A Wearable Insole System to Measure Plantar Pressure and Shear for People with Diabetes
Abstract
:1. Introduction
2. Development of the Sensorised Insole System
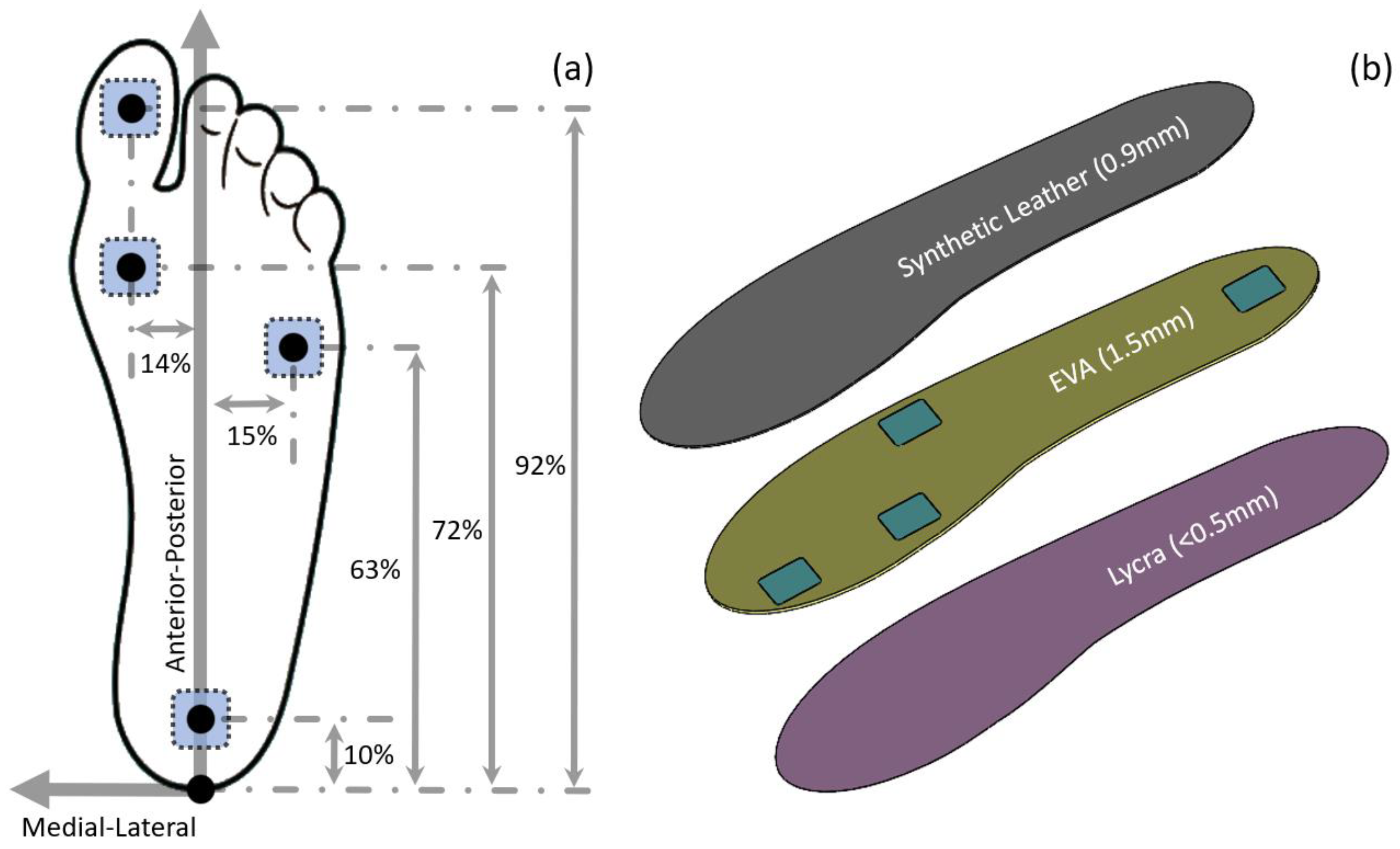
2.1. Sensor Locations
2.2. Insole Construction
2.3. Sensorised Insole System
3. Laboratory Evaluation of the Sensorised Insole System
3.1. Experimental Setup and Test Method
3.2. Pressure
3.3. Shear Stress
4. Evaluation of the Sensorised Insole System on a Human Participant
4.1. Test Protocol
4.2. Temporal Pressure and Shear Stress Profile during Level Walking
4.3. Effect of Footwear on Plantar Pressure and Shear Stresses
5. Safety Evaluation for Use in Shoes by Patients with Diabetes
5.1. Test Protocol
5.2. Safety Evaluation on People with Diabetes
6. Discussion
7. Conclusions
8. Future Work
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Armstrong, D.G.; Boulton, A.J.M.; Bus, S.A. Diabetic Foot Ulcers and Their Recurrence. N. Engl. J. Med. 2017, 376, 2367–2375. [Google Scholar] [CrossRef] [PubMed]
- Reiber, G.E.; Lipsky, B.A.; Gibbons, G.W. The Burden of Diabetic Foot Ulcers. Am. J. Surg. 1998, 176, 5S–10S. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, D.G.; Swerdlow, M.A.; Armstrong, A.A.; Conte, M.S.; Padula, W.V.; Bus, S.A. Five Year Mortality and Direct Costs of Care for People with Diabetic Foot Complications Are Comparable to Cancer. J. Foot Ankle Res. 2020, 13, 16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bus, S.A.; van Netten, J.J. A Shift in Priority in Diabetic Foot Care and Research: 75% of Foot Ulcers Are Preventable. Diabetes Metab. Res. Rev. 2016, 32 (Suppl. S1), 195–200. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- van Netten, J.J.; Raspovic, A.; Lavery, L.A.; Monteiro-Soares, M.; Rasmussen, A.; Sacco, I.C.N.; Bus, S.A. Prevention of Foot Ulcers in the at-Risk Patient with Diabetes: A Systematic Review. Diabetes Metab. Res. Rev. 2020, 36 (Suppl. S1), e3270. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nasser, A.R.; Hasan, A.M.; Humaidi, A.J.; Alkhayyat, A.; Alzubaidi, L.; Fadhel, M.A.; Santamaría, J.; Duan, Y. Iot and Cloud Computing in Health-Care: A New Wearable Device and Cloud-Based Deep Learning Algorithm for Monitoring of Diabetes. Electronics 2021, 10, 2719. [Google Scholar] [CrossRef]
- Balasubramanian, G.V.; Chockalingam, N.; Naemi, R. The Role of Cutaneous Microcirculatory Responses in Tissue Injury, Inflammation and Repair at the Foot in Diabetes. Front. Bioeng. Biotechnol. 2021, 9, 732753. [Google Scholar] [CrossRef]
- Jones, P.; Davies, M.J.; Khunti, K.; Fong, D.T.; Webb, D. In-Shoe Pressure Thresholds for People with Diabetes and Neuropathy at Risk of Ulceration: A Systematic Review. J. Diabetes Its Complicat. 2021, 35, 107815. [Google Scholar] [CrossRef]
- Abbott, C.A.; Chatwin, K.E.; Foden, P.; Hasan, A.N.; Sange, C.; Rajbhandari, S.M.; Reddy, P.N.; Vileikyte, L.; Bowling, F.L.; Boulton, A.J.M.; et al. Innovative Intelligent Insole System Reduces Diabetic Foot Ulcer Recurrence at Plantar Sites: A Prospective, Randomised, Proof-of-Concept Study. Lancet Digit. Health 2019, 1, e308–e318. [Google Scholar] [CrossRef] [Green Version]
- National Pressure Ulcer Advisory Panel; European Pressure Ulcer Advisory Panel; Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers: Quick Reference Guide; Haesler, E., Ed.; NPUAP: Osborne Park, WA, Australia, 2014. [Google Scholar]
- Bader, D.L.; Worsley, P.R. Technologies to Monitor the Health of Loaded Skin Tissues. Biomed. Eng. Online 2018, 17, 40. [Google Scholar] [CrossRef] [Green Version]
- Bus, S.A.; Lavery, L.A.; Monteiro-Soares, M.; Rasmussen, A.; Raspovic, A.; Sacco, I.C.N.; van Netten, J.J.; Foot International Working Group on the Diabetic. Guidelines on the Prevention of Foot Ulcers in Persons with Diabetes (Iwgdf 2019 Update). Diabetes Metab. Res. Rev. 2020, 36 (Suppl. S1), e3269. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yavuz, M. American Society of Biomechanics Clinical Biomechanics Award 2012: Plantar Shear Stress Distributions in Diabetic Patients with and without Neuropathy. Clin. Biomech. 2014, 29, 223–239. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, Q.; Wang, Y.L.; Xia, Y.; Wu, X.; Kirk, T.V.; Chen, X.D. A Low-Cost and Highly Integrated Sensing Insole for Plantar Pressure Measurement. Sens. Bio-Sens. Res. 2019, 26, 100298. [Google Scholar] [CrossRef]
- Tao, J.; Dong, M.; Li, L.; Wang, C.; Li, J.; Liu, Y.; Bao, R.; Pan, C. Real-Time Pressure Mapping Smart Insole System Based on a Controllable Vertical Pore Dielectric Layer. Microsyst. Nanoeng. 2020, 6, 62. [Google Scholar] [CrossRef] [PubMed]
- Martini, E.; Fiumalbi, T.; Dell, F.; Ivanic, Z.; Munih, M.; Vitiello, N.; Crea, S. Pressure-Sensitive Insoles for Real-Time Gait-Related Applications. Sensors 2020, 20, 1448. [Google Scholar] [CrossRef] [Green Version]
- Wang, L.; Jones, D.; Jones, A.; Chapman, G.J.; Siddle, H.J.; Russell, D.; Alazmani, A.; Culmer, P.R. A Portable Insole System to Simultaneously Measure Plantar Pressure and Shear Stress. IEEE Sens. J. 2022, 22, 9104–9113. [Google Scholar] [CrossRef]
- Amemiya, A.; Noguchi, H.; Oe, M.; Sanada, H.; Mori, T. Establishment of a Measurement Method for in-Shoe Pressure and Shear Stress in Specific Regions for Diabetic Ulcer Prevention. In Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Orlando, FL, USA, 16–20 August 2016; pp. 2291–2294. [Google Scholar]
- Takano, M.; Noguchi, H.; Oe, M.; Sanada, H.; Mori, T. Development and Evaluation of a System to Assess the Effect of Footwear on the in Shoe Plantar Pressure and Shear During Gait. ROBOMECH J. 2014, 1, 4. [Google Scholar] [CrossRef] [Green Version]
- Laszczak, P.; McGrath, M.; Tang, J.; Gao, J.; Jiang, L.; Bader, D.L.; Moser, D.; Zahedi, S. A Pressure and Shear Sensor System for Stress Measurement at Lower Limb Residuum/Socket Interface. Med. Eng. Phys. 2016, 38, 695–700. [Google Scholar] [CrossRef] [Green Version]
- Tang, J.; Jiang, L.; McGrath, M.; Bader, D.; Laszczak, P.; Moser, D.; Zahedi, S. Analysis of Lower Limb Prosthetic Socket Interface Based on Stress and Motion Measurements. Proc. Inst. Mech. Eng. Part H 2022, 236, 1349–1356. [Google Scholar] [CrossRef]
- Laszczak, P.; Jiang, L.; Bader, D.L.; Moser, D.; Zahedi, S. Development and Validation of a 3d-Printed Interfacial Stress Sensor for Prosthetic Applications. Med. Eng. Phys. 2015, 37, 132–137. [Google Scholar] [CrossRef]
- Petersen, B.J.; Rothenberg, G.M.; Lakhani, P.J.; Zhou, M.; Linders, D.R.; Bloom, J.D.; Wood, K.A.; Armstrong, D.G. Ulcer Metastasis? Anatomical Locations of Recurrence for Patients in Diabetic Foot Remission. J. Foot Ankle Res. 2020, 13, 1. [Google Scholar] [CrossRef] [PubMed]
- Price, C.; Nester, C. Foot Dimensions and Morphology in Healthy Weight, Overweight and Obese Males. Clin. Biomech. 2016, 37, 125–130. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Forghany, S.; Bonanno, D.R.; Menz, H.B.; Landorf, K.B. An Anatomically-Based Masking Protocol for the Assessment of in-Shoe Plantar Pressure Measurement of the Forefoot. J. Foot Ankle Res. 2018, 11, 31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ramanathan, A.K.; Kiran, P.; Arnold, G.P.; Wang, W.; Abboud, R.J. Repeatability of the Pedar-X in-Shoe Pressure Measuring System. Foot Ankle Surg. 2010, 16, 70–73. [Google Scholar] [CrossRef]
- Pataky, T.C. Spatial Resolution in Plantar Pressure Measurement Revisited. J. Biomech. 2012, 45, 2116–2124. [Google Scholar] [CrossRef]
- Pabon-Carrasco, M.; Reina-Bueno, M.; Vilar-Palomo, S.; Palomo-Toucedo, I.C.; Ramos-Ortega, J.; Juarez-Jimenez, J.M. Analysis and Assessment through Mechanical Static Compression Tests of Damping Capacity in a Series of Orthosis Plantar Materials Used as Supports. Int. J. Environ. Res. Public Health 2020, 18, 115. [Google Scholar] [CrossRef]
- Shi, Q.Q.; Li, P.L.; Yick, K.L.; Li, N.W.; Jiao, J. Effects of Contoured Insoles with Different Materials on Plantar Pressure Offloading in Diabetic Elderly During Gait. Sci. Rep. 2022, 12, 15395. [Google Scholar] [CrossRef]
- Parker, D.; Andrews, J.; Price, C. Validity and Reliability of the Xsensor in-Shoe Pressure Measurement System. PLoS ONE 2023, 18, e0277971. [Google Scholar] [CrossRef]
- Preece, S.J.; Chapman, J.D.; Braunstein, B.; Bruggemann, G.P.; Nester, C.J. Optimisation of Rocker Sole Footwear for Prevention of First Plantar Ulcer: Comparison of Group-Optimised and Individually-Selected Footwear Designs. J. Foot Ankle Res. 2017, 10, 27. [Google Scholar] [CrossRef] [Green Version]
- Alam, U.; Riley, D.R.; Jugdey, R.S.; Azmi, S.; Rajbhandari, S.; D’Août, K.; Malik, R.A. Diabetic Neuropathy and Gait: A Review. Diabetes Ther. 2017, 8, 1253–1264. [Google Scholar] [CrossRef] [Green Version]
- Goss, L.P.; Crafton, J.W.; Davis, B.L.; McMillan, G.R.; Berki, V.; Howe, A.E.; Papp, M. Plantar Pressure and Shear Measurement Using Surface Stress-Sensitive Film. Meas. Sci. Technol. 2020, 31, 025701. [Google Scholar] [CrossRef]
- Hazari, A.; Maiya, A.G.; Shivashankara, K.N.; Agouris, I.; Monteiro, A.; Jadhav, R.; Kumar, S.; Kumar, C.G.S.; Mayya, S.S. Kinetics and Kinematics of Diabetic Foot in Type 2 Diabetes Mellitus with and without Peripheral Neuropathy: A Systematic Review and Meta-Analysis. Springerplus 2016, 5, 1819. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jiang, X.; Deng, F.; Rui, S.; Ma, Y.; Wang, M.; Deng, B.; Wang, H.; Du, C.; Chen, B.; Yang, X.; et al. The Evaluation of Gait and Balance for Patients with Early Diabetic Peripheral Neuropathy: A Cross-Sectional Study. Risk Manag. Healthc. Policy 2022, 15, 543–552. [Google Scholar] [CrossRef] [PubMed]
- Arts, M.L.; Bus, S.A. Twelve Steps Per Foot Are Recommended for Valid and Reliable in-Shoe Plantar Pressure Data in Neuropathic Diabetic Patients Wearing Custom Made Footwear. Clin. Biomech. 2011, 26, 880–884. [Google Scholar] [CrossRef] [Green Version]
- Bus, S.A.; van Deursen, R.W.; Armstrong, D.G.; Lewis, J.E.; Caravaggi, C.F.; Cavanagh, P.R.; Foot International Working Group on the Diabetic. Footwear and Offloading Interventions to Prevent and Heal Foot Ulcers and Reduce Plantar Pressure in Patients with Diabetes: A Systematic Review. Diabetes Metab. Res. Rev. 2016, 32 (Suppl. S1), 99–118. [Google Scholar] [CrossRef] [Green Version]
- Chatwin, K.E.; Abbott, C.A.; Boulton, A.J.M.; Bowling, F.L.; Reeves, N.D. The Role of Foot Pressure Measurement in the Prediction and Prevention of Diabetic Foot Ulceration-a Comprehensive Review. Diabetes Metab. Res. Rev. 2020, 36, e3258. [Google Scholar] [CrossRef]









| Sensorised Insole | Without Insole | Effect | |||
|---|---|---|---|---|---|
| D_01 | Mean ± SD | Mean ± SD | S − W | % Diff | |
| Heel | 119.46 ± 10.98 | 118.90 ± 11.57 | 0.57 | 0% | - |
| 5MH | 46.83 ± 3.30 | 31.58 ± 4.06 | 15.25 | 33% | /\ |
| 1MH | 74.60 ± 3.88 | 85.68 ± 10.43 | −11.08 | −15% | \/ |
| Hallux | 171.45 ± 28.71 | 208.02 ± 15.54 | −36.57 | −21% | \/ |
| D_02 | Mean ± SD | Mean ± SD | S − W | % Diff | |
| Heel | 178.25 ± 20.56 | 211.37 ± 16.04 | −33.12 | −19% | \/ |
| 5MH | 92.84 ± 14.69 | 154.44 ± 34.51 | −61.59 | −66% | \/ |
| 1MH | 284.38 ± 28.62 | 308.89 ± 61.47 | −24.51 | −9% | \/ |
| Hallux | 123.94 ± 20.11 | 172.68 ± 26.08 | −48.74 | −39% | \/ |
| D_03 | Mean ± SD | Mean ± SD | S − W | % Diff | |
| Heel | 197.75 ± 26.18 | 185.24 ± 19.99 | 12.51 | 6% | /\ |
| 5MH | 94.45 ± 19.25 | 82.94 ± 10.74 | 11.51 | 12% | /\ |
| 1MH | 187.31 ± 53.43 | 257.36 ± 42.90 | −70.05 | −37% | \/ |
| Hallux | 244.82 ± 15.83 | 253.46 ± 27.35 | −8.65 | −4% | \/ |
| D_04 | Mean ± SD | Mean ± SD | S − W | % Diff | |
| Heel | 389.68 ± 19.89 | 422.73 ± 20.10 | −33.05 | −8% | \/ |
| 5MH | 168.99 ± 28.70 | 370.31 ± 62.10 | −201.32 | −119% | \/ |
| 1MH | 262.58 ± 53.02 | 277.80 ± 11.28 | −15.22 | −6% | \/ |
| Hallux | 159.82 ± 14.16 | 156.85 ± 7.61 | 2.97 | 2% | /\ |
| D_05 | Mean ± SD | Mean ± SD | S − W | % Diff | |
| Heel | 319.48 ± 9.26 | 397.56 ± 33.17 | −78.07 | −24% | \/ |
| 5MH | 168.76 ± 14.50 | 273.22 ± 41.83 | −104.46 | −62% | \/ |
| 1MH | 333.30 ± 53.14 | 381.77 ± 46.23 | −48.46 | −15% | \/ |
| Hallux | 304.76 ± 49.74 | 277.67 ± 39.40 | 27.09 | 9% | /\ |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tang, J.; Bader, D.L.; Moser, D.; Parker, D.J.; Forghany, S.; Nester, C.J.; Jiang, L. A Wearable Insole System to Measure Plantar Pressure and Shear for People with Diabetes. Sensors 2023, 23, 3126. https://doi.org/10.3390/s23063126
Tang J, Bader DL, Moser D, Parker DJ, Forghany S, Nester CJ, Jiang L. A Wearable Insole System to Measure Plantar Pressure and Shear for People with Diabetes. Sensors. 2023; 23(6):3126. https://doi.org/10.3390/s23063126
Chicago/Turabian StyleTang, Jinghua, Dan L. Bader, David Moser, Daniel J. Parker, Saeed Forghany, Christopher J. Nester, and Liudi Jiang. 2023. "A Wearable Insole System to Measure Plantar Pressure and Shear for People with Diabetes" Sensors 23, no. 6: 3126. https://doi.org/10.3390/s23063126






