Recent Innovations in Footwear and the Role of Smart Footwear in Healthcare—A Survey
Abstract
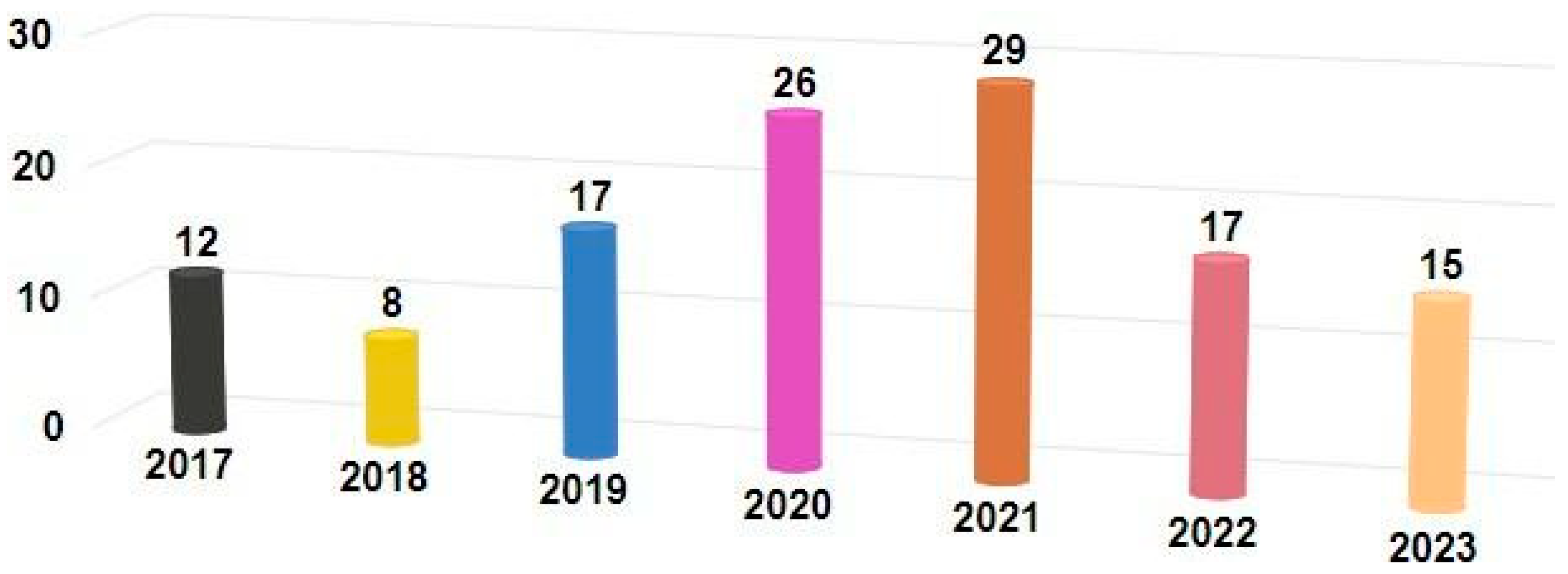
:1. Introduction
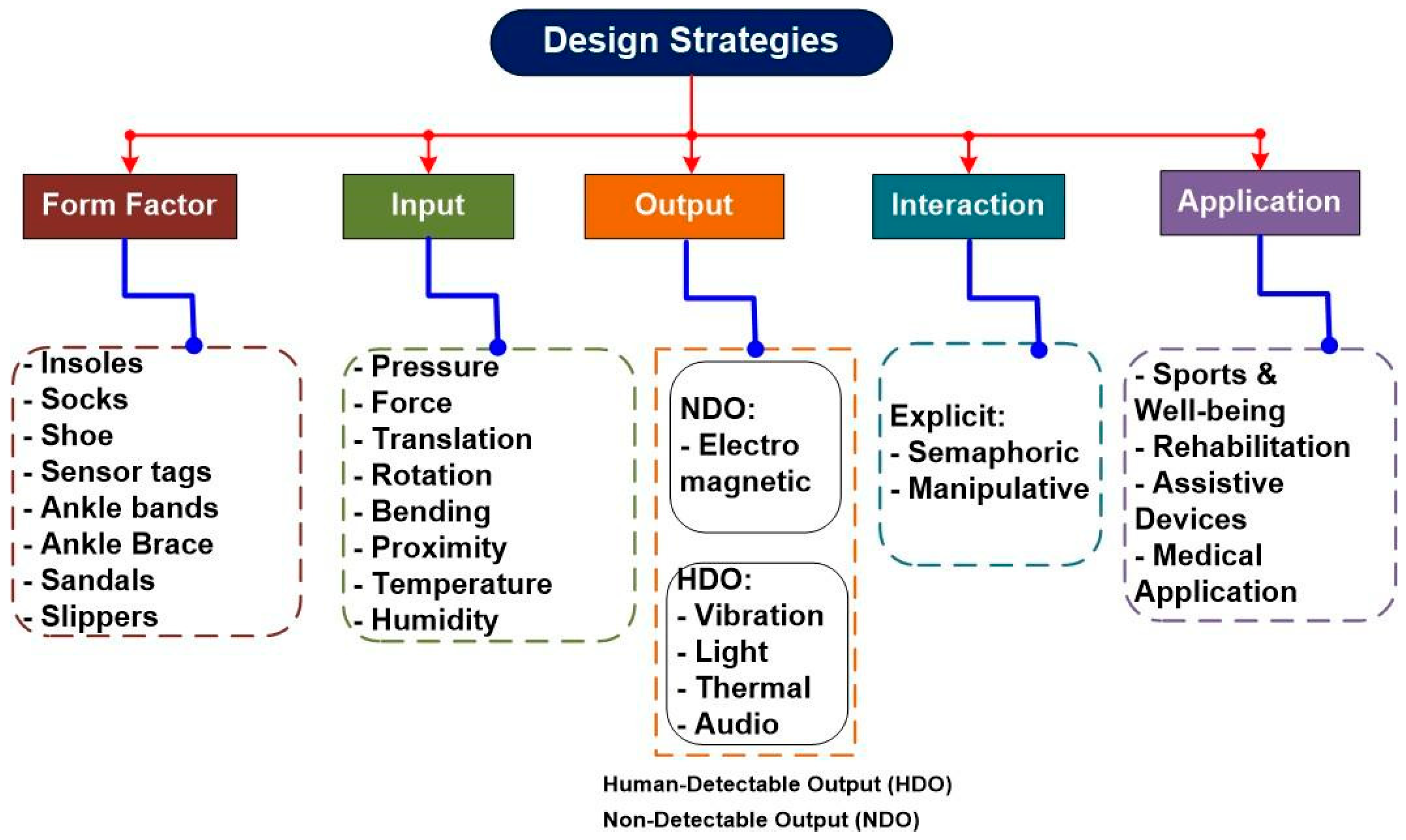
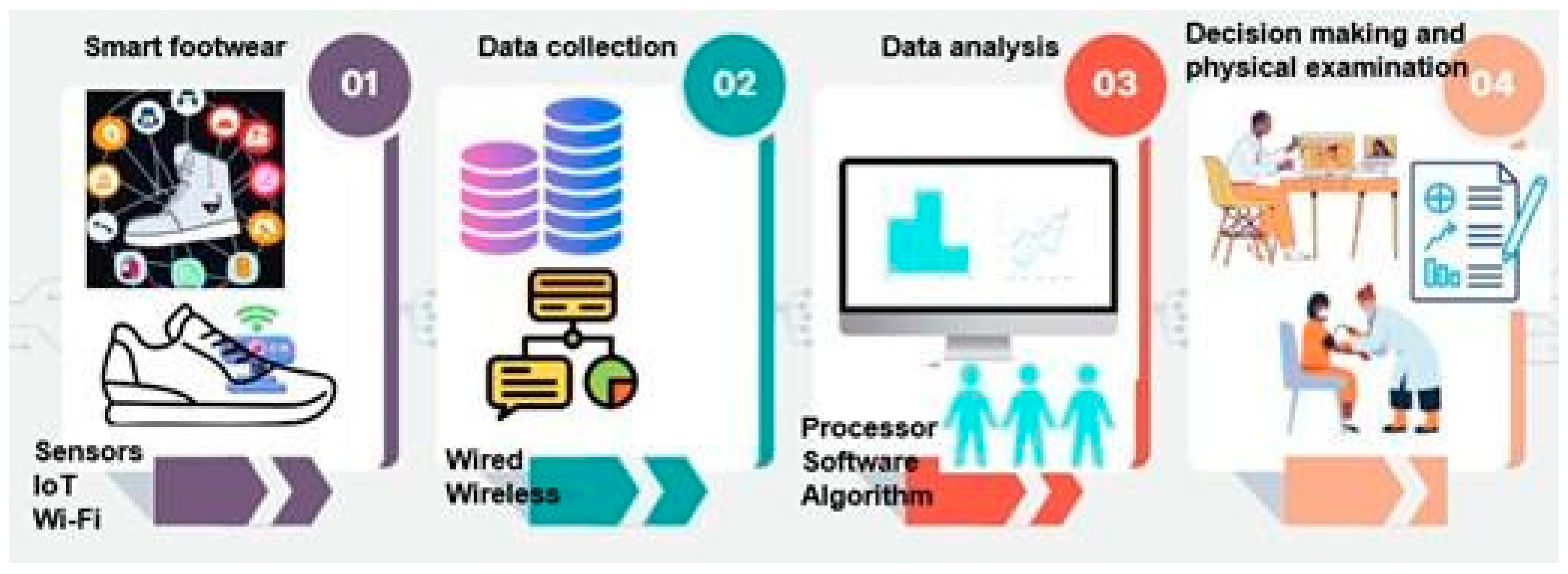
2. Overview of Smart Footwear—Sensors and Design
2.1. SF Sensors and Design
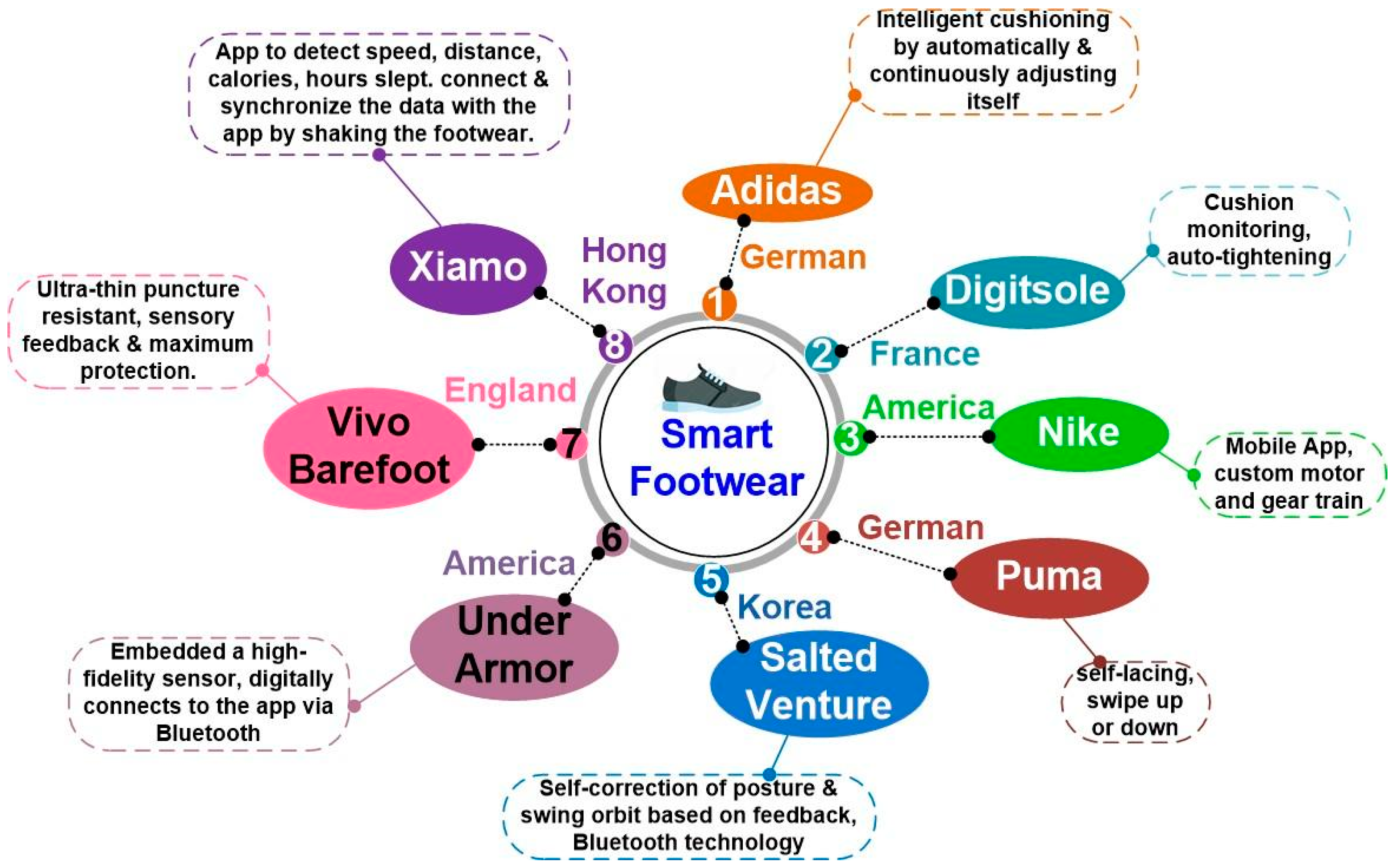
2.2. Various Types of SF Available in the Market
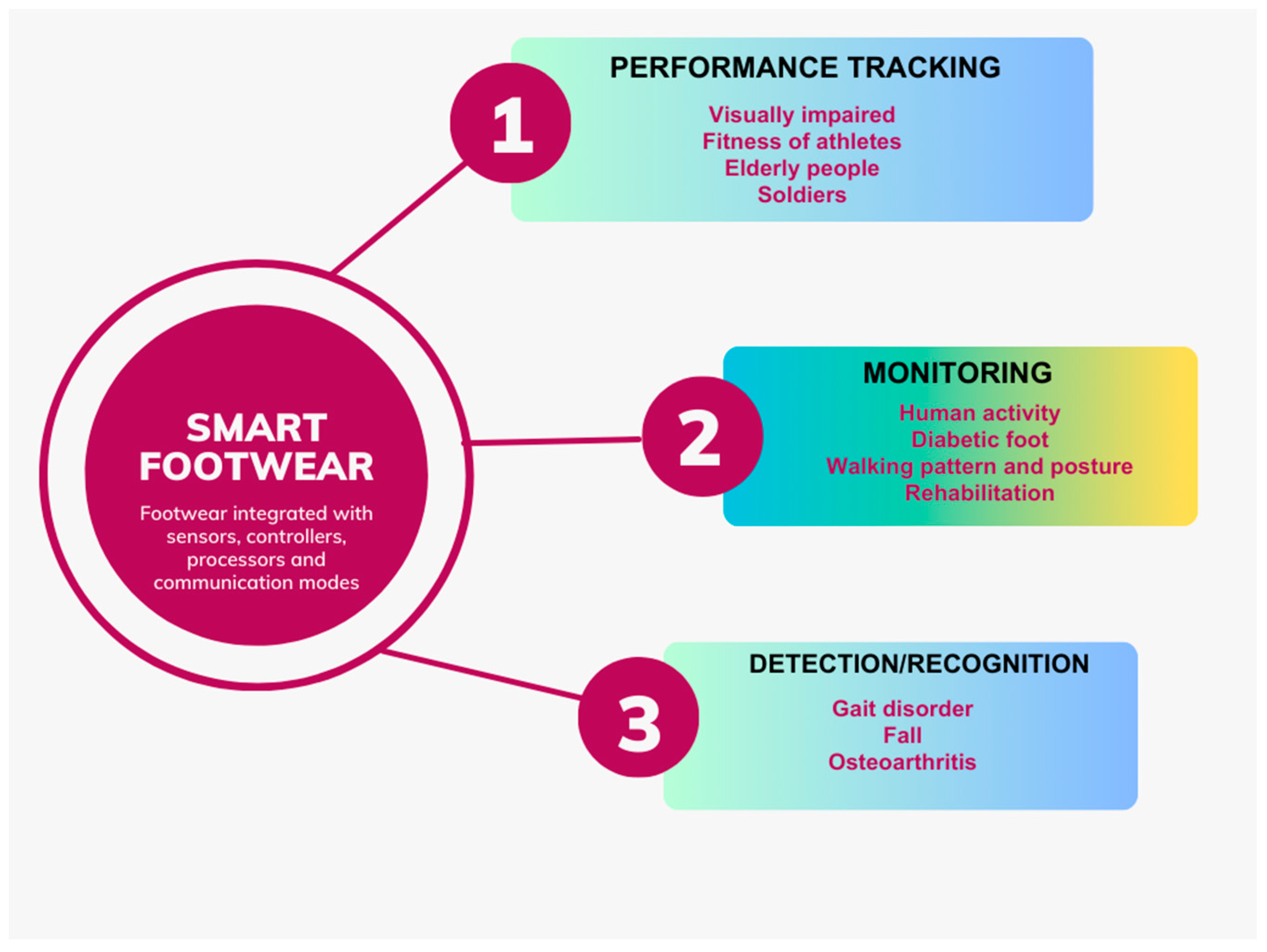
3. Smart Footwear Applications
3.1. Application 1: Performance Tracking
3.2. Application 2: Patient Monitoring
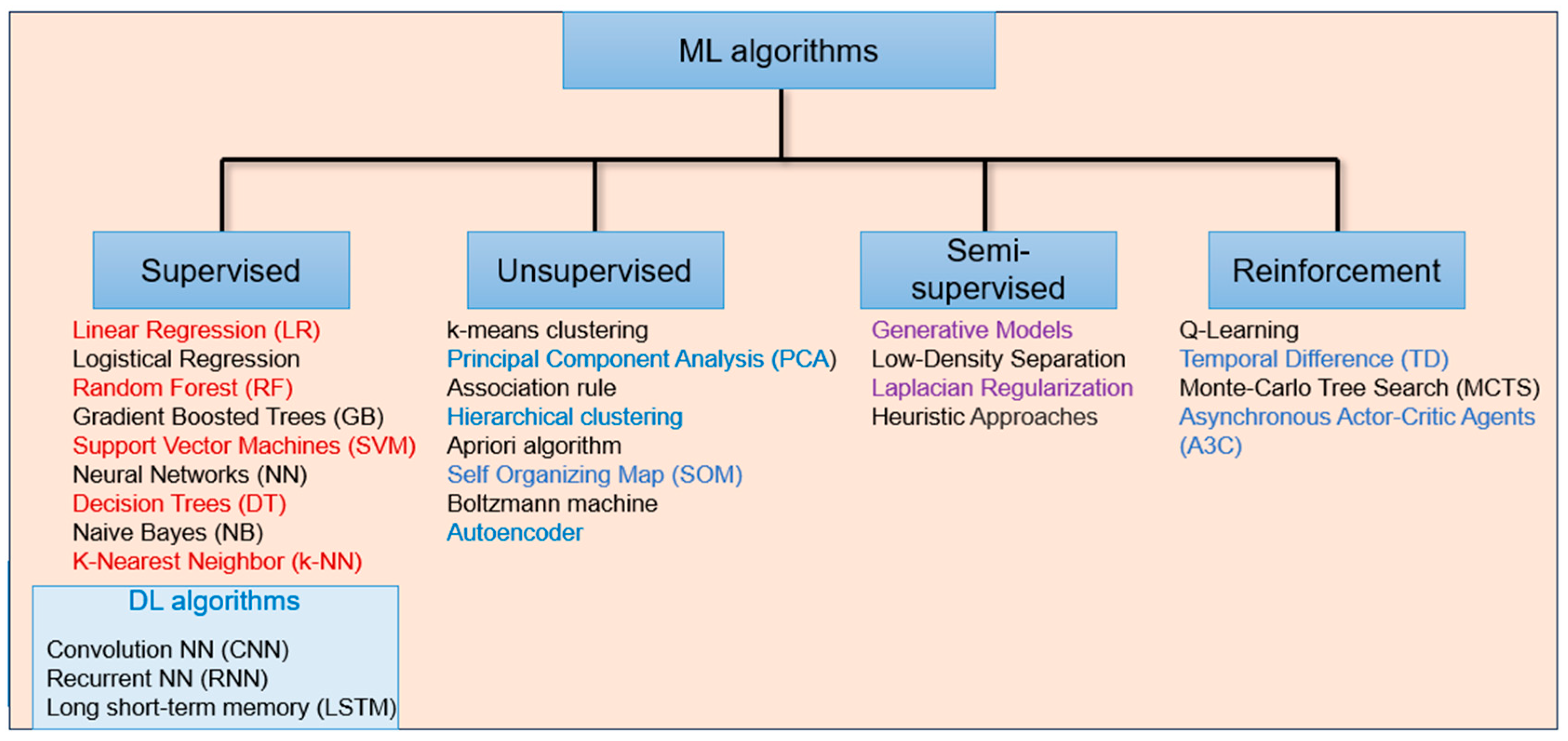
3.3. Application 3: Detection and Recognition (Classification of Disorders)
4. Observations and Future Perspectives
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gokalgandhi, D.; Kamdar, L.; Shah, N.; Mehendale, N. A Review of Smart Technologies Embedded in Shoes. J. Med. Syst. 2020, 44, 150. [Google Scholar] [CrossRef] [PubMed]
- Almuteb, I.; Hua, R.; Wang, Y. Smart insoles review over the last two decade: Applications, potentials, and future. Smart Health 2022, 25, 100301. [Google Scholar] [CrossRef]
- Wikimedia Commons. File. HC SR04 Ultrasonic Sensor 1480319 20. HDR Enhancer.jpg. 2014. Available online: https://commons.wikimedia.org/wiki (accessed on 26 July 2023).
- robokits.co.in. TINY LIDAR Laser Ranging Sensor TOF Based on VL53L0X 2 Meters Range. Available online: https://robokits.co.in/sensors/lidar-laser-rangefinders/tiny-lidar-laser-ranging-sensor-tof-based-on-vl53l0x-2-meters-range (accessed on 26 July 2023).
- Wikimedia Commons. File: MEMS Barometer Capacitive Principal.svg. 2022. Available online: https://commons.wikimedia.org/wiki/File:MEMS_barometer_capacitive_Principal.svg (accessed on 26 July 2023).
- Townsend, K. Comparing Gyroscope Datasheets. Adafruit Learning System. Available online: https://learn.adafruit.com/comparing-gyroscope-datasheets/overview (accessed on 26 July 2023).
- TE Connectivity. RTD Thin Film Element. Available online: https://www.te.com/usa-en/product-CAT-RTD0046.html (accessed on 26 July 2023).
- TE Connectivity. NTC. Thermistors. Available online: https://www.te.com/en/products/sensors/temperature-sensors/ntc-thermistors-sensors/ntc-thermistors.html?tab=pgp-story (accessed on 26 July 2023).
- TE Connectivity. Silicone Rubber Surface Thermocouple Sensor 420M. Available online: https://www.te.com/usa-en/product-CAT-TCS0019.html (accessed on 26 July 2023).
- TE Connectivity. G-TPMO-101: MEAS Thermopile Infrared Sensor. Available online: https://www.te.com/en/product-G-TPMO-101.html (accessed on 26 July 2023).
- TE Connectivity. G-NICO-023: MEAS Digital Temperature Sensors. Available online: https://www.te.com/en/product-G-NICO-023.html (accessed on 26 July 2023).
- moshimoshi-nippon.jp. Check Your Foot Odor with This New App and Pair of ‘SENSING SHOES’. Available online: https://www.moshimoshi-nippon.jp/75518 (accessed on 26 July 2023).
- Smart Shoe Market. Available online: https://www.futuremarketinsights.com/reports/smart-shoe-market (accessed on 17 May 2023).
- Jordi Carrabina. Available online: https://cdn.bdigital.org/PDF/XPABCN16/_/PPT_XPatientBcnCongress_JordiCarrabina.pdf (accessed on 10 June 2023).
- Prashant, G.; Amol, D.; Rameshwari, D.; Komal, G.; Shital, M.A. Smart Footwear System for Healthcare and Fitness Application—A Review. J. Eng. Appl. Sci. 2020, 5, 10–14. [Google Scholar]
- World Health Organization. World Sight Day: Achieve Access for All to Quality, Inclusive and Affordable Eye Care. Available online: https://www.who.int/southeastasia/news/detail/13-10-2022-world-sight-day-achieve-access-for-all-to-quality--inclusive-and-affordable-eye-care (accessed on 26 July 2023).
- Chava, T.; Srinivas, A.T.; Sai, A.L.; Rachapudi, V. IoT Based Smart Shoe for the Blind. In Proceedings of the 6th International Conference on Inventive Computation Technologies (ICICT), Coimbatore, India, 20–22 January 2021; pp. 220–223. [Google Scholar] [CrossRef]
- Nathan, S.S.; Ying, K.J.; Wen, L.H.; Weoi, L.X. Design of Smart Walking Shoe for Visually Impaired People. J. Adv. Res. Appl. Mech. 2023, 101, 53–61. [Google Scholar] [CrossRef]
- Mandal, S.; Chandran, A.B. Low-Cost Ultrasonic-Based Shoe for Visually Impaired People. In Smart Healthcare for Disease Diagnosis and Prevention; Academic Press: Cambridge, MA, USA, 2020; pp. 103–114. ISBN 9780128179130. [Google Scholar] [CrossRef]
- Khan, Z.; Varvade, R.; Fiaidhi, J. Smart Shoes for Visually Impaired. TechRxiv 2020. [Google Scholar]
- Kamaruddin, F.S.; Mahmood, N.H.; Razak, M.A.A.; Zakaria, N.A. Smart Assistive Shoes with Internet of Things Implementation for Visually Impaired People. J. Phys. Conf. Ser. 2021, 2107, 012030. [Google Scholar] [CrossRef]
- Thanuja, C.S.; Sahana, M.H.; Sindhu, G.; Shruti, B.P. Design of Smart Shoe for the Blind with Cordless Load. Int. J. Eng. Res. Technol. (IJERT) 2022, 10, 12. [Google Scholar]
- Sunitharam, C.; Baskar, B.M.; Vishnu, J. Smart Shoe for Visually Impaired People. Int. J. Adv. Eng. Manag. (IJAEM) 2023, 5, 29–33. [Google Scholar]
- Jabakumar, A.K.; Loganathan, D.; Gayathri, T.; Dhivya, K.; Saranraj, J.; Arun, T. Medical Electronics Based Smart Shoe for Blind People. J. Pharm. Negat. Results 2023, 14, 1911–1917. [Google Scholar] [CrossRef]
- Hersh, M. Wearable Travel Aids for Blind and Partially Sighted People: A Review with a Focus on Design Issues. Sensors 2022, 22, 5454. [Google Scholar] [CrossRef]
- Daou, R.A.Z.; Chehade, J.; Haydar, G.A.; Hayek, A.; Boercsoek, J.; Olmedo, J.J.S. Design and Implementation of Smart Shoes for Blind and Visually Impaired People for More Secure Movements. In Proceedings of the 32nd International Conference on Microelectronics (ICM), Aqaba, Jordan, 14–17 December 2020; pp. 1–6. [Google Scholar] [CrossRef]
- Darney, P.E.; Muthu, A.E.; Jeyakumar, K.; Krishnan, R.S.; Narayanan, K.L.; Robinson, Y.H. IoT Based Smart Shoes for Blind People. In Proceedings of the 3rd International Conference on Electronics and Sustainable Communication Systems (ICESC), Coimbatore, India, 17–19 August 2022; pp. 524–529. [Google Scholar] [CrossRef]
- Knopp, M.; Muñiz-Pardos, B.; Wackerhage, H.; Schönfelder, M.; Guppy, F.; Pitsiladis, Y.; Ruiz, D. Variability in Running Economy of Kenyan World-Class and European Amateur Male Runners with Advanced Footwear Running Technology: Experimental and Meta-analysis Results. Sports Med. 2023, 53, 1255–1271. [Google Scholar] [CrossRef] [PubMed]
- Gulas, S.B.; Imre, H.M. The Use of High-Performance Textile Surfaces in Sport Shoe Designs. J. Fash. Technol. Text. Eng. 2020, 8, 4. [Google Scholar]
- Drăgulinescu, A.; Drăgulinescu, A.-M.; Zincă, G.; Bucur, D.; Feieș, V.; Neagu, D.-M. Smart Socks and in-Shoe Systems: State-of-the-Art for Two Popular Technologies for Foot Motion Analysis, Sports, and Medical Applications. Sensors 2020, 20, 4316. [Google Scholar] [CrossRef]
- Lianzhen, C.; Hua, Z. Athlete Rehabilitation Evaluation System Based on Internet of Health Things and Human Gaint Analysis Algorithm. Complexity 2021, 2021, 6663224. [Google Scholar] [CrossRef]
- Xia, Y.; Gu, H.; Xu, L.; Chen, X.D.; Kirk, T.V. Extending Porous Silicone Capacitive Pressure Sensor Applications into Athletic and Physiological Monitoring. Sensors 2021, 21, 1119. [Google Scholar] [CrossRef] [PubMed]
- Barratt, G.K.; Bellenger, C.; Robertson, E.Y.; Lane, J.; Crowther, R.G. Validation of Plantar Pressure and Reaction Force Measured by Motion Pressure Sensor Insoles on a Concept 2 Rowing Ergometer. Sensors 2021, 21, 2418. [Google Scholar] [CrossRef]
- Beckham, J. The Shoe of Tomorrow Knows How Hard You Hustle. CULTURE, 3 April 2012. Available online: https://www.wired.com/2012/04/smart-sneakers/ (accessed on 10 June 2023).
- Guptha, N. Available online: https://www.timesnownews.com/explainer/world-population-day-2022-theme-history-22-of-world-population-will-be-over-65-years-by-2050-check-details-article-92795194 (accessed on 8 June 2023).
- Li, J. Functional Footwear Design for Preventing Falls in the Elderly: A Systematic Research Based on Fault Tree Analysis. Leather Footwear J. 2021, 21, 217–228. [Google Scholar] [CrossRef]
- Schiltz, R. Smart Tracking Device for Alzheimer’s, Senior Safety Advice. Available online: https://seniorsafetyadvice.com/what-are-gps-shoes/ (accessed on 10 June 2023).
- Cheng, W.K.; Lam, H.L.; Lin, F.; Ge, M. A Customizable Smart Shoe with Location Tracking Function for the Elderly. Mater. Today Proc. 2019, 16, 1423–1430. [Google Scholar] [CrossRef]
- Piau, A.; Steinmeyer, Z.; Charlon, Y.; Courbet, L.; Rialle, V.; Lepage, B.; Campo, E.; Nourhashemi, F. A Smart Shoe Insole to Monitor Frail Older Adults’ Walking Speed: Results of Two Evaluation Phases Completed in a Living Lab and Through a 12-Week Pilot Study. JMIR mHealth uHealth 2021, 9, e15641. [Google Scholar] [CrossRef]
- Callari, T.C.; Moody, L.; Magee, P.; Yang, D. ‘Smart—Not only intelligent’ Co-creating Priorities and Design Direction for ‘Smart’ Footwear to Support Independent Ageing. Int. J. Fash. Des. Technol. Educ. 2019, 12, 313–324. [Google Scholar] [CrossRef]
- Aznar-Gimeno, R.; Labata-Lezaun, G.; Adell-Lamora, A.; Abadía-Gallego, D.; Del-Hoyo-Alonso, R.; González-Muñoz, C. Deep Learning for Walking Behaviour Detection in Elderly People Using Smart Footwear. Entropy 2021, 23, 777. [Google Scholar] [CrossRef]
- Callari, T.C.; Moody, L.; Magee, P.; Yang, D.; Ozkan, G.; Martinez, D. Combining Design Innovation and Material Science to Support Independent Ageing. Des. J. 2019, 22, 2161–2162. [Google Scholar] [CrossRef]
- Nageswari, C.S.; Kumar, M.N.V.; Gayathri, C.R.; Florence, D.; Harshitha, U. Smart Wearable Shoe for Tracking and Monitoring Army Soldiers. Ann. Rom. Soc. Cell Biol. 2021, 25, 17774–17782. Available online: http://annalsofrscb.ro/index.php/journal/article/view/7890 (accessed on 12 June 2023).
- Jessica Pauline, S.; Bharkavi, A.G.; Jesgna, A.; Maheswari, S. Smart Shoe for Tracking and Monitoring of Army Soldiers. In Smart Intelligent Computing and Communication Technology; IOS Press: Amsterdam, The Netherlands, 2021. [Google Scholar] [CrossRef]
- Friedl, K.E. Military Applications of Soldier Physiological Monitoring. J. Sci. Med. Sport 2018, 21, 1147–1153. [Google Scholar] [CrossRef] [PubMed]
- Muthusamy, S.; Pandiyan, S.; Paramasivam, M. A Novel GPS Based Soldier Health Monitoring and Position Tracking System. Res. Sq. 2022. [CrossRef]
- Truong, P.H.; You, S.; Ji, S.-H.; Jeong, G.-M. Wearable System for Daily Activity Recognition Using Inertial and Pressure Sensors of a Smart Band and Smart Shoes. Int. J. Comput. Commun. Control 2019, 14, 726–742. [Google Scholar] [CrossRef]
- D’arco, L.; Wang, H.; Zheng, H. Assessing Impact of Sensors and Feature Selection in Smart-Insole-Based Human Activity Recognition. Methods Protoc. 2022, 5, 45. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Choffin, Z.; Jeong, N.; Callihan, M.; Sazonov, E.; Jeong, S. Lower body joint angle prediction using machine learning and applied biomechanical inverse dynamics. Sensors 2022, 23, 228. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ren, D.; Aubert-Kato, N.; Anzai, E.; Ohta, Y.; Tripette, J. Random Forest algorithms for recognizing daily life activities using plantar pressure information: A smart-shoe study. PeerJ 2020, 8, e10170. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bevilacqua, A.; MacDonald, K.; Rangarej, A.; Widjaya, V.; Caulfield, B.; Kechadi, T. Human Activity Recognition with Convolutional Neural Networks. In Lecture Notes in Computer Science, Proceedings of the Joint European Conference on Machine Learning and Knowledge Discovery in Databases, Dublin, Ireland, 10–14 September 2018; Springer: Cham, Switzerland, 2018; Volume 11053. [Google Scholar]
- Fridriksdottir, E.; Bonomi, A.G. Accelerometer-based human activity recognition for patient monitoring using a deep neural network. Sensors 2020, 20, 6424. [Google Scholar] [CrossRef]
- Kakarla, T.P.; Varma, K.A.; Preejith, S.P.; Joseph, J.; Sivaprakasam, M. Accuracy enhancement of total force by capacitive insoles. In Proceedings of the 2019 IEEE International Symposium on Medical Measurements and Applications (MeMeA), Istanbul, Turkey, 26–28 June 2019; pp. 1–6. [Google Scholar]
- Sorrentino, I.; Chavez, F.J.A.; Latella, C.; Fiorio, L.; Traversaro, S.; Rapetti, L.; Tirupachuri, Y.; Guedelha, N.; Maggiali, M.; Dussoni, S.; et al. A novel sensorised insole for sensing feet pressure distributions. Sensors 2020, 20, 747. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Chai, R.; Wang, H.; Ye, X. A plantar pressure sensing system with balancing sensitivity based on tailored MWC NTs/Pdms composites. Micromachines 2018, 9, 466. [Google Scholar] [CrossRef] [PubMed]
- Pham, C.; Diep, N.N.; Phuong, T.M. e-Shoes: Smart Shoes for Unobtrusive Human Activity Recognition. In Proceedings of the 2017 9th International Conference on Knowledge and Systems Engineering (KSE), Hue, Vietnam, 19–21 October 2017; pp. 1–6. [Google Scholar]
- Jeong, B.O.; Jeong, S.J.; Park, K.; Kim, B.-H.; Yim, S.-V.; Kim, S. Effects of three-dimensional image-based insole for healthy volunteers: A pilot clinical trial. Transl. Clin. Pharmacol. 2023, 31, 49–58. [Google Scholar] [CrossRef] [PubMed]
- Dogan, G.; Ertas, S.S.; Cay, I. Human Activity Recognition Using Convolutional Neural Networks. In Proceedings of the 2021 IEEE Conference on Computational Intelligence in Bioinformatics and Computational Biology (CIBCB), Melbourne, Australia, 13–15 October 2021; pp. 1–5. [Google Scholar] [CrossRef]
- World Health Organization. Diabetes. 2021. Available online: https://www.who.int/health-topics/diabetes#tab=tab_1 (accessed on 10 June 2023).
- Chen, L.; Sun, S.; Gao, Y.; Ran, X. Global mortality of diabetic foot ulcer: A systematic review and meta-analysis of observational studies. Diabetes Obes. Metab. 2023, 25, 36–45. [Google Scholar] [CrossRef] [PubMed]
- Preventing Diabetic Foot Ulcers: A 4-Pronged Approach. 2022. Available online: https://www.consultant360.com/articles/preventing-diabetic-foot-ulcers-4-pronged-approach (accessed on 16 June 2023).
- Moulaei, K.; Malek, M.; Sheikhtaheri, A. A smart wearable device for monitoring and self-management of diabetic foot: A proof-of-concept study. Int. J. Med. Inform. 2020, 146, 104343. [Google Scholar] [CrossRef] [PubMed]
- Altaf, M.; Al-Qahtani, M.; Al-Tayyar, S.; Al-Hammal, M.; Al-Amri, M.; Javed, R. Monitoring Diabetic Foot by Designing a New Smart Sole. SSRG Int. J. Pharm. Biomed. Eng. 2020, 7, 15–20. [Google Scholar]
- Sousa, L.B.; Almeida, I.; Bernardes, R.A.; Leite, T.R.; Negrão, R.; Apóstolo, J.; Salgueiro-Oliveira, A.; Parreira, P. A three step protocol for the development of an innovative footwear (shoe and sensor-based insole) to prevent diabetic foot ulceration. Front. Public Health 2023, 11, 1061383. [Google Scholar] [CrossRef] [PubMed]
- Kularathne, N.; Wijayathilaka, U.; Kottawaththa, N.; Hewakoralage, S.; Thelijjagoda, S. Dia-Shoe: A Smart Diabetic Shoe to Monitor and Prevent Diabetic Foot Ulcers. In Proceedings of the 2019 International Conference on Advancements in Computing (ICAC), Malabe, Sri Lanka, 5–7 December 2019; pp. 410–415. [Google Scholar] [CrossRef]
- Sudha, G.; Saranya, S.; Subbiah, S.; Vishnupriya, B.; Kalyani, V.S.; Isaiyarasi, P. Smart Footwear for Patients with Diabetic Neuropathy. Indian J. Nat. Sci. 2022, 13, 39669–39675. [Google Scholar]
- Abbott, C.A.; Chatwin, K.E.; Foden, P.; Hasan, A.N.; Sange, C.; Rajbhandari, S.M.; Reddy, P.N.; Vileikyte, L.; Bowling, F.L.; Boulton, A.J.M.; et al. Innovative intelligent insole system reduces diabetic foot ulcer recurrence at plantar sites: A prospective, randomized, proof-of-concept study. Lancet Digit. Health 2019, 1, e308–e318. [Google Scholar] [CrossRef]
- Aqueveque, P.; Osorio, R.; Pastene, F.; Saavedra, F.; Pino, E. Capacitive sensors array for plantar pressure measurement insole fabricated with flexible PCB. In Proceedings of the 40th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Honolulu, HI, USA, 18–21 July 2018; pp. 4393–4396. [Google Scholar]
- Ahmed, S.; Butterworth, P.; Barwick, A.; Sharma, A.; Hasan, Z.; Nancarrow, S. Footwear and insole design parameters to prevent occurrence and recurrence of neuropathic plantar forefoot ulcers in patients with diabetes: A series of N-of-1 trial study protocol. Trials 2022, 23, 1017. [Google Scholar] [CrossRef]
- Collings, R.; Freeman, J.; Latour, J.M.; Hosking, J.; Paton, J. Insoles to ease plantar pressure in people with diabetes and peripheral neuropathy: A feasibility randomized controlled trial with an embedded qualitative study. Pilot Feasibility Study 2023, 9, 20. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Saenz, S.D.; Franco-Perez, S.S.; Espinoza-Valdez, E.; Salido-Ruiz, R.A.; Curiel-Lopez, F.B. Instrumented footwear for diabetic foot monitoring: Foot sole temperature measurement. In Proceedings of the Latin American Conference on Biomedical Engineering, Cancun, Mexico, 2–5 October 2019; Springer: Cham, Switzerland, 2019; pp. 501–507. [Google Scholar]
- Collings, R.; Freeman, J.; Latour, J.M.; Paton, J. Footwear and insole design features for offloading the diabetic at-risk foot—A systematic review and meta-analyses. Endocrinol. Diabetes Metab. 2020, 11, 4. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.-Y.; Liu, Q.-L.; Yick, K.-L.; Yip, J.; Ng, S.-P. Analysis of Diabetic Foot Deformation and Plantar Pressure Distribution of Women at Different Walking Speeds. Int. J. Environ. Res. Public Health 2023, 20, 3688. [Google Scholar] [CrossRef] [PubMed]
- Ning, K.; Yick, K.-L.; Yu, A.; Yip, J. Effects of Textile-Fabricated Insole on Foot Skin Temperature and Humidity for Enhancing Footwear Thermal Comfort. Appl. Ergon. 2022, 104, 103803. [Google Scholar] [CrossRef] [PubMed]
- Shi, Q.-Q.; Li, P.-L.; Yick, K.-L.; Jiao, J.; Liu, Q.-L. Influence of Contoured Insoles with Different Materials on Kinematics and Kinetics Changes in Diabetic Elderly During Gait. Int. J. Environ. Res. Public Health 2022, 19, 12502. [Google Scholar] [CrossRef] [PubMed]
- Orlando, G.; Prior, Y.; Reeves, N.D.; Vileikyte, L. Patient and Provider Perspective of Smart Wearable Technology in Diabetic Foot Ulcer Prevention: A Systematic Review. Medicina 2021, 57, 1359. [Google Scholar] [CrossRef] [PubMed]
- Macdonald, E.M.; Perrin, B.M.; Hyett, N.; Kingsley, M.I.C. Factors Influencing Behavioural Intention to Use a Smart Shoe Insole in Regionally Based Adults with Diabetes: A Mixed Methods Study. J. Foot Ankle Res. 2019, 12, 29. [Google Scholar] [CrossRef] [PubMed]
- D’amico, M.; Kinel, E.; Roncoletta, P.; Gnaldi, A.; Ceppitelli, C.; Belli, F.; Murdolo, G.; Vermigli, C. Data-Driven CAD-CAM vs Traditional Total Contact Custom Insoles: A NovelQuantitative-Statistical Framework for the Evaluation of Insoles Offloading Performance in Diabetic Foot. PLoS ONE 2021, 16, e0247915. [Google Scholar] [CrossRef] [PubMed]
- Eskofier, B.M.; Lee, S.I.; Baron, M.; Simon, A.; Martindale, C.F.; Gaßner, H.; Klucken, J. An Overview of Smart Shoes in the Internet of Health Things: Gait and Mobility Assessment in Health Promotion and Disease Monitoring. Appl. Sci. 2017, 7, 986. [Google Scholar] [CrossRef]
- Pirker, W.; Katzenschlager, R. Gait Disorders in Adults and the Elderly: A Clinical Guide. Wien. Klin. Wochenschr. 2017, 129, 81–95. [Google Scholar] [CrossRef]
- HMenz, H.B.; Auhl, M.; Munteanu, S.E. Preliminary Evaluation of Prototype Footwear and Insoles to Optimise Balance and Gait in Older People. BMC Geriatr. 2017, 17, 212. [Google Scholar] [CrossRef]
- Chatzaki, C.; Skaramagkas, V.; Tachos, N.; Christodoulakis, G.; Maniadi, E.; Kefalopoulou, Z.; Fotiadis, D.I.; Tsiknakis, M. The Smart-Insole Dataset: Gait Analysis Using Wearable Sensors with a Focus on Elderly and Parkinson’s Patients. Sensors 2021, 21, 2821. [Google Scholar] [CrossRef]
- Alves Ferreira, H.; Ramos, G.C.; de Andrade Barbosa, T.M.G. Smart Shoes to Avoid Falls in the Elderly People. Int. J. Comput. Appl. 2021, 174, 12. [Google Scholar]
- Apoorva, Y.S.; George, S.M. Smart Shoes for Gait and Mobility Assessment. In Proceedings of the 2021 IEEE Mysore Sub Section International Conference (MysuruCon), Hassan, India, 24–25 October 2021; pp. 335–340. [Google Scholar] [CrossRef]
- Seo, M.; Shin, M.J.; Park, T.S.; Park, J.H. Clinometric Gait Analysis Using Smart Insoles in Patients with Hemiplegia After Stroke: Pilot Study. JMIR mHealth uHealth 2020, 8, e22208. [Google Scholar] [CrossRef]
- Mustafaoglu, A.; Aktas, F. IoMT-Based Smart Shoe Design for Healthy Foot-Flat Feet Gait Analysis, European. J. Sci. Technol. 2022, 42, 108–112. [Google Scholar]
- Wang, C.; Kim, Y.; Min, S.D. Soft-Material-Based Smart Insoles for a Gait Monitoring System. Materials 2018, 11, 2435. [Google Scholar] [CrossRef]
- Wu, J.; Kuruvithadam, K.; Schaer, A.; Stoneham, R.; Chatzipirpiridis, G.; Easthope, C.A.; Barry, G.; Martin, J.; Pané, S.; Nelson, B.J.; et al. An Intelligent in-Shoe System for Gait Monitoring and Analysis with Optimized Sampling and Real-Time Visualization Capabilities. Sensors 2021, 21, 2869. [Google Scholar] [CrossRef]
- Teufl, W.; Lorenz, M.; Miezal, M.; Taetz, B.; Fröhlich, M.; Bleser, G. Towards Inertial Sensor Based Mobile Gait Analysis: Event-Detection and Spatio-temporal Parameters. Sensors 2019, 19, 38. [Google Scholar] [CrossRef]
- Zhang, H.; Guo, Y.; Zanotto, D. Accurate Ambulatory Gait Analysis in Walking and Running Using Machine Learning Models. IEEE Trans. Neural Syst. Rehabil. Eng. 2020, 28, 1046. [Google Scholar] [CrossRef]
- Zhang, H.; Zanotto, D.; Agrawal, S.K. Estimating CoP Trajectories and Kinematic Gait Parameters in Walking and Running Using Instrumented Insoles. IEEE Robot Autom. Lett. 2017, 2, 2159–2165. [Google Scholar] [CrossRef]
- Xia, H.; Xu, J.; Wang, J.; Hunt, M.A.; Shull, P.B. Validation of a Smart Shoe for Estimating Foot Progression Angle During Walking Gait. J. Biomech. 2017, 61, 193–198. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.I.; Nam, H.S.; Garst, J.H.; Huang, A.; Campion, A.; Arnell, M.; Ghalehsariand, N.; Park, S.; Chang, H.-J.; Lu, D.C.; et al. Unobtrusive and Continuous Monitoring of Alcohol-Impaired Gait Using Smart Shoes. Methods Inf. Med. 2017, 56, 74–82. [Google Scholar] [CrossRef]
- Wang, H.; Basu, A.; Durandau, G.; Sartori, M. Wearable Real-Time Kinematic and Kinetic Measurement Sensor Setup for Human Locomotion. Wearable Technol. 2023, 4, e11. [Google Scholar] [CrossRef]
- Zhang, Q.; Wang, Y.L.; Xia, Y.; Wu, X.; Kirk, T.V.; Chen, X.D. A Low-Cost and Highly Integrated Sensing Insole for Plantar Pressure Measurement. Sens. Bio-Sens. Res. 2019, 26, 100298. [Google Scholar] [CrossRef]
- Ziagkas, E.; Loukovitis, A.; Zekakos, D.X.; Chau, T.D.-P.; Petrelis, A.; Grouios, G. A Novel Tool for Gait Analysis: Validation Study of the Smart Insole PODOSmart. Sensors 2021, 21, 5972. [Google Scholar] [CrossRef]
- Wang, Y.; Truong, T.E.; Chesebrough, S.W.; Willemsen, P.; Foreman, K.B.; Merryweather, A.S.; Hollerbach, J.M.; Minor, M.A. Augmenting Virtual Reality Terrain Display with Smart Shoe Physical Rendering: A Pilot Study. IEEE Trans. Haptics 2021, 14, 174–187. [Google Scholar] [CrossRef]
- Ho, J.-G.; Kim, Y.; Min, S.-D. Customized Textile Capacitive Insole Sensor for Center of Pressure Analysis. Sensors 2022, 22, 9390. [Google Scholar] [CrossRef]
- Cui, T.; Yang, L.; Han, X.; Xu, J.; Yang, Y.; Ren, T. A Low-Cost, Portable, and Wireless in-Shoe System Based on a Flexible Porous Graphene Pressure Sensor. Materials 2021, 14, 6475. [Google Scholar] [CrossRef]
- Luna-Perejón, F.; Salvador-Domínguez, B.; Perez-Peña, F.; Corral, J.M.R.; Escobar-Linero, E.; Morgado-Estévez, A. Smart Shoe Insole Based on Polydimethylsiloxane Composite Capacitive Sensors. Sensors 2023, 23, 1298. [Google Scholar] [CrossRef]
- Kiaghadi, A.M.; Bahramizadeh, M.; Hadadi, M. Effect of Textured and Prefabricated Insole Use with Medical or Sports Shoes on Dynamic Postural Control in Elderly People. Top. Geriatr. Rehabil. 2020, 36, 55–59. [Google Scholar] [CrossRef]
- Jun, S.P.; You, Y.W.; Park, S.B. The Pre-Study of Development of Smart Shoe with Musculoskeletal Injury Prevention and Monitoring System: Selection of Plantar Pressure Sensor Location and Development of Prototype. J. Ergon. Soc. Korea 2018, 37, 101–110. [Google Scholar] [CrossRef]
- Dai, Y.; Gao, J.; Zhang, W.; Wu, X.; Zhu, X.; Gu, W. Smart Insoles for Gait Analysis Based on Meshless Conductive Rubber Sensors and Neural Networks. J. Phys. 2023, 2500, 012007. [Google Scholar] [CrossRef]
- Burgo, J.M.D.A.D.; Haro, F.B.; D’amato, R.; Méndez, J.A.J. Development of a Smart Splint to Monitor Different Parameters during the Treatment Process. Sensors 2020, 20, 4207. [Google Scholar] [CrossRef] [PubMed]
- Guidozzi, F. Foot problems in older women. Climacteric 2017, 20, 518–521. [Google Scholar] [CrossRef]
- Golledge, J.; Fernando, M.; Lazzarini, P.; Najafi, B.; Armstrong, D.G. The Potential Role of Sensors, Wearables and Telehealth in the Remote Management of Diabetes-Related Foot Disease. Sensors 2020, 20, 4527. [Google Scholar] [CrossRef] [PubMed]
- Rice, H.; Patel, M. Manipulation of Foot Strike and Footwear Increases Achilles Tendon Loading During Running. Am. J. Sports Med. 2017, 45, 2411–2417. [Google Scholar] [CrossRef] [PubMed]
- Biswas, N.; Chakrabarti, S.; Jones, L.D.; Ashili, S. Smart Wearables Addressing Gait Disorders: A Review. Mater. Today Commun. 2023, 35, 106250. [Google Scholar] [CrossRef]
- Jain, R.; Semwal, V.B.; Kaushik, P. Stride Segmentation of Inertial Sensor Data Using Statistical Methods for Different Walking Activities. Robotica 2022, 40, 2567–2580. [Google Scholar] [CrossRef]
- Aqueveque, P.; Germany, E.; Osorio, R.; Pastene, F. Gait Segmentation Method Using a Plantar Pressure Measurement System with Custom-Made Capacitive Sensors. Sensors 2020, 20, 656. [Google Scholar] [CrossRef]
- Sunarya, U.; Hariyani, Y.S.; Cho, T.; Roh, J.; Hyeong, J.; Sohn, I.; Kim, S.; Park, C. Feature Analysis of Smart Shoe Sensors for Classification of Gait Patterns. Sensors 2020, 20, 6253. [Google Scholar] [CrossRef]
- Jeong, K.; Lee, K.-C. Artificial Neural Network-Based Abnormal Gait Pattern Classification Using Smart Shoes with a Gyro Sensor. Electronics 2022, 11, 3614. [Google Scholar] [CrossRef]
- Anderson, W.; Choffin, Z.; Jeong, N.; Callihan, M.; Jeong, S.; Sazonov, E. Empirical Study on Human Movement Classification Using Insole Footwear Sensor System and Machine Learning. Sensors 2022, 22, 2743. [Google Scholar] [CrossRef] [PubMed]
- Luna-Perejón, F.; Domínguez-Morales, M.; Gutiérrez-Galán, D.; Civit-Balcells, A. Low-Power Embedded System for Gait Classification Using Neural Networks. J. Low Power Electron. Appl. 2020, 10, 14. [Google Scholar] [CrossRef]
- Patil, P.; Kumar, K.; Gaud, N.; Semwal, V.B. Clinical Human Gait Classification: Extreme Learning Machine Approach. In Proceedings of the 1st International Conference on Advances in Science, Engineering and Robotics Technology (ICASERT), Dhaka, Bangladesh, 3–5 May 2019; pp. 1–6. [Google Scholar] [CrossRef]
- Dong, T.; Guo, Y.; Gu, Y.; Wang, L.; Liu, T.; Wang, X.; Li, P.; Li, X. Design of a Wireless and Fully Flexible Insole Using a Highly Sensitive Pressure Sensor for Gait Event Detection. Meas. Sci. Technol. 2021, 32, 105109. [Google Scholar] [CrossRef]
- Lee, S.-S.; Choi, S.T.; Choi, S.-I. Classification of Gait Type Based on Deep Learning Using Various Sensors with Smart Insole. Sensors 2019, 19, 1757. [Google Scholar] [CrossRef] [PubMed]
- Shakya, S.; Taparugssanagorn, A.; Silpasuwanchai, C. Convolutional Neural Network-Based Low-Powered Wearable Smart Device for Gait Abnormality Detection. IoT 2023, 4, 57–77. [Google Scholar] [CrossRef]
- Shah, N.; Kamdar, L.; Gokalgandhi, D.; Mehendale, N. Walking Pattern Analysis Using Deep Learning for Energy Harvesting Smart Shoes with IoT. Neural Comput. Appl. 2021, 33, 11617–11625. [Google Scholar] [CrossRef]
- Gao, J.; Gu, P.; Ren, Q.; Zhang, J.; Song, X. Abnormal Gait Recognition Algorithm Based on LSTM-CNN Fusion Network. IEEE Access 2019, 7, 163180–163190. [Google Scholar] [CrossRef]
- Domínguez-Morales, M.J.; Luna-Perejón, F.; Miró-Amarante, L.; Hernández-Velázquez, M.; Sevillano-Ramos, J.L. Smart Footwear Insole for Recognition of Foot Pronation and Supination Using Neural Networks. Appl. Sci. 2019, 9, 3970. [Google Scholar] [CrossRef]
- Moore, S.R.; Kranzinger, C.; Fritz, J.; Stöggl, T.; Kröll, J.; Schwameder, H. Foot Strike Angle Prediction and Pattern Classification Using Loadsoltm Wearable Sensors: A Comparison of Machine Learning Techniques. Sensors 2020, 20, 6737. [Google Scholar] [CrossRef]
- Santos, G.L.; Endo, P.T.; Monteiro, K.H.d.C.; Rocha, E.d.S.; Silva, I.; Lynn, T. Accelerometer-Based Human Fall Detection Using Convolutional Neural Networks. Sensors 2019, 19, 1644. [Google Scholar] [CrossRef]
- Montanini, L.; Del Campo, A.; Perla, D.; Spinsante, S.; Gambi, E. A Footwear-Based Methodology for Fall Detection. IEEE Sens. J. 2018, 18, 1233–1242. [Google Scholar] [CrossRef]
- Zitouni, M.; Pan, Q.; Brulin, D.; Campo, E. Design of a Smart Sole with Advanced Fall Detection Algorithm. J. Sens. Technol. 2019, 9, 71–90. [Google Scholar] [CrossRef]
- Codina, M.; Navarrete, M.; Rezaee, A.; Castells-Rufas, D.; Torrelles, M.J.; Burkard, S.; Arndt, H.; Drevet, S.; Boudissa, M.; Tonetti, J.; et al. Gait Analysis Platform for Measuring Surgery Recovery. Study Health Technol. Inform. 2021, 285, 199–204. [Google Scholar] [CrossRef]
- Sudharshan, J.; Goodman, G.; Bourbakis, N. Smart Shoes for Temporal Identification and Corrections to Assist People with Abnormal Walking Patterns. In Proceedings of the IEEE 20th International Conference on Bioinformatics and Bioengineering (BIBE), Cincinnati, OH, USA, 26–28 October 2020; pp. 929–933. [Google Scholar] [CrossRef]
- Cai, Y.; Qian, X.; Li, Q.; Lin, F.; Huang, M.-C. Closed-Looped Sensing and Stimulation System for Parkinson’s Disease Early Diagnosis and Rehabilitation. Smart Health 2022, 26, 100338. [Google Scholar] [CrossRef]
- Eizentals, P.; Katashev, A.; Oks, A. Gait Analysis by Using Smart Socks System. IOP Conf. Ser. Mater. Sci. Eng. 2018, 459, 012037. [Google Scholar] [CrossRef]
- Baek, S.; Eom, H.; Hariyani, Y.S.; Kim, G.; Roh, J.; Kim, S.; Park, C. Deep Learning Based Heart Rate Estimation Using Smart Shoes Sensor. In Proceedings of the IEEE International Conference on Consumer Electronics—Asia (ICCE-Asia), Seoul, Republic of Korea, 1–3 November 2020; pp. 1–4. [Google Scholar] [CrossRef]
- Eom, H.; Roh, J.; Hariyani, Y.S.; Baek, S.; Lee, S.; Kim, S.; Park, C. Deep Learning-Based Optimal Smart Shoes Sensor Selection for Energy Expenditure and Heart Rate Estimation. Sensors 2021, 21, 7058. [Google Scholar] [CrossRef]
- La Rosa, D.; Palumbo, F.; Ronca, A.; Sansone, F.; Tesconi, M.; Tonacci, A.; Conte, R. IoT Smart Shoe Solution for Neuromuscular Disease Monitoring. In Lecture Notes of the Institute for Computer Sciences, Social Informatics and Telecommunications Engineering, Proceedings of the Pervasive Computing Technologies for Healthcare, PH 2022, Thessaloniki, Greece, 12–14 December 2022; Tsanas, A., Triantafyllidis, A., Eds.; Springer: Cham, Switzerland, 2023; Volume 488. [Google Scholar] [CrossRef]
- Lee, S.I.; Campion, A.; Huang, A.; Park, E.; Garst, J.H.; Jahanforouz, N.; Espinal, M.; Siero, T.; Pollack, S.; Afridi, M.; et al. Identifying Predictors for Postoperative Clinical Outcome in Lumbar Spinal Stenosis Patients Using Smart-Shoe Technology. J. Neuroeng. Rehabil. 2017, 14, 77. [Google Scholar] [CrossRef] [PubMed]
- Hayakawa, Y.; Kimata, Y.; Kida, K. Study on Human Behavior Classification by Using High-Performance Shoes Equipped with Pneumatic Actuators. J. Robot. Mechatron. 2020, 32, 947–957. [Google Scholar] [CrossRef]
- Giraruchataporn, P.; Ekkachai, K.; Peuchpen, P.; Kijpaiboonwat, S.; Kongprawechnon, W.; Hasegawa, S. Smart Shoe for Predicting Knee Abduction Moment. In Proceedings of the 13th Asian Control. Conference (ASCC), Jeju, Republic of Korea, 4–7 May 2022; pp. 162–166. [Google Scholar] [CrossRef]



| Sl. No | Sensor Type, Its Operation Principle, and Possible Applications in Smart Footwear |
|---|---|
| 1 | Ultrasonic sensors [3]: These sensors utilise ultrasonic waves to measure distance and detect objects. They are one of the most commonly used sensors in footwear, specifically for aiding people with visual disability. They can detect the presence or absence of objects within a specific range. Further, these sensors can measure insole thickness and footwear wear and tear and suggest replacement schedules. |
| 2 | LiDAR sensors [4]: Light detection and ranging (LiDAR) based Time of Flight (ToF) sensors are currently the preferred technology for automotive and drone applications. ToF sensors have the emitter, receiver, and processor system on the same PCB/package for easy, cost-effective, and small-footprint integration. They offer high-speed, precise distance measurement independent of target size, colour, and reflectance. A LiDAR sensor can be integrated into footwear to replace the traditional ultrasonic sensor or added as an additional sensor to support features such as pothole detection, obstacle warning, etc. |
| 3 | Pressure sensors [5]: Pressure sensors measure pressure by converting the applied pressure into an electrical signal that can be measured and utilised for various applications.
|
| 4 | Accelerometers and Gyroscopes [6]: An accelerometer measures linear acceleration and can detect the movement of an object in terms of acceleration, deceleration, or changes in direction. On the other hand, a gyroscope measures angular velocity around a particular axis. It detects changes in orientation or rotational movements, such as tilting, rotating, or twisting. Inertial measurement units (IMUs) incorporate accelerometers and gyroscopes into a single sensor package, providing a more compact and integrated solution for motion-sensing applications. IMUs are integrated into wearable devices to monitor and analyse physical activities. They can measure steps, distance, speed, and calories burned and provide feedback on movement patterns and exercise techniques. |
| 5 | Sweat Sensors [3]: Skin-worn biosensors can analyse the wearer’s sweat to monitor various physiological conditions. Biomarkers in the sweat can be used to detect certain genetic conditions. Also, using the glucose-level correlation between sweat and blood leads to potential applications in the continuous monitoring of diabetes. |
| 6 | Temperature Sensors: Temperature sensors detect and measure the heat and coolness of air, liquids, or solid surfaces and convert them into electrical signals. Types of temperature sensor include:
|
| 7 | Gas sensors can be used to detect foot odour, and they can detect Bromodosis, possibly caused by fungal infection [12]. Bromodosis is smelly feet, and it is often caused by the interaction of sweat with bacteria on the skin’s surface. Fungal infections like athlete’s foot or other dermatophyte infections can also contribute to foot odour. Gas sensors can detect the specific gases emitted by these fungi, aiding in the early identification of such infections. |
| Smart Footwear (Name of the Company) | Applications | Type of Sensor (No. of Sensors Used) | Pressure (kPa) | IE | MDAR (Hz) | DTT | BA (Hrs.) | Cost |
|---|---|---|---|---|---|---|---|---|
| WIISEL | Continuous gait monitoring, analysis & fall risk assessment | Piezoresistive (14) | 350 | Yes | 33.3 | BLE | 16 | — |
| Pedar (Novel) | Footwear design and injury prevention | Pressure (99) | 600 | No | 100 | BT | 1 | 15,540 € |
| F-Scan (Tekscan) | Gait analysis & biomechanics, diabetic offloading, sports medicine | Pressure (960) | 862 | No | 165 | USB, Wi-fi | 0.2 | 16,000 $ |
| BioFoot (IBV) | Sports gait analysis, footwear design | Pressure (64) | 1200 | No | 500 | Wi-Fi | 1 | 12,995 € |
| paroLogg /parotec (paromed) | Foot pressure analysis | Pressure (32), Inertial | 625 | No | 300 | Wi-fi | 1.5 | — |
| Foot Pres- sure MS (Medilogic) | Gait, sports, health prevention, prosthesis and orthotics, diabetics | Solid State Relay (SSR) sensors (240) | 640 | No | 300 | Wireless | — | — |
| Smart Step | Rehabilitation process | — | — | No | — | Card | — | 6000 $ |
| Smart Insoles (24 eight, LLC) | Medical, sports, and gaming | Pressure (4), Inertial | 241 | Yes | — | Wireless | 100 | — |
| OpenGo science (Moticon) | Medical & sports science, Rehabilitation & training analysis | Pressure (13), Inertial | 400 | Yes | 100 | Wireless | — | 2000 $ |
| Footswitches Insole (B & L Engineering) | Gait analysis | Pressure sensors (4) | — | No | — | Wireless | — | 9000 $ |
| Ref. No. | Target Application | Technical Details | Main Findings |
|---|---|---|---|
| [47] | Inertial and plan- tar pressure measurement | Insole, wrist band, accelerometer, gyroscope, pressure sensor, BLE, smartphone, sampling rate 50 Hz. | The best body part for HAR: Feet or wrists. |
| [48] | Six ambulation activities detection | Smart insoles: accelerometer, gyroscope, magnetometer, ECU, BLE, ML algorithms, smartphone, 200 Hz, 120 min, 25–55 years. | Inertial sensors are reliable for dynamic and pressure sensors for stationary activities. |
| [53] | Foot pressure distribution | Capacitive sensor, ML. | ML provides the required pressure measurement. |
| [50] | Plantar pressure and activity recognition | Seven pressure sensors, FFT, ML, 100 Hz, 12-bit, 26 ± 9 years. | Generalization is needed for larger populations. |
| [54] | Foot pressure and motion activities | 280 capacitive pressure sensors, 56 temperature sensors, FT, wired. | Smart insole alternative for activity recognition. |
| [55] | Plantar pressure – daily activity | MWCNTs/PDMS piezoresistive nanocomposites, LAB View. | Useful for disease detection and diagnosis. |
| [56] | Daily activities recognition | Accelerometer, DL, wireless. | SF is user-friendly for all ages. |
| [58] | Locomotor activities | Accelerometer, gyroscope, magnetometer, FFT, CNN. | User-independent system for HAR possible. |
| [62] | Diabetic feet monitoring | Temperature, humidity sensors, eight pressure sensors, BLE, Arduino 328, 25–55 years. | Improves self-management and health outcomes. |
| [64] | DFU prevention | Flexible insoles, 99 capacitance-based sensors, 50 Hz, 2 sensors/cm2, 919 patient’s databases. | Pre-clinical studies met user needs. |
| [67] | DFU monitoring: plantar pressure | Eight pressure sensors, a smartwatch, 8 Hz, and an age group greater than 18 years. | Continuous monitoring reduces DFU recurrence. |
| [68] | DFU: Plantar pressure measurement | Eight capacitive sensors, flexible PCB, BLE, microcontroller, 100 Hz, 28 bits. | Enhances efficiency in studying diabetic foot conditions. |
| [70] | DFU monitoring: Plantar pressure | Pressure sensor, PC, 50 Hz, 76 participants. | Optimization is needed for real-time use. |
| [71] | Diabetic foot monitoring | Four temperature sensors, 35 participants. | Continuous monitoring provides preventative foot ulcer information. |
| [73] | DFU: pressure measurement | Nineteen female participants, 57–75 years, 4D scanner. | Custom insoles and heel pads help redistribute pressure. |
| [74] | DFU monitoring: Temperature, humidity | Textile insole, silicon tubes, leather, five sensors, and 21–30 years of age females. | Textile insoles enhance thermal comfort. |
| [81] | Balance and gait analysis in older women | Thirty women, 65–83 years, lab tests, ethyl vinyl acetate insoles. | Significant reduction in step width observed. |
| [82] | Gait analysis and PD study | Pressure sensors, accelerometer, 29 participants, 100 Hz, 20–59 years. | Dataset valuable for detailed gait analysis. |
| [83] | Fall detection in elderly | Arduino Nano, sensors array, buzzer, vibration motor. | Smart shoes with devices detect and prevent falls. |
| [84] | Mobility and gait assessment | Force sensing resistors, IMU, ultrasound sensor, Arduino, BLE. | Detects abnormalities in walking patterns. |
| [86] | Flat feet detection | Three force sensors, accelerometer, BLE, Arduino Nano. | Cost-effective alternative to motion capture systems. |
| [87] | Real-time gait monitoring | Soft insole, capacitance-based pressure sensor, conductive textile, microcontroller, 100 Hz, 15 participants. | Textile-based insole alternative to smart shoes. |
| [90] | Portable gait analysis | Piezoresistive sensor, IMU, logic unit, 500 Hz, 6 min recording, ML, 14 participants. | Learning-based methods improve gait parameters. |
| [91] | Gait parameters measurement | Piezoresistive sensors, microcontroller, WIFI, IMU, 500 Hz, 9 participants, MAT- LAB. | Useful for out-of-lab gait analysis. |
| [92] | Foot progression angle estimation | Inertial, magnetometer units, accelerometer, gyroscope, 100 Hz, 14 participants, 22–29 years. | Useful for knee osteoarthritis monitoring in daily life. |
| [93] | Detecting changes in gait by alcohol intoxication | Twenty participants, wireless mode, ML algorithm. | SF can be used for detecting alcohol-impaired gait. |
| [94] | Locomotion monitoring: real-time kinetic measurement | Pressure sensors, IMUs, WIFI, Smartphone, PC, sampling rate: 100 Hz, 9 participants, MATLAB 2019b software. | Acceptable matches were achieved for the measured CoPx and the calculated knee joint torques out of 13 movements. |
| [95] | Plantar pressure measurement | Capacitive sensor: silver and cotton, microchip, USB, laptop, BLE. | Gait phases and different patterns can be detected, and the system is bacterial-resistant. |
| [96] | Gait analysis tool: PODOS-mart® | IMUs: Sensors, 11 participants, age group: 20–49 years, BLE, sampling rate: 208 Hz. | Ease of use without technical education. |
| [97] | Evaluating haptic terrain for older adults and PD patients (TreadPort) | Five bladders, PC, VR terrain, WIFI, microcontroller, CAVE display, camera: 60 frames/sec. | Applicable for gait training for walking impediments caused by PD. |
| [98] | Locomotion monitoring: centre of pressure detection | Five textile capacitive sensors, WIFI, sampling rate: 100 Hz, MATLAB R2021a software. | Smart wearable sensors can improve quality of life. |
| [99] | Designing and fabricating biomimetic porous graphene flexible sensor: gait analysis | Graphene nanoplates, SBR foam, silver electrodes, microcontroller, BLE. | The system can monitor older and can help with gait training. |
| [100] | Plantar pressure measurement: gait analysis | Twelve capacitive sensors: copper and poly-dimethyl siloxane, PIC microcontroller, BLE, PC. | The design offers correct performance behaviour under footfall. |
| Ref. No. | Study Objectives | Techniques | Target Group | Outcomes |
|---|---|---|---|---|
| [109] | Stride segmentation of accelerometer data, classification of three walking patterns. | TinyML, edge computing. | - | Mean stride duration is around 1.1 with a 95% confidence interval. |
| [110] | Gait segmentation method based on plantar pressure only. | Thresholding: moving average, statistical analysis. | Six participants: 19–29 years. | The calculated distribution between stance-phase and swing-phase time is almost 60%/40%—aligned with literature studies. |
| [111] | Gait classification using feature analysis. | ML algorithms: RF, k-NN, LR, SVM. | Eighteen participants: 22–31 years. | A combination of accelerometer and gyroscope sensor features with SVM achieved the best performance with 89.36% accuracy. |
| [112] | Gait pattern classification. | ML algorithm: NN. | Eleven participants: 22–33 years. | A built-in accelerometer and gyro sensor gait-pattern classification system can be used without the constraints of a controlled environment. |
| [113] | Detecting 13 commonly used human movements. | ML algorithms: PCA, k-NN, ANN, SVM. | Thirty-four participants: average age 22.6 years. | The model proved to be effective, with an accuracy of 86%. |
| [114] | Gait pattern classification. | ML algorithm: NN. | Six participants. | The architecture with three nodes provided effectiveness metrics above 99.6%. |
| [115] | Gait pattern classification. | ML algorithms: k-NN, SVM, ELM, MLP. | - | ELM performed better, with an overall accuracy of 93.54%. |
| [41] | Detecting walking behaviour. | ML algorithms: NN, DL (CNN). | Three participants: 26–27 years. | The best performance was achieved with convolutional layered ANN with an average accuracy of 84%. |
| [117] | Gait type classification. | DL (CNN) | Fourteen participants: 20–30 years. | Experimental results for seven types of gait showed a high classification rate of more than 90%. |
| [118] | Gait abnormality detection. | DL (CNN) | Twenty-one participants: 24–37 years. | Deployment of CNN-LSTM in Nordic nRF52840 can be revisited with model- pruning and post-training quantization. |
| [119] | Walking pattern analysis. | DL | Video frames. | SF can detect any injury the shoe user is suffering from. |
| [120] | Abnormal gait pattern recognition. | DL (LSTM- CNN) | Twenty-five participants: avg. age 22 years. | A personalised gait classification approach, which is accurate and reliable. |
| [121] | Recognition of foot pronation and supination. | DL (NN) | Six participants. | The system can adequately detect the three footprints’ types with a global error of less than 0.86. |
| [122] | Foot strike pattern classification. | ML algorithms: LR, conditional inference tree, RF. | Thirty participants: 27–41 years. | The system aided in the research and coaching of running movements & obtained the highest classification accuracy of 94% using RF. |
| [124] | Fall detection. | Statistical tool and algorithm. | Seventeen participants: 21–55 years. | The method demonstrated satisfactory performances providing a maximum accuracy of 97.1%. |
| [125] | Fall detection. | Advanced Fall detection algorithm. | Six participants. | The insole can measure walking speed, the distance covered, and the measurement of balance or weight. |
| [88] | Gait analysis and monitoring. | PCA, event detection algorithm. | Four participants. | The new gait metric (eigen analysis) has great potential to be used as a powerful analytical tool for gait disorder diagnostics. |
| [127] | Identification and correction for people with abnormal walking patterns. | ML algorithm: DT. | One thousand two hundred fifty data points—five classes with 250 data points. | The machine learning approach has a 91.68% accuracy and shows promise for assisting people with arthritis. |
| [129] | Gait analysis. | Sum of Manhattan distances (SMD). | Three participants. | Smart socks can be an alternative to smart shoes. |
| [130] | Heart rate estimation. | DL (LSTM- CNN) | Fifteen participants. | Significant levels of heart rate estimation could be made using SF with a correlation of 0.91. |
| [131] | Heart rate and Energy expenditure estimation. | DL (CNN) | Ten participants: 20–24 years. | Estimations can be accurate by effectively selecting the optimal sensors. |
| [133] | Gait analysis. | Multivariate analysis, statistical tool. | Twenty-nine participants: 43–75 years. | SF is ideally suited for preoperative evaluation in the clinical setting. |
| [134] | Human be- haviour classification. | ML algorithm: RF. | Six participants: 20–22 years. | Four types of behaviour were classified with an F-measure of 78.6%. |
| [135] | Knee abduction movement detection. | ML algorithm: MLP regressor. | One participant: 24 years. | The system performed well in predicting KAM with an accuracy of 87%. However, more experimentation is required. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rukmini, P.G.; Hegde, R.B.; Basavarajappa, B.K.; Bhat, A.K.; Pujari, A.N.; Gargiulo, G.D.; Gunawardana, U.; Jan, T.; Naik, G.R. Recent Innovations in Footwear and the Role of Smart Footwear in Healthcare—A Survey. Sensors 2024, 24, 4301. https://doi.org/10.3390/s24134301
Rukmini PG, Hegde RB, Basavarajappa BK, Bhat AK, Pujari AN, Gargiulo GD, Gunawardana U, Jan T, Naik GR. Recent Innovations in Footwear and the Role of Smart Footwear in Healthcare—A Survey. Sensors. 2024; 24(13):4301. https://doi.org/10.3390/s24134301
Chicago/Turabian StyleRukmini, Pradyumna G., Roopa B. Hegde, Bommegowda K. Basavarajappa, Anil Kumar Bhat, Amit N. Pujari, Gaetano D. Gargiulo, Upul Gunawardana, Tony Jan, and Ganesh R. Naik. 2024. "Recent Innovations in Footwear and the Role of Smart Footwear in Healthcare—A Survey" Sensors 24, no. 13: 4301. https://doi.org/10.3390/s24134301








