The Use of Wearable Devices to Measure Sedentary Behavior during COVID-19: Systematic Review and Future Recommendations
Abstract
:1. Introduction
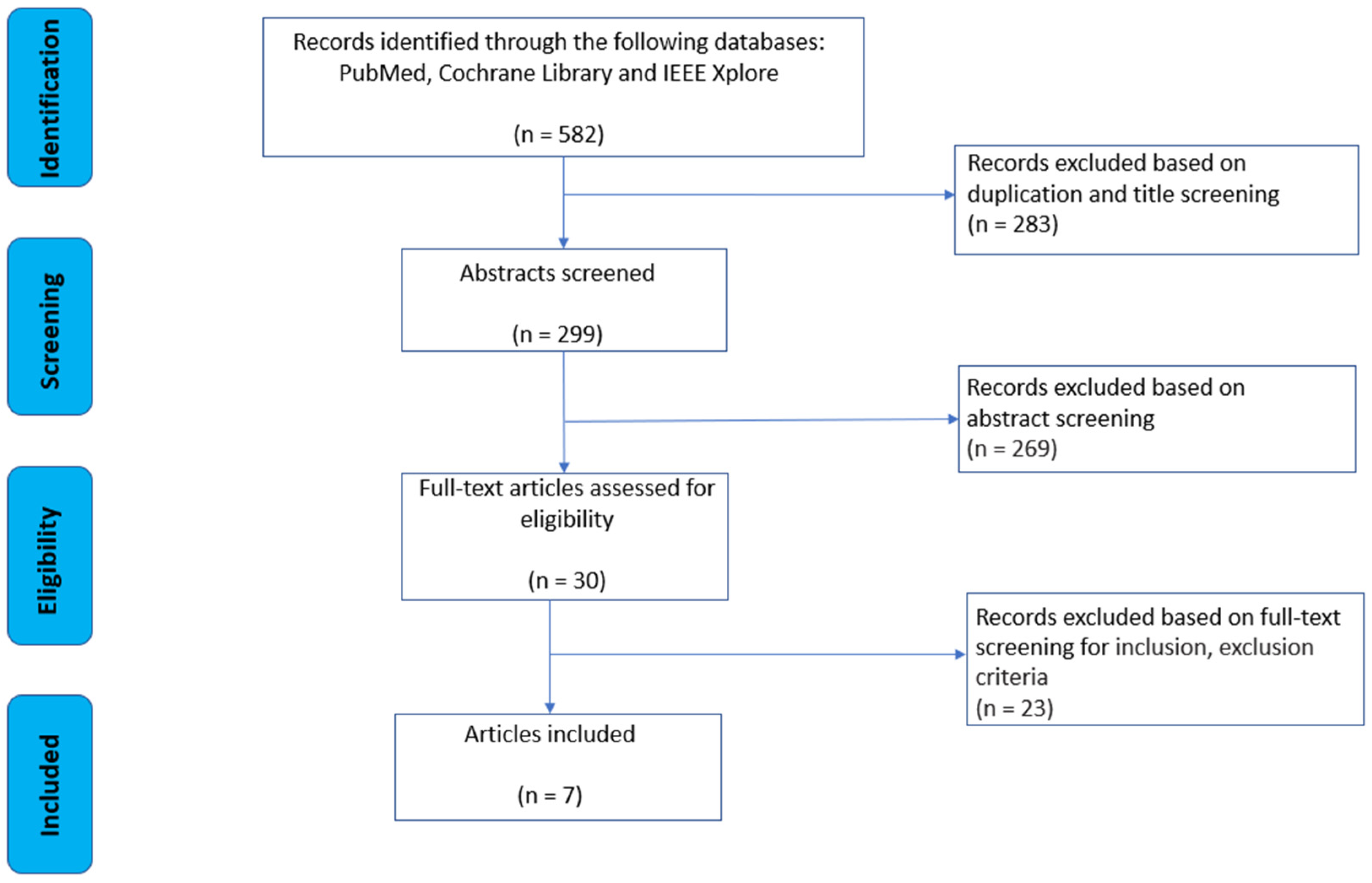
2. Methods
2.1. Search Strategy
2.2. Study Selection Strategy
- (1)
- Articles published in English.
- (2)
- Full original research articles published in peer-reviewed scientific journals.
- (3)
- Studies involving healthy adult human participants, aged between 18 and 75 years, with no pre-existing health conditions.
- (4)
- Studies focused on measuring sedentary behavior related to COVID-19 using characteristics derived from wearable devices or body-worn sensors.
- (5)
- Wearable devices need to be small, portable, easy to use, and unobtrusive for the desired analysis.
- (1)
- Studies that used animal models.
- (2)
- Conference papers.
- (3)
- Studies unrelated to sedentary behavior and COVID-19.
- (4)
- Adults with chronic lifestyle illnesses were excluded, as they might have fitness plans, dietician recommendations leading to physical mobility issues, or other physiological considerations, mental health issues, or health-related motivations.
- (5)
- Studies that did not primarily focus on wearable device analysis.
- (6)
- Studies that utilized invasive wearables.
- (7)
- Studies that employed wearables solely to track working status.
- (8)
- Studies that only proposed protocols without presenting results.
- (9)
- Studies primarily focused on virus spread prevention and social distancing.
- (10)
- Studies concentrating on robotics were also excluded.
2.3. Data Extraction
2.4. Methodological Quality
3. Results
3.1. Search Results
3.2. Study Characteristics and Reported Limitations
3.3. Study Parameters and Outcome Measures
3.3.1. Sensor Type and Body Location
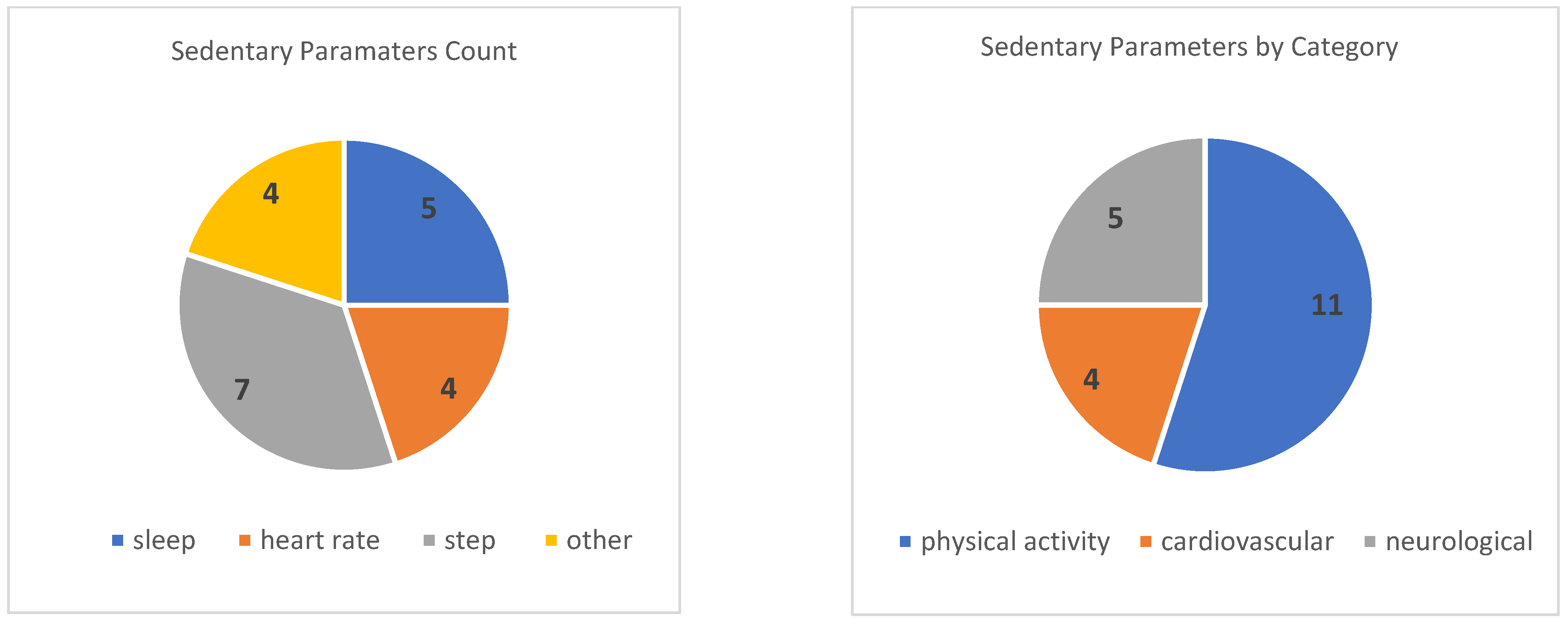
3.3.2. Key Sedentary Parameters and Assessment Procedures
3.4. Methodological Quality
4. Discussion
- (1)
- Sample selection: Several studies relied on convenience samples, which may not be representative of the wider population [20,23,24]. Additionally, some studies had skewed gender ratios [20] or overrepresented certain ethnic groups [19]. These limitations limit the generalizability of the findings to the wider population.
- (2)
- Data collection methods: Some studies used consumer-grade wearables to measure physical activity and sleep [21,22,24]. While these devices are convenient and widely used, they may be less valid than research-grade devices for assessing activity intensity and sleep quality [21]. On the other hand, these devices present a multitude of advantages for health research. They are not only more cost-effective than premium research devices [36], but also boast comfort in wear [37], making them easily accessible to consumers at an affordable price [38]. Additionally, some studies lacked pre-lockdown data for comparison [20,23], which makes it difficult to determine the true impact of COVID-19 on physical activity and sleep.
- (3)
- Data analysis: Some studies made assumptions about the linearity of relationships or the constancy of model parameters and were unable to use certain data analysis techniques due to the small sample size or noisy data [18]. These methodological limitations may have affected the accuracy of the findings.
4.1. Future Directions
- Telehealth Integration: We now comprehend the negative repercussions of extended waiting periods on overall health during the COVID-19 lockdowns and the burden in post-pandemic times [39]. One way to uphold preventative medicine measures and potentially bridge this gap may be to leverage wearable devices. Wearable devices have the potential to seamlessly integrate with telehealth platforms, enabling healthcare practitioners to remotely monitor sedentary behavior. This integration would empower healthcare professionals to offer individualized recommendations and interventions aligned with individuals’ well-being, thereby amplifying the effectiveness of remote healthcare services. Simultaneously, these wearable devices possess the capability to meticulously trace prolonged sedentary patterns, facilitating the discernment of overarching trends and their associations with diverse health consequences. This valuable insight could significantly inform the creation of targeted interventions and strategies for fostering behavioral changes.
- Self-Psychological and Emotional Assessment: The past few years have highlighted the role of physical activity to alleviate psychosocial challenges during a lockdown [40]. Advanced wearables equipped with sensors can record objective physiological indicators such as heart rate variability and electrodermal activity, providing quantifiable insights into stress levels and emotional well-being [41]. In conjunction with other tools, such as a mood diary, or a self-reported emotional scale, wearables may offer another layer of self-awareness for people to assess emotional shifts in line with sedentary behavior and take preventative measures during lockdowns.
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Guo, Y.R.; Cao, Q.D.; Hong, Z.S.; Tan, Y.Y.; Chen, S.D.; Jin, H.J.; Tan, K.S.; Wang, D.Y.; Yan, Y. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak—An update on the status. Mil. Med. Res. 2020, 7, 11. [Google Scholar] [CrossRef] [PubMed]
- Puhl, A.C.; Lane, T.R.; Ekins, S. Learning from COVID-19: How drug hunters can prepare for the next pandemic. Drug Discov. Today 2023, 28, 103723. [Google Scholar] [CrossRef] [PubMed]
- Nour, T.Y.; Altintaş, K.H. Effect of the COVID-19 pandemic on obesity and its risk factors: A systematic review. BMC Public Health 2023, 23, 1018. [Google Scholar] [CrossRef]
- Bames, J.; Behrens, T.K.; Benden, M.E.; Biddle, S.; Bond, D.; Brassard, P.; Brown, H.; Carr, L.; Carson, V.; Chaput, J.; et al. Standardized use of the terms “sedentary” and “sedentary behaviours”. Appl. Physiol. Nutr. Metab. Physiol. Appl. Nutr. Metab. 2012, 37, 540–542. [Google Scholar]
- Thorp, A.A. Deleterious associations of sitting time and television viewing time with cardiometabolic risk biomarkers: Australian Diabetes, Obesity and Lifestyle (AusDiab) study 2004–2005. Diabetes Care 2010, 33, 327–334. [Google Scholar] [CrossRef] [PubMed]
- Proper, K.I.; Singh, A.S.; van Mechelen, W.; Chinapaw, M.J. Sedentary Behaviors and Health Outcomes Among Adults: A Systematic Review of Prospective Studies. Am. J. Prev. Med. 2011, 40, 174–182. [Google Scholar] [CrossRef]
- Wilmot, E.G.; Edwardson, C.L.; Achana, F.A.; Davies, M.J.; Gorely, T.; Gray, L.J.; Khunti, K.; Yates, T.; Biddle, S.J.H. Sedentary time in adults and the association with diabetes, cardiovascular disease and death: Systematic review and meta-analysis. Diabetologia 2012, 55, 2895–2905. [Google Scholar] [CrossRef]
- Lynch, B.M. Sedentary Behavior and Cancer: A Systematic Review of the Literature and Proposed Biological Mechanisms. Cancer Epidemiol. Biomark. Prev. 2010, 19, 2691–2709. [Google Scholar] [CrossRef]
- Biswas, A.; Oh, P.I.; Faulkner, G.E.; Bajaj, R.R.; Silver, M.A.; Mitchell, M.S.; Alter, D.A. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: A systematic review and meta-analysis. Ann. Intern. Med. 2015, 162, 123–132. [Google Scholar] [CrossRef]
- Matthews, C.E.; George, S.M.; Moore, S.C.; Bowles, H.R.; Blair, A.; Park, Y.; Troiano, R.P.; Hollenbeck, A.; Schatzkin, A. Amount of time spent in sedentary behaviors and cause-specific mortality in US adults. Am. J. Clin. Nutr. 2012, 95, 437–445. [Google Scholar] [CrossRef]
- Zenic, N.; Taiar, R.; Gilic, B.; Blazevic, M.; Maric, D.; Pojskic, H.; Sekulic, D. Levels and Changes of Physical Activity in Adolescents during the COVID-19 Pandemic: Contextualizing Urban vs. Rural Living Environment. Appl. Sci. 2020, 10, 3997. [Google Scholar] [CrossRef]
- Xiang, M.; Zhang, Z.; Kuwahara, K. Impact of COVID-19 pandemic on children and adolescents’ lifestyle behavior larger than expected. Prog. Cardiovasc. Dis. 2020, 63, 531–532. [Google Scholar] [CrossRef] [PubMed]
- Ng, K.; Cooper, J.; McHale, F.; Clifford, J.; Woods, C. Barriers and facilitators to changes in adolescent physical activity during COVID-19. BMJ Open Sport Exerc. Med. 2020, 6, e000919. [Google Scholar] [CrossRef] [PubMed]
- Gilic, B.; Ostojic, L.; Corluka, M.; Volaric, T.; Sekulic, D. Contextualizing Parental/Familial Influence on Physical Activity in Adolescents before and during COVID-19 Pandemic: A Prospective Analysis. Children 2020, 7, 125. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.-Y.; Park, G.; Lee, S.-A.; Nam, Y. Analysis of Machine Learning-Based Assessment for Elbow Spasticity Using Inertial Sensors. Sensors 2020, 20, 1622. [Google Scholar] [CrossRef] [PubMed]
- Brognara, L.; Palumbo, P.; Grimm, B.; Palmerini, L. Assessing Gait in Parkinson’s Disease Using Wearable Motion Sensors: A Systematic Review. Diseases 2019, 7, 18. [Google Scholar] [CrossRef] [PubMed]
- Evenson, K.R.; Goto, M.M.; Furberg, R.D. Systematic review of the validity and reliability of consumer-wearable activity trackers. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 159. [Google Scholar] [CrossRef]
- Hojjatinia, S.; Lee, A.M.; Hojjatinia, S.; Lagoa, C.M.; Brunke-Reese, D.; Conroy, D.E. Physical Activity Dynamics During a Digital Messaging Intervention Changed After the Pandemic Declaration. Ann. Behav. Med. 2022, 56, 1188–1198. [Google Scholar] [CrossRef]
- Gilley, K.N.; Baroudi, L.; Yu, M.; Gainsburg, I.; Reddy, N.; Bradley, C.; Cislo, C.; Rozwadowski, M.L.; Clingan, C.A.; DeMoss, M.S.; et al. Risk Factors for COVID-19 in College Students Identified by Physical, Mental, and Social Health Reported During the Fall 2020 Semester: Observational Study Using the Roadmap App and Fitbit Wearable Sensors. JMIR Ment. Health 2022, 9, e34645. [Google Scholar] [CrossRef]
- Massar, S.A.A.; Ng, A.S.C.; Soon, C.S.; Ong, J.L.; Chua, X.Y.; Chee, N.I.Y.N.; Lee, T.S.; Chee, M.W.L. Reopening after lockdown: The influence of working-from-home and digital device use on sleep, physical activity, and wellbeing following COVID-19 lockdown and reopening. Sleep 2022, 45, zsab250. [Google Scholar] [CrossRef]
- Mair, J.L.; Hayes, L.D.; Campbell, A.K.; Buchan, D.S.; Easton, C.; Sculthorpe, N. A Personalized Smartphone-Delivered Just-in-time Adaptive Intervention (JitaBug) to Increase Physical Activity in Older Adults: Mixed Methods Feasibility Study. JMIR Form. Res. 2022, 6, e34662. [Google Scholar] [CrossRef]
- Leone, A.; Rescio, G.; Diraco, G.; Manni, A.; Siciliano, P.; Caroppo, A. Ambient and Wearable Sensor Technologies for Energy Expenditure Quantification of Ageing Adults. Sensors 2022, 22, 4893. [Google Scholar] [CrossRef] [PubMed]
- Capodilupo, E.R.; Miller, D.J. Changes in health promoting behavior during COVID-19 physical distancing: Utilizing wearable technology to examine trends in sleep, activity, and cardiovascular indicators of health. PLoS ONE 2021, 16, e0256063. [Google Scholar] [CrossRef] [PubMed]
- Ong, J.L.; Lau, T.; Massar, S.A.A.; Chong, Z.T.; Ng, B.K.L.; Koek, D.; Zhao, W.; Yeo, B.T.T.; Cheong, K.; Chee, M.W.L. COVID-19-related mobility reduction: Heterogenous effects on sleep and physical activity rhythms. Sleep 2021, 44, zsaa179. [Google Scholar] [CrossRef]
- Williams, P.V.; Fasano, M.B.; Fleisher, T. Preparing the Allergist/Immunologist for the Next Pandemic. J. Allergy Clin. Immunol. Pract. 2023, 11, 3373–3379. [Google Scholar] [CrossRef] [PubMed]
- Kuiken, T.; Fouchier, R.A.; Koopmans, M.P. Being ready for the next influenza pandemic? Lancet Infect. Dis. 2023, 23, 398–399. [Google Scholar] [CrossRef] [PubMed]
- Ricotta, E.E.; Rid, A.; Cohen, I.G.; Evans, N.G. Observational studies must be reformed before the next pandemic. Nat. Med. 2023, 29, 1903–1905. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. Ann. Intern. Med. 2009, 151, W-65–W-94. [Google Scholar] [CrossRef]
- Johnson, N.; Phillips, M. Rayyan for systematic reviews. J. Electron. Resour. Librariansh. 2018, 30, 46–48. [Google Scholar] [CrossRef]
- Benson, L.C.; Clermont, C.A.; Bošnjak, E.; Ferber, R. The use of wearable devices for walking and running gait analysis outside of the lab: A systematic review. Gait Posture 2018, 63, 124–138. [Google Scholar] [CrossRef]
- Campos, S.; Doxey, J.; Hammond, D. Nutrition labels on pre-packaged foods: A systematic review. Public Health Nutr. 2011, 14, 1496–1506. [Google Scholar] [CrossRef] [PubMed]
- Remuzzi, A.; Remuzzi, G. COVID-19 and Italy: What next? Lancet 2020, 395, 1225–1228. [Google Scholar] [CrossRef] [PubMed]
- Prill, R.; Walter, M.; Królikowska, A.; Becker, R. A Systematic Review of Diagnostic Accuracy and Clinical Applications of Wearable Movement Sensors for Knee Joint Rehabilitation. Sensors 2021, 21, 8221. [Google Scholar] [CrossRef] [PubMed]
- Weizman, Y.; Tirosh, O.; Fuss, F.K.; Tan, A.M.; Rutz, E. Recent State of Wearable IMU Sensors Use in People Living with Spasticity: A Systematic Review. Sensors 2022, 22, 1791. [Google Scholar] [CrossRef] [PubMed]
- Düking, P.; Fuss, F.K.; Holmberg, H.-C.; Sperlich, B. Recommendations for Assessment of the Reliability, Sensitivity, and Validity of Data Provided by Wearable Sensors Designed for Monitoring Physical Activity. JMIR Mhealth Uhealth 2018, 6, e102. [Google Scholar] [CrossRef] [PubMed]
- Carpenter, A.; Frontera, A. Smart-watches: A potential challenger to the implantable loop recorder? Europace 2016, 18, 791–793. [Google Scholar] [CrossRef] [PubMed]
- Jia, Y.; Wang, W.; Wen, D.; Liang, L.; Gao, L.; Lei, J. Perceived user preferences and usability evaluation of mainstream wearable devices for health monitoring. PeerJ 2018, 6, e5350. [Google Scholar] [CrossRef]
- Hickey, A.M.; Freedson, P.S. Utility of Consumer Physical Activity Trackers as an Intervention Tool in Cardiovascular Disease Prevention and Treatment. Prog. Cardiovasc. Dis. 2016, 58, 613–619. [Google Scholar] [CrossRef]
- Li, J.; Zhao, M.; She, H.; Chandra, A. The impact of the COVID-19 pandemic lockdown on rhegmatogenous retinal detachment services—Experiences from the Tongren eye center in Beijing. PLoS ONE 2021, 16, e0254751. [Google Scholar] [CrossRef]
- Alonso-Martínez, A.M.; Ramírez-Vélez, R.; García-Alonso, Y.; Izquierdo, M.; García-Hermoso, A. Physical Activity, Sedentary Behavior, Sleep and Self-Regulation in Spanish Preschoolers during the COVID-19 Lockdown. Int. J. Environ. Res. Public Heal. 2021, 18, 693. [Google Scholar] [CrossRef]
- Klimek, A.; Mannheim, I.; Schouten, G.; Wouters, E.J.M.; Peeters, M.W.H. Wearables measuring electrodermal activity to assess perceived stress in care: A scoping review. Acta Neuropsychiatr. 2023, 1–11. [Google Scholar] [CrossRef] [PubMed]
| Author [18,19,20,21,22,23,24] | Aim | Population Recruitment Characteristic | Selection Criteria | Participant Characteristics |
|---|---|---|---|---|
| Hojjatinia et al., 2022 [18] | To explore the effect of the COVID-19 pandemic on the dynamics of physical activity responses to digital message interventions. | Young adults | Inclusion Criteria: Ambulatory individuals aged 18–29 with no functional limitations, a visual impairment that hinders smartphone use, and fluency in English (both verbal and written). Participants must own a smartphone running iPhone iOS v10.0 or later or Android OS v7 or later and be willing to install the Random AIM and Fitbit apps. Exclusion Criteria: individuals engaging in 90 min or more of moderate or higher intensity physical activity per week, participating in mandatory physical activity programs, relying on mobility-assistive devices, diagnosed with cancer, cardiovascular disease, type I or type II diabetes, or metabolic syndrome, pregnant or planning to become pregnant in the next 6 months, or having any contradictions to physical activity based on the Physical Activity Readiness Questionnaire were excluded. | N: 28; Gender: M/F: 10/12 Mean age: 22.2 ± 1.7 |
| Gilley et al., 2022 [19] | 1. Evaluate self-reported physical, mental, and social health outcomes based on COVID-19 status. 2. Measure physical activity using consumer-grade wearable sensors (Fitbit). 3. Identify risk factors linked to COVID-19 positivity in a population of college students before the vaccine was available. | College students | Inclusion Criteria: Participants aged 18 years or older who are confirmed undergraduate or graduate students at the University of Michigan (whether on campus or at home). They must be capable of providing informed consent digitally, comfortable with reading and speaking English, and have access to the necessary resources for participating in an mHealth technology-based intervention (such as a smartphone or tablet device and internet access). Participants should also be willing to use their personal equipment or the Internet for the study. Exclusion Criteria: participants who did not complete the final (exit) assessment, did not complete a minimum of two monthly assessments, did not report a COVID-19 diagnosis, or did not wear the Fitbit device. | N: 1997; Gender: M/F/Other: 613/1367/16; Mean age: not reported (age ≥ 18) |
| Massar et al., 2021 [20] | To examine the changes in physical activity behaviors during the reopening phase, specifically exploring the potential influences of continued remote work and smartphone usage. | University students and staff | Inclusion: not reported Exclusion: not reported | N: 198; Gender: M/F: 61/137; Mean age: 26.1 ± 5.8; |
| Mair et al., 2022 [21] | This study aims to provide a comprehensive description of JitaBug, a personalized Just-in-Time Adaptive Intervention (JITAI) delivered through smartphones. The intervention is designed to support older adults in either increasing or maintaining their physical activity levels. Additionally, the feasibility of conducting an effective trial for the JitaBug intervention will be assessed, and the acceptability of JitaBug among older adults in a real-world setting will be explored. | Ambulatory, community-dwelling older adults who use a smartphone | Inclusion: ambulatory, community-dwelling older adults who use a smartphone Exclusion: knee injury participants excluded | N: 31; Gender: M/F: 14/17; Mean age not reported (Age: 56–72 years old) |
| Leone et al., 2022 [22] | In order to develop a platform that is widely accepted by users, two different sensor technologies were utilized to accurately measure and quantify the energy expenditure of older adults. | Aging Adults | Inclusion: not reported Exclusion: not reported | N: 11; Gender: M/F: 6/5; Mean age not reported (Age: 65–73 years old) |
| Capodilupo et al., 2020 [23] | The objective of this study is to measure and analyze changes in sleep/wake behavior, exercise behavior, and physiological markers of health during the period of physical distancing implemented during the COVID-19 pandemic. | WHOOP strap members (US-based) | Inclusion Criteria: Participants must have recorded their sleep for at least 120 out of the 135 days (89% of the days) between January 1 and March 9 in both 2019 and 2020. Additionally, participants should fall within the age range of 18 to 80 years on May 15th, 2020, which was the date when data were extracted for analysis. Exclusion Criteria: there are no specific exclusion criteria mentioned in the provided information. | N: 5436; Gender: M/F: 3900/1536 Mean Age: 40.25 ± 11.33 |
| Ong et al., 2021 [24] | The aim of this study is to analyze sleep and physical activity (PA) data obtained from the “Health Insights Singapore” (hiSG) cohort. | Fitbit users from the Health Insights Singapore (high) study | Inclusion: young working adults between the age 21 and 40 Exclusion: not reported | N: 1824; Gender: M/F: 883/941; Mean age: 30.9 ± 4.6 |
| Author [18,19,20,21,22,23,24] | Sensor Type and Specifications | Location on Body | Calculated Physical Activity Parameters | Sensor Assessment Protocol | Environment | Main Findings |
|---|---|---|---|---|---|---|
| Hojjatinia et al., 2022 [18] | ActiGraph—wGT3X-BT (Stage 1); 30 Hz sampling rate. Fitbit Versa/Versa Lite Smartwatch (Stage 2). | Waist (stage 1), on the participant’s dominant side at the midline of their thigh, wrist (stage 2) | (1) Stage 1: (1) daily step counts were measured as counts per minute, and (2) the mean overall speed of physical activity was calculated. (2) Stage 2: (1) Minute-level step counts and (2) heart rate were recorded. Before and after the pandemic declaration, seven features were extracted separately for weekends and weekdays. These features included initial delay, peak magnitude, peak delay, steady state, rise time, settling time, and effective time. | Stage 1 (Screening Stage): physical activity was measured over a period of 7 consecutive days in the field. Stage 2 (Intervention Stage): Participants who wore the device for at least 5 days with a minimum of 600 min per day and had an average of less than 21.4 min per day of moderate-to-vigorous physical activity (equivalent to 150 min per week) were invited to participate in the second stage of the study. They were asked to continue wearing the device for the next 6 months. | Day to day | Following the declaration of the pandemic, there was a significant decrease in daily step counts on weekdays (Cohen’s d = −1.40), while no significant change was observed on weekends (d = −0.26). The mean overall speed of the response related to physical activity (dominant pole magnitude) did not show significant changes on both weekdays (d = −0.18) and weekends (d = −0.21). However, there was limited consistency in the ranking of specific features of intervention responses before and after the pandemic declaration. |
| Gilley et al., 2022 [19] | Fitbit wristband | Wrist | (1) Number of steps per day, (2) heart rate, and (3) sleep | Participants were provided with Fitbit devices, which were sent to their homes via mail. They received instructions to wear the Fitbit continuously for a minimum of approximately 40 h per week during the 3-month monitoring period. The Fitbit was used to measure their physical activity, heart rate, and sleep patterns throughout this duration. | Day to day | A significant proportion of students (24% with moderate and 49% with severe anxiety levels) reported anxiety according to the State Trait Anxiety Index. About one-third of the students (33%) disclosed having a mental health disorder. Mental health issues were prevalent among the student population, and factors like substance use were linked to increased COVID-19 risk. These findings underscore the need to focus on innovative strategies that promote health and well-being and consider the long-term impacts of COVID-19 on college students. |
| Massar et al., 2021 [20] | Oura Ring; | Finger (not specified) | (1) Sleep, (2) physical activity (step count) | Participants were required to wear the Oura ring consistently throughout the entire duration of both the lockdown and non-lockdown periods, which lasted for a total of 8 weeks. | Day to day | After the lockdown, the reopening phase resulted in noticeable changes, including earlier sleep timing, increased physical activity, and changes in mental well-being. These changes were influenced by factors such as work/study arrangements and patterns of smartphone usage. |
| Mair et al., 2022 [21] | Fitbit (Charge 4); ActiGraph wGTX3-BT accelerometer at 100 Hz | Non-dominant wrist (both sensors) | (1) Daily steps, (2) activity minutes goal | Participants were given Fitbit activity trackers to wear on their nondominant wrist, with no other trackers nearby. They wore these devices continuously for 8 days, 24 h a day, except for bathing or showering. The accelerometers, set to collect data at 100 Hz, were synchronized with GMT and started recording at 6 AM the day after participants received them to ensure full data capture. | Day to day | The study indicates that a smartphone-delivered Just-in-Time Adaptive Intervention (JITAI) is a well-accepted method of supporting physical activity (PA) in older adults within the community. The intervention was found to be feasible overall; however, user feedback suggests that further technical refinements to the JitaBug app are needed to improve its usability, engagement, and user satisfaction before progressing to effectiveness trials. |
| Leone et al., 2022 [22] | Shimmer3; 50 Hz | Chest | Human postures: (1) Standing, (2) Sitting, (3) Bending, (4) Lying down, (5) Walking | Each participant underwent three data acquisition sessions, each consisting of specific protocols involving standing, sitting, bending, and lying tasks. Each task lasted between 30 and 90 s. The protocols included sequences of static postures and walking at various speeds. The goal was to assess the classification performance of each individual sensory node, even in challenging situations that could potentially affect the accuracy of the classification. | Controlled | The study results demonstrated the platform’s ability to accurately measure energy expenditure using different sensing technologies. The wearable sensor achieved an average accuracy of 93.8% in posture classification, while the ambient sensor achieved 93.3% accuracy in walking activity classification. Combining the data from both sensors resulted in an approximately 4% improvement. As a result, the estimated energy expenditure had a relative error of less than 3.2% for each participant, successfully classifying high-level information such as postures and walking activities. These findings support the proposed architecture of the platform in terms of hardware and software. Novelty: “implementation of a platform that provides a novel tool for the automatic quantification of Energy Expenditure (EE)”. |
| Capodilupo et al., 2020 [23] | WHOOP strap | Wrist | (1) Sleep opportunity duration, (2) Social jet lag, (3) Sleep opportunity offset, (4) Sleep duration, (5) Exercise frequency, (6) Exercise type, (7) Exercise intensity, (8) Resting heart rate, (9) Heart rate variability | To assess the immediate changes in health-related behavior, the study defined the period from 1 January 2020 to 9 March 2020 as the baseline period. The period from 10 March 2020 to 15 May 2020 was identified as the physical distancing period, during which restrictions were implemented. | Day to day | The findings indicate that individuals demonstrated improved health-related behaviors, such as increased exercise intensity and longer sleep duration, during the period of physical distancing restrictions. There were positive changes observed in cardiovascular indicators of health. However, it remains unclear whether these changes can be directly attributed to the behavior changes or if other factors were involved. |
| Ong et al., 2021 [24] | Fitbit Ionic | Wrist | (1) Bedtime, (2) Waketime, (3) Time in bed (TIB), (4) Total sleep time (TST), (5) Sleep efficiency, (6) Step counts, (7) Time spent in MVPA, and (8) Resting heart rate | The collected physical activity (PA) data included total daily steps, moderate-to-vigorous physical activity (MVPA) minutes, resting heart rate levels, and 15 min interval step counts. To ensure data accuracy, certain filtering criteria were applied, excluding days with insufficient Fitbit wear time or atypical activity levels. Atypical activity levels were defined by specific thresholds for daily steps and sedentary minutes. The PA data analysis involved an average of 1375 participants at each time point, with an average daily wear time of 18–19 h. | Day to day | During the initial phase of COVID-19 mobility restrictions, physical activity (PA) was found to be more significantly impacted compared to sleep. An evaluation using the RAR (Response Analysis and Reporting) technique revealed that there was a variation in individuals’ responses to the lockdown, which could potentially be linked to different outcomes if the resolution of COVID-19 continues for an extended period. This suggests that prolonged restrictions may have varying effects on individuals’ physical activity levels and overall well-being. Novelty: “demonstrate how heterogenous groups are affected by using novel rest-activity rhythm and hierarchical clustering approaches”. |
| Question | Hojjatinia et al., 2022 [18] | Gilley et al., 2022 [19] | Massar et al., 2021 [20] | Mair et al., 2022 [21] | Leone et al., 2022 [22] | Capodilupo et al., 2020 [23] | Ong et al., 2021 [24] |
|---|---|---|---|---|---|---|---|
| Q1. Is the hypothesis/aim/objective of the study clearly described? | Y | Y | Y | Y | Y | Y | Y |
| Q2. Are the main outcomes clearly described in the Introduction or Methods? | Y | Y | Y | Y | Y | Y | Y |
| Q3. Are the characteristics of the participants clearly described (including age, sex, and status as healthy/injured/pathological)? | Y | N | N | N | N | Y | Y |
| Q4. Are the inclusion and exclusion criteria described and appropriate? | Y | N | N | N | N | N | N |
| Q5. Are the main findings of the study clearly described? | Y | Y | Y | Y | Y | Y | Y |
| Q6. Are estimates of the random variability in the data for the main outcomes provided? | Y | Y | Y | Y | Y | Y | Y |
| Q7. Have actual probability values been reported for the main outcomes? | Y | Y | Y | Y | Y | N | Y |
| Q8. Are the participants representative of the entire population from which they were recruited? | Y | Y | Y | Y | Y | Y | Y |
| Q9. Are the setting and conditions typical for the population represented by the participants? | Y | Y | Y | Y | Y | Y | Y |
| Q10. Are the statistical tests used to assess the main outcomes appropriate? | Y | Y | Y | Y | Y | Y | Y |
| Q11. Are the main outcome measures used accurate (valid and reliable)? | Y | Y | Y | Y | Y | Y | Y |
| Q12. Is a sample size justification, power description, or variance and effect estimates provided? | N | N | N | N | N | N | N |
| Study/Wearable Sensor Charectaristic | Hojjatinia et al., 2022 [18] | Gilley et al., 2022 [19] | Massar et al., 2021 [20] | Mair et al., 2022 [21] | Leone et al., 2022 [22] | Capodilupo et al., 2020 [23] | Ong et al., 2021 [24] |
|---|---|---|---|---|---|---|---|
| Main sedentary measured paramaters | Step count, heart rate | Step count, heart rate, sleep | Sleep, step count | Step count, personalized physical activity time goal | Standing, sitting, bending, lying down (sleep), walking (step) | Sleep, heart rate, physical activity (step) | Step count, sleep, heart rate |
| Day–day environment | + | + | + | + | - | + | + |
| Controlled environment | - | - | - | - | + | - | - |
| Number of sensors | 2 | 1 | 1 | 2 | 1 | 1 | 1 |
| Upper limb placement | + (Fitbit) | + | + | + | - | + | + |
| Lower limb placement | + (Act.Gr) | - | - | - | - | - | - |
| Trunk placement | - | - | - | - | + | - | - |
| Commercial device/s | + | + | + | + | + | + | + |
| Sampling frequency: <50 Hz | + | N.R | N.R | - | - | N.R | N.R |
| Sampling frequency: 50–100 Hz | - | N.R | N.R | + (Act.Gr) | + | N.R | N.R |
| Weight: <50 g | N.R | N.R | N.R | N.R | N.R | N.R | N.R |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Weizman, Y.; Tan, A.M.; Fuss, F.K. The Use of Wearable Devices to Measure Sedentary Behavior during COVID-19: Systematic Review and Future Recommendations. Sensors 2023, 23, 9449. https://doi.org/10.3390/s23239449
Weizman Y, Tan AM, Fuss FK. The Use of Wearable Devices to Measure Sedentary Behavior during COVID-19: Systematic Review and Future Recommendations. Sensors. 2023; 23(23):9449. https://doi.org/10.3390/s23239449
Chicago/Turabian StyleWeizman, Yehuda, Adin Ming Tan, and Franz Konstantin Fuss. 2023. "The Use of Wearable Devices to Measure Sedentary Behavior during COVID-19: Systematic Review and Future Recommendations" Sensors 23, no. 23: 9449. https://doi.org/10.3390/s23239449
APA StyleWeizman, Y., Tan, A. M., & Fuss, F. K. (2023). The Use of Wearable Devices to Measure Sedentary Behavior during COVID-19: Systematic Review and Future Recommendations. Sensors, 23(23), 9449. https://doi.org/10.3390/s23239449







