Validity and Reliability of a Wearable Goniometer Sensor Controlled by a Mobile Application for Measuring Knee Flexion/Extension Angle during the Gait Cycle
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
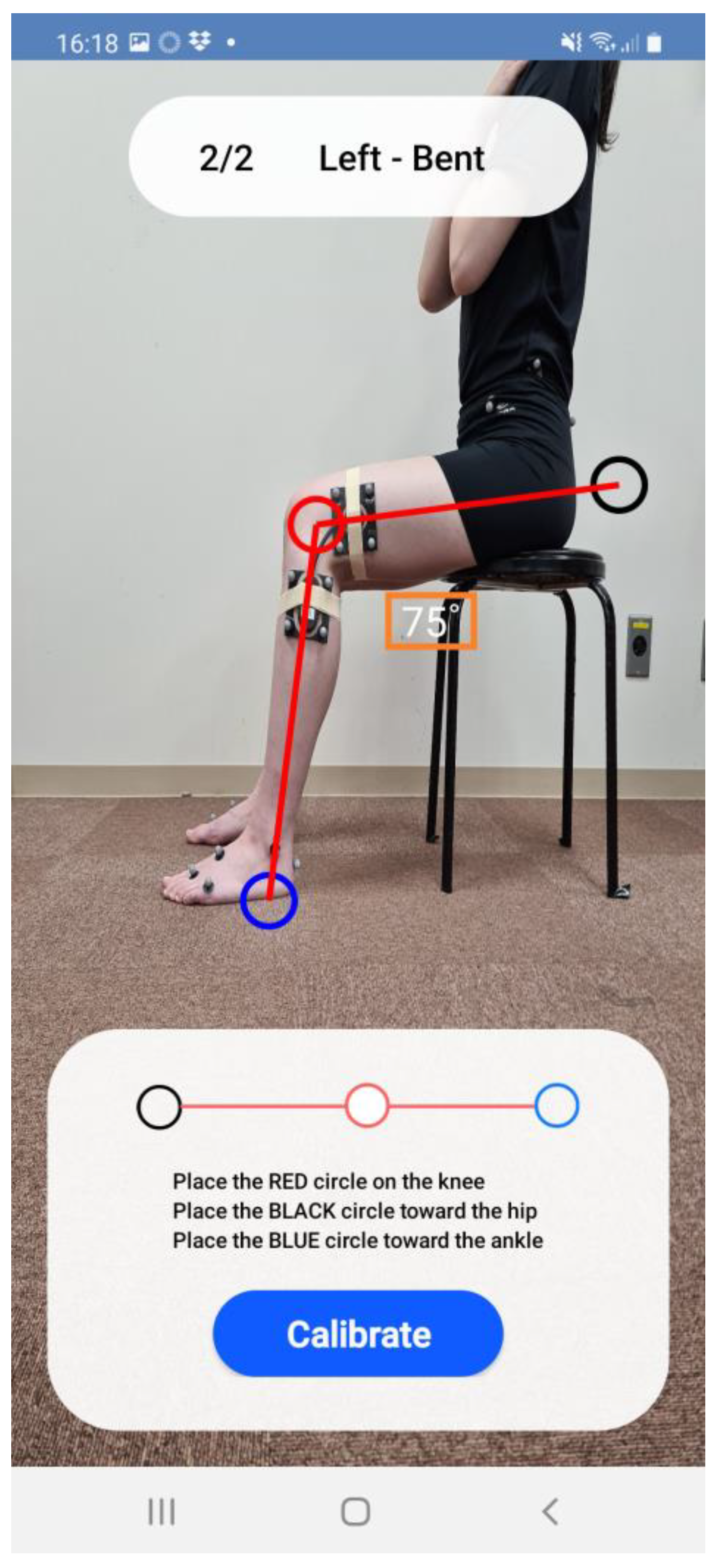
2.3. Assessment Using a Wearable Goniometer
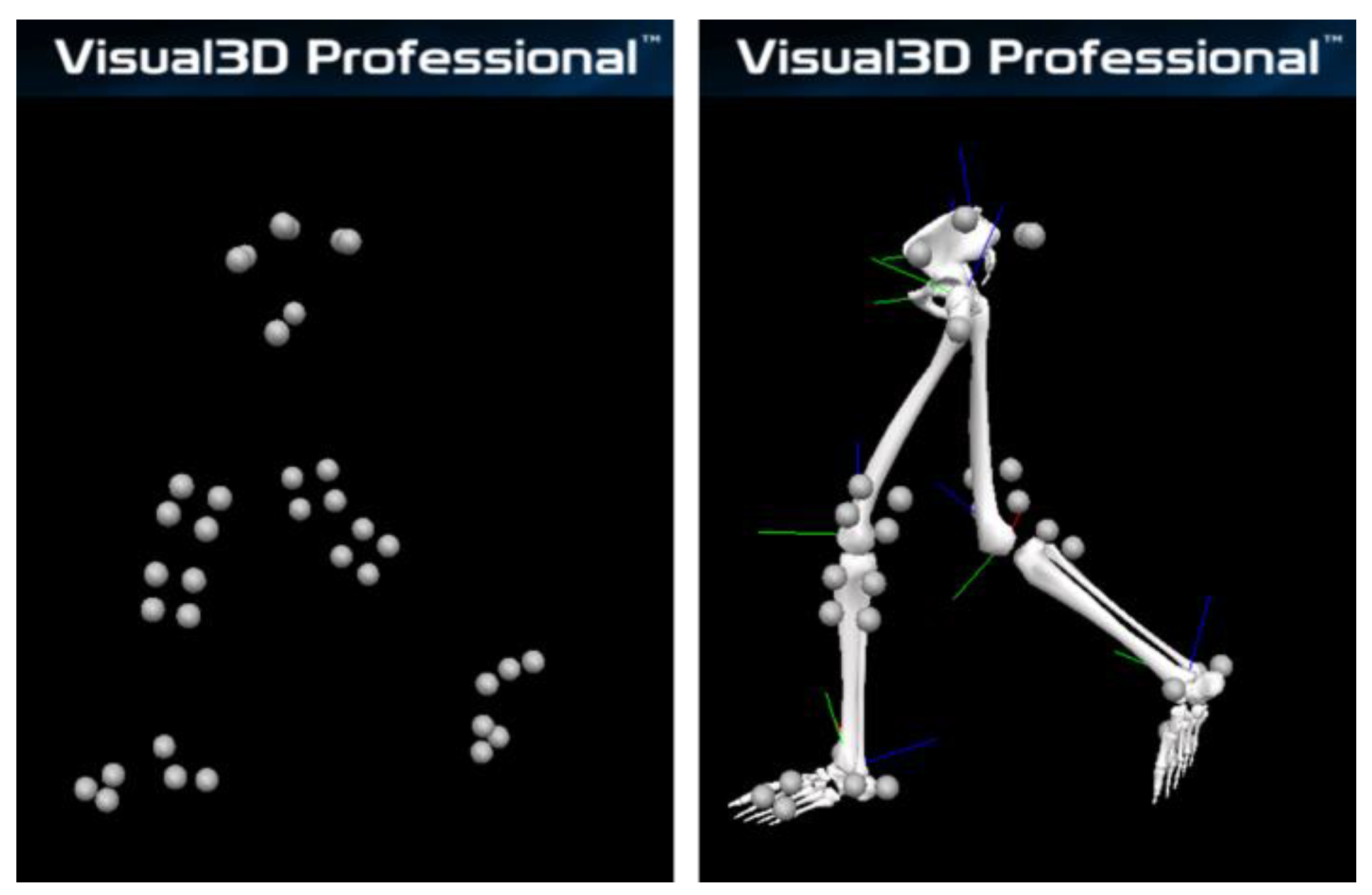
2.4. Assessment Using a Standard Optical Motion Analysis System
2.5. Data Collection
2.6. Data Analysis
2.7. Statistical Analysis
- CMC ≥ 0.95: excellent
- 0.95 > CMC ≥ 0.85: very good
- 0.85 > CMC ≥ 0.75: good
- 0.75 > CMC ≥ 0.65: moderate
- AE ≤ 2°: good accuracy
- 2 < AE ≤ 5°: acceptable accuracy
- 5° < AE ≤ 10°: tolerable accuracy
- AE > 10°: unacceptable accuracy
- R ≥ 0.9: extremely large
- 0.7 ≤ R < 0.9: very large
- 0.5 ≤ R < 0.7: large
- 0.3 ≤ R < 0.5: moderate
- 0.1 ≤ R < 0.3: small
- R < 0.1: trivial
- ICC ≥ 0.75: excellent
- 0.4 ≤ ICC < 0.75: fair to good
- ICC < 0.4: poor
3. Results
3.1. The Validation Study
3.2. The Reliability Study
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mills, K.; Hunt, M.A.; Ferber, R. Biomechanical deviations during level walking associated with knee osteoarthritis: A systematic review and meta-analysis. Arthritis Care Res. 2013, 65, 1643–1665. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hart, H.F.; Culvenor, A.G.; Collins, N.J.; Ackland, D.C.; Cowan, S.M.; Machotka, Z.; Crossley, K.M. Knee kinematics and joint moments during gait following anterior cruciate ligament reconstruction: A systematic review and meta-analysis. Br. J. Sports Med. 2016, 50, 597–612. [Google Scholar] [CrossRef] [PubMed]
- Teng, H.-L.; Wu, D.; Su, F.; Pedoia, V.; Souza, R.B.; Ma, C.B.; Li, X. Gait Characteristics Associated With a Greater Increase in Medial Knee Cartilage T1ρ and T2 Relaxation Times in Patients Undergoing Anterior Cruciate Ligament Reconstruction. Am. J. Sports Med. 2017, 45, 3262–3271. [Google Scholar] [CrossRef] [PubMed]
- Khandha, A.; Manal, K.; Wellsandt, E.; Capin, J.; Snyder-Mackler, L.; Buchanan, T.S. Gait mechanics in those with/without medial compartment knee osteoarthritis 5 years after anterior cruciate ligament reconstruction. J. Orthop. Res. 2017, 35, 625–633. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Favre, J.; Erhart-Hledik, J.C.; Chehab, E.F.; Andriacchi, T.P. Baseline ambulatory knee kinematics are associated with changes in cartilage thickness in osteoarthritic patients over 5 years. J. Biomech. 2016, 49, 1859–1864. [Google Scholar] [CrossRef]
- Buckthorpe, M.; Della Villa, F. Optimising the ‘Mid-Stage’ Training and Testing Process After ACL Reconstruction. Sports Med. 2020, 50, 657–678. [Google Scholar] [CrossRef]
- Herrington, L.; Myer, G.; Horsley, I. Task based rehabilitation protocol for elite athletes following Anterior Cruciate ligament reconstruction: A clinical commentary. Phys. Ther. Sport. 2013, 14, 188–198. [Google Scholar] [CrossRef]
- Riskowski, J.L. Gait and neuromuscular adaptations after using a feedback-based gait monitoring knee brace. Gait Posture 2010, 32, 242–247. [Google Scholar] [CrossRef]
- Kawaji, H.; Kojima, S. Effect of altered sagittal-plane knee kinematics on loading during the early stance phase of gait. Gait Posture 2019, 74, 108–113. [Google Scholar] [CrossRef]
- Kataoka, Y.; Saito, Y.; Takeda, R.; Ishida, T.; Tadano, S.; Suzuki, T.; Nakamura, K.; Nakata, A.; Osuka, S.; Yamada, S.; et al. Evaluation of Lower-Limb Kinematics during Timed Up and Go (TUG) Test in Subjects with Locomotive Syndrome (LS) Using Wearable Gait Sensors (H-Gait System). Sensors 2023, 23, 687. [Google Scholar] [CrossRef]
- Saito, Y.; Ishida, T.; Kataoka, Y.; Takeda, R.; Tadano, S.; Suzuki, T.; Nakamura, K.; Nakata, A.; Osuka, S.; Yamada, S.; et al. Evaluation of gait characteristics in subjects with locomotive syndrome using wearable gait sensors. BMC Musculoskelet. Disord. 2022, 23, 457. [Google Scholar] [CrossRef] [PubMed]
- Tsuchida, W.; Kobayashi, Y.; Inoue, K.; Horie, M.; Yoshihara, K.; Ooie, T. Kinematic characteristics during gait in frail older women identified by principal component analysis. Sci. Rep. 2022, 12, 1676. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, A.A.; Baba, J.; Beyea, J.; Landry, J.; Sexton, A.; McGibbon, C.A. Comparison of strain-gage and fiber-optic goniometry for measuring knee kinematics during activities of daily living and exercise. J. Biomech. Eng. 2012, 134, 084502. [Google Scholar] [CrossRef] [PubMed]
- Shull, P.B.; Jirattigalachote, W.; Hunt, M.A.; Cutkosky, M.R.; Delp, S.L. Quantified self and human movement: A review on the clinical impact of wearable sensing and feedback for gait analysis and intervention. Gait Posture 2014, 40, 11–19. [Google Scholar] [CrossRef]
- Rivera, B.; Cano, C.; Luis, I.; Elias, D.A. A 3D-Printed Knee Wearable Goniometer with a Mobile-App Interface for Measuring Range of Motion and Monitoring Activities. Sensors 2022, 22, 763. [Google Scholar] [CrossRef] [PubMed]
- de Oliveira Sato, T.; Hansson, G.-Å.; Coury, H.J.C.G. Goniometer crosstalk compensation for knee joint applications. Sensors 2010, 10, 9994–10005. [Google Scholar] [CrossRef]
- Freeman, M.A.R.; Pinskerova, V. The movement of the normal tibio-femoral joint. J. Biomech. 2005, 38, 197–208. [Google Scholar] [CrossRef]
- van der Linden, M.L.; Rowe, P.J.; Nutton, R.W. Between-day repeatability of knee kinematics during functional tasks recorded using flexible electrogoniometry. Gait Posture 2008, 28, 292–296. [Google Scholar] [CrossRef]
- Indramohan, V.P.; Valsan, G.; Rowe, P.J. Development and validation of a user-friendly data logger (SUDALS) for use with flexible electrogoniometers to measure joint movement in clinical trials. J. Med. Eng. Technol. 2009, 33, 650–655. [Google Scholar] [CrossRef]
- Petersen, E.T.; Rytter, S.; Koppens, D.; Dalsgaard, J.; Hansen, T.B.; Larsen, N.E.; Andersen, M.S.; Stilling, M. Patients with knee osteoarthritis can be divided into subgroups based on tibiofemoral joint kinematics of gait–an exploratory and dynamic radiostereometric study. Osteoarthr. Cartil. 2022, 30, 249–259. [Google Scholar] [CrossRef]
- Neal, K.; Williams, J.R.; Alfayyadh, A.; Capin, J.J.; Khandha, A.; Manal, K.; Snyder-Mackler, L.; Buchanan, T.S. Knee joint biomechanics during gait improve from 3 to 6 months after anterior cruciate ligament reconstruction. J. Orthop. Res. 2022, 40, 2025–2038. [Google Scholar] [CrossRef] [PubMed]
- Asano, T.; Akagi, M.; Nakamura, T. The functional flexion-extension axis of the knee corresponds to the surgical epicondylar axis: In vivo analysis using a biplanar image-matching technique. J. Arthroplast. 2005, 20, 1060–1067. [Google Scholar] [CrossRef]
- Ishida, T.; Samukawa, M.; Endo, D.; Kasahara, S.; Tohyama, H. Effects of Changing Center of Pressure Position on Knee and Ankle Extensor Moments During Double-Leg Squatting. J. Sport. Sci. Med. 2022, 21, 341–346. [Google Scholar] [CrossRef] [PubMed]
- Winter, D.A. Biomechanics and Motor Control of Human Movement, 4th ed.; Wiley: Hoboken, NJ, USA, 2009; p. 384. [Google Scholar]
- Bell, A.L.; Brand, R.A.; Pedersen, D.R. Prediction of hip joint centre location from external landmarks. Hum. Mov. Sci. 1989, 8, 3–16. [Google Scholar] [CrossRef]
- Ishida, T.; Samukawa, M.; Koshino, Y.; Ino, T.; Kasahara, S.; Tohyama, H. Pelvic Rotation Is Associated With Asymmetry in the Knee Extensor Moment During Double-Leg Squatting After Anterior Cruciate Ligament Reconstruction. J. Appl. Biomech. 2023, 39, 62–68. [Google Scholar] [CrossRef] [PubMed]
- Grood, E.S.; Suntay, W.J. A joint coordinate system for the clinical description of three-dimensional motions: Application to the knee. J. Biomech. Eng. 1983, 105, 136–144. [Google Scholar] [CrossRef]
- Cole, G.K.; Nigg, B.M.; Ronsky, J.L.; Yeadon, M.R. Application of the joint coordinate system to three-dimensional joint attitude and movement representation: A standardization proposal. J. Biomech. Eng. 1993, 115, 344–349. [Google Scholar] [CrossRef]
- Ferrari, A.; Cutti, A.G.; Cappello, A. A new formulation of the coefficient of multiple correlation to assess the similarity of waveforms measured synchronously by different motion analysis protocols. Gait Posture 2010, 31, 540–542. [Google Scholar] [CrossRef]
- Ferrari, A.; Cutti, A.G.; Garofalo, P.; Raggi, M.; Heijboer, M.; Cappello, A.; Davalli, A. First in vivo assessment of “Outwalk”: A novel protocol for clinical gait analysis based on inertial and magnetic sensors. Med. Biol. Eng. Comput. 2010, 48, 1–15. [Google Scholar] [CrossRef]
- McGinley, J.L.; Baker, R.; Wolfe, R.; Morris, M.E. The reliability of three-dimensional kinematic gait measurements: A systematic review. Gait Posture 2009, 29, 360–369. [Google Scholar] [CrossRef]
- Bessone, V.; Höschele, N.; Schwirtz, A.; Seiberl, W. Validation of a new inertial measurement unit system based on different dynamic movements for future in-field applications. Sports Biomech. 2022, 21, 685–700. [Google Scholar] [CrossRef] [PubMed]
- Hopkins, W.G.; Marshall, S.W.; Batterham, A.M.; Hanin, J. Progressive statistics for studies in sports medicine and exercise science. Med. Sci. Sports Exerc. 2009, 41, 3–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Growney, E.; Meglan, D.; Johnson, M.; Cahalan, T.; An, K.N. Repeated measures of adult normal walking using a video tracking system. Gait Posture 1997, 6, 147–162. [Google Scholar] [CrossRef]
- Fleiss, J.L. The Design and Analysis of Clinical Experiments; Wiley: Hoboken, NJ, USA, 1986. [Google Scholar]
- Shuai, Z.; Dong, A.; Liu, H.; Cui, Y. Reliability and Validity of an Inertial Measurement System to Quantify Lower Extremity Joint Angle in Functional Movements. Sensors 2022, 22, 863. [Google Scholar] [CrossRef] [PubMed]
- Tadano, S.; Takeda, R.; Miyagawa, H. Three dimensional gait analysis using wearable acceleration and gyro sensors based on quaternion calculations. Sensors 2013, 13, 9321–9343. [Google Scholar] [CrossRef]







Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ishida, T.; Samukawa, M. Validity and Reliability of a Wearable Goniometer Sensor Controlled by a Mobile Application for Measuring Knee Flexion/Extension Angle during the Gait Cycle. Sensors 2023, 23, 3266. https://doi.org/10.3390/s23063266
Ishida T, Samukawa M. Validity and Reliability of a Wearable Goniometer Sensor Controlled by a Mobile Application for Measuring Knee Flexion/Extension Angle during the Gait Cycle. Sensors. 2023; 23(6):3266. https://doi.org/10.3390/s23063266
Chicago/Turabian StyleIshida, Tomoya, and Mina Samukawa. 2023. "Validity and Reliability of a Wearable Goniometer Sensor Controlled by a Mobile Application for Measuring Knee Flexion/Extension Angle during the Gait Cycle" Sensors 23, no. 6: 3266. https://doi.org/10.3390/s23063266
APA StyleIshida, T., & Samukawa, M. (2023). Validity and Reliability of a Wearable Goniometer Sensor Controlled by a Mobile Application for Measuring Knee Flexion/Extension Angle during the Gait Cycle. Sensors, 23(6), 3266. https://doi.org/10.3390/s23063266





