Validation of an Activity Type Recognition Model Classifying Daily Physical Behavior in Older Adults: The HAR70+ Model
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedure
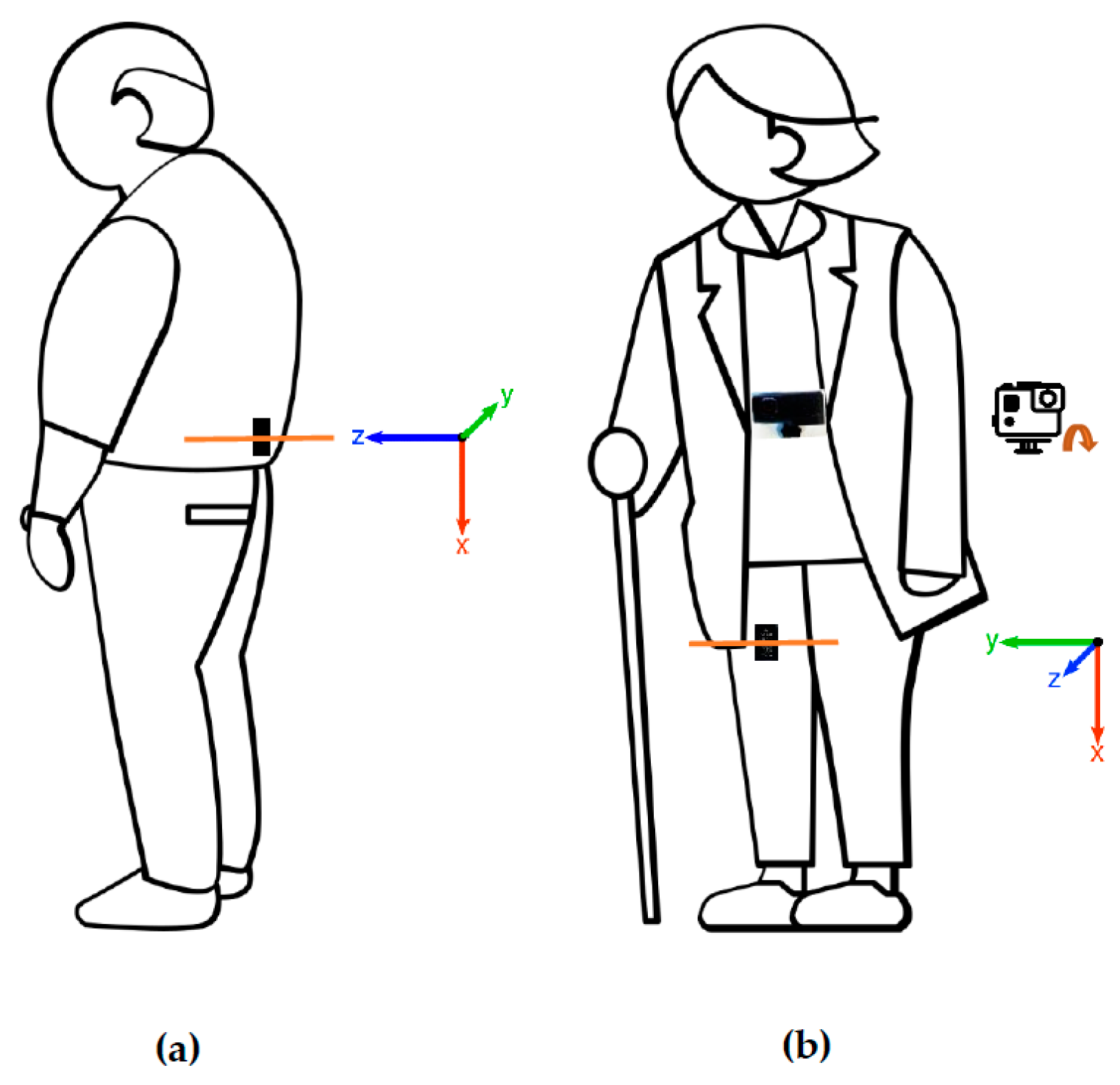
2.2.1. Activity Monitors
2.2.2. Video Recordings
2.2.3. Validation Protocol
2.3. Data Processing
2.3.1. Video Analysis
2.3.2. Accelerometer Data Pre-Processing
2.3.3. Machine Learning
2.4. Statistical Analysis
3. Results
3.1. The HAR70+ Dataset
3.2. Performance of the ML Models
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Report on Ageing and Health. Available online: https://apps.who.int/iris/bitstream/handle/10665/186463/9789240694811_eng.pdf (accessed on 4 June 2020).
- Danneskiold-Samsøe, B.; Bartels, E.M.; Bülow, P.M.; Lund, H.; Stockmarr, A.; Holm, C.C.; Wätjen, I.; Appleyard, M.; Bliddal, H. Isokinetic and isometric muscle strength in a healthy population with special reference to age and gender. Acta Physiol. 2009, 197 (Suppl. S673), 1–68. [Google Scholar] [CrossRef]
- Evans, W.J.; Campbell, W.W. Sarcopenia and age-related changes in body composition and functional capacity. J. Nutr. 1993, 123, 465–468. [Google Scholar] [CrossRef] [PubMed]
- Kanekar, N.; Aruin, A.S. The effect of aging on anticipatory postural control. Exp. Brain Res. 2014, 232, 1127–1136. [Google Scholar] [CrossRef] [Green Version]
- Izquierdo, M.; Merchant, R.A.; Morley, J.E.; Anker, S.D.; Aprahamian, I.; Arai, H.; Aubertin-Leheudre, M.; Bernabei, R.; Cadore, E.L.; Cesari, M.; et al. International Exercise Recommendations in Older Adults (ICFSR): Expert Consensus Guidelines. J. Nutr. Health Aging 2021, 25, 824–853. [Google Scholar] [CrossRef]
- Ofori-Asenso, R.; Chin, K.L.; Mazidi, M.; Zomer, E.; Ilomaki, J.; Zullo, A.R.; Gasevic, D.; Ademi, Z.; Korhonen, M.J.; LoGiudice, D.; et al. Global Incidence of Frailty and Prefrailty among Community-Dwelling Older Adults: A Systematic Review and Meta-analysis. JAMA Netw. Open 2019, 2, e198398. [Google Scholar] [CrossRef] [Green Version]
- Tari, A.R.; Nauman, J.; Zisko, N.; Skjellegrind, H.K.; Bosnes, I.; Bergh, S.; Stensvold, D.; Selbæk, G.; Wisløff, U. Temporal changes in cardiorespiratory fitness and risk of dementia incidence and mortality: A population-based prospective cohort study. Lancet Public Health 2019, 4, e565–e574. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wijndaele, K.; Westgate, K.; Stephens, S.K.; Blair, S.N.; Bull, F.C.; Chastin, S.F.M.; Dunstan, D.W.; Ekelund, U.L.F.; Esliger, D.W.; Freedson, P.S.; et al. Utilization and Harmonization of Adult Accelerometry Data: Review and Expert Consensus. Med. Sci. Sports Exerc. 2015, 47, 2129–2139. [Google Scholar] [CrossRef] [Green Version]
- Stevens, M.L.; Gupta, N.; Inan Eroglu, E.; Crowley, P.J.; Eroglu, B.; Bauman, A.; Granat, M.; Straker, L.; Palm, P.; Stenholm, S.; et al. Thigh-worn accelerometry for measuring movement and posture across the 24-hour cycle: A scoping review and expert statement. BMJ Open Sport Exerc. Med. 2020, 6, e000874. [Google Scholar] [CrossRef]
- Evenson, K.R.; Scherer, E.; Peter, K.M.; Cuthbertson, C.C.; Eckman, S. Historical development of accelerometry measures and methods for physical activity and sedentary behavior research worldwide: A scoping review of observational studies of adults. PLoS ONE 2022, 17, e0276890. [Google Scholar] [CrossRef] [PubMed]
- Heesch, K.C.; Hill, R.L.; Aguilar-Farias, N.; van Uffelen, J.G.Z.; Pavey, T. Validity of objective methods for measuring sedentary behaviour in older adults: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 119. [Google Scholar] [CrossRef]
- Gorman, E.; Hanson, H.M.; Yang, P.H.; Khan, K.M.; Liu-Ambrose, T.; Ashe, M.C. Accelerometry analysis of physical activity and sedentary behavior in older adults: A systematic review and data analysis. Eur. Rev. Aging Phys. Act. 2014, 11, 35–49. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barnett, A.; van den Hoek, D.; Barnett, D.; Cerin, E. Measuring moderate-intensity walking in older adults using the ActiGraph accelerometer. BMC Geriatr. 2016, 16, 211. [Google Scholar] [CrossRef] [Green Version]
- Fleg, J.L.; Morrell, C.H.; Bos, A.G.; Brant, L.J.; Talbot, L.A.; Wright, J.G.; Lakatta, E.G. Accelerated longitudinal decline of aerobic capacity in healthy older adults. Circulation 2005, 112, 674–682. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garber, C.E.; Blissmer, B.; Deschenes, M.R.; Franklin, B.A.; Lamonte, M.J.; Lee, I.M.; Nieman, D.C.; Swain, D.P. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Med. Sci. Sports Exerc. 2011, 43, 1334–1359. [Google Scholar] [CrossRef] [PubMed]
- Wullems, J.A.; Verschueren, S.M.P.; Degens, H.; Morse, C.I.; Onambélé, G.L. A review of the assessment and prevalence of sedentarism in older adults, its physiology/health impact and non-exercise mobility counter-measures. Biogerontology 2016, 17, 547–565. [Google Scholar] [CrossRef] [Green Version]
- Simpson, M.E.; Serdula, M.; Galuska, D.A.; Gillespie, C.; Donehoo, R.; Macera, C.; Mack, K. Walking trends among U.S. adults: The Behavioral Risk Factor Surveillance System, 1987–2000. Am. J. Prev. Med. 2003, 25, 95–100. [Google Scholar] [CrossRef]
- Lindemann, U.; Zijlstra, W.; Aminian, K.; Chastin, S.F.M.; de Bruin, E.D.; Helbostad, J.L.; Bussmann, H. Recommendations for Standardizing Validation Procedures Assessing Physical Activity of Older Persons by Monitoring Body Postures and Movements. Sensors 2014, 14, 1267–1277. [Google Scholar] [CrossRef] [Green Version]
- Elshehabi, M.; Del Din, S.; Hobert, M.A.; Warmerdam, E.; Sünkel, U.; Schmitz-Hübsch, T.; Behncke, L.M.; Heinzel, S.; Brockmann, K.; Metzger, F.G.; et al. Walking parameters of older adults from a lower back inertial measurement unit, a 6-year longitudinal observational study. Front. Aging Neurosci. 2022, 14, 789220. [Google Scholar] [CrossRef]
- Schrack, J.A.; Simonsick, E.M.; Chaves, P.H.M.; Ferrucci, L. The Role of Energetic Cost in the Age-Related Slowing of Gait Speed. J. Am. Geriatr. Soc. 2012, 60, 1811–1816. [Google Scholar] [CrossRef] [Green Version]
- Taraldsen, K.; Askim, T.; Sletvold, O.; Einarsen, E.K.; Bjåstad, K.G.; Indredavik, B.; Helbostad, J.L. Evaluation of a Body-Worn Sensor System to Measure Physical Activity in Older People with Impaired Function. Phys. Ther. 2011, 91, 277–285. [Google Scholar] [CrossRef] [Green Version]
- Bach, K.; Kongsvold, A.; Bårdstu, H.; Bardal, E.M.; Kjærnli, H.S.; Herland, S.; Logacjov, A.; Mork, P.J. A Machine Learning Classifier for Detection of Physical Activity Types and Postures During Free-Living. J. Meas. Phys. Behav. 2022, 5, 24–31. [Google Scholar] [CrossRef]
- Awais, M.; Chiari, L.; Ihlen, E.A.F.; Helbostad, J.L.; Palmerini, L. Physical Activity Classification for Elderly People in Free-Living Conditions. IEEE J Biomed. Health Inform. 2019, 23, 197–207. [Google Scholar] [CrossRef] [PubMed]
- Stewart, T.; Narayanan, A.; Hedayatrad, L.; Neville, J.; Mackay, L.; Duncan, S. A Dual-Accelerometer System for Classifying Physical Activity in Children and Adults. Med. Sci. Sports Exerc. 2018, 50, 2595–2602. [Google Scholar] [CrossRef] [PubMed]
- Narayanan, A.; Stewart, T.; Mackay, L. A Dual-Accelerometer System for Detecting Human Movement in a Free-living Environment. Med. Sci. Sports Exerc. 2020, 52, 252–258. [Google Scholar] [CrossRef] [PubMed]
- Schrack, J.A.; Cooper, R.; Koster, A.; Shiroma, E.J.; Murabito, J.M.; Rejeski, W.J.; Ferrucci, L.; Harris, T.B. Assessing Daily Physical Activity in Older Adults: Unraveling the Complexity of Monitors, Measures, and Methods. J. Gerontol. A Biol. Sci. Med. Sci. 2016, 71, 1039–1048. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rosenberg, D.; Godbole, S.; Ellis, K.; Di, C.; Lacroix, A.; Natarajan, L.; Kerr, J. Classifiers for Accelerometer-Measured Behaviors in Older Women. Med. Sci. Sports Exerc. 2017, 49, 610–616. [Google Scholar] [CrossRef] [Green Version]
- Taylor, L.M.; Klenk, J.; Maney, A.J.; Kerse, N.; Macdonald, B.M.; Maddison, R. Validation of a body-worn accelerometer to measure activity patterns in octogenarians. Arch. Phys. Med. Rehabil. 2014, 95, 930–934. [Google Scholar] [CrossRef] [PubMed]
- He, B.; Bai, J.; Zipunnikov, V.V.; Koster, A.; Caserotti, P.; Lange-Maia, B.; Glynn, N.W.; Harris, T.B.; Crainiceanu, C.M. Predicting human movement with multiple accelerometers using movelets. Med. Sci. Sports Exerc. 2014, 46, 1859–1866. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wullems, J.A.; Verschueren, S.M.P.; Degens, H.; Morse, C.I.; Onambélé, G.L. Performance of thigh-mounted triaxial accelerometer algorithms in objective quantification of sedentary behaviour and physical activity in older adults. PLoS ONE 2017, 12, e0188215. [Google Scholar] [CrossRef] [Green Version]
- Dedeyne, L.; Wullems, J.A.; Dupont, J.; Tournoy, J.; Gielen, E.; Verschueren, S. Exploring Machine Learning Models Based on Accelerometer Sensor Alone or Combined With Gyroscope to Classify Home-Based Exercises and Physical Behavior in (Pre)sarcopenic Older Adults. J. Meas. Phys. Behav. 2021, 4, 174–186. [Google Scholar] [CrossRef]
- Sasaki, J.E.; Hickey, A.M.; Staudenmayer, J.W.; John, D.; Kent, J.A.; Freedson, P.S. Performance of Activity Classification Algorithms in Free-Living Older Adults. Med. Sci. Sports Exerc. 2016, 48, 941–950. [Google Scholar] [CrossRef] [Green Version]
- Chigateri, N.G.; Kerse, N.; Wheeler, L.; MacDonald, B.; Klenk, J. Validation of an accelerometer for measurement of activity in frail older people. Gait Posture 2018, 66, 114–117. [Google Scholar] [CrossRef]
- Davoudi, A.; Mardini, M.T.; Nelson, D.; Albinali, F.; Ranka, S.; Rashidi, P.; Manini, T.M. The Effect of Sensor Placement and Number on Physical Activity Recognition and Energy Expenditure Estimation in Older Adults: Validation Study. JMIR mHealth uHealth 2021, 9, e23681. [Google Scholar] [CrossRef] [PubMed]
- Charette, C.; Best, K.L.; Smith, E.M.; Miller, W.C.; Routhier, F. Walking Aid Use in Canada: Prevalence and Demographic Characteristics among Community-Dwelling Users. Phys. Ther. 2018, 98, 571–577. [Google Scholar] [CrossRef] [PubMed]
- Awais, M.; Palmerini, L.; Bourke, A.K.; Ihlen, E.A.F.; Helbostad, J.L.; Chiari, L. Performance Evaluation of State of the Art Systems for Physical Activity Classification of Older Subjects Using Inertial Sensors in a Real Life Scenario: A Benchmark Study. Sensors 2016, 16, 2105. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kipp, M. ANVIL: A Universal Video Research Tool. In Handbook of Corpus Phonology; Durand, J., Gut, U., Kristofferson, G., Eds.; Oxford University Press: Oxford, UK, 2014; pp. 420–436. [Google Scholar]
- Logacjov, A.; Bach, K.; Kongsvold, A.; Bårdstu, H.B.; Mork, P.J. HARTH: A Human Activity Recognition Dataset for Machine Learning. Sensors 2021, 21, 7853. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.; Guestrin, C. XGBoost: A scalable tree boosting system. In Proceedings of the 22nd ACM SIGKDD International Conference on Knowledge Discovery and Data Mining, San Francisco, CA, USA, 13–17 August 2016; pp. 785–794. [Google Scholar]
- Cohen, J. A coefficient of agreement for nominal scales. Educ. Psychol. Meas. 1960, 20, 37–46. [Google Scholar] [CrossRef]
- Guo, Y.; Zhao, Y.; Salem, Y.; Miller, K.; Quiben, M.; Liu, H. Postural effect on gait characteristics by using rolling walkers. Geriatr. Nurs. 2020, 41, 916–920. [Google Scholar] [CrossRef] [PubMed]
- Del Din, S.; Godfrey, A.; Galna, B.; Lord, S.; Rochester, L. Free-living gait characteristics in ageing and Parkinson’s disease: Impact of environment and ambulatory bout length. J. Neuroeng. Rehabil. 2016, 13, 46. [Google Scholar] [CrossRef] [Green Version]
- Orendurff, M.S.; Schoen, J.A.; Bernatz, G.C.; Segal, A.D.; Klute, G.K. How humans walk: Bout duration, steps per bout, and rest duration. J. Rehabil. Res. Dev. 2008, 45, 1077–1089. [Google Scholar] [CrossRef]



| Total Group | Without Walking Aids | With Walking Aids | |
|---|---|---|---|
| n (%) | 18 (100) | 13 (72) | 5 (28) |
| female (%) | 9 (50) | 6 (46) | 3 (60) |
| age (years) | 79.6 ± 7.6 [70–95] | 77.2 ± 6.6 [70–95] | 85.8 ± 7.0 [76–94] |
| weight (kg) | 80.0 ± 9.3 [67–100] | 79.8 ± 9.9 [67–100] | 80.4 ± 8.8 [70–93] |
| height (cm) | 173 ± 7.8 [161–186] | 173 ± 8.0 [161–186] | 171 ± 7.6 [164–180] |
| BMI (kg/m2) | 26.8 ± 2.7 [22.6–31.2] | 26.6 ± 2.8 [22.6–31.1] | 27.6 ± 2.6 [25.1–31.2] |
| Activity Type | Definition |
|---|---|
| Walking | Locomotion towards a destination with one stride or more (one step with each foot). Walking could occur in all directions. Walking along a curved line is allowed. Walking could occur using walking aids. |
| Stairs (up/down) | Start: Heel-off of the foot that will land on the first step of the stairs. End: When the heel-strike of the last foot is placed on flat ground. If both feet rests at the same step with no feet movement, standing should be labeled. |
| Shuffling | Stepping in place by non-cyclical and non-directional movement of the feet. Includes turning on the spot with feet movements that are not part of a walking bout. When not able to see the feet, and movement of the upper body and surroundings indicate non-directional feet movement, shuffling should be labeled. |
| Standing | Upright, feet supporting the person’s body weight, with no feet movement, otherwise, this should be labeled as shuffling/walking. Movement of upper body and arms is allowed. If feet position is equal before and after upper body movement, standing should be labeled. When not able to see the feet, and upper body and surroundings indicate no feet movement, standing should be labeled. |
| Sitting | When the person’s buttocks are on the seat of a chair, bed, or floor. Sitting can include some movement in the upper body and legs; this should not be labeled as a separate transition. Adjustment of sitting position is allowed. |
| Lying | The person lies either on the stomach, on the back, or on the right/left shoulder. Movement of arms, feet, and head is allowed. |
| HARTH Model | |||||||
| Activity Type | Sensitivity | Specificity | Precision | F1 Score | |||
| Total group | |||||||
| Walking | 0.88 | [0.84, 0.92] | 0.97 | [0.97, 0.98] | 0.97 | [0.96, 0.97] | 0.93 |
| Standing | 0.93 | [0.92, 0.95] | 0.93 | [0.91, 0.95] | 0.79 | [0.76, 0.83] | 0.86 |
| Sitting | 0.97 | [0.96, 0.99] | 0.97 | [0.95, 1.00] | 0.93 | [0.87, 0.99] | 0.94 |
| Lying | 0.79 | [0.60, 0.99] | 1.00 | [0.99, 1.00] | 0.86 | [0.69, 1.00] | 0.86 |
| Without walking aids | |||||||
| Walking | 0.92 | [0.91, 0.94] | 0.97 | [0.97, 0.98] | 0.97 | [0.97, 0.98] | 0.95 |
| Standing | 0.94 | [0.92, 0.95] | 0.95 | [0.94, 0.96] | 0.83 | [0.80, 0.86] | 0.89 |
| Sitting | 0.97 | [0.95, 1.00] | 0.97 | [0.94, 1.00] | 0.93 | [0.85, 1.00] | 0.93 |
| Lying | 0.83 | [0.61, 1.00] | 1.00 | [0.99, 1.00] | 0.90 | [0.73, 1.00] | 0.86 |
| With walking aids | |||||||
| Walking | 0.77 | [0.66, 0.89] | 0.97 | [0.95, 0.99] | 0.95 | [0.93, 0.97] | 0.86 |
| Standing | 0.92 | [0.86, 0.98] | 0.88 | [0.81, 0.95] | 0.70 | [0.63, 0.78] | 0.79 |
| Sitting | 0.98 | [0.96, 1.00] | 0.97 | [0.92, 1.00] | 0.93 | [0.80, 1.00] | 0.96 |
| Lying | 0.68 | [0.00, 1.00] | 1.00 | [1.00, 1.00] | 0.74 | [0.00, 1.00] | 0.84 |
| HAR70+ Model | |||||||
| Activity Type | Sensitivity | Specificity | Precision | F1 score | |||
| Total group | |||||||
| Walking | 0.95 | [0.94, 0.97] | 0.95 | [0.94, 0.96] | 0.94 | [0.93, 0.95] | 0.95 |
| Standing | 0.87 | [0.85, 0.89] | 0.97 | [0.97, 0.98] | 0.90 | [0.88, 0.92] | 0.89 |
| Sitting | 0.97 | [0.93, 1.00] | 0.99 | [0.99, 1.00] | 0.98 | [0.97, 0.99] | 0.98 |
| Lying | 0.98 | [0.94, 1.00] | 0.99 | [0.98, 1.00] | 0.97 | [0.91, 1.00] | 0.96 |
| Without walking aids | |||||||
| Walking | 0.96 | [0.95, 0.97] | 0.95 | [0.94, 0.96] | 0.95 | [0.94, 0.96] | 0.96 |
| Standing | 0.88 | [0.86, 0.90] | 0.98 | [0.97, 0.98] | 0.91 | [0.89, 0.93] | 0.90 |
| Sitting | 0.96 | [0.91, 1.00] | 1.00 | [1.00, 1.00] | 0.98 | [0.98, 0.99] | 0.97 |
| Lying | 0.99 | [0.99, 1.00] | 0.99 | [0.98, 1.00] | 0.96 | [0.89, 1.00] | 0.97 |
| With walking aids | |||||||
| Walking | 0.93 | [0.88, 0.97] | 0.94 | [0.91, 0.97] | 0.92 | [0.89, 0.95] | 0.93 |
| Standing | 0.85 | [0.78, 0.91] | 0.96 | [0.94, 0.98] | 0.87 | [0.81, 0.92] | 0.86 |
| Sitting | 0.99 | [0.98, 1.00] | 0.98 | [0.95, 1.00] | 0.97 | [0.91, 1.00] | 0.98 |
| Lying | 0.91 | [0.72, 1.00] | 1.00 | [1.00, 1.00] | 0.99 | [0.98, 1.00] | 0.94 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ustad, A.; Logacjov, A.; Trollebø, S.Ø.; Thingstad, P.; Vereijken, B.; Bach, K.; Maroni, N.S. Validation of an Activity Type Recognition Model Classifying Daily Physical Behavior in Older Adults: The HAR70+ Model. Sensors 2023, 23, 2368. https://doi.org/10.3390/s23052368
Ustad A, Logacjov A, Trollebø SØ, Thingstad P, Vereijken B, Bach K, Maroni NS. Validation of an Activity Type Recognition Model Classifying Daily Physical Behavior in Older Adults: The HAR70+ Model. Sensors. 2023; 23(5):2368. https://doi.org/10.3390/s23052368
Chicago/Turabian StyleUstad, Astrid, Aleksej Logacjov, Stine Øverengen Trollebø, Pernille Thingstad, Beatrix Vereijken, Kerstin Bach, and Nina Skjæret Maroni. 2023. "Validation of an Activity Type Recognition Model Classifying Daily Physical Behavior in Older Adults: The HAR70+ Model" Sensors 23, no. 5: 2368. https://doi.org/10.3390/s23052368








