Non-Invasive Assessment of Abdominal/Diaphragmatic and Thoracic/Intercostal Spontaneous Breathing Contributions
Abstract
:1. Introduction
2. Materials and Methods
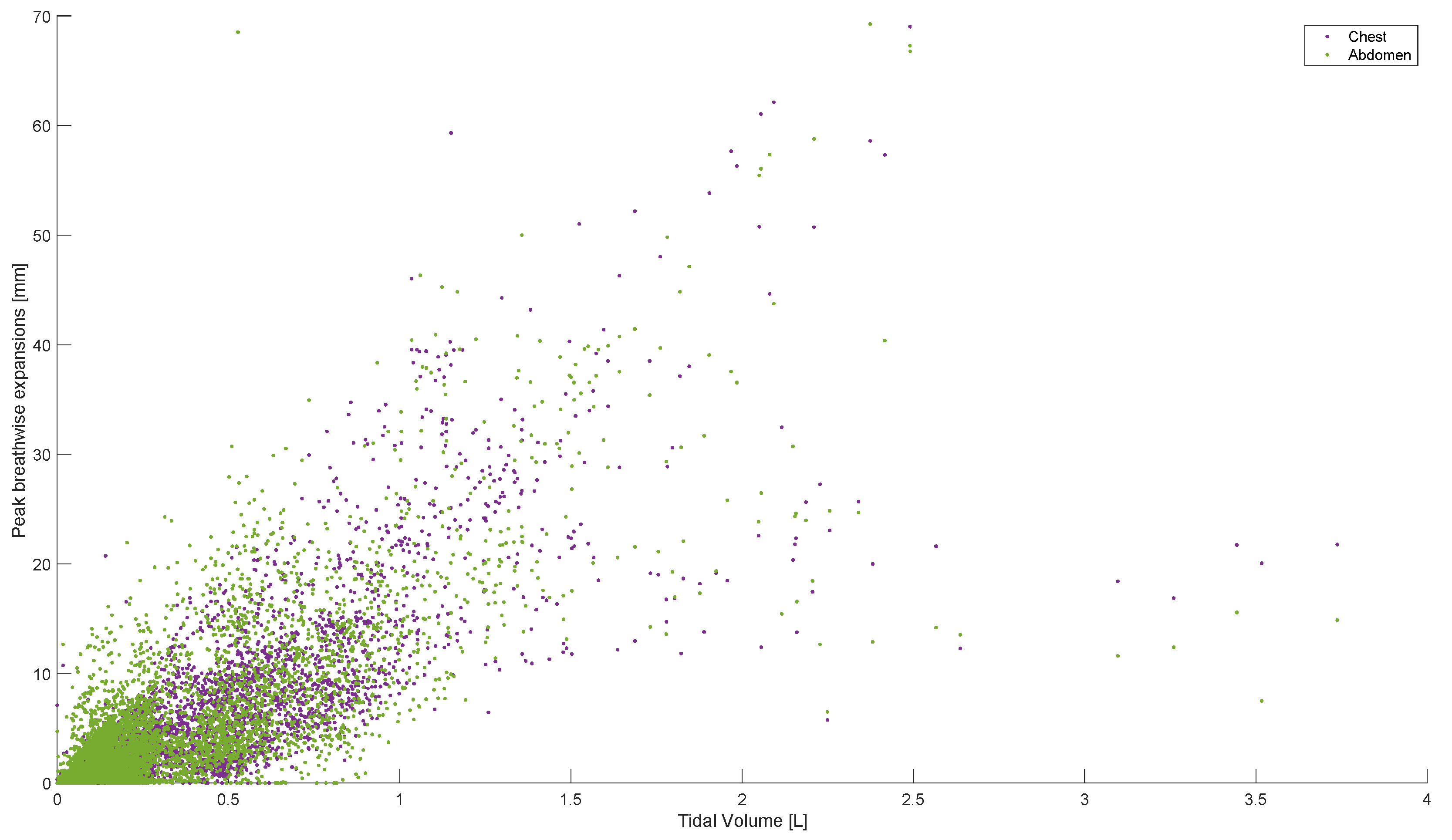
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ferkol, T.; Schraufnagel, D. The global burden of respiratory disease. Ann. Am. Thorac. Soc. 2014, 11, 404–406. [Google Scholar] [CrossRef] [PubMed]
- D’Amato, G.; Cecchi, L.; D’Amato, M.; Annesi-Maesano, I. Climate change and respiratory diseases. Eur. Respir. Rev. 2014, 23, 161–169. [Google Scholar] [CrossRef] [PubMed]
- Burney, P.; Jarvis, D.; Perez-Padilla, R. The global burden of chronic respiratory disease in adults. Int. J. Tuberc. Lung Dis. 2015, 19, 10–20. [Google Scholar] [CrossRef] [PubMed]
- Dwyer-Lindgren, L.; Bertozzi-Villa, A.; Stubbs, R.W.; Morozoff, C.; Shirude, S.; Naghavi, M.; Mokdad, A.H.; Murray, C.J. Trends and patterns of differences in chronic respiratory disease mortality among US counties, 1980–2014. JAMA 2017, 318, 1136–1149. [Google Scholar] [CrossRef]
- Zammit, C.; Liddicoat, H.; Moonsie, I.; Makker, H. Obesity and respiratory diseases. Int. J. Gen. Med. 2010, 3, 335–343. [Google Scholar]
- Vincent, J.-L.; Abraham, E.; Kochanek, P.; Moore, F.A.; Fink, M.P. Textbook of Critical Care E-Book; Elsevier Health Sciences: Amsterdam, The Netherlands, 2011. [Google Scholar]
- West, J.B.; Luks, A.M. West’s Respiratory Physiology; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2020. [Google Scholar]
- West, J.B. Pulmonary Pathophysiology: The Essentials; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2008. [Google Scholar]
- Des Jardins, T.; Burton, G.G. Clinical Manifestations & Assessment of Respiratory Disease-E-Book; Elsevier Health Sciences: Amsterdam, The Netherlands, 2023. [Google Scholar]
- Pellegrino, R.; Viegi, G.; Brusasco, V.; Crapo, R.O.; Burgos, F.; Casaburi, R.; Coates, A.; Van Der Grinten, C.; Gustafsson, P.; Hankinson, J. Interpretative strategies for lung function tests. Eur. Respir. J. 2005, 26, 948–968. [Google Scholar] [CrossRef]
- Butler, J.; Caro, C.G.; Alcala, R.; DuBois, A.B. Physiological factors affecting airway resistance in normal subjects and in patients with obstructive respiratory disease. J. Clin. Investig. 1960, 39, 584–591. [Google Scholar] [CrossRef]
- Macintyre, N.R. Muscle dysfunction associated with chronic obstructive pulmonary disease. Respir. Care 2006, 51, 840–852. [Google Scholar]
- Melo, L.C.; Silva, M.A.M.d.; Calles, A.C.d.N. Obesity and lung function: A systematic review. Einstein 2014, 12, 120–125. [Google Scholar] [CrossRef]
- Taskar, V.S.; Coultas, D.B. Is idiopathic pulmonary fibrosis an environmental disease? Proc. Am. Thorac. Soc. 2006, 3, 293–298. [Google Scholar] [CrossRef]
- Martinez-Pitre, P.J.; Sabbula, B.R.; Cascella, M. Restrictive Lung Disease; StatPearls Publishing: Treasure Island, FL, USA, 2020. [Google Scholar]
- Sulli, D.; Dhopte, A.; Agrawal, K. Impact of burn contractures of chest wall and their surgical release on pulmonary function. Burns 2019, 45, 929–935. [Google Scholar] [CrossRef]
- Loveridge, B.; West, P.; Kryger, M.; Anthonisen, N. Alteration in breathing pattern with progression of chronic obstructive pulmonary disease. Am. Rev. Respir. Dis. 1986, 134, 930–934. [Google Scholar] [CrossRef] [PubMed]
- Brack, T.; Jubran, A.; Tobin, M.J. Dyspnea and decreased variability of breathing in patients with restrictive lung disease. Am. J. Respir. Crit. Care Med. 2002, 165, 1260–1264. [Google Scholar] [CrossRef] [PubMed]
- Tobin, M.J.; Chadha, T.S.; Jenouri, G.; Birch, S.J.; Gazeroglu, H.B.; Sackner, M.A. Breathing patterns: 2. Diseased subjects. Chest 1983, 84, 286–294. [Google Scholar] [CrossRef] [PubMed]
- Flenady, T.; Dwyer, T.; Applegarth, J. Accurate respiratory rates count: So should you! Australas. Emerg. Nurs. J. 2017, 20, 45–47. [Google Scholar] [CrossRef] [PubMed]
- Elliott, M.; Williamson, R. Is Respiratory Rate Measurement Important? An Audit of Fundamental Nursing Textbooks. Mediterr. Nurs. Midwifery 2021, 1, 120–130. [Google Scholar] [CrossRef]
- Boulding, R.; Stacey, R.; Niven, R.; Fowler, S.J. Dysfunctional breathing: A review of the literature and proposal for classification. Eur. Respir. Rev. 2016, 25, 287–294. [Google Scholar] [CrossRef]
- Smyth, C.M.; Winter, S.L.; Dickinson, J.W. Breathing Pattern Disorders Distinguished from Healthy Breathing Patterns Using Oxptoelectronic Plethysmography. Transl. Sports Med. 2022, 2022, 2816781. [Google Scholar] [CrossRef]
- Chaitow, L.; Gilbert, C.; Bradley, D. What Are Breathing Pattern Disorders. Recognizing and Treating Breathing Disorders: A Multidisciplinary Approach; Churchill Livingstone: London, UK, 2014; pp. 1–10. [Google Scholar]
- Barker, N.; Everard, M.L. Getting to grips with ‘dysfunctional breathing’. Paediatr. Respir. Rev. 2015, 16, 53–61. [Google Scholar] [CrossRef]
- Kiesel, K.; Rhodes, T.; Mueller, J.; Waninger, A.; Butler, R. Development of a screening protocol to identify individuals with dysfunctional breathing. Int. J. Sports Phys. Ther. 2017, 12, 774. [Google Scholar] [CrossRef]
- Hansen-Honeycutt, J.; Chapman, E.B.; Nasypany, A.; Baker, R.T.; May, J. A clinical guide to the assessment and treatment of breathing pattern disorders in the physically active: Part 2, a case series. Int. J. Sports Phys. Ther. 2016, 11, 971. [Google Scholar] [PubMed]
- Henry, H.; Wells, C. Identification and management of dysfunctional breathing in primary care. Pract. Nurs. 2021, 32, 474–479. [Google Scholar] [CrossRef]
- CliftonSmith, T.; Rowley, J. Breathing pattern disorders and physiotherapy: Inspiration for our profession. Phys. Ther. Rev. 2011, 16, 75–86. [Google Scholar] [CrossRef]
- Jones, M.; Harvey, A.; Marston, L.; O’Connell, N.E. Breathing exercises for dysfunctional breathing/hyperventilation syndrome in adults. Cochrane Database Syst. Rev. 2013, 5, CD009041. [Google Scholar] [CrossRef]
- Reilly, C.C.; Floyd, S.V.; Lee, K.; Warwick, G.; James, S.; Gall, N.; Rafferty, G.F. Breathlessness and dysfunctional breathing in patients with postural orthostatic tachycardia syndrome (POTS): The impact of a physiotherapy intervention. Auton. Neurosci. 2020, 223, 102601. [Google Scholar] [CrossRef] [PubMed]
- Lumb, A.B.; Thomas, C.R. Nunn’s Applied Respiratory Physiology Ebook; Elsevier Health Sciences: Amsterdam, The Netherlands, 2020. [Google Scholar]
- Miravitlles, M.; Anzueto, A. Antibiotics for acute and chronic respiratory infection in patients with chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 2013, 188, 1052–1057. [Google Scholar] [CrossRef]
- Alangari, A.A. Corticosteroids in the treatment of acute asthma. Ann. Thorac. Med. 2014, 9, 187. [Google Scholar] [CrossRef]
- Becq, F.; Mall, M.A.; Sheppard, D.N.; Conese, M.; Zegarra-Moran, O. Pharmacological therapy for cystic fibrosis: From bench to bedside. J. Cyst. Fibros. 2011, 10, S129–S145. [Google Scholar] [CrossRef]
- Hoshino, T.; Toda, R.; Aizawa, H. Pharmacological treatment in asthma and COPD. Allergol. Int. 2009, 58, 341–346. [Google Scholar] [CrossRef]
- Kahya, Y.P.; Guler, E.C.; Sahin, S. Respiratory disease diagnosis using lung sounds. In Proceedings of the 19th Annual International Conference of the IEEE Engineering in Medicine and Biology Society. ‘Magnificent Milestones and Emerging Opportunities in Medical Engineering’ (Cat. No. 97CH36136), Chicago, IL, USA, 30 October–2 November 1997; pp. 2051–2053. [Google Scholar]
- Cacho, G.; Pérez-Calle, J.; Barbado, A.; Lledó, J.; Ojea, R.; Fernández-Rodríguez, C. Capnography is superior to pulse oximetry for the detection of respiratory depression during colonoscopy. Rev. Esp. Enfermedades Dig. 2010, 102, 86. [Google Scholar] [CrossRef]
- Pretto, J.J.; Roebuck, T.; Beckert, L.; Hamilton, G. Clinical use of pulse oximetry: Official guidelines from the Thoracic Society of Australia and New Zealand. Respirology 2014, 19, 38–46. [Google Scholar] [CrossRef]
- Chapman, E.B.; Hansen-Honeycutt, J.; Nasypany, A.; Baker, R.T.; May, J. A clinical guide to the assessment and treatment of breathing pattern disorders in the physically active: Part 1. Int. J. Sports Phys. Ther. 2016, 11, 803. [Google Scholar] [PubMed]
- Carson, S.S.; Cox, C.E.; Holmes, G.M.; Howard, A.; Carey, T.S. The changing epidemiology of mechanical ventilation: A population-based study. J. Intensive Care Med. 2006, 21, 173–182. [Google Scholar] [CrossRef] [PubMed]
- Carter, C.; Osborn, M.; Agagah, G.; Aedy, H.; Notter, J. COVID-19 disease: Invasive ventilation. Clin. Integr. Care 2020, 1, 100004. [Google Scholar] [CrossRef]
- Popat, B.; Jones, A.T. Invasive and non-invasive mechanical ventilation. Medicine 2012, 40, 298–304. [Google Scholar] [CrossRef] [PubMed]
- Stasche, N. Selective indication for positive airway pressure (PAP) in sleep-related breathing disorders with obstruction. GMS Curr. Top. Otorhinolaryngol. Head Neck Surg. 2006, 5, Doc06. [Google Scholar]
- Sutherland, K.; Vanderveken, O.M.; Tsuda, H.; Marklund, M.; Gagnadoux, F.; Kushida, C.A.; Cistulli, P.A. Oral appliance treatment for obstructive sleep apnea: An update. J. Clin. Sleep Med. 2014, 10, 215–227. [Google Scholar] [CrossRef]
- Gottlieb, D.J.; Punjabi, N.M. Diagnosis and management of obstructive sleep apnea: A review. Jama 2020, 323, 1389–1400. [Google Scholar] [CrossRef]
- Chang, H.P.; Chen, Y.F.; Du, J.K. Obstructive sleep apnea treatment in adults. Kaohsiung J. Med. Sci. 2020, 36, 7–12. [Google Scholar] [CrossRef]
- Guy, E.F.S.; Knopp, J.L.; Lerios, T.; Chase, J.G. Model-based Identification of Work of Breathing in CPAP Ventilation of Healthy Adults. IFAC-PapersOnLine 2023, 56, 2073–2078. [Google Scholar] [CrossRef]
- Schranz, C.; Knöbel, C.; Kretschmer, J.; Zhao, Z.; Möller, K. Hierarchical Parameter Identification in Models of Respiratory Mechanics. IEEE Trans. Biomed. Eng. 2011, 58, 3234–3241. [Google Scholar] [CrossRef]
- Chee, J.Z.; Chiew, Y.S.; Tan, C.P.; Arunachalam, G. Identifiability of patient effort respiratory mechanics model. In Proceedings of the 2018 IEEE-EMBS Conference on Biomedical Engineering and Sciences (IECBES), Sarawak, Malaysia, 3–6 December 2018; pp. 48–53. [Google Scholar]
- Stahl, C.A.; Möller, K.; Schumann, S.; Kuhlen, R.; Sydow, M.; Putensen, C.; Guttmann, J. Dynamic versus static respiratory mechanics in acute lung injury and acute respiratory distress syndrome. Crit. Care Med. 2006, 34, 2090–2098. [Google Scholar] [CrossRef] [PubMed]
- Rees, S.E.; Allerød, C.; Murley, D.; Zhao, Y.; Smith, B.W.; Kjaergaard, S.; Thorgaard, P.; Andreassen, S. Using physiological models and decision theory for selecting appropriate ventilator settings. J. Clin. Monit. Comput. 2006, 20, 421–429. [Google Scholar] [CrossRef] [PubMed]
- Rees, S.E. The Intelligent Ventilator (INVENT) project: The role of mathematical models in translating physiological knowledge into clinical practice. Comput. Methods Programs Biomed. 2011, 104, S1–S29. [Google Scholar] [CrossRef] [PubMed]
- Suki, B.; Bates, J. A nonlinear viscoelastic model of lung tissue mechanics. J. Appl. Physiol. 1991, 71, 826–833. [Google Scholar] [CrossRef]
- Telias, I.; Abbott, M.; Brochard, L. Monitoring respiratory drive and effort during mechanical ventilation. J. Transl. Crit. Care Med. 2021, 3, 13. [Google Scholar] [CrossRef]
- De Vries, H.J.; Tuinman, P.R.; Jonkman, A.H.; Liu, L.; Qiu, H.; Girbes, A.R.; Zhang, Y.; De Man, A.M.; de Grooth, H.-J.; Heunks, L. Performance of noninvasive airway occlusion maneuvers to assess lung stress and diaphragm effort in mechanically ventilated critically ill patients. Anesthesiology 2023, 138, 274–288. [Google Scholar] [CrossRef]
- Alter, A.; Aboussouan, L.S.; Mireles-Cabodevila, E. Neuromuscular weakness in chronic obstructive pulmonary disease: Chest wall, diaphragm, and peripheral muscle contributions. Curr. Opin. Pulm. Med. 2017, 23, 129–138. [Google Scholar] [CrossRef]
- Bureau, C.; Van Hollebeke, M.; Dres, M. Managing respiratory muscle weakness during weaning from invasive ventilation. Eur. Respir. Rev. 2023, 32, 220205. [Google Scholar] [CrossRef]
- Del Corral, T.; Fabero-Garrido, R.; Plaza-Manzano, G.; Fernández-de-Las-Peñas, C.; Navarro-Santana, M.; López-de-Uralde-Villanueva, I. Home-based respiratory muscle training on quality of life and exercise tolerance in long-term post-COVID-19: Randomized controlled trial. Ann. Phys. Rehabil. Med. 2023, 66, 101709. [Google Scholar] [CrossRef]
- Sheel, A.W.; Boushel, R.; Dempsey, J.A. Competition for blood flow distribution between respiratory and locomotor muscles: Implications for muscle fatigue. J. Appl. Physiol. 2018, 125, 820–831. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Z.; Steinmann, D.; Frerichs, I.; Guttmann, J.; Möller, K. PEEP titration guided by ventilation homogeneity: A feasibility study using electrical impedance tomography. Crit. Care 2010, 14, R8. [Google Scholar] [CrossRef] [PubMed]
- Zhou, C.; Chase, J.G. Low-cost structured light imaging of regional volume changes for use in assessing mechanical ventilation. Comput. Methods Programs Biomed. 2022, 226, 107176. [Google Scholar] [CrossRef] [PubMed]
- Guy, E.F.; Chase, J.G.; Holder-Pearson, L.R. Respiratory bi-directional pressure and flow data collection device with thoracic and abdominal circumferential monitoring. HardwareX 2022, 12, e00354. [Google Scholar] [CrossRef] [PubMed]
- Guy, E.F.S.; Knopp, J.; Lerios, T.; Chase, J.G. Pressure, flow, and dynamic thoraco-abdominal circumferences data for adults breathing under CPAP therapy. PhysioNet 2023, 101, e215–e220. [Google Scholar] [CrossRef]
- Guy, E.F.; Knopp, J.L.; Lerios, T.; Chase, J.G. Airflow and dynamic circumference of abdomen and thorax for adults at varied continuous positive airway pressure ventilation settings and breath rates. Sci. Data 2023, 10, 481. [Google Scholar] [CrossRef]
- Konno, K.; Mead, J. Measurement of the separate volume changes of rib cage and abdomen during breathing. J. Appl. Physiol. 1967, 22, 407–422. [Google Scholar] [CrossRef]
- Petty, C. Implementation of Breathing Exercises to Improve Chronic Disease Management; Oklahoma City University: Oklahoma City, OK, USA, 2023. [Google Scholar]
- Vickery, R.L. The Effect of Breathing Pattern Retraining on Performance in Competitive Cyclists; Auckland University of Technology: Auckland, New Zealand, 2008. [Google Scholar]
- Watson, A. Breathing in Singing. In The Oxford Handbook of Singing; Oxford University Press: Oxford, UK, 2014. [Google Scholar]
- Fernandez, R.; Mancebo, J.; Blanch, L.; Benito, S.; Calaf, N.; Net, A. Intrinsic PEEP on static pressure-volume curves. Intensive Care Med. 1990, 16, 233–236. [Google Scholar] [CrossRef]














| Subject | Sex (M/F) | Age (Years) | Weight (kg) | Height (cm) | BMI | Asthmatic (Y/N) | Smoker/Vaper (Y/N) |
|---|---|---|---|---|---|---|---|
| 1 | M | 37 | 96 | 177 | 30.6 | N | N |
| 2 | F | 23 | 65 | 169 | 22.8 | N | N |
| 3 | F | 21 | 63 | 171 | 21.5 | N | Y |
| 4 | M | 23 | 105 | 183 | 31.4 | N | N |
| 5 | M | 26 | 79 | 178 | 24.9 | N | N |
| 6 | M | 23 | 65 | 183 | 19.4 | Y | N |
| 7 | F | 20 | 60 | 170 | 20.8 | N | N |
| 8 | M | 23 | 75 | 182 | 22.6 | N | Y |
| 9 | F | 21 | 60 | 165 | 22.0 | N | N |
| 10 | M | 23 | 75 | 172 | 25.4 | N | N |
| 11 | M | 23 | 79 | 168 | 28.0 | N | N |
| 12 | M | 26 | 77 | 183 | 23.0 | N | N |
| 13 | F | 21 | 71.5 | 179 | 22.3 | N | N |
| 14 | F | 20 | 72 | 167 | 25.8 | N | N |
| 15 | F | 22 | 80 | 173 | 26.7 | Y | Y |
| 16 | M | 22 | 70 | 188 | 19.8 | N | N |
| 17 | F | 19 | 50 | 165 | 18.4 | N | Y |
| 18 | F | 27 | 73 | 153 | 31.2 | N | N |
| 19 | F | 23 | 57 | 158 | 22.8 | N | Y |
| 20 | F | 19 | 69 | 164 | 25.7 | N | N |
| 21 | M | 21 | 90 | 176 | 29.1 | N | N |
| 22 | M | 22 | 76.6 | 187 | 21.9 | N | N |
| 23 | M | 35 | 108 | 185 | 31.6 | N | N |
| 24 | M | 23 | 75 | 163 | 28.2 | N | N |
| 25 | M | 23 | 80 | 186 | 23.1 | N | Y |
| 26 | F | 20 | 55 | 163 | 20.7 | N | N |
| 27 | F | 22 | 97 | 169 | 34.0 | N | Y |
| 28 | F | 21 | 78 | 183 | 23.3 | N | Y |
| 29 | F | 20 | 52.8 | 160 | 20.6 | N | N |
| Subject | Medication Used | Frequency of Use |
|---|---|---|
| 6 | Ventolin | <once weekly |
| 15 | Vanair (Budesonide + Formoterol) | 2 times daily |
| Subject | Frequency | Duration |
|---|---|---|
| 3 | <once daily | 2 years |
| 8 | <once daily | 2 years |
| 15 | 10 inhales daily | 1.5 years |
| 17 | 150–200 inhales daily | 2 years |
| 19 | Once a day | 4 years |
| 25 | 20 inhales daily | Intermittent |
| 27 | 3 times a day | 1 year |
| 28 | 10 times a day | 2 months |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guy, E.F.S.; Clifton, J.A.; Knopp, J.L.; Holder-Pearson, L.R.; Chase, J.G. Non-Invasive Assessment of Abdominal/Diaphragmatic and Thoracic/Intercostal Spontaneous Breathing Contributions. Sensors 2023, 23, 9774. https://doi.org/10.3390/s23249774
Guy EFS, Clifton JA, Knopp JL, Holder-Pearson LR, Chase JG. Non-Invasive Assessment of Abdominal/Diaphragmatic and Thoracic/Intercostal Spontaneous Breathing Contributions. Sensors. 2023; 23(24):9774. https://doi.org/10.3390/s23249774
Chicago/Turabian StyleGuy, Ella F. S., Jaimey A. Clifton, Jennifer L. Knopp, Lui R. Holder-Pearson, and J. Geoffrey Chase. 2023. "Non-Invasive Assessment of Abdominal/Diaphragmatic and Thoracic/Intercostal Spontaneous Breathing Contributions" Sensors 23, no. 24: 9774. https://doi.org/10.3390/s23249774
APA StyleGuy, E. F. S., Clifton, J. A., Knopp, J. L., Holder-Pearson, L. R., & Chase, J. G. (2023). Non-Invasive Assessment of Abdominal/Diaphragmatic and Thoracic/Intercostal Spontaneous Breathing Contributions. Sensors, 23(24), 9774. https://doi.org/10.3390/s23249774






