Extended Reality Telemedicine Collaboration System Using Patient Avatar Based on 3D Body Pose Estimation
Abstract
:1. Introduction
2. Related Work
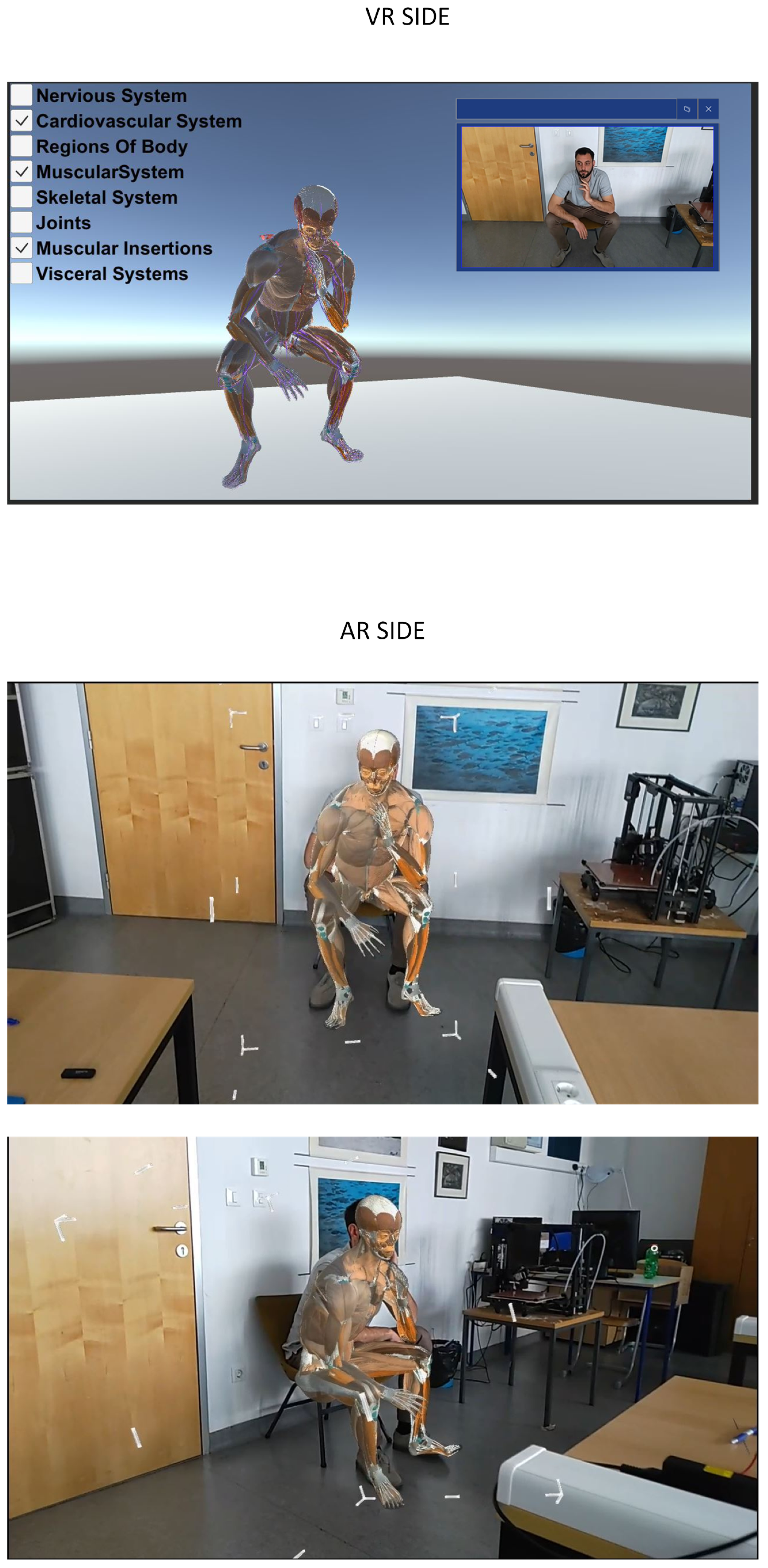
3. Proposed Method
3.1. Avatar Control
- Low latency, which is especially important for real-time interaction in videoconferencing and telemedicine applications
- Peer-to-peer (P2P) communication, where video streams are sent directly between users, which eliminates the need for a server.
- High-quality supporting adaptive bitrates needed to handle varying network conditions.
- Open source and standardized: the developers’ community ensures constant improvements.
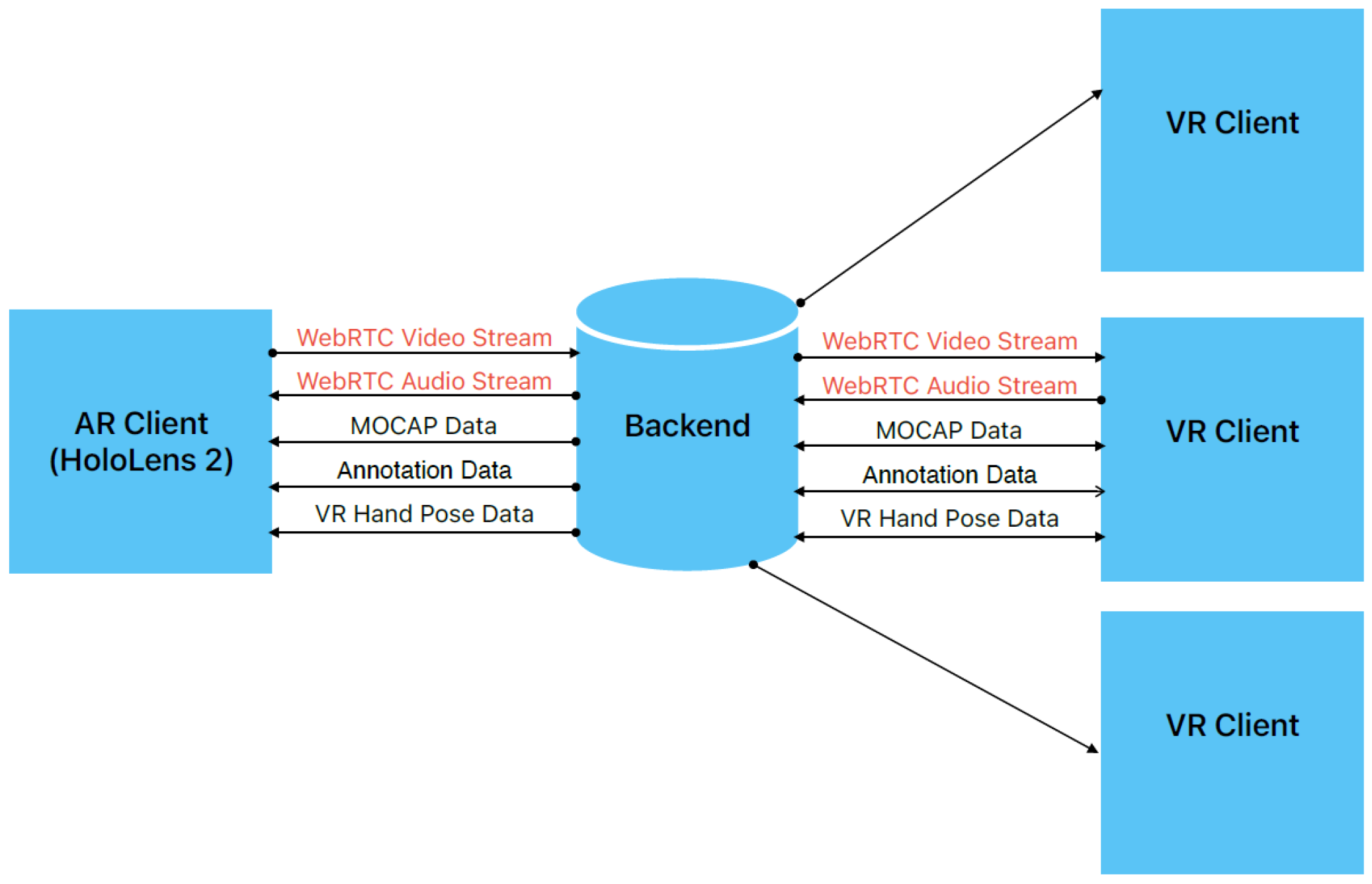
- The WebRTC data (OFFER, ANSWER, ICECANDIDATES) needed for establishing a RTC connection.
- MOCAP data obtained by pose estimation, which are used for avatar control in the XR space (shared 3D space).
- Collaborative cross-platform hand pose data are 3D vectors that enable the visualization of the user’s hands/controllers. In this way, the AR and VR sides are able to virtually collaborate on the patient’s 3D model.
- Annotation data: the remote or local expert can annotate a point on an avatar and send its position and textual description.
3.2. Pose Estimation
4. Results
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Petkova, R.; Poulkov, V.; Manolova, A.; Tonchev, K. Challenges in Implementing Low-Latency Holographic-Type Communication Systems. Sensors 2022, 22, 9617. [Google Scholar] [CrossRef] [PubMed]
- Qualcomm Technologies, Inc. VR and AR Pushing Connectivity Limits; Qualcomm Technologies, Inc.: San Diego, CA, USA, 2018. [Google Scholar]
- Lin, P.J.; Tsai, B.C.; Tsai, Y.W. Telemedicine System Based on Mixed Reality and Cognitive Speech Service Technologies. In Proceedings of the 2022 IEEE 4th Eurasia Conference on Biomedical Engineering, Healthcare and Sustainability (ECBIOS), Tainan, Taiwan, 27–29 May 2022; pp. 241–244. [Google Scholar]
- Anton, D.; Kurillo, G.; Yang, A.Y.; Bajcsy, R. Augmented telemedicine platform for real-time remote medical consultation. In Proceedings of the MultiMedia Modeling: 23rd International Conference, MMM 2017, Reykjavik, Iceland, 4–6 January 2017; Proceedings, Part I 23. Springer: Cham, Switzerland, 2017; pp. 77–89. [Google Scholar]
- Carbone, M.; Freschi, C.; Mascioli, S.; Ferrari, V.; Ferrari, M. A wearable augmented reality platform for telemedicine. In Proceedings of the Augmented Reality, Virtual Reality, and Computer Graphics: Third International Conference, AVR 2016, Lecce, Italy, 15–18 June 2016; Proceedings, Part II 3. Springer: Cham, Switzerland, 2016; pp. 92–100. [Google Scholar]
- Strak, R.; Yu, K.; Pankratz, F.; Lazarovici, M.; Sandmeyer, B.; Reichling, J.; Weidert, S.; Kraetsch, C.; Roegele, B.; Navab, N.; et al. Comparison between video-mediated and asymmetric 3d teleconsultation during a preclinical scenario. In Proceedings of the Mensch und Computer 2021, Ingolstadt, Germany, 5–8 September 2021; pp. 227–235. [Google Scholar]
- Gasques, D.; Johnson, J.G.; Sharkey, T.; Feng, Y.; Wang, R.; Xu, Z.R.; Zavala, E.; Zhang, Y.; Xie, W.; Zhang, X.; et al. ARTEMIS: A collaborative mixed-reality system for immersive surgical telementoring. In Proceedings of the 2021 CHI Conference on Human Factors in Computing Systems, Yokohama, Japan, 8–13 May 2021; pp. 1–14. [Google Scholar]
- Roth, D.; Yu, K.; Pankratz, F.; Gorbachev, G.; Keller, A.; Lazarovici, M.; Wilhelm, D.; Weidert, S.; Navab, N.; Eck, U. Real-time mixed reality teleconsultation for intensive care units in pandemic situations. In Proceedings of the 2021 IEEE Conference on Virtual Reality and 3D User Interfaces Abstracts and Workshops (VRW), Lisbon, Portugal, 27 March–1 April 2021; pp. 693–694. [Google Scholar]
- Weibel, N.; Gasques, D.; Johnson, J.; Sharkey, T.; Xu, Z.R.; Zhang, X.; Zavala, E.; Yip, M.; Davis, K. Artemis: Mixed-reality environment for immersive surgical telementoring. In Proceedings of the Extended Abstracts of the 2020 CHI Conference on Human Factors in Computing Systems, Honolulu, HI, USA, 25–30 April 2020; pp. 1–4. [Google Scholar]
- Kalbas, Y.; Jung, H.; Ricklin, J.; Jin, G.; Li, M.; Rauer, T.; Dehghani, S.; Navab, N.; Kim, J.; Pape, H.C.; et al. Remote Interactive Surgery Platform (RISP): Proof of Concept for an Augmented-Reality-Based Platform for Surgical Telementoring. J. Imaging 2023, 9, 56. [Google Scholar] [CrossRef] [PubMed]
- Sultan, L.R.; Haertter, A.; Al-Hasani, M.; Demiris, G.; Cary, T.W.; Tung-Chen, Y.; Sehgal, C.M. Can Artificial Intelligence Aid Diagnosis by Teleguided Point-of-Care Ultrasound? A Pilot Study for Evaluating a Novel Computer Algorithm for COVID-19 Diagnosis Using Lung Ultrasound. AI 2023, 4, 875–887. [Google Scholar] [CrossRef] [PubMed]
- Hill, R. Using augmented reality to improve patient outcomes with negative pressure wound therapy. Wounds 2022, 33, 47–50. [Google Scholar] [CrossRef] [PubMed]
- Borresen, A.; Chakka, K.; Wu, R.; Lin, C.K.; Wolfe, C.; Prabhakaran, B.; Annaswamy, T.M. Comparison of in-person and synchronous remote musculoskeletal exam using augmented reality and haptics: A pilot study. PM&R 2023, 15, 891–898. [Google Scholar]
- Mediapipe Object Detection. 2023. Available online: https://developers.google.com/mediapipe/solutions/vision/object_detector (accessed on 13 October 2023).
- Tan, M.; Pang, R.; Le, Q.V. Efficientdet: Scalable and efficient object detection. In Proceedings of the IEEE/CVF Conference on Computer Vision and Pattern Recognition, Seattle, WA, USA, 13–19 June 2020; pp. 10781–10790. [Google Scholar]
- Python Package Face-Recogntion. 2023. Available online: https://pypi.org/project/face-recognition/ (accessed on 13 October 2023).
- Rong, Y.; Shiratori, T.; Joo, H. Frankmocap: A monocular 3d whole-body pose estimation system via regression and integration. In Proceedings of the IEEE/CVF International Conference on Computer Vision, Montreal, BC, Canada, 11–17 October 2021; pp. 1749–1759. [Google Scholar]
- Pavlakos, G.; Choutas, V.; Ghorbani, N.; Bolkart, T.; Osman, A.A.; Tzionas, D.; Black, M.J. Expressive body capture: 3d hands, face, and body from a single image. In Proceedings of the IEEE/CVF Conference on Computer Vision and Pattern Recognition, Long Beach, CA, USA, 15–20 June 2019; pp. 10975–10985. [Google Scholar]
- Loper, M.; Mahmood, N.; Romero, J.; Pons-Moll, G.; Black, M.J. SMPL: A skinned multi-person linear model. In Seminal Graphics Papers: Pushing the Boundaries, Volume 2; Association for Computing Machinery: New York, NY, USA, 2023; pp. 851–866. [Google Scholar]
- Kolotouros, N.; Pavlakos, G.; Black, M.J.; Daniilidis, K. Learning to reconstruct 3D human pose and shape via model-fitting in the loop. In Proceedings of the IEEE/CVF International Conference on Computer Vision, Seoul, Republic of Korea, 27 October–2 November 2019; pp. 2252–2261. [Google Scholar]
- Sanyal, S.; Bolkart, T.; Feng, H.; Black, M.J. Learning to regress 3D face shape and expression from an image without 3D supervision. In Proceedings of the IEEE/CVF Conference on Computer Vision and Pattern Recognition, Long Beach, CA, USA, 15–20 June 2019; pp. 7763–7772. [Google Scholar]


| Service | Time Delay (ms) |
|---|---|
| WebRTC P2P | 200–300 |
| Grab frame | 3–8 |
| Person detection | 25–60 |
| Person identification | 30–60 |
| 3D pose estimation | 15–50 |
| WebSocket MOCAP | 50 |
| Unity 3D model transformation (running on laptop) | 5–15 |
| Unity 3D model transformation (running on HoloLens 2) | 10–25 |
| AR Build | AR Remote | VR Build | ||||
|---|---|---|---|---|---|---|
| Body System | No Light (FPS) | Light (FPS) | No Light (FPS) | Light (FPS) | No Light (FPS) | Light (FPS) |
| Visceral system | 26 | 25 | 60 | 60 | 120 | 120 |
| Muscural system | 13 | 12 | 60 | 60 | 120 | 120 |
| Cardiovascular system | 8 | 8 | 60 | 60 | 120 | 120 |
| Nervous system and sence organs | 13 | 13 | 60 | 60 | 120 | 120 |
| Regions of human body/skin | 54 | 51 | 60 | 60 | 120 | 120 |
| Skeletal system | 28 | 28 | 60 | 60 | 120 | 120 |
| Joints | 38 | 36 | 60 | 60 | 120 | 120 |
| Muscular insertion | 26 | 26 | 60 | 60 | 120 | 120 |
| Lymphoid organs | 50 | 46 | 60 | 60 | 120 | 120 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Šarić, M.; Russo, M.; Kraljević, L.; Meter, D. Extended Reality Telemedicine Collaboration System Using Patient Avatar Based on 3D Body Pose Estimation. Sensors 2024, 24, 27. https://doi.org/10.3390/s24010027
Šarić M, Russo M, Kraljević L, Meter D. Extended Reality Telemedicine Collaboration System Using Patient Avatar Based on 3D Body Pose Estimation. Sensors. 2024; 24(1):27. https://doi.org/10.3390/s24010027
Chicago/Turabian StyleŠarić, Matko, Mladen Russo, Luka Kraljević, and Davor Meter. 2024. "Extended Reality Telemedicine Collaboration System Using Patient Avatar Based on 3D Body Pose Estimation" Sensors 24, no. 1: 27. https://doi.org/10.3390/s24010027
APA StyleŠarić, M., Russo, M., Kraljević, L., & Meter, D. (2024). Extended Reality Telemedicine Collaboration System Using Patient Avatar Based on 3D Body Pose Estimation. Sensors, 24(1), 27. https://doi.org/10.3390/s24010027








