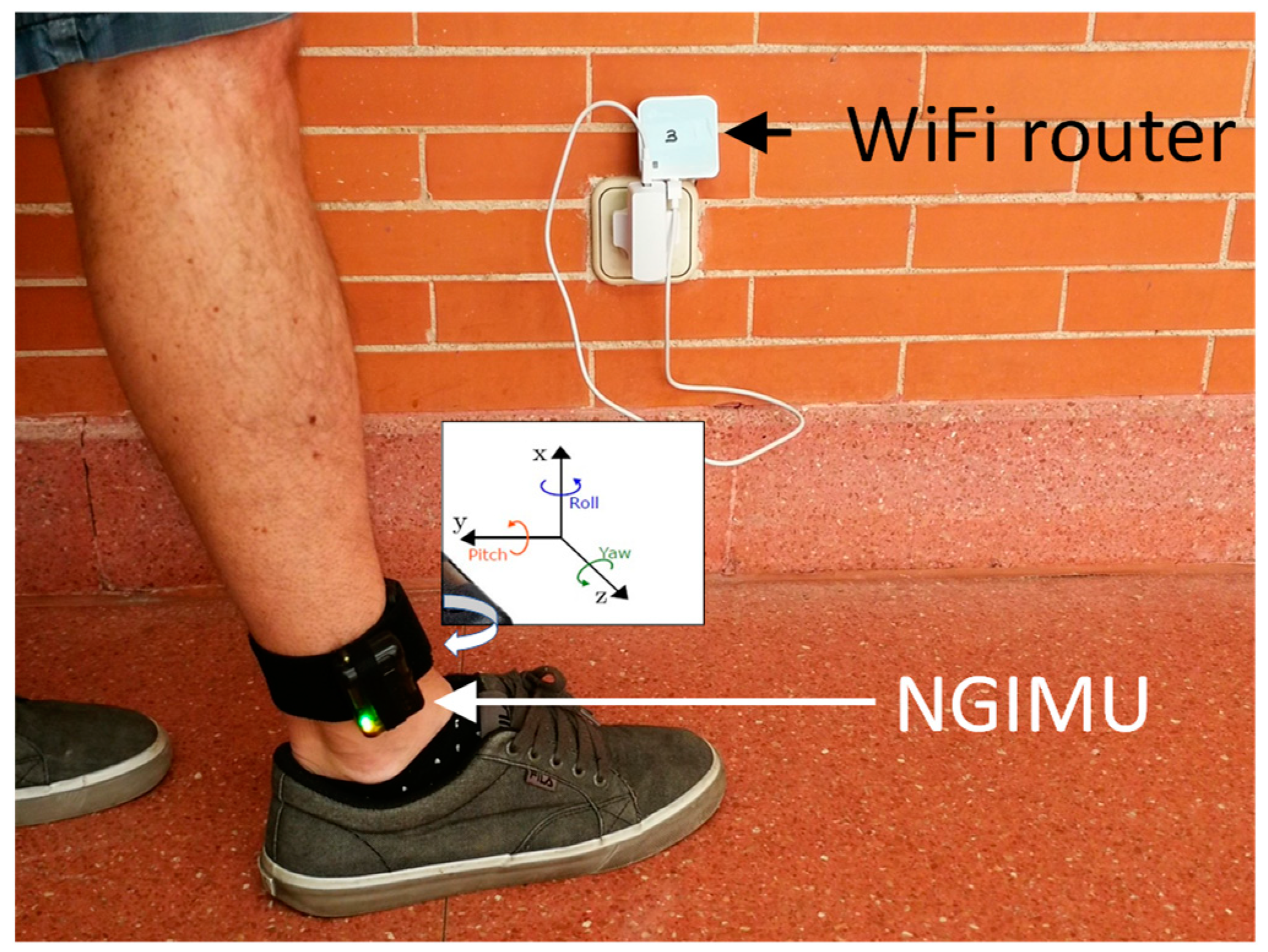
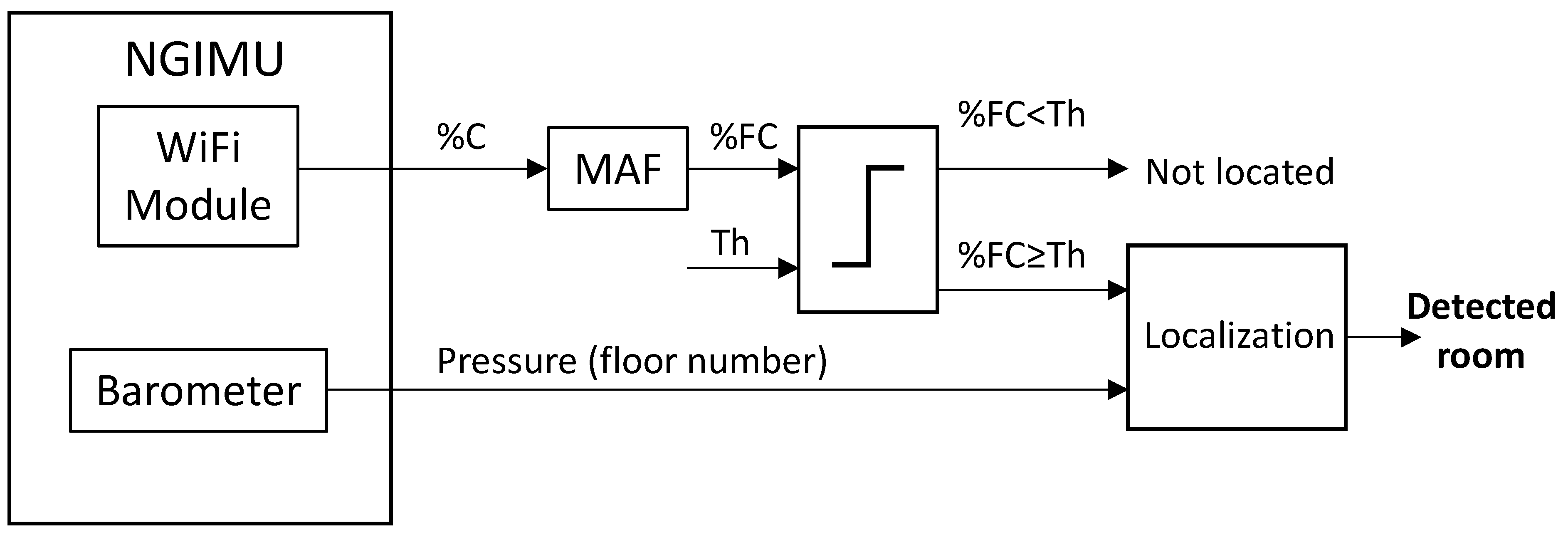
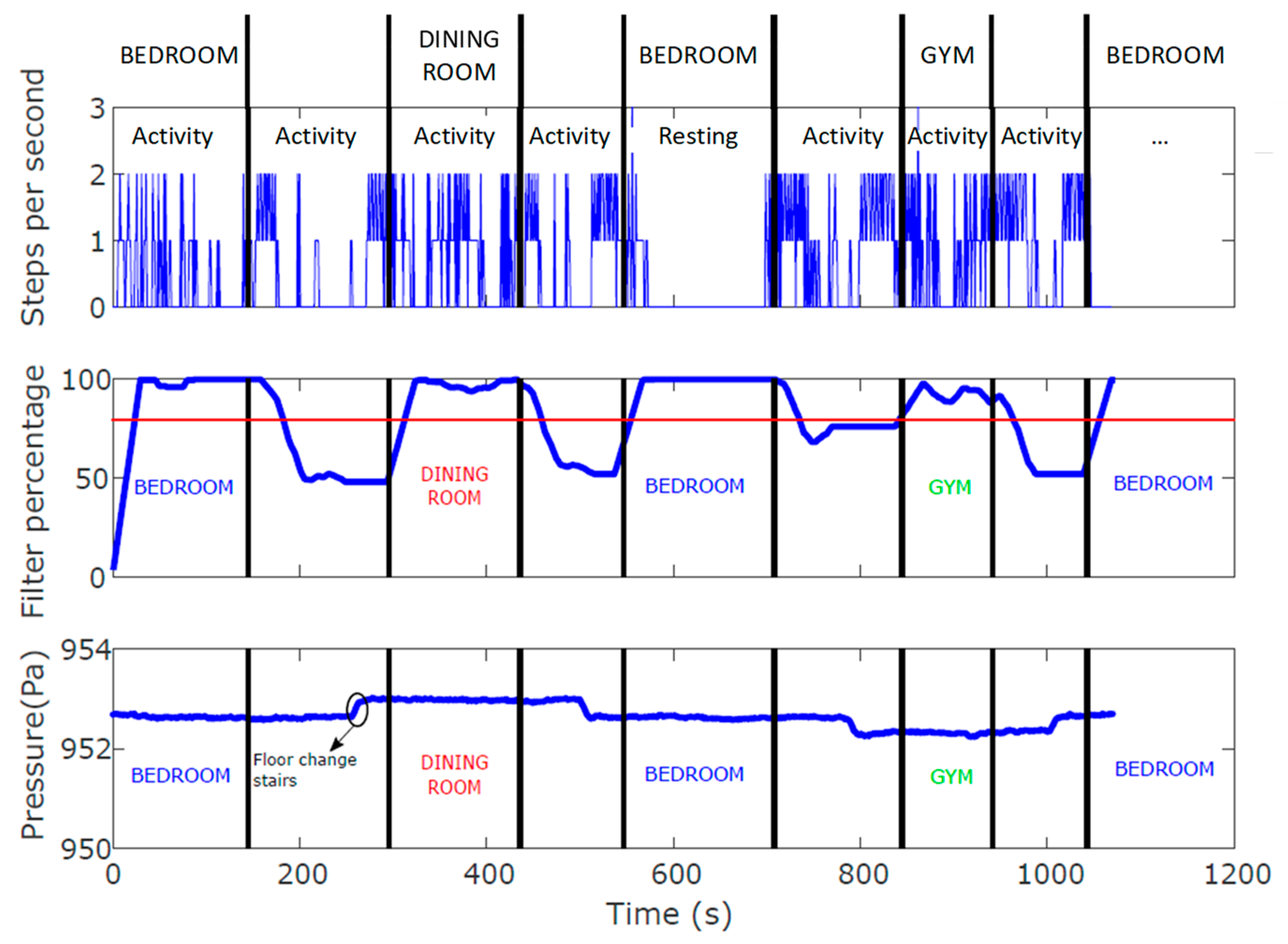
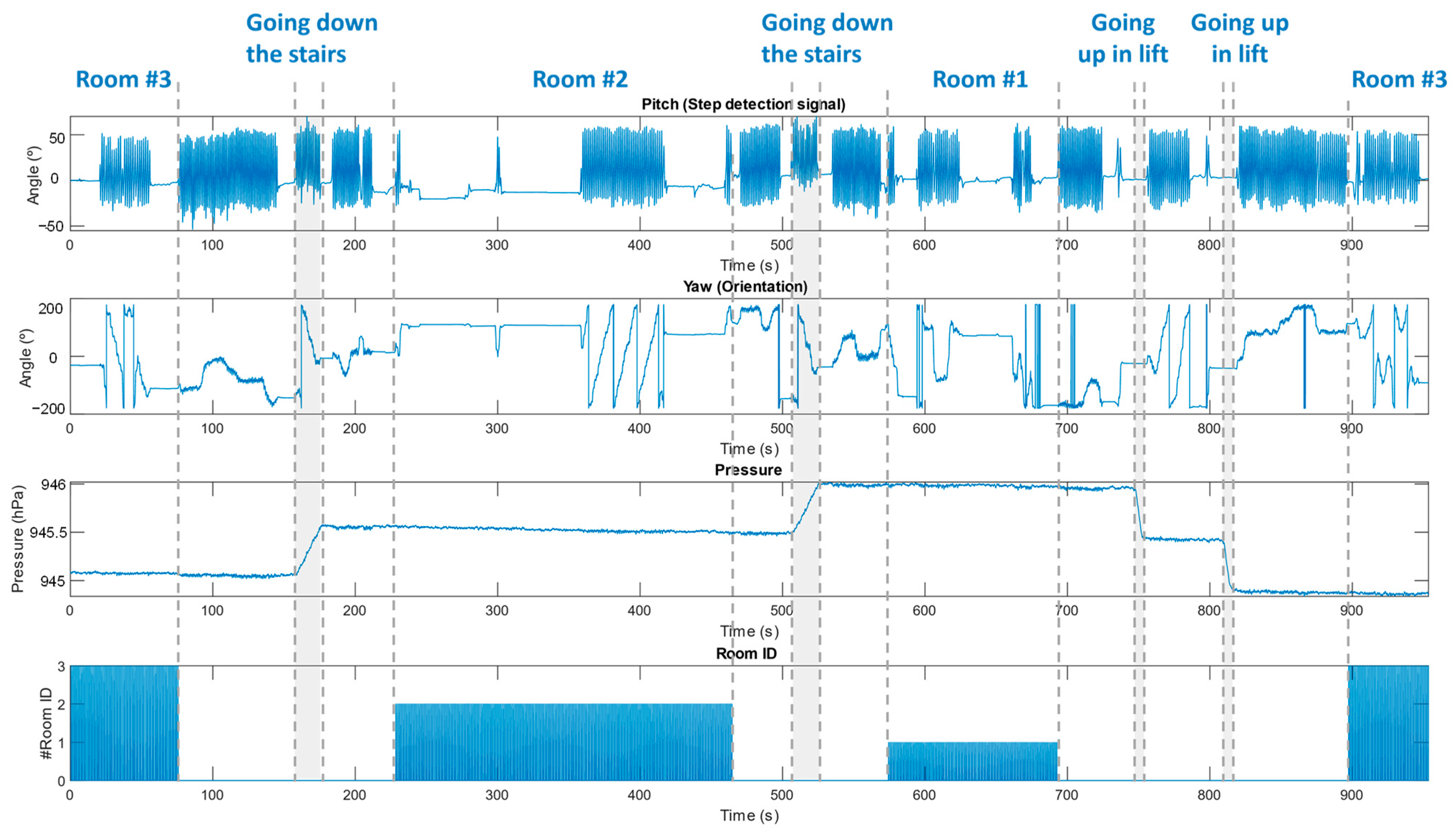
3.1.2. Symbolic Location-Based Monitoring Approach
3.1.3. Precise Positioning-Based Approach: The FrailWear System
3.2. Participants
- Two healthy men living in their own home, both 75 years of age, clinically defined as robust/prefrail according to the Fried Frailty Index at the start of the study;
- Two frail women, an 88- and 92-year-old, institutionalized in the nursing home of Albertia, Las Palmeras, in Azuqueca de Henares (Spain). Both women used a walking aid.
3.3. Test Environments
- Preliminary tests were performed in the School of Engineering of the University of Alcalá (Madrid, Spain);
- Other tests were developed in the participants’ home;
- Finally, other experiments took place in a nursing home with approximately 100 residents. The residence has a total of four floors with approximately 2875 m2 per floor. Each floor has different facilities, which are specified in Table 1.
4. Inertial Sensor-Based Monitoring Approach
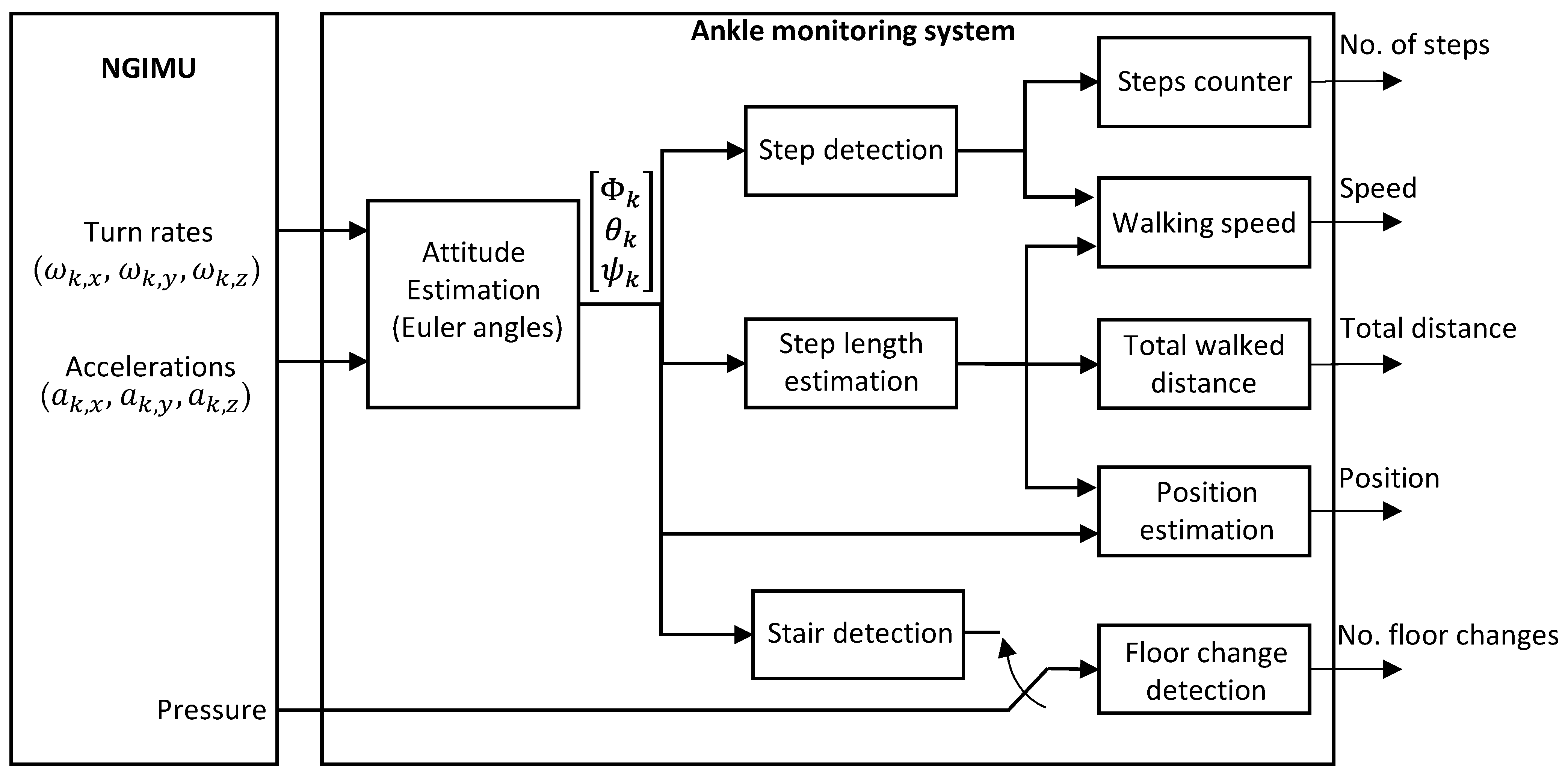
4.1. System Description
4.2. Algorithms
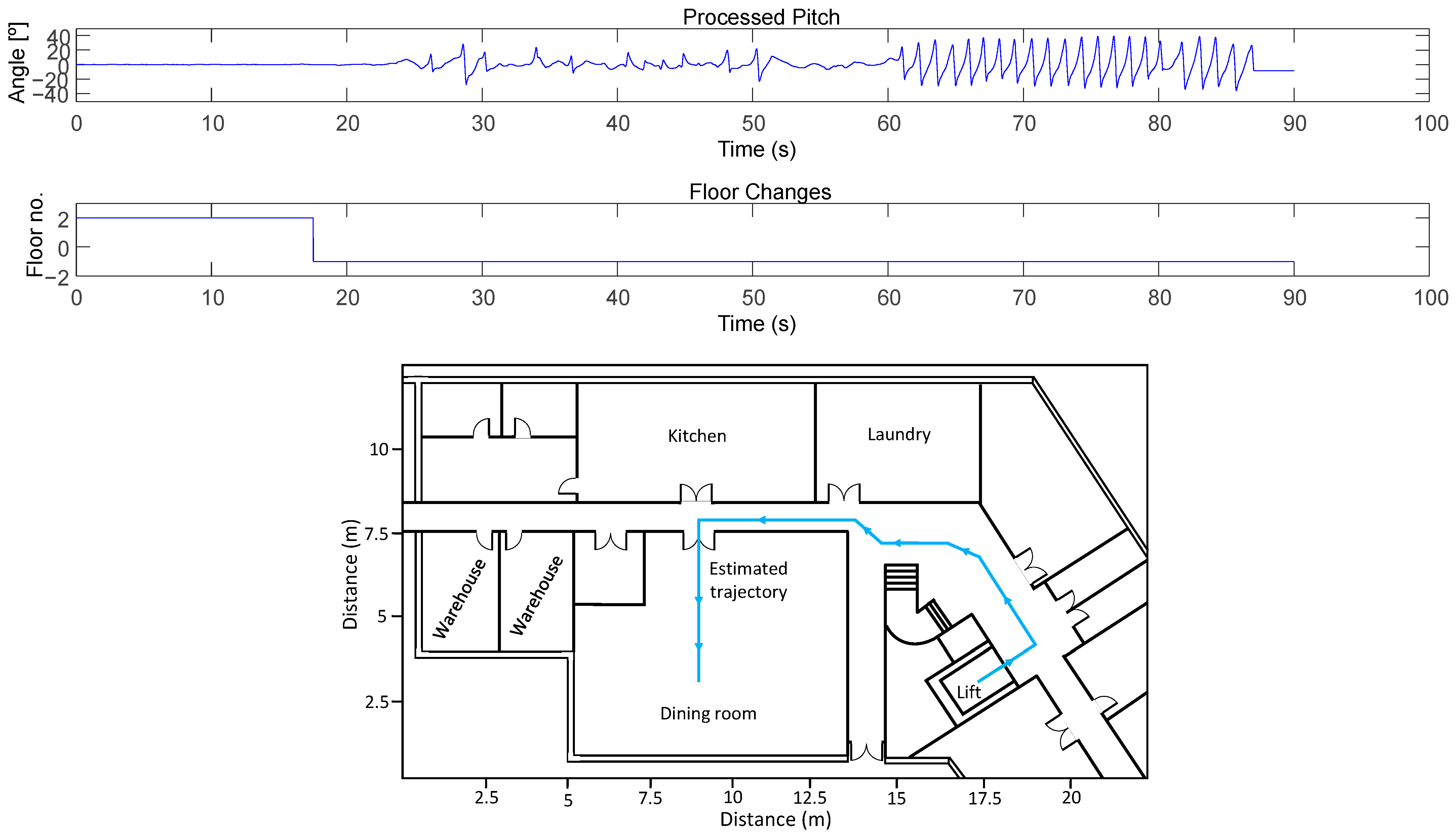
4.2.1. Step Detection
| Algorithm 1: Step detection algorithm |
| Inputs: pitch Outputs: n_steps n_steps = 0 max_processed = inf min_processed = −inf if(k > 100) then mean_pitch(k) = mean(pitch(k − 100:k)) pitch_processed(k) = pitch(k) − mean_pitch(k) if pitch_processed(k − 1)<0 && pitch_processed(k) > 0 then n_ZC = n_ZC + 1 up = 1 down = 0 if pitch_processed(k − 1) > 0 && pitch_processed(k) < 0 then n_ZC = n_ZC + 1 up = 0 down = 1 if up == 1 && pitch_processed(k) > max_ processed then max_processed = pitch_processed(k) if down == 1 && pitch_processed(k) < min_ processed then min_ processed = pitch_processed(k) if n_ZC == 2 then if abs(max_processed − min_processed) > 25 then if max_processed > 7 && min_processed < −7 then n_steps = n_steps + 1 n_ZC = 0 |
4.2.2. Step Length Estimation
4.2.3. Floor-Change Detection
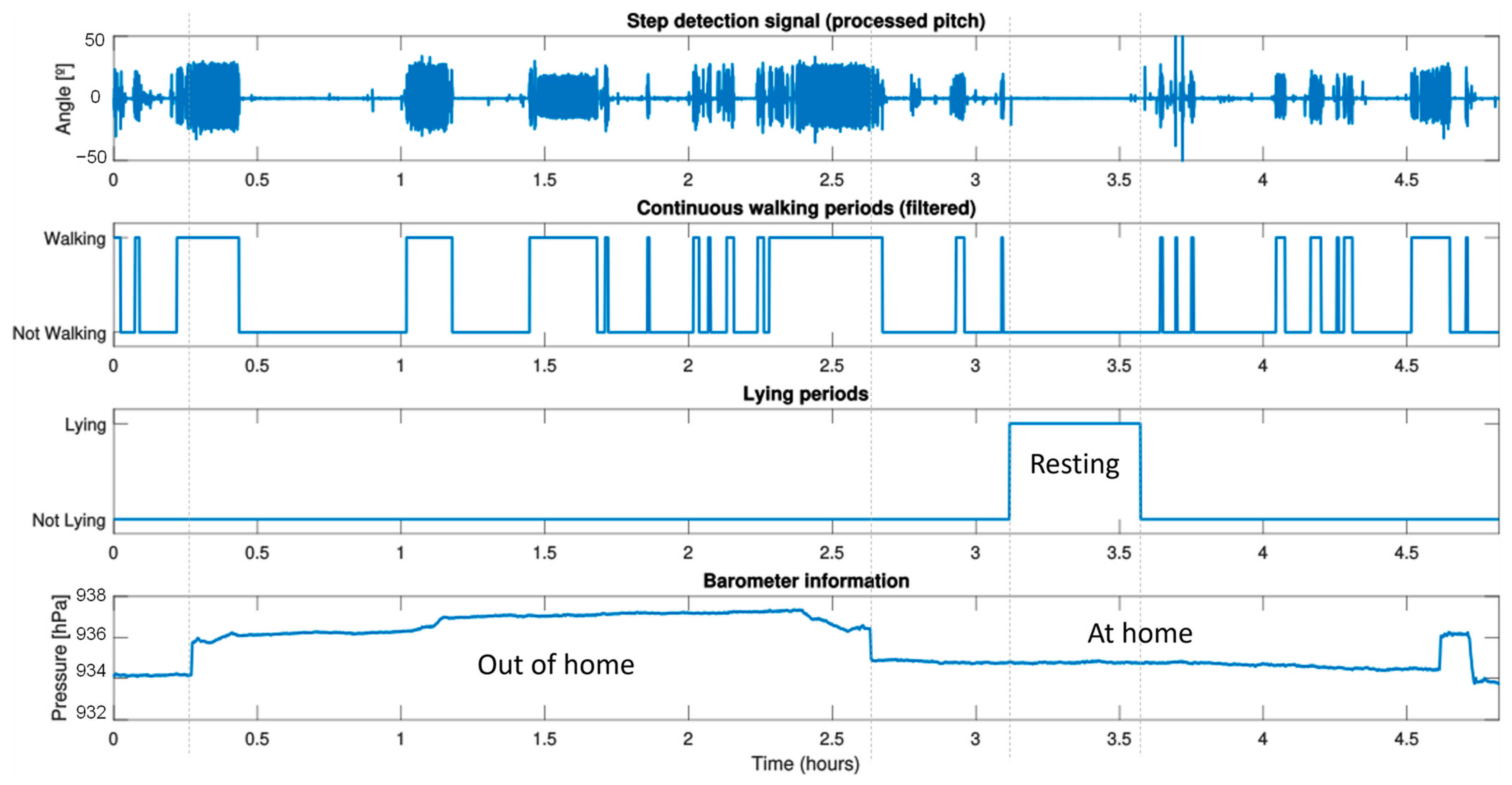
4.3. Experiments for Monitoring Physical Activity over Time
4.3.1. Short-Term Monitoring
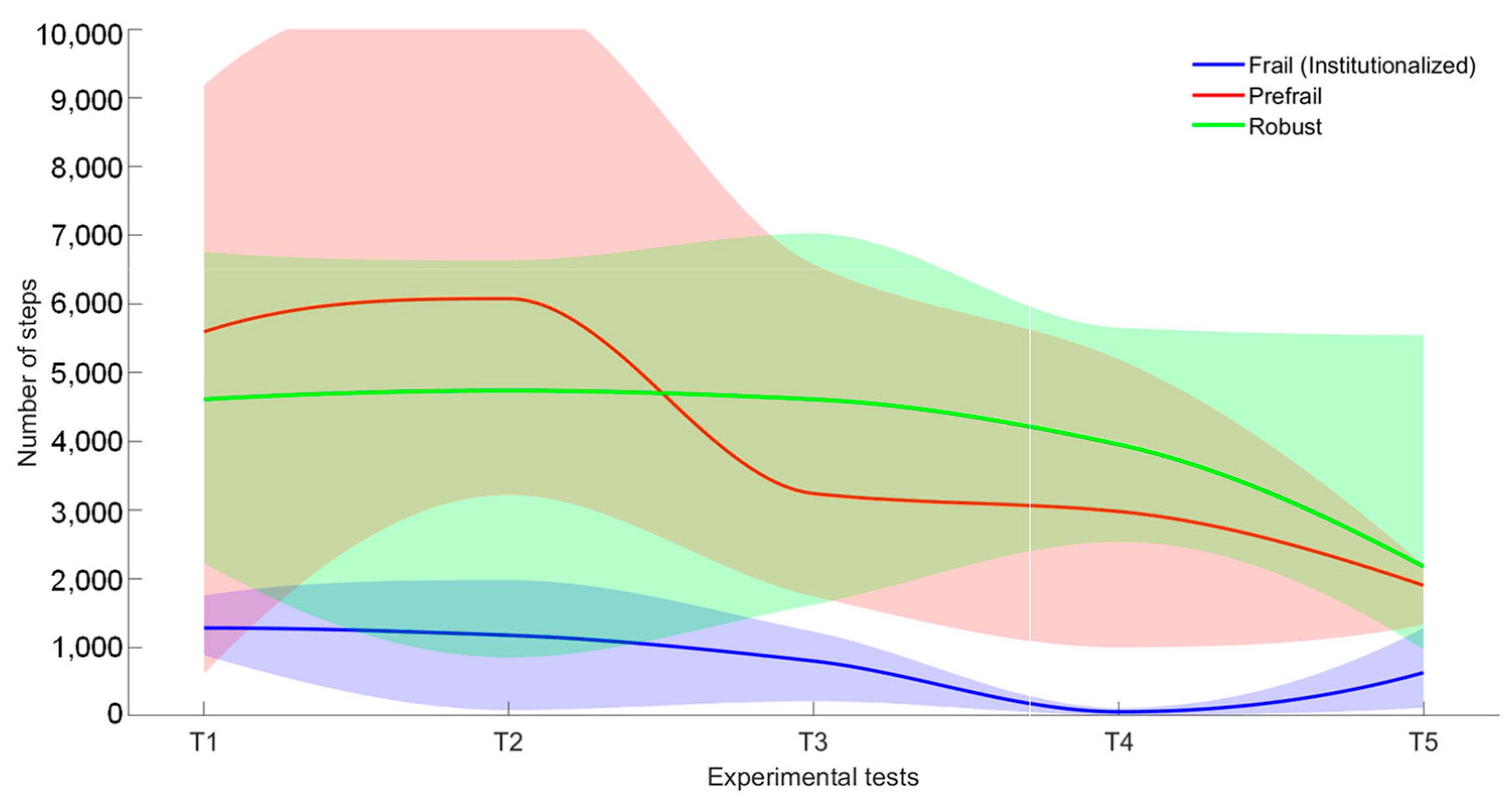
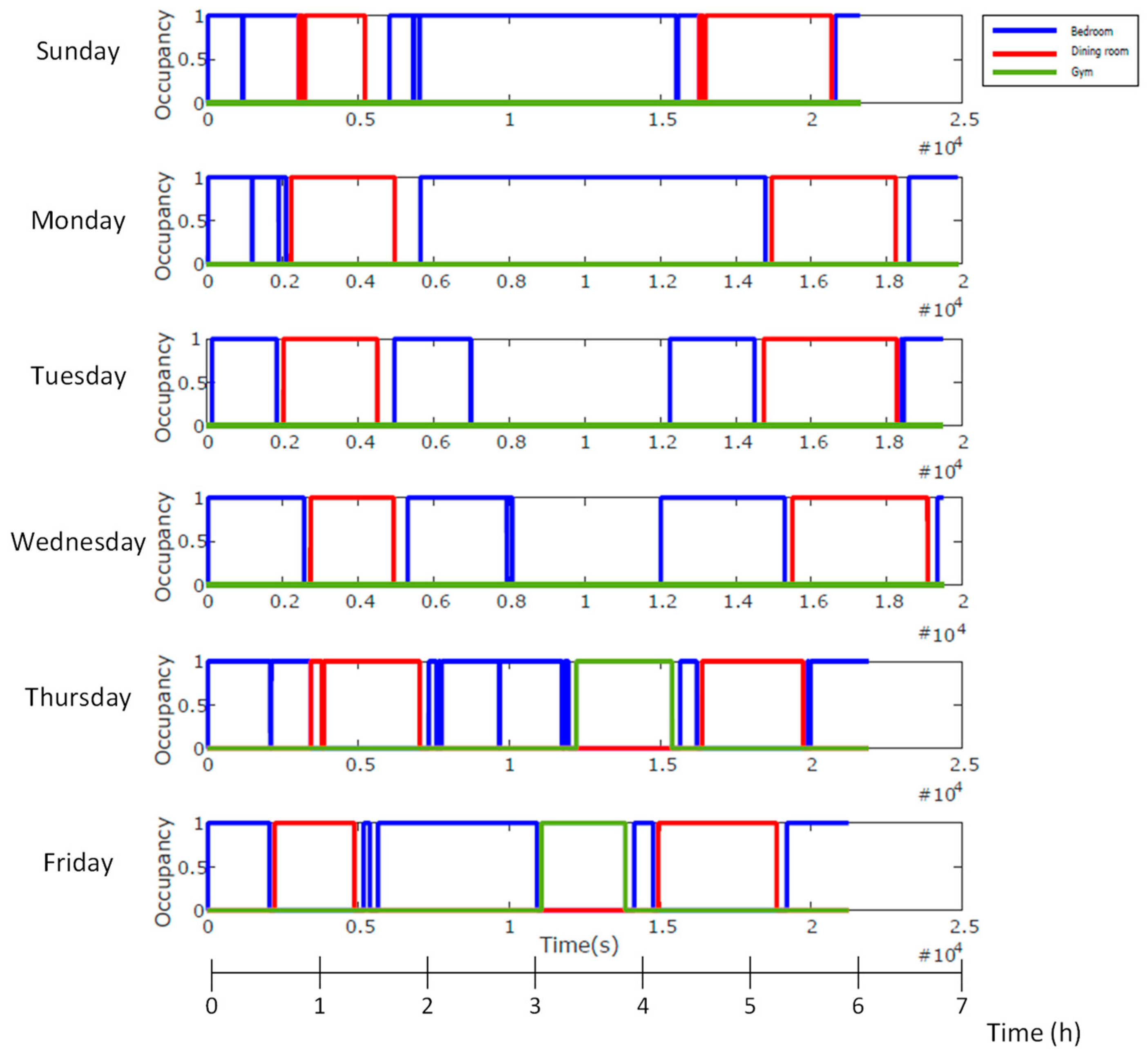
4.3.2. Long-Term Monitoring
5. Symbolic Location-Based Monitoring Approach
5.1. System Description
5.2. Symbolic Localization
5.3. Experimental Results
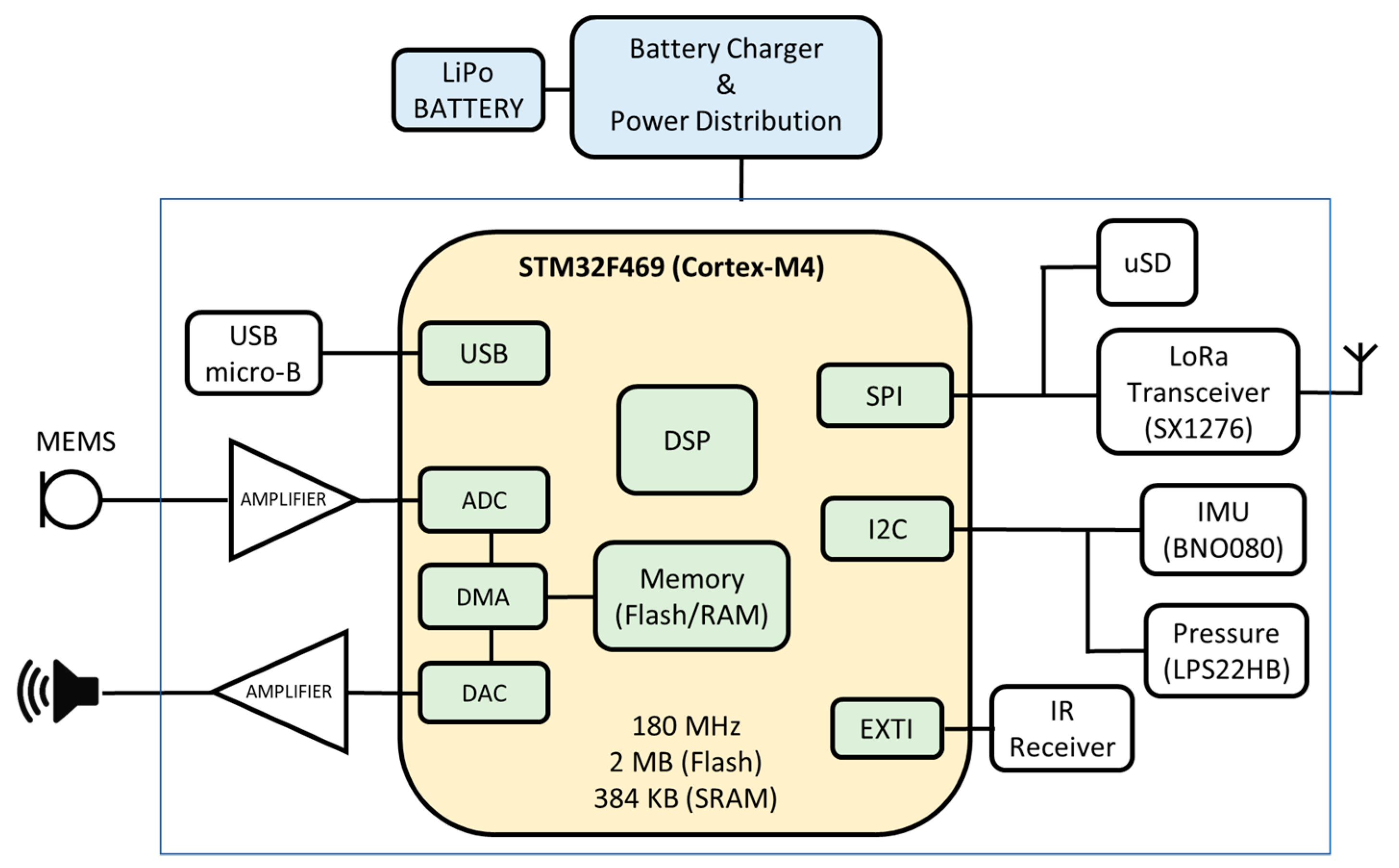
6. Precise Positioning-Based Approach: The FrailWear System
6.1. The Global FrailWear System
- The main core of the device is a Cortex-M4 processor (STMicroelectronics, 32-bit STM32F469 [42]), which reads through I2C (Inter-Integrated Circuit), and SPI (Serial Peripheral Interface) buses the information of digital sensors. It is particularly distinct in its capability to acquire the ultrasonic signals from the encoded beacons (with Kasami codes) through a microphone, to decode the information and to process it to autonomously to provide 3D positioning. Algorithm 2 shows the US-based localization algorithm (more details about how our ULPS works can be found in [39]);
- It incorporates an IMU subsystem, implemented on a dedicated board using a Bosch’s BNO080 sensor [43]. This sensor integrates a 3-axis accelerometer, gyroscope and magnetometer, packaged with an ARM Cortex M0+ microcontroller that allows to implement high-level algorithms to reduce the computation load of the main microcontroller;
- The barometer utilized is a high-resolution MEMS nano pressure sensor with absolute digital output (STMicroelectronics, LPS22HB [44]) and an accuracy of ±0.1 hPa, which is equivalent to about 10 cm in vertical resolution. Additionally, the chip has an integrated temperature sensor with a 12-bit resolution that provides an accuracy of 1.5 °C. This temperature value is then used to obtain higher accuracy when calculating the ToF (Time-of-Flight) of the ultrasonic signals for the precise positioning.
| Algorithm 2: US-based localization algorithm |
| Inputs: int_IR //infrared signal synchronization Outputs: x, y, z //3D positioning kasami_code = load_kasami_codes() f = 100e3 // Sample frequency v = calculate_sound_speed(temperature) // Sound speed sequence_samples = 1224 if (int_IR == 1) then room_ID = decode_IR_code() US_signal = acquire_US_buffer() pos_US_beacons = load_US_beacons(room_ID) for i=1:n_US_beacons corr(i) = correlation(US_signal, kasami_code(i)) pos_peak(i) = peak_detection(corr(i)) distances(i) = (pos_peak(i)- sequence_samples)*v/f x, y, z = Gauss_Newton(distances, pos_US_beacons) |
- The infrared module is based on the TSOP7000 infrared receiver from Vishay [45] and works at a 455 kHz carrier frequency. It is used to synchronize the whole ultrasonic positioning system. To obtain a symbolic location at a room-level accuracy, the signal emitted by the synchronization beacon is encoded with an 8-bit code. This allows the room where the person is located to be uniquely differentiated as the infrared signal is confined within the walls. By default, the IR beacons are configured with an emission frequency of 1 Hz, i.e., they emit both the synchronism pulse and the room identification code every second (it is required that the person stays in the room more than one second to be identified);
- The ultrasonic signals emitted by the beacons are acquired with a MEMS microphone SPU0414HR5H-SB [46] followed by a built-in amplification and high-pass filtering stage previous to an analog-to-digital converter (ADC). The microphone is mounted on an external board to place it on a body location where the best ultrasonic coverage is achieved;
- The system is continuously recording a log of all the parameters obtained on a microSD memory card for further analysis, although it also has a LoRa communication port so that data can be transmitted to the cloud even in low coverage environments with long-range, low-power wireless communication (this feature is not used in the current work).
6.2. Experimental Results
7. Discussion
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rogers, W.A.; Mitzner, T.L. Envisioning the future for older adults: Autonomy, health, well-being, and social connectedness with technology support. Futures 2017, 87, 133–139. [Google Scholar] [CrossRef] [PubMed]
- Binette, J.; Kerri, V. 2018 Home and Community Preferences: A National Survey of Adults Age 18-Plus; AARP Research: Washington, DC, USA, 2018. [Google Scholar] [CrossRef]
- Kim, D.; Bian, H.; Chang, C.K.; Dong, L.; Margrett, J. In-Home Monitoring Technology for Aging in Place: Scoping Review. Interact. J. Med. Res. 2022, 11, 2. [Google Scholar] [CrossRef] [PubMed]
- Olmedo-Aguirre, J.O.; Reyes-Campos, J.; Alor-Hernández, G.; Machorro-Cano, I.; Rodríguez-Mazahua, L.; Sánchez-Cervantes, J.L. Remote Healthcare for Elderly People Using Wearables: A Review. Biosensors 2022, 12, 73. [Google Scholar] [CrossRef] [PubMed]
- Manickam, P.; Mariappan, S.A.; Murugesan, S.M.; Hansda, S.; Kaushik, A.; Shinde, R.; Thipperudraswamy, S.P. Artificial Intelligence (AI) and Internet of Medical Things (IoMT) Assisted Biomedical Systems for Intelligent Healthcare. Biosensors 2022, 12, 562. [Google Scholar] [CrossRef]
- Izquierdo, M.; Duque, G.; Morley, J.E. Physical activity guidelines for older people: Knowledge gaps and future directions. Lancet Healthy Longev. 2021, 2, 6. [Google Scholar] [CrossRef]
- Langhammer, B.; Bergland, A.; Rydwik, E. The Importance of Physical Activity Exercise among Older People. BioMed Res. Int. 2018, 2018, 7856823. [Google Scholar] [CrossRef]
- Rao, A.K. Wearable Sensor Technology to Measure Physical Activity (PA) in the Elderly. Curr. Geriatr. Rep. 2019, 8, 55–66. [Google Scholar] [CrossRef]
- Groessl, E.J.; Kaplan, R.M.; Rejeski, W.J.; Katula, J.A.; King, A.C.; Frierson, G.; Glynn, N.W.; Hsu, F.-C.; Walkup, M.; Pahor, M. Health-related quality of life in older adults at risk for disability. Am. J. Prev. Med. 2007, 33, 214–218. [Google Scholar] [CrossRef]
- Stessman, J.; Hammerman-Rozenberg, R.; Cohen, A.; Ein-Mor, E.; Jacobs, J.M. Physical activity, function, and longevity among the very old. Arch. Int. Med. 2009, 169, 1476–1483. [Google Scholar] [CrossRef]
- Yeom, H.A.; Fleury, J.; Keller, C. Risk factors for mobility limitation in community-dwelling older adults: A social ecological perspective. Geriatr. Nurs. 2008, 29, 133–140. [Google Scholar] [CrossRef]
- Hirvensalo, M.; Rantanen, T.; Heikkinen, E. Mobility difficulties and physical activity as predictors of mortality and loss of independence in the community-living older population. J. Am. Geriatr. Soc. 2000, 48, 493–498. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Yan, K. Indoor Location Based on Radio and Sensor Measurements. IEEE Sens. J. 2021, 21, 25090–25097. [Google Scholar] [CrossRef]
- Bai, L.; Ciravegna, F.; Bond, R.; Mulvenna, M. A Low Cost Indoor Positioning System Using Bluetooth Low Energy. IEEE Access 2020, 8, 136858–136871. [Google Scholar] [CrossRef]
- Minici, D.; Cola, G.; Giordano, A.; Antoci, S.; Girardi, E.; Di Bari, M.; Avvenuti, M. Towards automated assessment of frailty status using a wrist-worn device. IEEE J. Biomed. Health Inform. 2021, 26, 1013–1022. [Google Scholar] [CrossRef] [PubMed]
- Plaza, S.L.; Villadangos Carrizo, J.M.; García Domínguez, J.J.; Jiménez Martín, A.; Gómez, D.G. FrailWear: A Wearable IoT Device for Daily Activity Monitoring of Elderly Patients. In Proceedings of the XXXV Conference on Design of Circuits and Integrated Systems (DCIS) 2020, Segovia, Spain, 18–20 November 2020; pp. 1–6. [Google Scholar] [CrossRef]
- Shum, L.C.; Faieghi, R.; Borsook, T.; Faruk, T.; Kassam, S.; Nabavi, H.; Spasojevic, S.; Tung, J.; Khan, S.S.; Iaboni, A. Indoor Location Data for Tracking Human Behaviours: A Scoping Review. Sensors 2022, 22, 1220. [Google Scholar] [CrossRef] [PubMed]
- Alam, F.; Faulkner, N.; Parr, B. Device-Free Location: A Review of Non-RF Techniques for Unobtrusive Indoor Positioning. IEEE Int. Things J. 2021, 8, 4228–4249. [Google Scholar] [CrossRef]
- Yint Tun, S.Y.; Madanian, S.; Mirza, F. Internet of things (IoT) applications for elderly care: A reflective review. Aging Clin. Exp. Res. 2021, 33, 855–867. [Google Scholar] [CrossRef]
- Panhwar, Y.; Naghdy, F.; Naghdy, G.; Stirling, D.; Potter, J. Assessment of frailty: A survey of quantitative and clinical methods. BMC Biomed. Eng. 2019, 1, 7. [Google Scholar] [CrossRef]
- Roberts, L.M.; Jaeger, B.C.; Baptista, L.C.; Harper, S.A.; Gardner, A.K.; Jackson, E.A.; Pekmezi, D.; Sandesara, B.; Manini, T.M.; Anton, S.T.; et al. Wearable Technology To Reduce Sedentary Behavior And CVD Risk In Older Adults: A Pilot Randomized Clinical Trial. Clin. Interv. Aging 2019, 14, 1817–1828. [Google Scholar] [CrossRef]
- Yuki, A.; Lee, S.; Kim, H.; Kozakai, R.; Ando, F.; Shimokata, H. Relationship between physical activity and brain atrophy progression. Med. Sci. Sports Exerc. 2012, 44, 2362–2368. [Google Scholar] [CrossRef]
- Rapp, K.; Mikolaizak, S.; Rothenbacher, D.; Denkinger, M.D.; Klenk, J. Prospective analysis of time out-of-home and objectively measured walking duration during a week in a large cohort of older adults. Eur. Rev. Aging Phys. Act. 2018, 15, 8. [Google Scholar] [CrossRef] [PubMed]
- Mahant, P.R.; Stacy, M.A. Movement disorders and normal aging. Neurol. Clin. 2001, 19, 553–563. [Google Scholar] [CrossRef]
- Ramezani, R.; Zhang, W.; Xie, Z.; Shen, J.; Elashoff, D.; Roberts, P.; Stanton, A.; Eslami, M.; Wenger, N.; Sarrafzadeh, M.; et al. A Combination of Indoor Localization and Wearable Sensor–Based Physical Activity Recognition to Assess Older Patients Undergoing Subacute Rehabilitation: Baseline Study Results. JMIR mHealth uHealth 2019, 7, e14090. [Google Scholar] [CrossRef] [PubMed]
- Fillekes, M.P.; Kim, E.-K.; Trumpf, R.; Zijlstra, W.; Giannouli, E.; Weibel, R. Assessing Older Adults’ Daily Mobility: A Comparison of GPS-Derived and Self-Reported Mobility Indicators. Sensors 2019, 19, 4551. [Google Scholar] [CrossRef]
- VandeWeerd, C.; Yalcin, A.; Aden-Buie, G.; Wang, Y.; Roberts, M.; Mahser, N.; Fnu, C.; Fabiano, D. HomeSense: Design of an ambient home health and wellness monitoring platform for older adults. Health Technol. 2020, 10, 1291–1309. [Google Scholar] [CrossRef]
- Hyväri, S.; Elo, S.; Kukkohovi, S.; Lotvonen, S. Utilizing activity sensors to identify the behavioural activity patterns of elderly home care clients. Disabil. Rehabil. Assist. Technol. 2022, 1–10. [Google Scholar] [CrossRef]
- Forkan, A.R.M.; Branch, P.; Jayaramana, P.P.; Ferretto, A. Halley Assist: A Personalised Internet of Things Technology to Assist the Elderly in Daily Living. In Proceedings of the 52nd Hawaii International Conference on System Sciences, Maui, HI, USA, 8–11 January 2019. [Google Scholar]
- Alharbia, M.; Straitona, N.; Smithb, S.; Neubeckc, L.; Gallaghera, R. Data management and wearables in older adults: A systematic review. Maturitas 2019, 124, 100–110. [Google Scholar] [CrossRef]
- Leirós-Rodríguez, R.; García-Soidán, J.L.; Romo-Pérez, V. Analyzing the Use of Accelerometers as a Method of Early Diagnosis of Alterations in Balance in Elderly People: A Systematic Review. Sensors 2019, 19, 3883. [Google Scholar] [CrossRef]
- Wipfli, B.; Rice, S.P.M.; Olson, R.; Ha, K.; Trullinger-Dwyer, C.; Bodner, T. Describing Physical Activity Patterns of Truck Drivers Using Actigraphy. Saf. Health Work. 2023, 14, 340–346. [Google Scholar] [CrossRef]
- Ummels, D.; Bijnens, W.; Aarts, J.; Meijer, K.; Beurskens, A.J.; Beekman, E. The Validation of a Pocket Worn Activity Tracker for Step Count and Physical Behavior in Older Adults during Simulated Activities of Daily Living. Gerontol. Geriatr. Med. 2020, 6, 2333721420951732. [Google Scholar] [CrossRef]
- Chen, Y.L.; Yang, I.J.; Fu, L.C.; Lai, J.S.; Liang, H.W.; Lu, L. IMU-Based Estimation of Lower Limb Motion Trajectory with Graph Convolution Network. IEEE Sens. J. 2021, 21, 24549–24557. [Google Scholar] [CrossRef]
- Silsupadol, P.; Prupetkaew, P.; Kamnardsiri, T.; Lugade, V. Smartphone-based assessment of gait during straight walking, turning, and walking speed modulation in laboratory and free-living environments. IEEE J. Biomed. Health Inform. 2019, 24, 1188–1195. [Google Scholar] [CrossRef] [PubMed]
- Ramanujam, E.; Perumal, T.; Padmavathi, S. Human Activity Recognition With Smartphone and Wearable Sensors Using Deep Learning Techniques: A Review. IEEE Sens. J. 2021, 21, 13029–13040. [Google Scholar] [CrossRef]
- Joosen, P.; Piette, D.; Buekers, J.; Taelman, J.; Berckmans, D.; Boever, P. A smartphone-based solution to monitor daily physical activity in a care home. J. Telemed. Telecare 2019, 25, 611–622. [Google Scholar] [CrossRef]
- NGIMU, X-IO. Available online: http://x-io.co.uk/ngimu/ (accessed on 31 July 2023).
- Gualda, D.; Pérez-Rubio, M.C.; Ureña, J.; Pérez-Bachiller, S.; Villadangos, J.M.; Hernández, Á.; García, J.J.; Jiménez, A. LOCATE-US: Indoor Positioning for Mobile Devices Using Encoded Ultrasonic Signals, Inertial Sensors and Graph-Matching. Sensors 2021, 21, 1950. [Google Scholar] [CrossRef]
- Munoz–Diaz, E.; Mendiguchia–Gonzalez, A.L. Step Detector and Step Length Estimator for an Inertial Pocket Navigation System. In Proceedings of the International Conference of Indoor Positioning and Indoor Navigation (IPIN) 2014, Busan, Republic of Korea, 27–30 October 2014; pp. 105–110. [Google Scholar] [CrossRef]
- TP-LINKTL-WR802N. Available online: https://www.tp-link.com/en/home-networking/wifi-router/tl-wr820n/#specifications (accessed on 31 July 2023).
- STMicroelectronics. STM32F469xx Product Datasheet. 2021. DS11189. pp. 1–220. Available online: https://www.st.com/resource/en/datasheet/stm32f469ae.pdf (accessed on 17 October 2023).
- CEVA. BNO08X Data Sheet. 2023. 1000-3927 v1.16. pp. 1–59. Available online: https://www.ceva-dsp.com/wp-content/uploads/2019/10/BNO080_085-Datasheet.pdf (accessed on 17 October 2023).
- STMicroelectronics. LPS22HB MEMS Nano Pressure Sensor: 260–1260 hPa Absolute Digital Output Barometer. 2017. D027083. pp. 1–49. Available online: https://www.st.com/resource/en/datasheet/lps22hb.pdf (accessed on 17 October 2023).
- Vishay Semiconductors. TSOP7000. IR Receiver for High Data Rate PCM at 455 kHz. 2003. 82147. pp. 1–7. Available online: https://www.tme.eu/Document/0a7701c716b24d147be2f244f54bf755/tsop7000.pdf (accessed on 17 October 2023).
- Knowles. SPU0414HR5H-SB Product Data Sheet. 2012. Revision: E. pp. 1–11. Available online: https://mm.digikey.com/Volume0/opasdata/d220001/medias/docus/1220/SPU0414HR5H-SB.pdf (accessed on 17 October 2023).


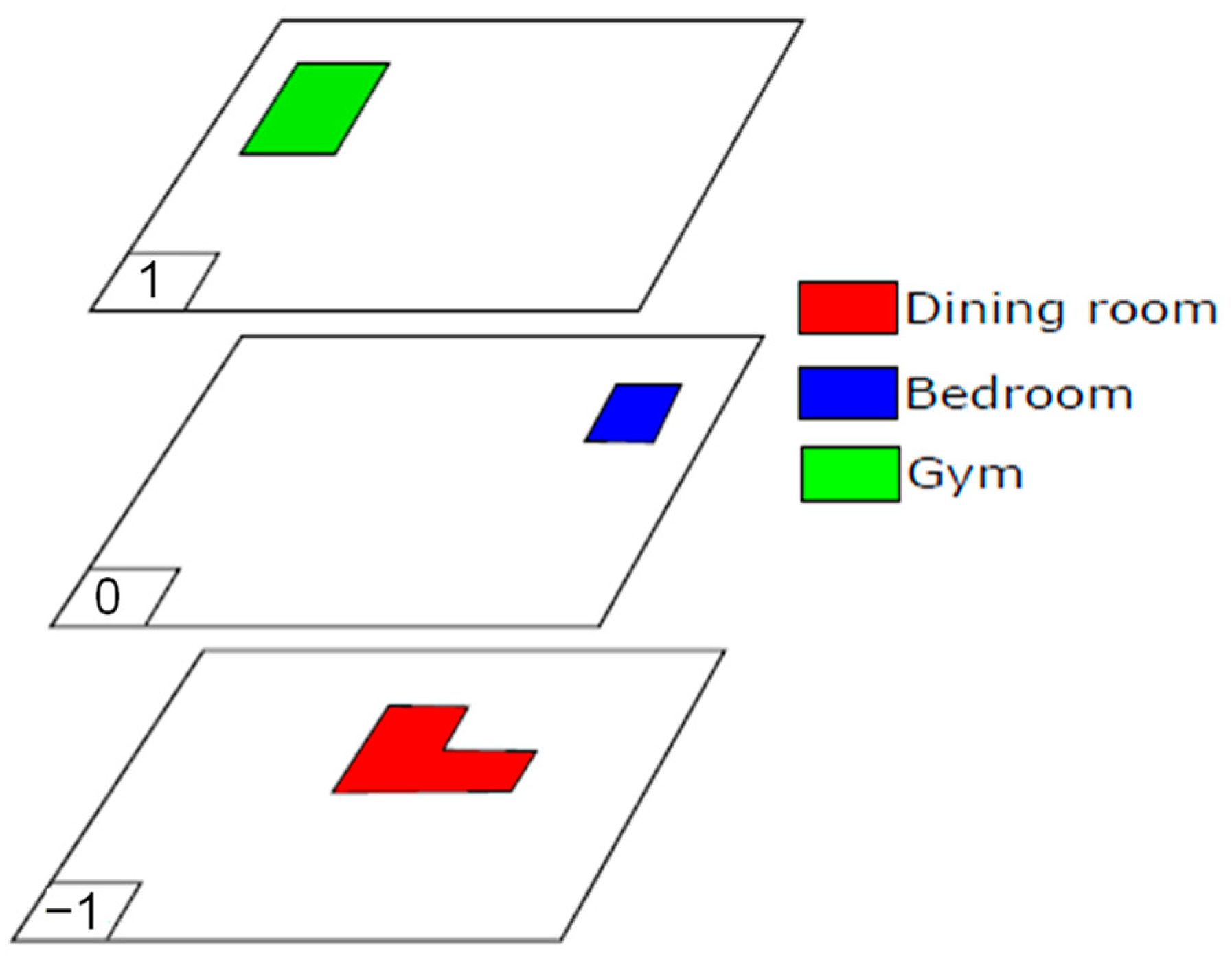



| Floor | Facilities |
|---|---|
| −1 | 2 living rooms, chapel, dining room and garden |
| 0 | 20 bedrooms, living room with TV and terrace |
| 1 | 27 bedrooms, terrace, living room and gym |
| 2 | 18 bedrooms and living room |
| 58 d | 365 d | 120 d | 15 d | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T1 (20 d) | T2 (14 d) | T3 (11 d) | T4 (5 d) | T5 (5 d) | ||||||||||||||
| Parameter | Avg | SD | Avg | SD | Avg | SD | Avg | SD | Avg | SD | ||||||||
| Walking hours | 0.81 | 0.30 | 0.92 | 0.45 | 1.34 | 0.39 | 1.00 | 0.34 | 0.58 | 0.47 | ||||||||
| Sitting hours | 9.00 | 1.45 | 8.95 | 1.41 | 10.62 | 1.45 | 11.30 | 1.48 | 11.52 | 0.33 | ||||||||
| Lying hours | 3.00 | 1.08 | 2.69 | 1.61 | 2.50 | 1.06 | 1.13 | 1.24 | 0.95 | 0.45 | ||||||||
| Steps per day | 4611 | 1354 | 4737 | 1863 | 4612 | 1619 | 3954 | 1320 | 2174 | 1932 | ||||||||
| Speed (m/s) | 1.03 | 0.07 | 1.00 | 0.12 | 1.00 | 0.06 | 0.97 | 0.08 | 0.75 | 0.22 | ||||||||
| 58 d | 89 d | 286 d | 90 d | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T1 (20 d) | T2 (13 d) | T3 (8 d) | T4 (8 d) | T5 (4 d) | ||||||||||||||
| Parameter | Avg | SD | Avg | SD | Avg | SD | Avg | SD | Avg | SD | ||||||||
| Walking hours | 1.81 | 0.72 | 1.95 | 0.95 | 1.05 | 0.50 | 1.02 | 0.58 | 0.63 | 0.18 | ||||||||
| Sitting hours | 9.15 | 1.55 | 10.76 | 0.96 | 9.17 | 0.95 | 11.38 | 2.42 | 8.30 | 0.43 | ||||||||
| Lying hours | 1.01 | 0.69 | 0.87 | 0.49 | 1.40 | 0.74 | 1.69 | 1.29 | 1.53 | 1.37 | ||||||||
| Steps per day | 5595 | 2158 | 6080 | 2672 | 3238 | 1586 | 2976 | 1699 | 1900 | 495 | ||||||||
| Speed (m/s) | 0.98 | 0.09 | 0.98 | 0.06 | 0.81 | 0.17 | 0.76 | 0.08 | 0.90 | 0.04 | ||||||||
| 94 d | 122 d | 17 d | 38 d | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T1 (11 d) | T2 (26 d) | T3 (11 d) | T4 (8 d) | T5 (7 d) | ||||||||||||||
| Parameter | Avg | SD | Avg | SD | Avg | SD | Avg | SD | Avg | SD | ||||||||
| Walking hours | 0.43 | 0.08 | 0.42 | 0.11 | 0.23 | 0.12 | 0.10 | 0.10 | 0.20 | 0.18 | ||||||||
| Sitting hours | 9.47 | 0.58 | 9.44 | 0.62 | 9.38 | 0.53 | 9.03 | 0.76 | 9.64 | 0.77 | ||||||||
| Lying hours | 1.60 | 0.39 | 1.62 | 0.37 | 1.87 | 0.41 | 1.88 | 0.80 | 1.78 | 0.45 | ||||||||
| Steps per day | 1282 | 250 | 1175 | 549 | 800 | 348 | 56 | 50 | 629 | 465 | ||||||||
| Speed (m/s) | 0.56 | 0.02 | 0.51 | 0.07 | 0.61 | 0.09 | 0.55 | 0.27 | 0.61 | 0.20 | ||||||||
| Floor changes per day | 7.80 | 1.52 | 7.50 | 2.09 | 6.91 | 1.64 | 7.00 | 1.26 | 7.14 | 1.35 | ||||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lluva-Plaza, S.; Jiménez-Martín, A.; Gualda-Gómez, D.; Villadangos-Carrizo, J.M.; García-Domínguez, J.J. Multisensory System for Long-Term Activity Monitoring to Facilitate Aging-in-Place. Sensors 2023, 23, 8646. https://doi.org/10.3390/s23208646
Lluva-Plaza S, Jiménez-Martín A, Gualda-Gómez D, Villadangos-Carrizo JM, García-Domínguez JJ. Multisensory System for Long-Term Activity Monitoring to Facilitate Aging-in-Place. Sensors. 2023; 23(20):8646. https://doi.org/10.3390/s23208646
Chicago/Turabian StyleLluva-Plaza, Sergio, Ana Jiménez-Martín, David Gualda-Gómez, José Manuel Villadangos-Carrizo, and Juan Jesús García-Domínguez. 2023. "Multisensory System for Long-Term Activity Monitoring to Facilitate Aging-in-Place" Sensors 23, no. 20: 8646. https://doi.org/10.3390/s23208646
APA StyleLluva-Plaza, S., Jiménez-Martín, A., Gualda-Gómez, D., Villadangos-Carrizo, J. M., & García-Domínguez, J. J. (2023). Multisensory System for Long-Term Activity Monitoring to Facilitate Aging-in-Place. Sensors, 23(20), 8646. https://doi.org/10.3390/s23208646





