Determinants of Perceived Comfort: Multi-Dimensional Thinking in Smart Bedding Design
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Settings
2.2. Participants
2.3. Variables and Measurement
2.4. Procedure
2.5. Statistical Data Analysis
3. Results
3.1. Descriptive Statistics
3.2. Main Results
3.2.1. Relationship between Body Pressure and Perceived Comfort
3.2.2. Influence of Condition on Perceived Comfort
3.2.3. Multivariate Factors of Perceived Comfort
4. Discussion
- The results of the study indicated that, after adjusting for other factors, only mean pressure showed a negative correlation with buttocks and thigh comfort.
- The body pressure distribution and comfort did not always change in tandem, possibly due to the fact that large changes in bed condition lead to instability in users’ body postures, requiring additional muscle activity. This consequently results in stretching and fatigue of the back and buttock muscles.
- Sleep posture has consistently been a major influence on perceived comfort.
- When the head or foot of the smart bed was lifted too high without corresponding support on the other side, the comfort level dropped sharply. Consideration can be given to adding a linkage mechanism in the next design. This mechanism would adjust the leg board height proportionally when the back board is lifted or lowered, achieving relative body balance.
- The variation in body pressure and comfort across different conditions of the smart bed is significant, and can prevent excessive accumulation of pressure in specific areas. It is feasible to explore the implementation pathway of smart bedding in reducing health risks and improving health status (such as pressure ulcers and obstructive sleep apnea) through special designs.
5. Strengths and Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kent, R.G.; Uchino, B.N.; Cribbet, M.R.; Bowen, K.; Smith, T.W. Social Relationships and Sleep Quality. Ann. Behav. Med. 2015, 49, 912–917. [Google Scholar] [CrossRef]
- Souza, F.J.F.d.B.; Genta, P.R.; de Souza Filho, A.J.; Wellman, A.; Lorenzi-Filho, G. The influence of head-of-bed elevation in patients with obstructive sleep apnea. Sleep Breath. 2017, 21, 815–820. [Google Scholar] [CrossRef]
- Brush, Z.; Bowling, A.; Tadros, M.; Russell, M. Design and control of a smart bed for pressure ulcer prevention. In Proceedings of the 2013 IEEE/ASME International Conference on Advanced Intelligent Mechatronics, Wollongong, NSW, Australia, 9–12 July 2013. [Google Scholar] [CrossRef]
- Wang, J.X.; Zhang, Y.; Liu, Y.Y. Annual Sleep Report of China 2023; Social Sciences Academic Press: Beijing, China, 2023. [Google Scholar]
- Grandner, M.A. Sleep, Health, and Society. Sleep Med. Clin. 2022, 17, 117–139. [Google Scholar] [CrossRef] [PubMed]
- Seo, E.; Bae, S.; Choi, H.; Choi, D. Preference and usability of Smart-Home services and items—A Focus on the Smart-Home living-lab. J. Asian Archit. Build. Eng. 2021, 20, 650–662. [Google Scholar] [CrossRef]
- Zemp, R.; Taylor, W.R.; Lorenzetti, S. Are pressure measurements effective in the assessment of office chair comfort/discomfort? A review. Appl. Ergon. 2015, 48, 273–282. [Google Scholar] [CrossRef]
- Styf, J.R.; Hutchinson, K.; Carlsson, S.G.; Hargens, A.R. Depression, mood state, and back pain during microgravity simulated by bed rest. Psychosom. Med. 2001, 63, 862–864. [Google Scholar] [CrossRef]
- De Looze, M.P.; Kuijt-Evers, L.F.M.; van Dieen, J. Sitting comfort and discomfort and the relationships with objective measures. Ergonomics 2003, 46, 985–997. [Google Scholar] [CrossRef] [PubMed]
- Vink, P.; Anjani, S.; Udomboonyanupap, S.; Torkashvand, G.; Albin, T.; Miguez, S.; Li, W.H.; Reuter, C.; Vanacore, A. Differences and similarities in comfort and discomfort experience in nine countries in Asia, the Americas and Europe. Ergonomics 2021, 64, 553–570. [Google Scholar] [CrossRef]
- Yang, X.; Wang, R.; Tang, C.; Luo, L.; Mo, X. Emotional design for smart product-service system: A case study on smart beds. J. Clean Prod. 2021, 298, 126823. [Google Scholar] [CrossRef]
- Ghafurian, M.; Wang, K.; Dhode, I.; Kapoor, M.; Morita, P.P.; Dautenhahn, K. Smart Home Devices for Supporting Older Adults: A Systematic Review. IEEE Access 2023, 11, 47137–47158. [Google Scholar] [CrossRef]
- Kopecek, M.; Kremlacek, J. Eye-tracking control of an adjustable electric bed: Construction and validation by immobile patients with multiple sclerosis. J. Neuroeng. Rehabil. 2023, 20, 75. [Google Scholar] [CrossRef]
- Balaei, A.T.; Sutherland, K.; Cistulli, P.; de Chazal, P. Prediction of obstructive sleep apnea using facial landmarks. Physiol. Meas. 2018, 39, 094004. [Google Scholar] [CrossRef] [PubMed]
- Haex, B. Back and Bed: Ergonomic Aspects of Sleeping; CRC Press: Boca Raton, FL, USA, 2004. [Google Scholar] [CrossRef]
- Ajami, S.; Khaleghi, L. A review on equipped hospital beds with wireless sensor networks for reducing bedsores. J. Res. Med. Sci. 2015, 20, 1007–1015. [Google Scholar] [CrossRef]
- Verhaert, V.; Van Deun, D.; Verbraecken, J.; Vandekerckhove, M.; Exadaktylos, V.; Haex, B.; Vander Sloten, J. Smart control of spinal alignment through active adjustment of mechanical bed properties during sleep. J. Ambient. Intell. Smart Environ. 2013, 5, 369–380. [Google Scholar] [CrossRef]
- Dangal, S.; Smulders, M.; Vink, P. Implementing spring-foam technology to design a lightweight and comfortable aircraft seat-pan. Appl. Ergon. 2021, 91, 103174. [Google Scholar] [CrossRef]
- Li, M.Y.; Li, B.; Chen, G.Y.; Li, H.; Ding, B.H.; Shi, C.Y.; Yu, F. Research on the design and evaluation method of vehicle seat comfort for driving experience. Int. J. Ind. Ergon. 2024, 100, 103567. [Google Scholar] [CrossRef]
- de Mare, L.; de Groot, B.; de Koning, F.; Geers, R.; Tetteroo, D. The influence of a contoured seating base on pressure distribution and discomfort. Disabil. Rehabil.-Assist. Technol. 2023, 18, 1–7. [Google Scholar] [CrossRef]
- Yao, X.H.; He, Y.F.; Udomboonyanupap, S.; Hessenberger, N.; Song, Y.; Vink, P. Measuring pressure distribution under the seat cushion and dividing the pressure map in six regions might be beneficial for comfort studies of aircraft seats. Ergonomics 2023, 66, 1594–1607. [Google Scholar] [CrossRef]
- Ebe, K.; Griffin, M.J. Factors affecting static seat cushion comfort. Ergonomics 2001, 44, 901–921. [Google Scholar] [CrossRef] [PubMed]
- Huang, S.F.; Sun, D.Y.; Zhang, L.; Zhou, J.H.; Wang, Z.H. Comfort assessment and optimization based on FE simulation for high-Speed train seats: Comparison with different design parameters. Sustainability 2022, 14, 15185. [Google Scholar] [CrossRef]
- Wegner, M.; Martic, R.; Franz, M.; Vink, P. A system to measure seat-human interaction parameters which might be comfort relevant. Appl. Ergon. 2020, 84, 103008. [Google Scholar] [CrossRef] [PubMed]
- Ren, L.Y.; Shi, Y.J.; Xu, R.M.; Wang, C.X.; Guo, Y.; Yue, H.; Ni, Z.G.; Sha, X.F.; Chen, Y.X. Effect of mattress bedding layer structure on pressure relief performance and subjective lying comfort. J. Tissue Viability 2023, 32, 9–19. [Google Scholar] [CrossRef] [PubMed]
- Park, S.J.; Kim, J.S.; Kim, C.B. Comfort evaluation and bed adjustment according to sleeping positions. Hum. Factors Ergon. Manuf. 2009, 19, 145–157. [Google Scholar] [CrossRef]
- Ito, J.; Usuki, S. Measurement and control of body pressure towards smart bed system. Int. J. Autom. Technol. 2024, 18, 104–111. [Google Scholar] [CrossRef]
- Vanacore, A.; Lanzotti, A.; Percuoco, C.; Capasso, A.; Vitolo, B. Design and analysis of comparative experiments to assess the (dis-)comfort of aircraft seating. Appl. Ergon. 2019, 76, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.L.; Chan, Y.C.; Zhang, L.P. Postural variabilities associated with the most comfortable sitting postures: A preliminary study. Q2/Z4 Healthc. 2021, 9, 1685. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Torres, M.; Porcar, R.; Solaz, J.; Romero, T. Objective firmness, average pressure and subjective perception in mattresses for the elderly. Appl. Ergon. 2008, 39, 123–130. [Google Scholar] [CrossRef] [PubMed]
- Caballero-Bruno, I.; Töpfer, D.; Wohllebe, T.; Hernández-Castellano, P.M. Assessing Car Seat Posture through Comfort and User Experience. Appl. Sci. 2022, 12, 3376. [Google Scholar] [CrossRef]
- Li Auto Inc. Hosts 2024 Spring Launch Event. Available online: https://ir.lixiang.com/news-releases/news-release-details/li-auto-inc-hosts-2024-spring-launch-event (accessed on 1 March 2024).
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P.; Initiative, S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- Bonisteel, I.; Shulman, R.; Newhook, L.A.; Guttmann, A.; Smith, S.; Chafe, R. Reconceptualizing recruitment in qualitative research. Int. J. Qual. Meth. 2021, 20, 16094069211042493. [Google Scholar] [CrossRef]
- Lindorfer, J.; Kroll, J.; Schwameder, H. Comfort assessment of running footwear: Does assessment type affect inter-session reliability? Eur. J. Sport Sci. 2019, 19, 177–185. [Google Scholar] [CrossRef] [PubMed]
- Passetti, E.; Tenucci, A. Eco-efficiency measurement and the influence of organisational factors: Evidence from large Italian companies. J. Clean Prod. 2016, 122, 228–239. [Google Scholar] [CrossRef]
- Sharma, G.; Yukhymenko-Lescroart, M.; Kang, Z. Sense of Purpose Scale: Development and initial validation. Appl. Dev. Sci. 2018, 22, 188–199. [Google Scholar] [CrossRef]
- Waongenngarm, P.; van der Beek, A.J.; Akkarakittichoke, N.; Janwantanakul, P. Perceived musculoskeletal discomfort and its association with postural shifts during 4-h prolonged sitting in office workers. Appl. Ergon. 2020, 89, 103225. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.Z.; Meng, L.; Gong, Y.; Wang, N. The influence of backrest angles on the passenger neck comfort during sleep in the economy class air seat without head support. Int. J. Ind. Ergon. 2021, 84, 103074. [Google Scholar] [CrossRef]
- Stanglmeier, M.J.; Paternoster, F.K.; Paternoster, S.; Bichler, R.J.; Wagner, P.-O.; Schwirtz, A. Automated driving: A biomechanical approach for sleeping positions. Appl. Ergon. 2020, 86, 103103. [Google Scholar] [CrossRef] [PubMed]
- Lantoine, P.; Lecocq, M.; Bougard, C.; Dousset, E.; Marqueste, T.; Bourdin, C.; Allegre, J.-M.; Bauvineau, L.; Mesure, S. Influence of car seat firmness on seat pressure profiles and perceived discomfort during prolonged simulated driving. Appl. Ergon. 2022, 100, 103666. [Google Scholar] [CrossRef]
- Keshner, E.A.; Campbell, D.; Katz, R.T.; Peterson, B.W. Neck muscle activation patterns in humans during isometric head stabilization. Exp. Brain Res. 1989, 75, 335–344. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.Y.; Yuan, H.; Li, X. A novel method for comfort assessment in a supine sleep position using three-dimensional scanning technology. Int. J. Ind. Ergon. 2018, 67, 104–113. [Google Scholar] [CrossRef]
- Caddick, Z.A.; Gregory, K.; Flynn-Evans, E.E. (Eds.) Sleep environment recommendations for future spaceflight vehicles. In Advances in Human Aspects of Transportation; Springer International Publishing: Cham, Switzerland, 2017; pp. 923–933. [Google Scholar] [CrossRef]
- Desouzart, G.; Matos, R.; Melo, F.; Filgueiras, E. Effects of sleeping position on back pain in physically active seniors: A controlled pilot study. Work-J. Prev. Assess. Rehabil. 2016, 53, 235–240. [Google Scholar] [CrossRef]
- Lu, Y.H.; Niu, M.M.; Song, W.F.; Liu, Y.P.; Wang, M. Investigation on the total and local thermal insulation of the bedding system: Effects of filling materials, weights and body postures. Build. Environ. 2021, 204, 108161. [Google Scholar] [CrossRef]
- Cheng, X.G.; Hu, F.; Yang, B.; Wang, F.M.; Olofsson, T. Contactless sleep posture measurements for demand-controlled sleep thermal comfort: A pilot study. Indoor Air 2022, 32, e13175. [Google Scholar] [CrossRef]
- Sprigle, S.; Sonenblum, S. Assessing evidence supporting redistribution of pressure for pressure ulcer prevention: A review. J. Rehabil. Res. Dev. 2011, 48, 203–213. [Google Scholar] [CrossRef] [PubMed]
- Gorecki, C.; Closs, S.J.; Nixon, J.; Briggs, M. Patient-reported pressure ulcer pain: A mixed-methods systematic review. J. Pain Symptom Manag. 2011, 42, 443–459. [Google Scholar] [CrossRef]
- Hong, Y.-S. Smart care beds for elderly patients with impaired mobility. Wirel. Commun. Mob. Comput. 2018, 2018, 1780904. [Google Scholar] [CrossRef]
- Menon, A.; Kumar, M. Influence of body position on severity of obstructive sleep apnea: A systematic review. ISRN Otolaryngol. 2013, 2013, 670381. [Google Scholar] [CrossRef]
- Alonge, E.O.; Guo, C.F.; Wang, Y.X.; Zhang, H.Q. The mysterious role of epidural fat tissue in spine surgery: A comprehensive descriptive literature review. Clin. Spine Surg. 2023, 36, 1–7. [Google Scholar] [CrossRef]
- Özkal, Ö.; Kara, M.; Topuz, S.; Kaymak, B.; Baki, A.; Özçakar, L. Assessment of core and lower limb muscles for static/dynamic balance in the older people: An ultrasonographic study. Age Ageing 2019, 48, 881–887. [Google Scholar] [CrossRef] [PubMed]
- Vink, P.; Lips, D. Sensitivity of the human back and buttocks: The missing link in comfort seat design. Appl. Ergon. 2017, 58, 287–292. [Google Scholar] [CrossRef]
- De Carvalho, D.; Randhawa, K.; Verville, L.; Hogg-Johnson, S.; Howarth, S.J.; Liang, C.R.; Mior, S.; Côté, P. The vehicle seating intervention trial: Cross-over randomized controlled trial to evaluate the impact of 2 car seat configurations on spinal posture. J. Appl. Biomech. 2023, 40, 40–49. [Google Scholar] [CrossRef]
- Vink, P.; Hallbeck, S. Comfort and discomfort studies demonstrate the need for a new model. Appl. Ergon. 2012, 43, 271–276. [Google Scholar] [CrossRef] [PubMed]


| Typical Conditions | Angles (1 & 2, 2 & 3) | Schemas | Typical Conditions | Angles (1 & 2, 2 & 3) | Schemas |
|---|---|---|---|---|---|
| A0 | 0°, 0° |  | B2 | 60°, 40° |  |
| A1 | 20°, 0° |  | C1 | 40°, 40° |  |
| A2 | 40°, 0° |  | C2 | 20°, 40° |  |
| A3 | 60°, 0° |  | C3 | 0°, 40° |  |
| B1 | 60°, 20° |  | D1 | 0°, 20° |  |
| Variable | Category | Mean or Frequency | Standard Deviation or Percentage (%) |
|---|---|---|---|
| Sex | Male | 256 | 64.0 |
| Female | 144 | 36.0 | |
| Age (years) | 28.28 | 3.41 | |
| Weight (kg) | 65.10 | 16.50 | |
| Height (cm) | 169.36 | 9.13 | |
| BMI (kg/m2) | 22.39 | 3.95 |
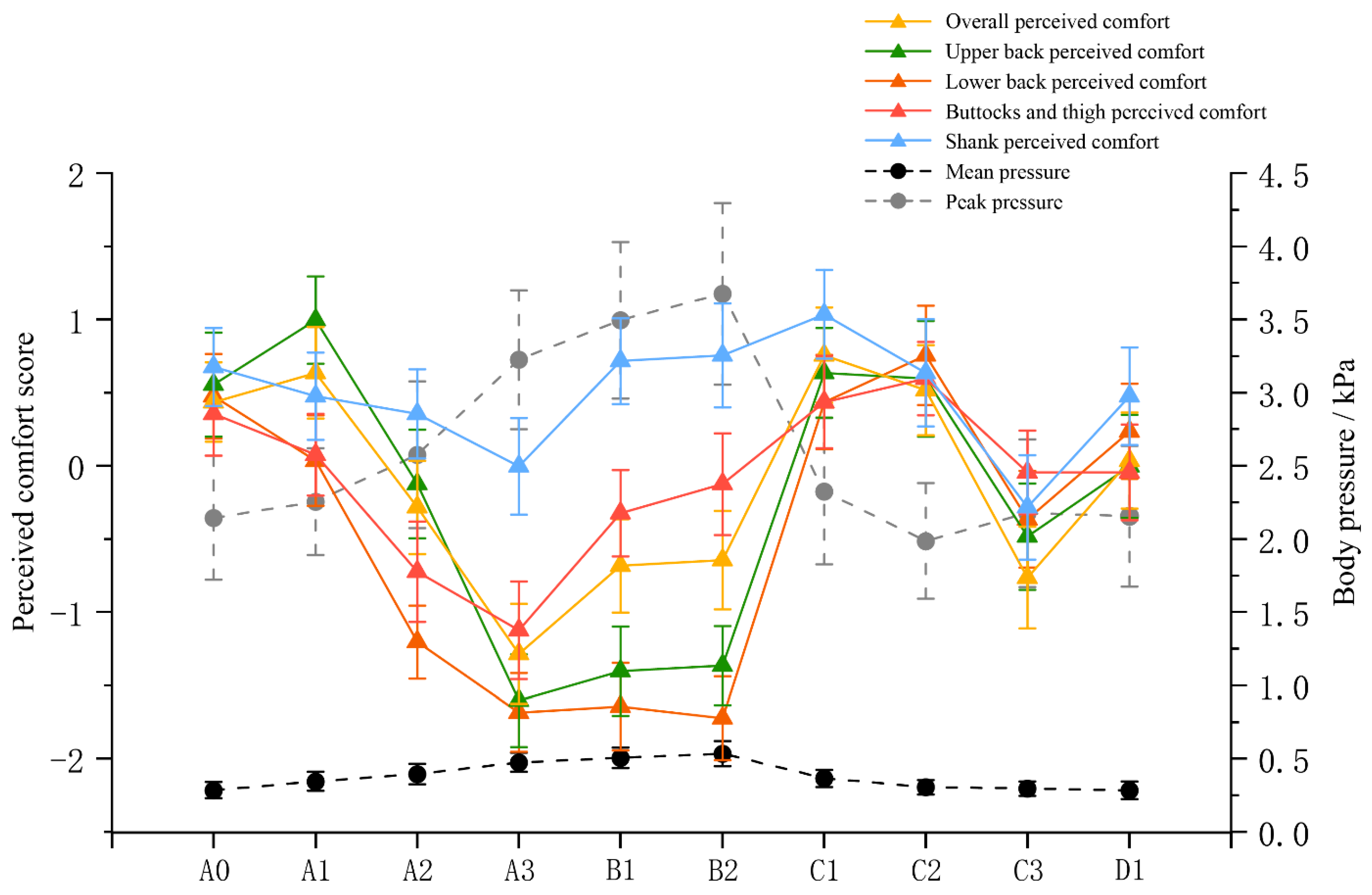
| A0 | A1 | A2 | A3 | B1 | B2 | C1 | C2 | C3 | D1 | F * | p Value | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall perceived comfort | 0.44 (1.08) | 0.64 (1.25) | −0.28 (1.28) | −1.28 (1.37) | −0.68 (1.28) | −0.64 (1.35) | 0.76 (1.30) | 0.52 (1.23) | −0.76 (1.39) | 0.04 (1.31) | 7.489 | <0.000 |
| Upper back perceived comfort | 0.56 (1.42) | 1.00 (1.19) | −0.12 (1.48) | −1.60 (1.26) | −1.40 (1.22) | −1.36 (1.08) | 0.64 (1.22) | 0.60 (1.58) | −0.48 (1.45) | 0.00 (1.41) | 12.745 | <0.000 |
| Lower back perceived comfort | 0.48 (1.16) | 0.04 (1.24) | −1.20 (1.00) | −1.68 (1.07) | −1.64 (1.19) | −1.72 (1.14) | 0.44 (1.29) | 0.76 (1.36) | −0.36 (1.32) | 0.24 (1.30) | 16.924 | <0.000 |
| Buttocks and thigh perceived comfort | 0.36 (1.15) | 0.08 (1.12) | −0.72 (1.37) | −1.12 (1.33) | −0.32 (1.18) | −0.12 (1.39) | 0.44 (1.26) | 0.60 (1.00) | −0.04 (1.14) | −0.04 (1.31) | 4.595 | <0.000 |
| Shank perceived comfort | 0.68 (1.07) | 0.48 (1.19) | 0.36 (1.22) | 0.00 (1.32) | 0.72 (1.17) | 0.76 (1.42) | 1.04 (1.21) | 0.64 (1.47) | −0.28 (1.43) | 0.48 (1.33) | 2.234 | 0.021 |
| Mean pressure (kPa) | 0.29 (0.11) | 0.35 (0.13) | 0.40 (0.14) | 0.48 (0.13) | 0.51 (0.14) | 0.54 (0.17) | 0.37 (0.12) | 0.31 (0.10) | 0.30 (0.10) | 0.29 (0.12) | 13.848 | <0.000 |
| Peak pressure (kPa) | 2.15 (0.85) | 2.26 (0.73) | 2.58 (1.00) | 3.23 (0.95) | 3.50 (1.07) | 3.68 (1.24) | 2.33 (1.00) | 1.99 (0.79) | 2.18 (1.01) | 2.16 (0.96) | 10.329 | <0.000 |
| Overall Perceived Comfort | Upper Back Perceived Comfort | Lower Back Perceived Comfort | Buttocks and Thigh Perceived Comfort | Shank Perceived Comfort | Mean Pressure | Peak Pressure | |
|---|---|---|---|---|---|---|---|
| Overall perceived comfort | 1 | ||||||
| Upper back perceived comfort | 0.759 ** | 1 | |||||
| Lower back perceived comfort | 0.645 ** | 0.689 ** | 1 | ||||
| Buttocks and thigh perceived comfort | 0.559 ** | 0.383 ** | 0.456 ** | 1 | |||
| Shank perceived comfort | 0.467 ** | 0.319 ** | 0.218 ** | 0.549 ** | 1 | ||
| Mean pressure | −0.149 * | −0.237 ** | −0.401 ** | −0.133 * | 0.077 | 1 | |
| Peak pressure | −0.133 * | −0.219 ** | −0.356 ** | −0.075 | 0.095 | 0.726 ** | 1 |
| Ratio | Standard Error | Standardized Regression Coefficient | t | p Value | 95% Confidence Interval | |||
|---|---|---|---|---|---|---|---|---|
| Overall perceived comfort 1 | Height | −0.161 | 0.075 | −1.029 | −2.141 | 0.033 | −0.309 | −0.013 |
| Weight | 0.191 | 0.099 | 2.200 | 1.933 | 0.054 | −0.004 | 0.385 | |
| BMI | −0.637 | 0.283 | −1.763 | −2.253 | 0.025 | −1.195 | −0.080 | |
| Condition | ||||||||
| A0 | 1.000 | |||||||
| A1 | 0.190 | 0.367 | 0.040 | 0.518 | 0.605 | −0.533 | 0.913 | |
| A2 | −0.831 | 0.405 | −0.175 | −2.052 | 0.041 | −1.629 | −0.033 | |
| A3 | −1.905 | 0.467 | −0.400 | −4.076 | 0.000 | −2.826 | −0.984 | |
| B1 | −1.264 | 0.462 | −0.266 | −2.737 | 0.007 | −2.173 | −0.354 | |
| B2 | −1.180 | 0.462 | −0.248 | −2.552 | 0.011 | −2.091 | −0.269 | |
| C1 | 0.328 | 0.369 | 0.069 | 0.888 | 0.375 | −0.399 | 1.055 | |
| C2 | 0.108 | 0.362 | 0.023 | 0.300 | 0.765 | −0.604 | 0.821 | |
| C3 | −1.192 | 0.360 | −0.251 | −3.308 | 0.001 | −1.902 | −0.482 | |
| D1 | 0.360 | −0.083 | −1.097 | 0.274 | −1.105 | 0.314 | −0.395 | |
| Upper back perceived comfort 2 | Height | −0.200 | 0.076 | −1.146 | −2.629 | 0.009 | −0.351 | −0.050 |
| Weight | 0.250 | 0.100 | 2.580 | 2.501 | 0.013 | 0.053 | 0.447 | |
| BMI | −0.852 | 0.287 | −2.109 | −2.973 | 0.003 | −1.417 | −0.288 | |
| Contact area | 0.000 | 0.000 | 0.370 | 2.705 | 0.007 | 0.000 | 0.001 | |
| Condition | ||||||||
| A0 | 1.000 | |||||||
| A1 | 0.316 | 0.372 | 0.059 | 0.849 | 0.397 | −0.417 | 1.048 | |
| A2 | −1.110 | 0.410 | −0.209 | −2.705 | 0.007 | −1.918 | −0.302 | |
| A3 | −2.845 | 0.473 | −0.535 | −6.009 | 0.000 | −3.778 | −1.912 | |
| B1 | −2.572 | 0.468 | −0.484 | −5.500 | 0.000 | −3.494 | −1.651 | |
| B2 | −2.474 | 0.468 | −0.465 | −5.280 | 0.000 | −3.397 | −1.551 | |
| C1 | −0.034 | 0.374 | −0.006 | −0.092 | 0.927 | −0.771 | 0.702 | |
| C2 | 0.050 | 0.366 | 0.009 | 0.136 | 0.892 | −0.672 | 0.772 | |
| C3 | −1.048 | 0.365 | −0.197 | −2.870 | 0.004 | −1.767 | −0.328 | |
| D1 | −0.554 | 0.365 | −0.104 | −1.520 | 0.130 | −1.273 | 0.164 | |
| Lower back perceived comfort 3 | Sex | −0.649 | 0.240 | −0.205 | −2.708 | 0.007 | −1.121 | −0.177 |
| Height | −0.197 | 0.070 | −1.181 | −2.800 | 0.006 | −0.335 | −0.058 | |
| Weight | 0.215 | 0.092 | 2.328 | 2.331 | 0.021 | 0.033 | 0.396 | |
| BMI | −0.617 | 0.264 | −1.606 | −2.338 | 0.020 | −1.138 | −0.097 | |
| Condition | ||||||||
| A0 | 1.000 | |||||||
| A1 | −0.323 | 0.343 | −0.064 | −0.942 | 0.347 | −0.997 | 0.352 | |
| A2 | −1.417 | 0.378 | −0.280 | −3.748 | 0.000 | −2.162 | −0.672 | |
| A3 | −1.690 | 0.436 | −0.334 | −3.873 | 0.000 | −2.549 | −0.830 | |
| B1 | −1.593 | 0.431 | −0.315 | −3.697 | 0.000 | −2.442 | −0.744 | |
| B2 | −1.612 | 0.432 | −0.318 | −3.734 | 0.000 | −2.462 | −0.761 | |
| C1 | 0.116 | 0.345 | 0.023 | 0.335 | 0.738 | −0.563 | 0.794 | |
| C2 | 0.301 | 0.338 | 0.059 | 0.892 | 0.373 | −0.364 | 0.966 | |
| C3 | −0.812 | 0.336 | −0.161 | −2.415 | 0.017 | −1.475 | −0.150 | |
| D1 | −0.234 | 0.336 | −0.046 | −0.696 | 0.487 | −0.896 | 0.428 | |
| Buttocks and thigh perceived comfort 4 | Age | −0.062 | 0.027 | −0.163 | −2.309 | 0.022 | −0.115 | −0.009 |
| Height | −0.273 | 0.069 | −1.906 | −3.932 | 0.000 | −0.410 | −0.136 | |
| Weight | 0.343 | 0.091 | 4.332 | 3.776 | 0.000 | 0.164 | 0.522 | |
| BMI | −1.113 | 0.261 | −3.366 | −4.267 | 0.000 | −1.627 | −0.599 | |
| Contact area | 0.004 | 0.001 | 0.602 | 2.768 | 0.006 | 0.001 | 0.006 | |
| Mean pressure | −2.024 | 0.917 | −0.239 | −2.207 | 0.028 | −3.830 | −0.217 | |
| Condition | ||||||||
| A0 | 1.000 | |||||||
| A1 | −0.219 | 0.338 | −0.050 | −0.648 | 0.518 | −0.886 | 0.447 | |
| A2 | −1.056 | 0.373 | −0.243 | −2.828 | 0.005 | −1.792 | −0.320 | |
| A3 | −1.458 | 0.431 | −0.335 | −3.385 | 0.001 | −2.307 | −0.609 | |
| B1 | −0.605 | 0.426 | −0.139 | −1.422 | 0.156 | −1.444 | 0.233 | |
| B2 | −0.339 | 0.426 | −0.078 | −0.794 | 0.428 | −1.179 | 0.501 | |
| C1 | 0.177 | 0.340 | 0.041 | 0.521 | 0.603 | −0.493 | 0.848 | |
| C2 | 0.301 | 0.334 | 0.069 | 0.903 | 0.368 | −0.356 | 0.958 | |
| C3 | −0.375 | 0.332 | −0.086 | −1.128 | 0.260 | −1.030 | 0.280 | |
| D1 | 0.332 | −0.090 | −1.180 | 0.239 | −1.046 | 0.262 | −0.392 | |
| Shank perceived comfort 5 | Age | −0.114 | 0.028 | −0.298 | −4.083 | 0.000 | −0.169 | −0.059 |
| Height | −0.293 | 0.072 | −2.031 | −4.067 | 0.000 | −0.435 | −0.151 | |
| Weight | 0.400 | 0.094 | 5.010 | 4.239 | 0.000 | 0.214 | 0.586 | |
| BMI | −1.267 | 0.271 | −3.804 | −4.681 | 0.000 | −1.801 | −0.734 | |
| Condition | ||||||||
| A0 | 1.000 | |||||||
| A1 | −0.280 | 0.351 | −0.064 | −0.798 | 0.426 | −0.972 | 0.412 | |
| A2 | −0.585 | 0.388 | −0.133 | −1.509 | 0.133 | −1.349 | 0.179 | |
| A3 | −1.113 | 0.447 | −0.254 | −2.488 | 0.014 | −1.994 | −0.232 | |
| B1 | −0.362 | 0.442 | −0.083 | −0.819 | 0.414 | −1.232 | 0.509 | |
| B2 | −0.298 | 0.442 | −0.068 | −0.673 | 0.501 | −1.170 | 0.574 | |
| C1 | 0.281 | 0.353 | 0.064 | 0.795 | 0.427 | −0.415 | 0.977 | |
| C2 | −0.034 | 0.346 | −0.008 | −0.099 | 0.921 | −0.716 | 0.648 | |
| C3 | −0.967 | 0.345 | −0.221 | −2.805 | 0.005 | −1.646 | −0.288 | |
| D1 | −0.198 | 0.345 | −0.045 | −0.574 | 0.567 | −0.877 | 0.481 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bai, X.; Liu, Y.; Dai, Z.; Chen, Y.; Fang, P.; Ma, J. Determinants of Perceived Comfort: Multi-Dimensional Thinking in Smart Bedding Design. Sensors 2024, 24, 4058. https://doi.org/10.3390/s24134058
Bai X, Liu Y, Dai Z, Chen Y, Fang P, Ma J. Determinants of Perceived Comfort: Multi-Dimensional Thinking in Smart Bedding Design. Sensors. 2024; 24(13):4058. https://doi.org/10.3390/s24134058
Chicago/Turabian StyleBai, Xiangtian, Yonghong Liu, Zhe Dai, Yongkang Chen, Pingping Fang, and Jun Ma. 2024. "Determinants of Perceived Comfort: Multi-Dimensional Thinking in Smart Bedding Design" Sensors 24, no. 13: 4058. https://doi.org/10.3390/s24134058
APA StyleBai, X., Liu, Y., Dai, Z., Chen, Y., Fang, P., & Ma, J. (2024). Determinants of Perceived Comfort: Multi-Dimensional Thinking in Smart Bedding Design. Sensors, 24(13), 4058. https://doi.org/10.3390/s24134058





