The Agreement between Wearable Sensors and Force Plates for the Analysis of Stride Time Variability
Abstract
1. Introduction
2. Methods
2.1. Participants
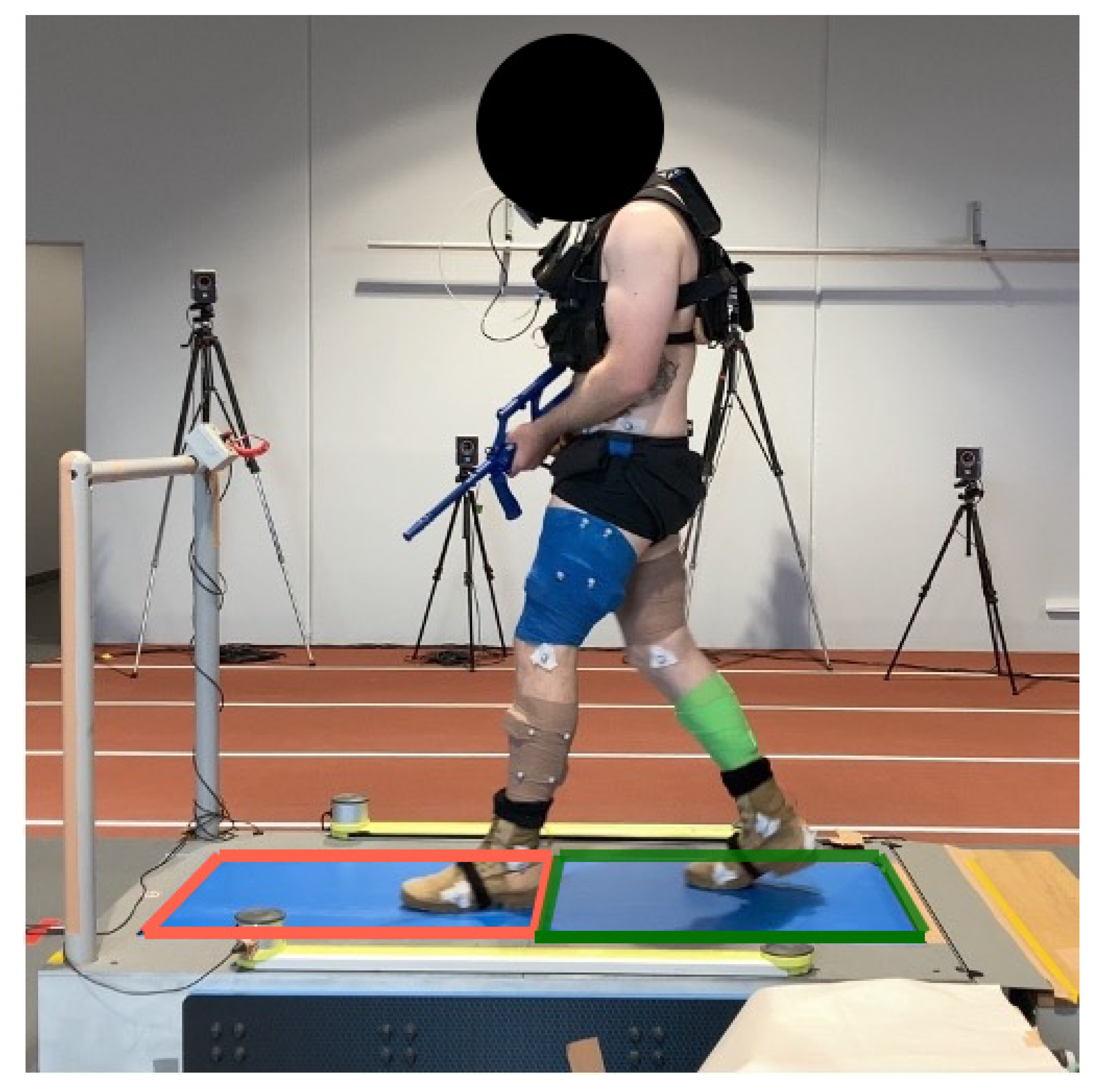
2.2. Experimental Overview
2.3. Data Analysis
2.3.1. Instrumented Treadmill
2.3.2. Wearable Sensors
2.4. Data Processing
2.5. Statistical Analysis
3. Results
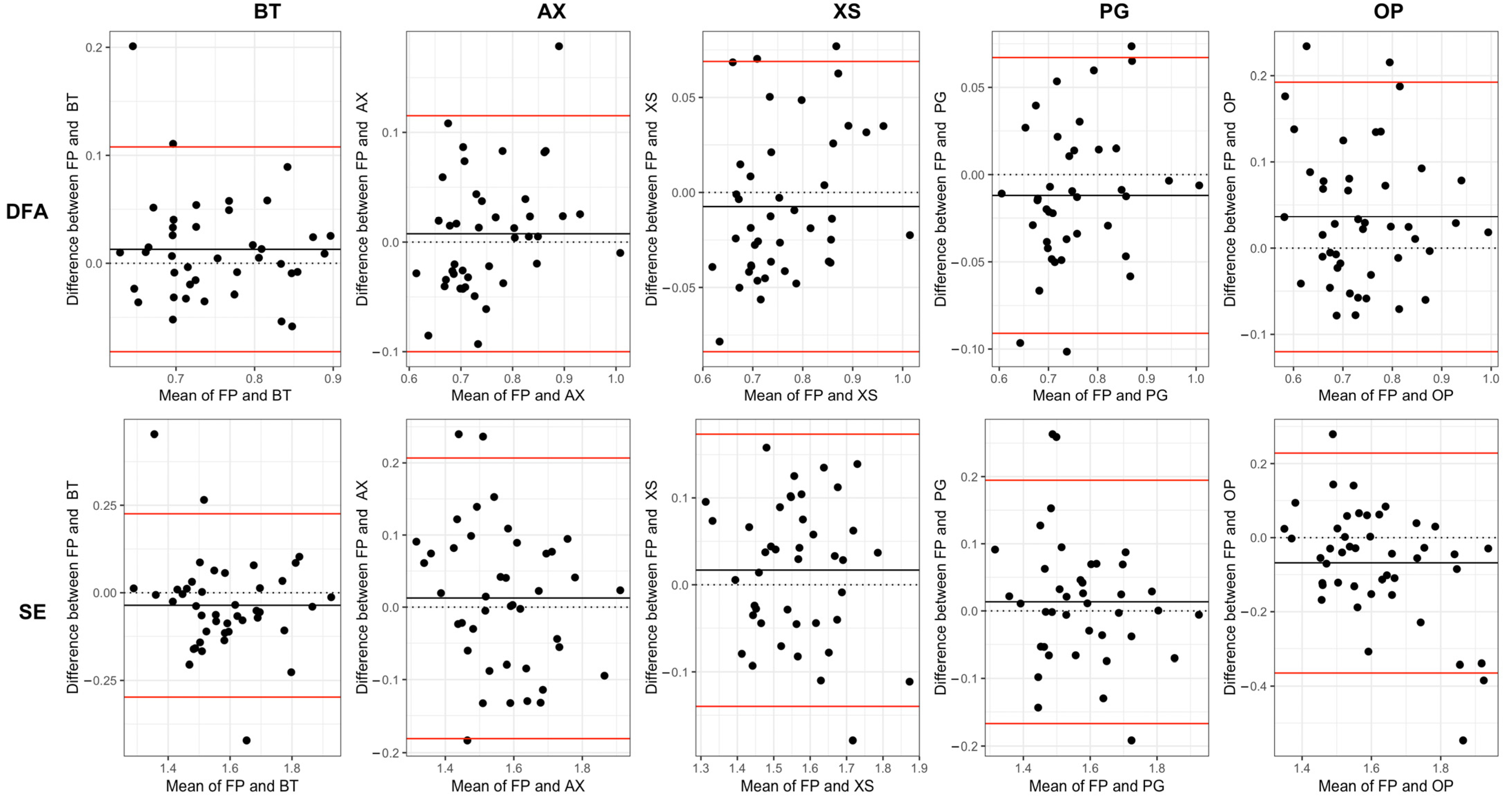
3.1. Absolute Agreement
3.2. Relative Agreement
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| BT | AX | XS | PG | OP | |
|---|---|---|---|---|---|
| SD | 0.97 | 0.98 | 0.98 | 0.99 | 0.87 |
| CV | 0.97 | 0.98 | 0.98 | 0.99 | 0.90 |
| DFA | 0.84 | 0.82 | 0.83 | 0.88 | 0.60 |
| SE | 0.5 | −0.03 | −0.03 | 0.63 | 0.01 |
| BT | AX | XS | PG | OP | |
|---|---|---|---|---|---|
| SD | 0.97 | 0.98 | 0.98 | 0.99 | 0.93 |
| CV | 0.97 | 0.98 | 0.99 | 0.99 | 0.94 |
| DFA | 0.83 | 0.87 | 0.90 | 0.89 | 0.72 |
| SE | 0.68 | −0.03 | −0.09 | 0.66 | 0.01 |
References
- Dijksma, I.; Sharma, J.; Gabbett, T.J. Training load monitoring and injury prevention in military recruits: Considerations for preparing soldiers to fight sustainably. Strength Cond. J. 2021, 43, 23–30. [Google Scholar] [CrossRef]
- Warfe, P.; Jones, D.; Prigg, S. Developing injury prevention strategies for the australian defence force. J. Mil. Veterans’ Health 2011, 19, 45. [Google Scholar]
- Schram, B.; Pope, R.; Orr, R. Injuries in australian army full-time and part-time personnel undertaking basic training. BMC Musculoskelet. Disord. 2019, 20, 6. [Google Scholar] [CrossRef] [PubMed]
- Lyons, K.D.; Parks, A.G.; Dadematthews, O.; Zandieh, N.; McHenry, P.; Games, K.E.; Goodlett, M.D.; Murrah, W.; Roper, J.; Sefton, J.M. Core and whole body vibration exercise influences muscle sensitivity and posture during a military foot march. Int. J. Environ. Res. Public Health 2021, 18, 4966. [Google Scholar] [CrossRef]
- Almeida, S.A.; Williams, K.M.; Shaffer, R.A.; Brodine, S.K. Epidemiological patterns of musculoskeletal injuries and physical training. Med. Sci. Sports Exerc. 1999, 31, 1176–1182. [Google Scholar] [CrossRef]
- Orr, R.M.; Coyle, J.; Johnston, V.; Pope, R. Self-reported load carriage injuries of military soldiers. Int. J. Inj. Control Saf. Promot. 2017, 24, 189–197. [Google Scholar] [CrossRef]
- Hauschild, V.; Roy, T.; Grier, T.; Schuh, A.; Jones, B.H. Foot Marching, Load Carriage, and Injury Risk; Army Public Health Center Aberdeen Proving Ground: Edgewood, MD, USA, 2016. [Google Scholar]
- Rudzki, S.J. Injuries in australian army recruits. Part I: Decreased incidence and severity of injury seen with reduced running distance. Mil. Med. 1997, 162, 472–476. [Google Scholar] [CrossRef]
- Sherrard, J.; Lenne, M.; Cassell, E.; Stokes, M.; Ozanne-Smith, J. Injury prevention during physical activity in the australian defence force. J. Sci. Med. Sport 2004, 7, 106–117. [Google Scholar] [CrossRef] [PubMed]
- Grenier, J.G.; Peyrot, N.; Castells, J.; Oullion, R.; Messonnier, L.; Morin, J.B. Energy cost and mechanical work of walking during load carriage in soldiers. Med. Sci. Sports Exerc. 2012, 44, 1131–1140. [Google Scholar] [CrossRef]
- LaFiandra, M.; Wagenaar, R.C.; Holt, K.G.; Obusek, J.P. How do load carriage and walking speed influence trunk coordination and stride parameters? J. Biomech. 2003, 36, 87–95. [Google Scholar] [CrossRef]
- Kroneberg, D.; Elshehabi, M.; Meyer, A.C.; Otte, K.; Doss, S.; Paul, F.; Nussbaum, S.; Berg, D.; Kuhn, A.A.; Maetzler, W.; et al. Less is more—Estimation of the number of strides required to assess gait variability in spatially confined settings. Front. Aging Neurosci. 2018, 10, 435. [Google Scholar] [CrossRef] [PubMed]
- Hausdorff, J.M.; Rios, D.A.; Edelberg, H.K. Gait variability and fall risk in community-living older adults: A 1-year prospective study. Arch. Phys. Med. Rehabil. 2001, 82, 1050–1056. [Google Scholar] [CrossRef]
- Zanardi, A.P.J.; da Silva, E.S.; Costa, R.R.; Passos-Monteiro, E.; Santos, I.O.D.; Kruel, L.F.M.; Peyre-Tartaruga, L.A. Gait parameters of parkinson’s disease compared with healthy controls: A systematic review and meta-analysis. Sci. Rep. 2021, 11, 752. [Google Scholar] [CrossRef] [PubMed]
- Springer, S.; Gottlieb, U.; Lozin, M. Spatiotemporal gait parameters as predictors of lower-limb overuse injuries in military training. Sci. World J. 2016, 2016, 5939164. [Google Scholar] [CrossRef] [PubMed]
- Di Bacco, V.E.; Gage, W.H. Evaluation of a smartphone accelerometer system for measuring nonlinear dynamics during treadmill walking: Concurrent validity and test-retest reliability. J. Biomech. 2023, 151, 111527. [Google Scholar] [CrossRef] [PubMed]
- Almurad, Z.M.H.; Delignières, D. Evenly spacing in detrended fluctuation analysis. Phys. A Stat. Mech. Its Appl. 2016, 451, 63–69. [Google Scholar] [CrossRef]
- Marmelat, V.; Torre, K.; Beek, P.J.; Daffertshofer, A. Persistent fluctuations in stride intervals under fractal auditory stimulation. PLoS ONE 2014, 9, e91949. [Google Scholar] [CrossRef] [PubMed]
- Alkjaer, T.; Raffalt, P.C.; Dalsgaard, H.; Simonsen, E.B.; Petersen, N.C.; Bliddal, H.; Henriksen, M. Gait variability and motor control in people with knee osteoarthritis. Gait Posture 2015, 42, 479–484. [Google Scholar] [CrossRef] [PubMed]
- Warlop, T.; Detrembleur, C.; Stoquart, G.; Lejeune, T.; Jeanjean, A. Gait complexity and regularity are differently modulated by treadmill walking in parkinson’s disease and healthy population. Front. Physiol. 2018, 9, 68. [Google Scholar] [CrossRef]
- Hreljac, A.; Marshall, R.N. Algorithms to determine event timing during normal walking using kinematic data. J. Biomech. 2000, 33, 783–786. [Google Scholar] [CrossRef]
- Hansen, A.H.; Childress, D.S.; Meier, M.R. A simple method for determination of gait events. J. Biomech. 2002, 35, 135–138. [Google Scholar] [CrossRef] [PubMed]
- Sun, R.; Moon, Y.; McGinnis, R.S.; Seagers, K.; Motl, R.W.; Sheth, N.; Wright, J.A.; Ghaffari, R.; Patel, S.; Sosnoff, J.J. Assessment of postural sway in individuals with multiple sclerosis using a novel wearable inertial sensor. Digit. Biomark. 2018, 2, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Lach, J.; Lo, B.; Yang, G.Z. Toward pervasive gait analysis with wearable sensors: A systematic review. IEEE J. Biomed. Health Inform. 2016, 20, 1521–1537. [Google Scholar] [CrossRef] [PubMed]
- Johnston, W.; Patterson, M.; O’Mahony, N.; Caulfield, B. Validation and comparison of shank and lumbar-worn imus for step time estimation. Biomed. Tech. 2017, 62, 537–545. [Google Scholar] [CrossRef] [PubMed]
- Patterson, M.; Johnston, W.; O’Mahony, N.; O’Mahony, S.; Nolan, E.; Caulfield, B. Validation of temporal gait metrics from three imu locations to the gold standard force plate. In Proceedings of the 2016 38th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Orlando, FL, USA, 16–20 August 2016; Volume 2016, pp. 667–671. [Google Scholar]
- Kobsar, D.; Charlton, J.M.; Tse, C.T.F.; Esculier, J.F.; Graffos, A.; Krowchuk, N.M.; Thatcher, D.; Hunt, M.A. Validity and reliability of wearable inertial sensors in healthy adult walking: A systematic review and meta-analysis. J. Neuroeng. Rehabil. 2020, 17, 62. [Google Scholar] [CrossRef] [PubMed]
- Rantalainen, T.; Karavirta, L.; Pirkola, H.; Rantanen, T.; Linnamo, V. Gait variability using waist- and ankle-worn inertial measurement units in healthy older adults. Sensors 2020, 20, 2858. [Google Scholar] [CrossRef] [PubMed]
- Pacini Panebianco, G.; Bisi, M.C.; Stagni, R.; Fantozzi, S. Analysis of the performance of 17 algorithms from a systematic review: Influence of sensor position, analysed variable and computational approach in gait timing estimation from imu measurements. Gait Posture 2018, 66, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Bailey, C.A.; Uchida, T.K.; Nantel, J.; Graham, R.B. Validity and sensitivity of an inertial measurement unit-driven biomechanical model of motor variability for gait. Sensors 2021, 21, 7690. [Google Scholar] [CrossRef] [PubMed]
- Phinyomark, A.; Larracy, R.; Scheme, E. Fractal analysis of human gait variability via stride interval time series. Front. Physiol. 2020, 11, 333. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Cofré Lizama, L.E.; Wheat, J.; Slattery, P.; Middleton, K. Can handling a weapon make soldiers more unstable? Ergonomics 2023, 66, 1246–1254. [Google Scholar] [CrossRef] [PubMed]
- Matlab. 2022. The MathWorks, Inc.: Natick, Massachusetts. Available online: https://www.mathworks.com/ (accessed on 1 March 2022).
- Ravi, D.K.; Marmelat, V.; Taylor, W.R.; Newell, K.M.; Stergiou, N.; Singh, N.B. Assessing the temporal organization of walking variability: A systematic review and consensus guidelines on detrended fluctuation analysis. Front. Physiol. 2020, 11, 562. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2023. [Google Scholar]
- Liddy, J.J.; Haddad, J.M. Evenly spaced detrended fluctuation analysis: Selecting the number of points for the diffusion plot. Phys. A Stat. Mech. Its Appl. 2018, 491, 233–248. [Google Scholar] [CrossRef]
- Richman, J.S.; Moorman, J.R. Physiological time-series analysis using approximate entropy and sample entropy. Am. J. Physiol. Heart Circ. Physiol. 2000, 278, H2039–H2049. [Google Scholar] [CrossRef] [PubMed]
- Hoaglin, D.C. Volume 16: How to Detect and Handle Outliers; Quality Press: Milwaukee, WI, USA, 2013. [Google Scholar]
- Gamer, M.; Lemon, J.; Singh, I.F.P. Irr: Various Coefficients of Interrater Reliability and Agreement; R Foundation for Statistical Computing: Vienna, Austria, 2019. [Google Scholar]
- Koo, T.K.; Li, M.Y. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Datta, D. Blandr: A Bland-Altman Method Comparison Package for R; R Foundation for Statistical Computing: Vienna, Austria, 2017. [Google Scholar]
- Hamner, B.; Frasco, M. Metrics: Evaluation Metrics for Machine Learning; R Foundation for Statistical Computing: Vienna, Austria, 2018. [Google Scholar]
- Rantalainen, T.; Pirkola, H.; Karavirta, L.; Rantanen, T.; Linnamo, V. Reliability and concurrent validity of spatiotemporal stride characteristics measured with an ankle-worn sensor among older individuals. Gait Posture 2019, 74, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Marmelat, V.; Duncan, A.; Meltz, S. Effect of sampling frequency on fractal fluctuations during treadmill walking. PLoS ONE 2019, 14, e0218908. [Google Scholar] [CrossRef] [PubMed]
- Liddy, J.J.; Ducharme, S.W.; van Emmerik, R.E.A.; Haddad, J.M. Temporal correlations in human locomotion: Recommendations for sampling rate and foot strike detection. Phys. A Stat. Mech. Its Appl. 2019, 532, 121784. [Google Scholar] [CrossRef]
- Wijnants, M.L.; Cox, R.F.; Hasselman, F.; Bosman, A.M.; Van Orden, G. Does sample rate introduce an artifact in spectral analysis of continuous processes? Front. Physiol. 2012, 3, 495. [Google Scholar] [CrossRef]
- Rhea, C.K.; Kiefer, A.W.; Wright, W.G.; Raisbeck, L.D.; Haran, F.J. Interpretation of postural control may change due to data processing techniques. Gait Posture 2015, 41, 731–735. [Google Scholar] [CrossRef]
- Raffalt, P.C.; McCamley, J.; Denton, W.; Yentes, J.M. Sampling frequency influences sample entropy of kinematics during walking. Med. Biol. Eng. Comput. 2019, 57, 759–764. [Google Scholar] [CrossRef] [PubMed]
- Raffalt, P.; Alkjær, T.; Brynjólfsson, B.; Rgensen, L.; Bartholdy, C.; Henriksen, M. Test-retest reliability of non-linear methods to assess walking dynamics. J. Biomech. Eng. 2018, 140, 124501. [Google Scholar] [CrossRef] [PubMed]
- Coates, L.; Shi, J.; Rochester, L.; Del Din, S.; Pantall, A. Entropy of real-world gait in parkinson’s disease determined from wearable sensors as a digital marker of altered ambulatory behavior. Sensors 2020, 20, 2631. [Google Scholar] [CrossRef] [PubMed]
- Moveo Explorer. 2020, Moveo Technologies Inc. Available online: https://share.apdm.com/documentation/MoveoExplorerUserGuide.pdf (accessed on 5 February 2021).


| Measure | FP (Left) | FP (Right) | BT | AX | XS | PG | OP |
|---|---|---|---|---|---|---|---|
| Mean (s) | 1.03 ± 0.05 | 1.03 ± 0.05 | 1.03 ± 0.05 | 1.01 ± 0.05 + | 1.03 ± 0.05 + | 1.03 ± 0.05 | 1.04 ± 0.05 + |
| SD (ms) | 14.35 ± 2.84 | 14.49 ± 2.88 | 14.61 ± 2.85 | 14.35 ± 3.26 * | 14.5 ± 3.26 | 14.54 ± 3.35 | 15.24 ± 3.22 + |
| RMSE | 0.56 | 0.82 | 0.51 | 0.54 | 1.70 | ||
| CV (%) | 1.40 ± 0.30 | 1.41 ± 0.30 | 1.43 ± 0.30 | 1.43 ± 0.33 | 1.41 ± 0.33 | 1.42 ± 0.34 | 1.48 ± 0.33 + |
| RMSE | 0.06 | 0.06 | 0.05 | 0.05 | 0.16 | ||
| DFA (α) | 0.76 ± 0.10 | 0.75 ± 0.10 | 0.74 ± 0.08 | 0.76 ± 0.10 | 0.78 ± 0.10 | 0.77 ± 0.10 | 0.72 ± 0.11 + |
| RMSE | 0.05 | 0.06 | 0.04 | 0.04 | 0.09 | ||
| SE (S) | 1.58 ± 0.13 | 1.57 ± 0.15 | 1.6 ± 0.17 | 1.56 ± 0.16 | 1.56 ± 0.13 | 1.57 ± 0.15 | 1.65 ± 0.20 + |
| RMSE | 0.14 | 0.10 | 0.08 | 0.09 | 0.16 |
| BT | AX | XS | PG | OP | |
|---|---|---|---|---|---|
| SD | 0.98 | 0.96 | 0.98 | 0.98 | 0.85 |
| CV | 0.98 | 0.94 | 0.97 | 0.97 | 0.88 |
| DFA | 0.80 | 0.82 | 0.92 | 0.89 | 0.67 |
| SE | 0.63 | 0.77 | 0.80 | 0.79 | 0.57 |
| BT | AX | XS | PG | OP | |
|---|---|---|---|---|---|
| SD | 0.98 | 0.97 | 0.99 | 0.99 | 0.88 |
| CV | 0.98 | 0.98 | 0.97 | 0.99 | 0.90 |
| DFA | 0.81 | 0.89 | 0.91 | 0.90 | 0.71 |
| SE | 0.65 | 0.78 | 0.80 | 0.80 | 0.66 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Slattery, P.; Cofré Lizama, L.E.; Wheat, J.; Gastin, P.; Dascombe, B.; Middleton, K. The Agreement between Wearable Sensors and Force Plates for the Analysis of Stride Time Variability. Sensors 2024, 24, 3378. https://doi.org/10.3390/s24113378
Slattery P, Cofré Lizama LE, Wheat J, Gastin P, Dascombe B, Middleton K. The Agreement between Wearable Sensors and Force Plates for the Analysis of Stride Time Variability. Sensors. 2024; 24(11):3378. https://doi.org/10.3390/s24113378
Chicago/Turabian StyleSlattery, Patrick, L. Eduardo Cofré Lizama, Jon Wheat, Paul Gastin, Ben Dascombe, and Kane Middleton. 2024. "The Agreement between Wearable Sensors and Force Plates for the Analysis of Stride Time Variability" Sensors 24, no. 11: 3378. https://doi.org/10.3390/s24113378
APA StyleSlattery, P., Cofré Lizama, L. E., Wheat, J., Gastin, P., Dascombe, B., & Middleton, K. (2024). The Agreement between Wearable Sensors and Force Plates for the Analysis of Stride Time Variability. Sensors, 24(11), 3378. https://doi.org/10.3390/s24113378






