Data-Fusion-Based Quality Enhancement for HR Measurements Collected by Wearable Sensors
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants and Experimental Equipment
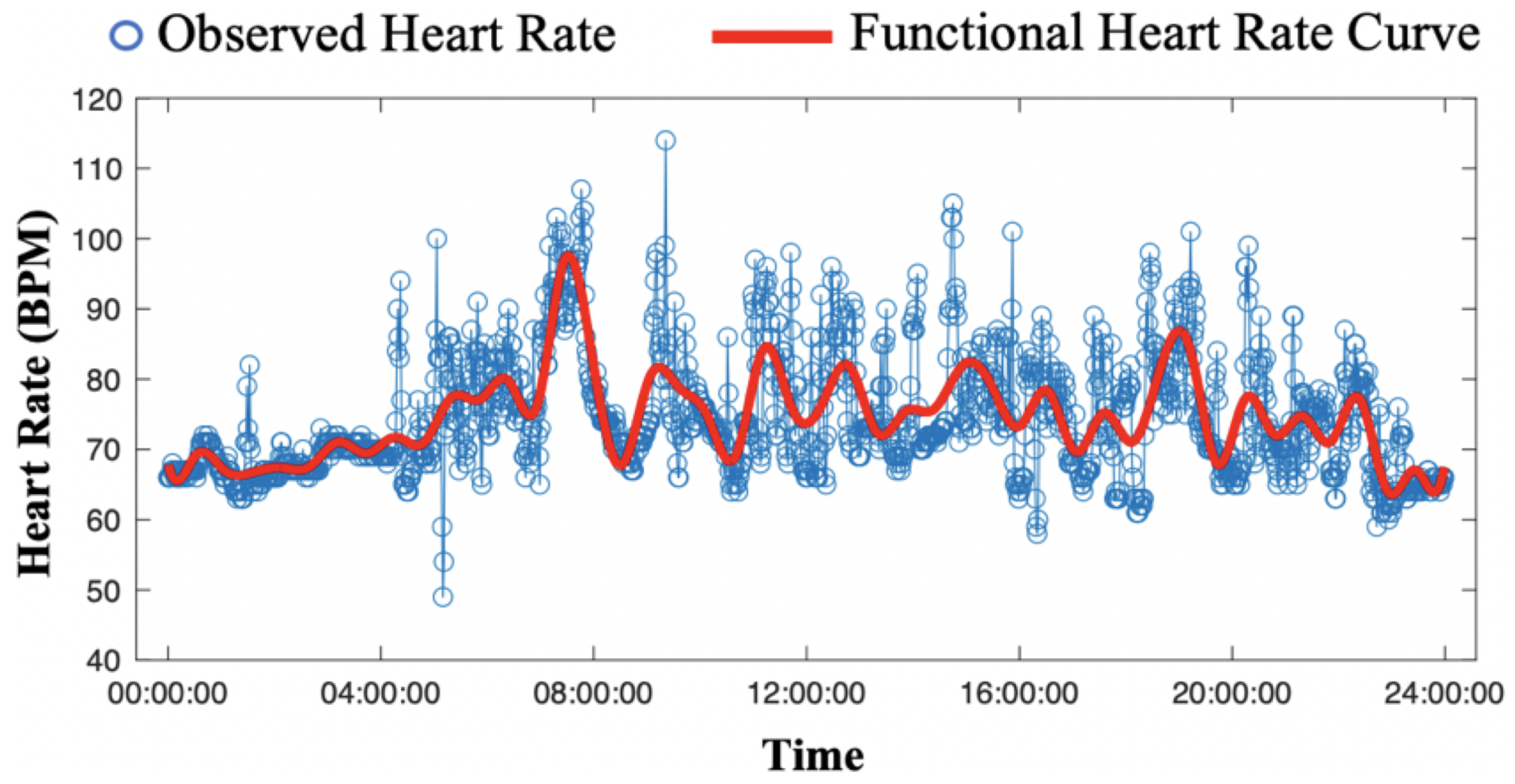
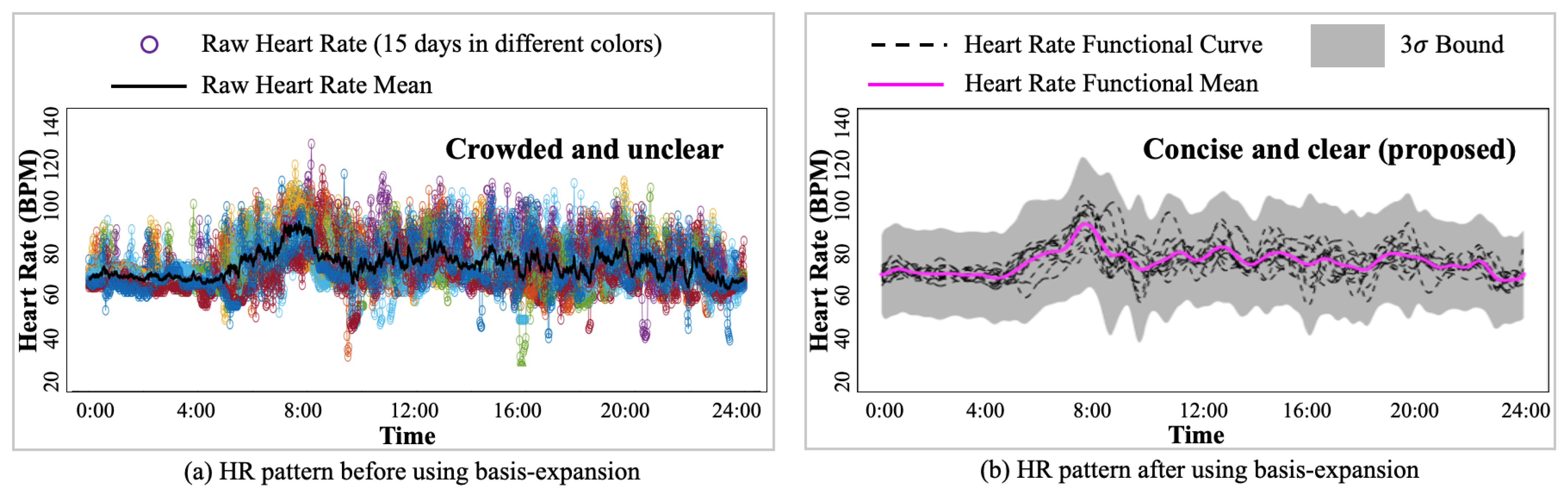
2.2. Motion Artifacts Removal by Basis Expansion
2.3. HR Calibration by Basis-Expansion-Based Gaussian Process
2.4. HR Pattern Calibration by Gaussian Process Posterior Updating
3. Results
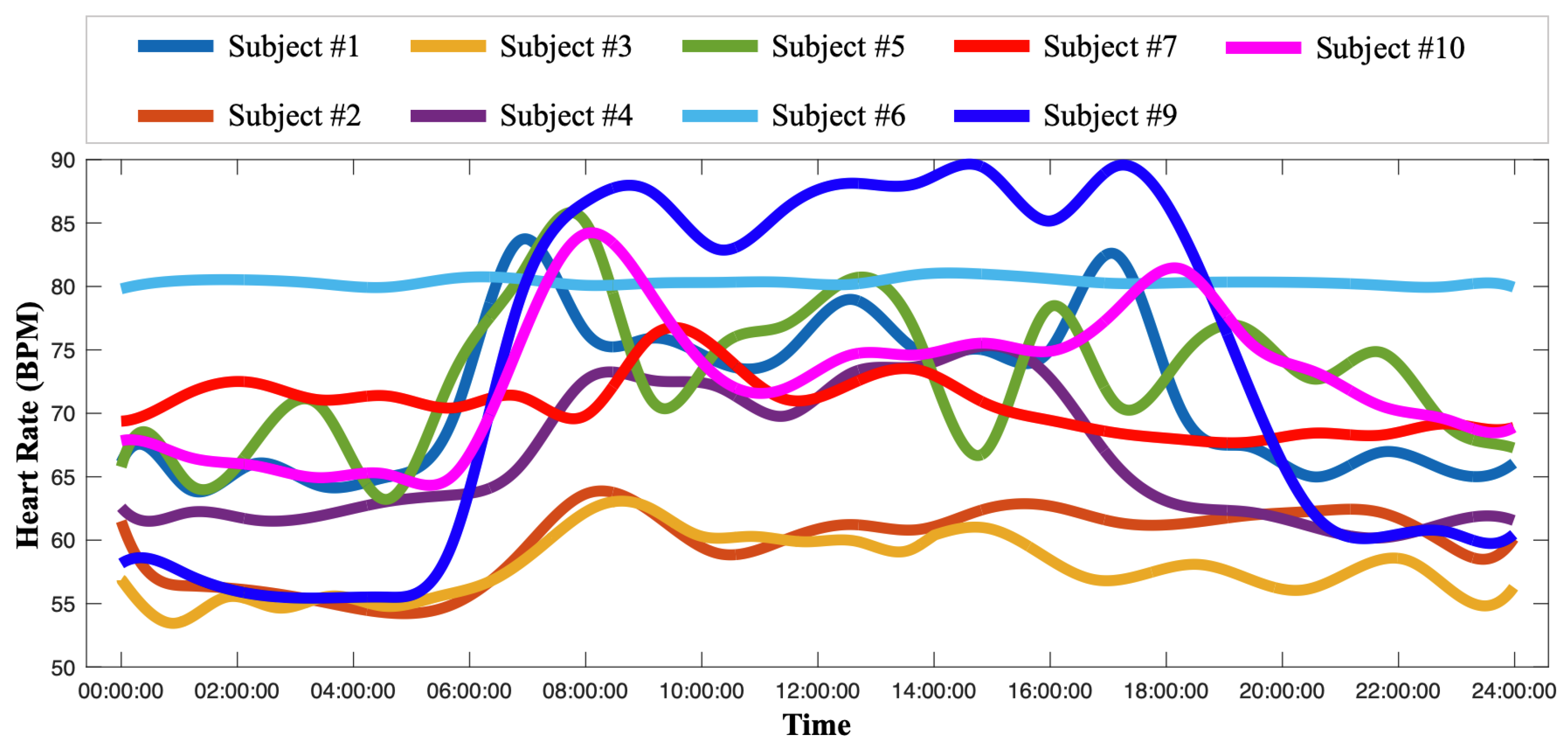
3.1. Motion Artifact Removal and Personalized HR Pattern Estimation
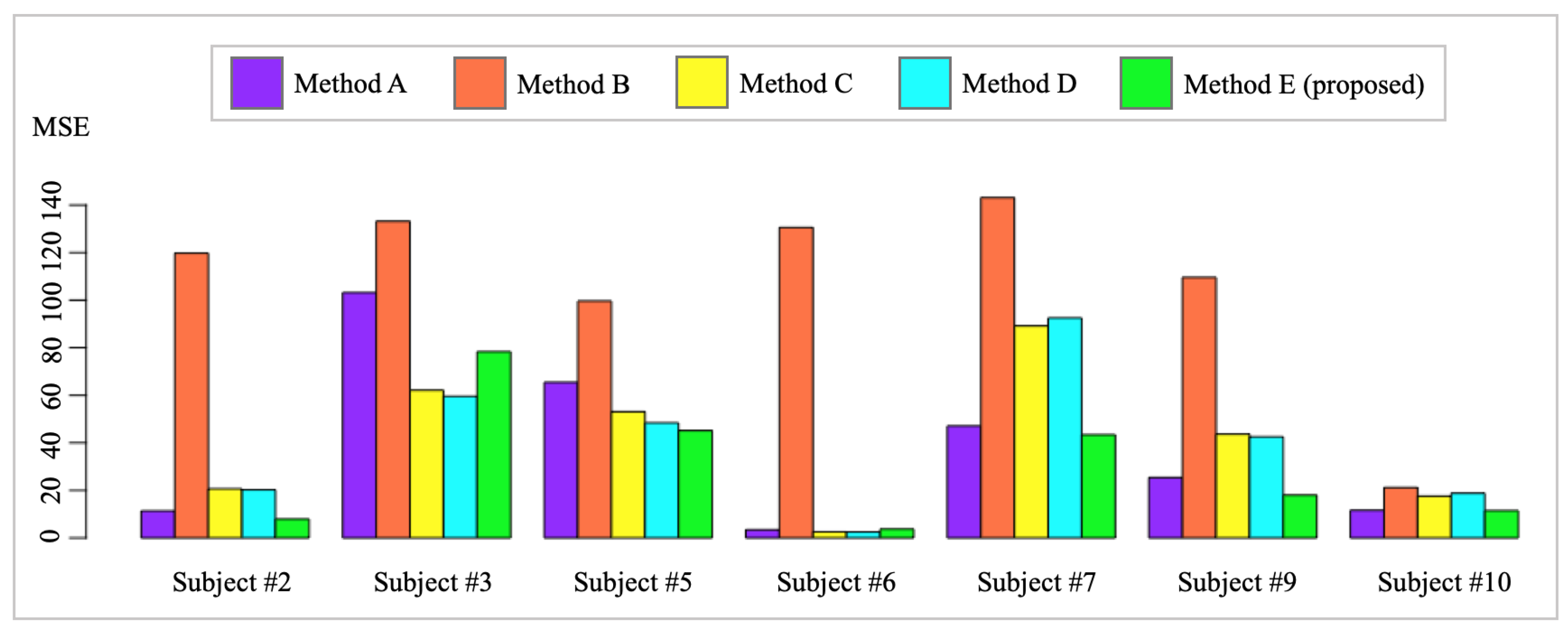
3.2. HR Pattern Calibration
- Method A: raw Garmin HR measurements;
- Method B: population mean of all subjects;
- Method C: subject-specific mean;
- Method D: functional mean of subject-specific HR;
- Method E: functional mean of calibrated HR. (proposed method)
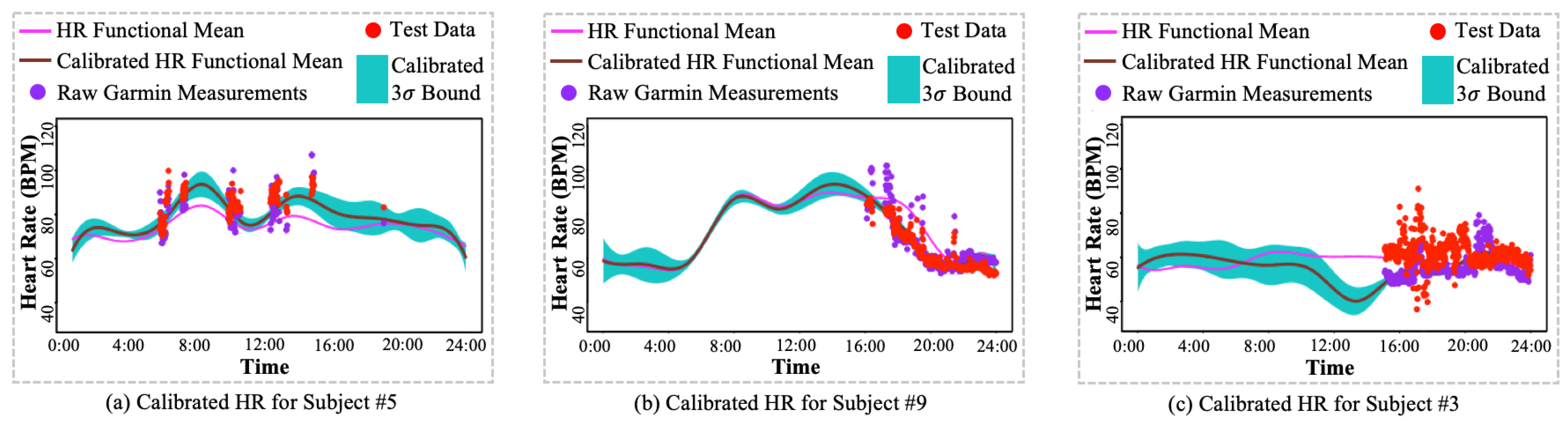
- I.: Large variations from Polar H10 HR measurements. The Polar H10 HR measurements are selected as the HR measurements ground truth because of its use of ECG to allow accurate elimination of artifacts, which offers high precision and accuracy. As shown in Figure 8a,b, the Polar H10 HR measurements, i.e., test data (red dots), provide more precise and accurate HR measurements than raw Garmin HR measurements (purple dots). However, as shown in Figure 8c, subject #3’s Polar H10 HR measurements have much higher variations than the Garmin HR measurements. Such abnormal Polar H10 HR measurements can be caused by the sensor displacement or malfunction, which needs to be further investigated.
- II.: Large HR magnitude discrepancy between Polar H10 HR measurements and Garmin HR measurements. The proposed method was developed to mitigate the impact of missing values and large variations from the wearable devices. As shown in Figure 8a,b, the calibrated HR functional mean provides a complete and precise HR estimation by the proposed method. However, as shown in Figure 8c, most of the raw Garmin HR measurements are much lower than the test data, i.e., Polar H10 HR measurements, leading to an underestimation of HR by the proposed method. The large HR magnitude discrepancy between Polar H10 HR measurements and Garmin HR measurements may be caused by the sensor inaccuracy or malfunction, which cannot be solved by the proposed method.
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wilmoth, J.; Bas, D.; Mukherjee, S.; Hanif, N. Others World Social Report 2023: Leaving No One behind in an Ageing World; UN: New York, NY, USA, 2023. [Google Scholar]
- Soon, S.; Svavarsdottir, H.; Downey, C.; Jayne, D. Wearable devices for remote vital signs monitoring in the outpatient setting: An overview of the field. BMJ Innov. 2020, 6, 55–71. [Google Scholar] [CrossRef]
- Wang, J.; Spicher, N.; Warnecke, J.; Haghi, M.; Schwartze, J.; Deserno, T. Unobtrusive health monitoring in private spaces: The smart home. Sensors 2021, 21, 864. [Google Scholar] [CrossRef] [PubMed]
- Olmedo-Aguirre, J.; Reyes-Campos, J.; Alor-Hernández, G.; Machorro-Cano, I.; Rodríguez-Mazahua, L.; Sánchez-Cervantes, J. Remote healthcare for elderly people using wearables: A review. Biosensors 2022, 12, 73. [Google Scholar] [CrossRef] [PubMed]
- Achten, J.; Jeukendrup, A. Heart rate monitoring: Applications and limitations. Sports Med. 2003, 33, 517–538. [Google Scholar] [CrossRef] [PubMed]
- Saxena, A.; Minton, D.; Lee, D.; Sui, X.; Fayad, R.; Lavie, C.; Blair, S. Protective role of resting heart rate on all-cause and cardiovascular disease mortality. Mayo Clin. Proc. 2013, 88, 1420–1426. [Google Scholar] [CrossRef] [PubMed]
- Prince, M.; Wu, F.; Guo, Y.; Robledo, L.; O’Donnell, M.; Sullivan, R.; Yusuf, S. The burden of disease in older people and implications for health policy and practice. Lancet 2015, 385, 549–562. [Google Scholar] [CrossRef] [PubMed]
- Rizzuto, D.; Bellocco, R.; Kivipelto, M.; Clerici, F.; Wimo, A.; Fratiglioni, L. Dementia after age 75: Survival in different severity stages and years of life lost. Curr. Alzheimer Res. 2012, 9, 795–800. [Google Scholar] [CrossRef]
- Freilich, S.; Barker, R. Others Predicting falls risk in patients: The value of cardiovascular variability assessment. Br. J. Med. Pract. 2009, 2, 44–48. [Google Scholar]
- Hossain, T.; Ahad, M.; Inoue, S. A method for sensor-based activity recognition in missing data scenario. Sensors 2020, 20, 3811. [Google Scholar] [CrossRef]
- Di, J.; Demanuele, C.; Kettermann, A.; Karahanoglu, F.; Cappelleri, J.; Potter, A.; Bury, D.; Cedarbaum, J.; Byrom, B. Considerations to address missing data when deriving clinical trial endpoints from digital health technologies. Contemp. Clin. Trials 2022, 113, 106661. [Google Scholar] [CrossRef]
- Bent, B.; Goldstein, B.; Kibbe, W.; Dunn, J. Investigating sources of inaccuracy in wearable optical heart rate sensors. NPJ Digit. Med. 2020, 3, 18. [Google Scholar] [CrossRef] [PubMed]
- Ludwig, M.; Hoffmann, K.; Endler, S.; Asteroth, A.; Wiemeyer, J. Measurement, prediction, and control of individual heart rate responses to exercise—Basics and options for wearable devices. Front. Physiol. 2018, 9, 778. [Google Scholar] [CrossRef] [PubMed]
- Castaneda, D.; Esparza, A.; Ghamari, M.; Soltanpur, C.; Nazeran, H. A review on wearable photoplethysmography sensors and their potential future applications in health care. Int. J. Biosens. Bioelectron. 2018, 4, 195. [Google Scholar]
- Newgard, C.; Lewis, R. Missing data: How to best account for what is not known. JAMA 2015, 314, 940–941. [Google Scholar] [CrossRef] [PubMed]
- Sprint, G.; Cook, D.; Weeks, D.; Dahmen, J.; La Fleur, A. Analyzing sensor-based time series data to track changes in physical activity during inpatient rehabilitation. Sensors 2017, 17, 2219. [Google Scholar] [CrossRef] [PubMed]
- Feng, J.; Li, Y.; Zhang, C.; Sun, F.; Meng, F.; Guo, A.; Jin, D. Deepmove: Predicting human mobility with attentional recurrent networks. In Proceedings of the 2018 World Wide Web Conference, Lyon, France, 23–27 April 2018; pp. 1459–1468. [Google Scholar]
- Cao, B.; Zheng, L.; Zhang, C.; Yu, P.; Piscitello, A.; Zulueta, J.; Ajilore, O.; Ryan, K.; Leow, A. Deepmood: Modeling mobile phone typing dynamics for mood detection. In Proceedings of the 23rd ACM SIGKDD International Conference on Knowledge Discovery 502 and Data Mining, Halifax, NS, Canada, 13–17 August 2017; pp. 747–755. [Google Scholar]
- Staffini, A.; Svensson, T.; Chung, U.; Svensson, A. Heart rate modeling and prediction using autoregressive models and deep learning. Sensors 2021, 22, 34. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.; Chen, J.; Zhang, R. Heart Rate Estimation from Incomplete Electrocardiography Signals. Sensors 2023, 23, 597. [Google Scholar] [CrossRef] [PubMed]
- Clifton, L.; Clifton, D.; Pimentel, M.; Watkinson, P.; Tarassenko, L. Gaussian processes for personalized e-health monitoring with wearable sensors. IEEE Trans. Biomed. Eng. 2012, 60, 193–197. [Google Scholar] [CrossRef] [PubMed]
- Hu, Z.; Du, D. A new analytical framework for missing data imputation and classification with uncertainty: Missing data imputation and heart failure readmission prediction. PLoS ONE 2020, 15, e0237724. [Google Scholar] [CrossRef]
- Henriques, T.; Ribeiro, M.; Teixeira, A.; Castro, L.; Antunes, L.; Costa-Santos, C. Nonlinear methods most applied to heart-rate time series: A review. Entropy 2020, 22, 309. [Google Scholar] [CrossRef]
- Ismail, S.; Akram, U.; Siddiqi, I. Heart rate tracking in photoplethysmography signals affected by motion artifacts: A review. EURASIP J. Adv. Signal Process. 2021, 2021, 5. [Google Scholar] [CrossRef]
- Ullah, S.; Finch, C. Applications of functional data analysis: A systematic review. BMC Med. Res. Methodol. 2013, 13, 5. [Google Scholar] [CrossRef] [PubMed]
- Makowski, D.; Pham, T.; Lau, Z.; Brammer, J.; Lespinasse, F.; Pham, H.; Schölzel, C.; Chen, S. NeuroKit2: A Python toolbox for neurophysiological signal processing. Behav. Res. Methods 2021, 53, 1689–1696. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Wang, K.; Chen, N. Monitoring wafers’ geometric quality using an additive Gaussian process model. IIE Trans. 2016, 48, 1–15. [Google Scholar] [CrossRef]
- Nayak, S.; Pradhan, B.; Mohanty, B.; Sivaraman, J.; Ray, S.; Wawrzyniak, J.; Jarzębski, M.; Pal, K. A Review of Methods and Applications for a Heart Rate Variability Analysis. Algorithms 2023, 16, 433. [Google Scholar] [CrossRef]
- Cajal, D.; Hernando, D.; Lázaro, J.; Laguna, P.; Gil, E.; Bailón, R. Effects of missing data on heart rate variability metrics. Sensors 2022, 22, 5774. [Google Scholar] [CrossRef] [PubMed]
- Liu, F.; Panagiotakos, D. Real-world data: A brief review of the methods, applications, challenges and opportunities. BMC Med. Res. Methodol. 2022, 22, 287. [Google Scholar] [CrossRef]
- Hilden, P. Analysis Approaches for Wearable Device Data. Doctoral Thesis, Columbia University, New York, NY, USA, 2021. [Google Scholar]
- Zhang, T.; Du, X.; Gu, Y.; Dong, Y.; Zhang, W.; Yuan, Z.; Huang, X.; Zou, C.; Zhou, Y.; Liu, Z. Others Analysis of Diurnal Variations in Heart Rate: Potential Applications for Chronobiology and Cardiovascular Medicine. Front. Physiol. 2022, 13, 325. [Google Scholar]



| Characteristic | Value (10 Subjects) |
|---|---|
| Age | 79.6 (5.7) * years old |
| Sex | 5 male, 5 female |
| Ethnicity | Number of Subjects (Percentage) |
| Hispanic or Latino | 3 (30%) |
| White | 3 (30%) |
| Black or African American | 2 (20%) |
| American Indian or Alaska Native | 1 (10%) |
| Asian American | 1 (10%) |
| Health Condition | Number of Subjects (Percentage) |
| High Blood Pressure | 8 (80%) |
| Hypotension | 2 (20%) |
| Dyslipidemia | 7 (70%) |
| Ischemic/Coronary Heart Disease | 2 (22%); one missed |
| Diabetes | 4 (40%) |
| Chronic Kidney Disease | 6 (60%) |
| Hypothyroidism | 4 (40%) |
| Heart Failure | 1 (11%); one missed |
| Depression | 5 (50%) |
| Dementia/Alzheimer’s Disease | 7 (70%) |
| Chronic Obstructive Pulmonary Disease | 1 (10%) |
| With Medicine of Changing Heart Rate | 5 (50%) |
| Subject ID | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| #1 | #2 | #3 | #4 | #5 | #6 | #7 | #8 | #9 | #10 | |
| Garmin Missing Data Rate | 0.4209 | 0.1700 | 0.1809 | 0.2709 | 0.1150 | 0.3076 | 0.2371 | - | 0.1725 | 0.2617 |
| Days of Data Collection | 16 | 16 | 15 | 12 | 15 | 14 | 15 | - | 13 | 16 |
| Subject ID | Method A | Method B | Method C | Method D | Method E |
|---|---|---|---|---|---|
| #2 | 11.36 (1.96) § | 119.78 (3.26) | 20.66 (2.35) | 20.25 (2.28) | 7.92 * (1.63) * |
| #3 | 103.19 (6.80) | 133.18 (5.39) | 62.10 (5.75) | 59.56 (5.67) | 78.31 (6.16) |
| #5 | 65.48 (4.50) | 99.63 (5.21) | 53.10 (3.96) | 48.40 (3.82) | 45.12 (4.27) |
| #6 | 3.42 (1.66) | 130.60 (3.74) | 2.57 (1.45) | 2.50 (1.46) | 3.74 (1.57) |
| #7 | 47.07 (4.62) | 143.14 (5.76) | 89.17 (5.40) | 92.53 (5.22) | 43.42 (4.64) |
| #9 | 25.41 (3.65) | 109.60 (3.62) | 43.67 (3.98) | 42.55 (3.91) | 17.98 (2.74) |
| #10 | 11.59 (2.66) | 21.20 (3.52) | 17.58 (2.81) | 18.75 (2.79) | 11.46 (2.41) |
| Overall | 49.15 (5.31) | 97.32 (5.53) | 42.48 (4.61) | 40.13 (4.38) | 35.83 (4.25) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xia, S.; Wung, S.-F.; Chen, C.-C.; Coompson, J.L.K.; Roveda, J.; Liu, J. Data-Fusion-Based Quality Enhancement for HR Measurements Collected by Wearable Sensors. Sensors 2024, 24, 2970. https://doi.org/10.3390/s24102970
Xia S, Wung S-F, Chen C-C, Coompson JLK, Roveda J, Liu J. Data-Fusion-Based Quality Enhancement for HR Measurements Collected by Wearable Sensors. Sensors. 2024; 24(10):2970. https://doi.org/10.3390/s24102970
Chicago/Turabian StyleXia, Shenghao, Shu-Fen Wung, Chang-Chun Chen, Jude Larbi Kwesi Coompson, Janet Roveda, and Jian Liu. 2024. "Data-Fusion-Based Quality Enhancement for HR Measurements Collected by Wearable Sensors" Sensors 24, no. 10: 2970. https://doi.org/10.3390/s24102970
APA StyleXia, S., Wung, S. -F., Chen, C. -C., Coompson, J. L. K., Roveda, J., & Liu, J. (2024). Data-Fusion-Based Quality Enhancement for HR Measurements Collected by Wearable Sensors. Sensors, 24(10), 2970. https://doi.org/10.3390/s24102970







