Accelerometer Thresholds for Estimating Physical Activity Intensity Levels in Infants: A Preliminary Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Population and Setting
2.2. Observational Rating (Video Coding)
2.3. Wearable Accelerometer Data Processing
2.4. Threshold Determination Using True Positive Rate
2.5. Threshold Determination Using Predicted Activity Proportion
2.6. Measures of Evaluation Used
2.7. Validation
3. Results
4. Discussion
5. Limitations of This Study
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Timmons, B.W.; LeBlanc, A.G.; Carson, V.; Connor Gorber, S.; Dillman, C.; Janssen, I.; Kho, M.E.; Spence, J.C.; Stearns, J.A.; Tremblay, M.S. Systematic review of physical activity and health in the early years (aged 0–4 years). Appl. Physiol. Nutr. Metabolism 2012, 37, 773–792. [Google Scholar] [CrossRef] [PubMed]
- Pitchford, E.A.; Ketcheson, L.R.; Kwon, H.J.; Ulrich, D.A. Minimum accelerometer wear time in infants: A generalizability study. J. Phys. Act. Health 2017, 14, 421–428. [Google Scholar] [CrossRef] [PubMed]
- Sirard, J.R.; Trost, S.G.; Pfeiffer, K.A.; Dowda, M.; Pate, R.R. Calibration and evaluation of an objective measure of physical activity in preschool children. J. Phys. Act. Health. 2005, 2, 345–357. [Google Scholar] [CrossRef]
- Rachele, J.N.; McPhail, S.M.; Washington, T.L.; Cuddihy, T.F. Practical physical activity measurement in youth: A review of contemporary approaches. World J. Pediatrics 2012, 8, 207–216. [Google Scholar] [CrossRef]
- Trost, S.G.; Fees, B.S.; Haar, S.J.; Murray, A.D.; Crowe, L.K. Identification and validity of accelerometer cut-points for toddlers. Obesity 2012, 20, 2317–2319. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Jiang, H.; Zhang, T.; Yin, L.; Chen, X.; Luo, J. Comparison of methods for the estimation of the maximum oxygen uptake of men drug addicts. Front. Physiol. 2021, 12, 683942. [Google Scholar] [CrossRef] [PubMed]
- Sylvia, L.G.; Bernstein, E.E.; Hubbard, J.L.; Keating, L.; Anderson, E.J. A practical guide to measuring physical activity. J. Acad. Nutr. Diet. 2014, 114, 199–208. [Google Scholar] [CrossRef]
- Adamo, K.B.; Prince, S.A.; Tricco, A.C.; Connor-Gorber, S.; Tremblay, M. A comparison of indirect versus direct measures for assessing physical activity in the pediatric population: A systematic review. Int. J. Pediatr. Obes. 2009, 4, 2–27. [Google Scholar] [CrossRef]
- da Silva, P.M.R.; Soares, S.H.D.S.S.; Mota, J.A.P.S.; Viana, P.M.M.M.G.; Carvalho, P.M.M.S. Reviving Direct Observation Methods for Physical Activity Behavior. J. Sports Sci. 2021, 9, 9–16. [Google Scholar]
- Trost, S.G.; Loprinzi, P.D.; Moore, R.; Pfeiffer, K.A. Comparison of accelerometer cut points for predicting activity intensity in youth. Med. Sci. Sports Exerc. 2011, 43, 1360–1368. [Google Scholar] [CrossRef] [PubMed]
- Eaton, W.O.; Dureski, C.M. Parent and actometer measures of motor activity level in the young infant. Infant. Behav. Dev. 1986, 9, 383–393. [Google Scholar] [CrossRef]
- Worobey, J.; Islas-Lopez, M. Temperament measures of African-American infants: Change and convergence with age. Early Child Dev. Care 2009, 179, 107–112. [Google Scholar] [CrossRef] [PubMed]
- Evenson, K.R.; Catellier, D.J.; Gill, K.; Ondrak, K.S.; McMurray, R.G. Calibration of two objective measures of physical activity for children. J. Sports Sci. 2008, 26, 1557–1565. [Google Scholar] [CrossRef] [PubMed]
- Giurgiu, M.; Kolb, S.; Nigg, C.; Burchartz, A.; Timm, I.; Becker, M.; Rulf, E.; Doster, A.K.; Koch, E.; Bussmann, J.B.; et al. Assessment of 24-hour physical behaviour in children and adolescents via wearables: A systematic review of free-living validation studies. BMJ Open Sport Exerc. Med. 2022, 8, e001267. [Google Scholar] [CrossRef] [PubMed]
- Camerota, M.; Tully, K.P.; Grimes, M.; Gueron-Sela, N.; Propper, C.B. Assessment of infant sleep: How well do multiple methods compare? Sleep 2018, 41, zsy146. [Google Scholar] [CrossRef] [PubMed]
- Unno, M.; Morisaki, T.; Kinoshita, M.; Saikusa, M.; Iwata, S.; Fukaya, S.; Yamashita, Y.; Nakayama, M.; Saitoh, S.; Iwata, O. Validation of actigraphy in hospitalised newborn infants using video polysomnography. J. Sleep Res. 2022, 31, e13437. [Google Scholar] [CrossRef] [PubMed]
- Bruijns, B.A.; Truelove, S.; Johnson, A.M.; Gilliland, J.; Tucker, P. Infants’ and toddlers’ physical activity and sedentary time as measured by accelerometry: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 14. [Google Scholar] [CrossRef] [PubMed]
- Borkhoff, C.M.; Heale, L.D.; Anderson, L.N.; Tremblay, M.S.; Maguire, J.L.; Parkin, P.C.; Birken, C.S. Objectively measured physical activity of young Canadian children using accelerometry. Appl. Physiol. Nutr. Metab. 2015, 40, 1302–1308. [Google Scholar] [CrossRef] [PubMed]
- Jia, Z.; Zhang, J.; Trindade, D.; Sobko, T. Physical activity patterns and correlates of 9-month-old Chinese infants in the Macau population. Matern. Child Health J. 2018, 22, 1526–1533. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.C.; Chen, L.C.; Tung, Y.C.; Lee, C.C.; Tsai, S.Y. Physical activity and objectively assessed sleep in 6-month-old infants in Taiwan. Res. Nurs. Health 2019, 42, 128–135. [Google Scholar] [CrossRef] [PubMed]
- Tsai, S.Y.; Barnard, K.E.; Lentz, M.J.; Thomas, K.A. Mother-infant activity synchrony as a correlate of the emergence of circadian rhythm. Biol. Res. Nurs. 2011, 13, 80–88. [Google Scholar] [CrossRef] [PubMed]
- Lettink, A.; Altenburg, T.M.; Arts, J.; van Hees, V.T.; Chinapaw, M.J.M. Systematic review of accelerometer-based methods for 24-h physical behavior assessment in young children (0–5 years old). Int. J. Behav. Nutr. Phys. Act. 2022, 19, 116. [Google Scholar] [CrossRef] [PubMed]
- Galland, B.C.; Kennedy, G.J.; Mitchell, E.A.; Taylor, B.J. Algorithms for using an activity-based accelerometer for identification of infant sleep–wake states during nap studies. Sleep Med. 2012, 13, 743–751. [Google Scholar] [CrossRef] [PubMed]
- Insana, S.P.; Gozal, D.; Montgomery-Downs, H.E. Invalidity of one actigraphy brand for identifying sleep and wake among infants. Sleep Med. 2010, 11, 191–196. [Google Scholar] [CrossRef] [PubMed]
- Rioualen, S.; Roué, J.M.; Lefranc, J.; Gouillou, M.; Nowak, E.; Alavi, Z.; Dubourg, M.; Sizun, J. Actigraphy is not a reliable method for measuring sleep patterns in neonates. Acta Paediatr. 2015, 104, e478–e482. [Google Scholar] [CrossRef] [PubMed]
- Lewicke, A.T.; Sazonov, E.S.; Schuckers, S.A.C. Sleep-wake identification in infants: Heart rate variability compared to actigraphy. In Proceedings of the 26th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, San Francisco, CA, USA, 1–5 September 2004; Volume 1, pp. 442–445. [Google Scholar]
- Horger, M.N.; Marsiliani, R.; DeMasi, A.; Allia, A.; Berger, S.E. Researcher choices for infant sleep assessment: Parent report, actigraphy, and a novel video system. J. Genet. Psychol. 2021, 182, 218–235. [Google Scholar] [CrossRef]
- Sadeh, A.; Acebo, C.; Seifer, R.; Aytur, S.; Carskadon, M.A. Activity-based assessment of sleep-wake patterns during the 1st year of life. Infant. Behav. Dev. 1995, 18, 329–337. [Google Scholar] [CrossRef]
- Gnidovec, B.; Neubauer, D.; Zidar, J. Actigraphic assessment of sleep–wake rhythm during the first 6 months of life. Clin. Neurophysiol. 2002, 113, 1815–1821. [Google Scholar] [CrossRef]
- Hewitt, L.; Stanley, R.M.; Cliff, D.; Okely, A.D. Objective measurement of tummy time in infants (0–6 months): A validation study. PLoS ONE 2019, 14, e0210977. [Google Scholar] [CrossRef] [PubMed]
- Greenspan, B.; Cunha, A.B.; Lobo, M.A. Design and validation of a smart garment to measure positioning practices of parents with young infants. Infant. Behav. Dev. 2021, 62, 101530. [Google Scholar] [CrossRef] [PubMed]
- Airaksinen, M.; Räsänen, O.; Ilén, E.; Häyrinen, T.; Kivi, A.; Marchi, V.; Gallen, A.; Blom, S.; Varhe, A.; Kaartinen, N.; et al. Automatic posture and movement tracking of infants with wearable movement sensors. Sci. Rep. 2020, 10, 169. [Google Scholar] [CrossRef] [PubMed]
- Jun, K.; Choi, S. Unsupervised end-to-end deep model for newborn and infant activity recognition. Sensors 2020, 20, 6467. [Google Scholar] [CrossRef] [PubMed]
- Smith, B.A.; Trujillo-Priego, I.A.; Lane, C.J.; Finley, J.M.; Horak, F.B. Daily quantity of infant leg movement: Wearable sensor algorithm and relationship to walking onset. Sensors 2015, 15, 19006–19020. [Google Scholar] [CrossRef] [PubMed]
- Liu, T.; Benjamin-Neelon, S.E. A longitudinal study of infant 24-hour sleep: Comparisons of sleep diary and accelerometer with different algorithms. Sleep 2023, 46, zsad160. [Google Scholar] [CrossRef] [PubMed]
- Bucko, A.G.; Armstrong, B.; McIver, K.L.; McLain, A.C.; Pate, R.R. Longitudinal associations between sleep and weight status in infants and toddlers. Pediatr. Obes. 2023, 18, e13056. [Google Scholar] [CrossRef] [PubMed]
- Ricardo, L.I.C.; Da Silva, I.C.M.; Martins, R.C.; Wendt, A.; Gonçalves, H.; Hallal, P.R.C.; Wehrmeister, F.C. Protocol for objective measurement of infants’ physical activity using accelerometry. Med. Sci. Sports Exerc. 2018, 50, 1084–1092. [Google Scholar] [CrossRef] [PubMed]
- Thelagathoti, R.K.; Chaudhary, P.; Knarr, B.; Schenkelberg, M.; Ali, H.H.; Dinkel, D. Exploring infant physical activity using a population-based network analysis approach. Analytics 2024, 3, 14–29. [Google Scholar] [CrossRef]
- Thureen, P.J.; Phillips, R.E.; Baron, K.A.; DeMarie, M.P.; Hay, W.W., Jr. Direct measurement of the energy expenditure of physical activity in preterm infants. J. Appl. Physiol. 1998, 85, 223–230. [Google Scholar] [CrossRef] [PubMed]
- Deng, W.; Trujillo-Priego, I.A.; Smith, B.A. How many days are necessary to represent an infant’s typical daily leg movement behavior using wearable sensors? Phys. Ther. 2019, 99, 730–738. [Google Scholar] [CrossRef]
- Deng, W.; Nishiyori, R.; Vanderbilt, D.L.; Smith, B.A. How many days are necessary to represent typical daily leg movement behavior for infants at risk of developmental disabilities? Sensors 2020, 20, 5344. [Google Scholar] [CrossRef] [PubMed]
- Neishabouri, A.; Nguyen, J.; Samuelsson, J.; Guthrie, T.; Biggs, M.; Wyatt, J.; Cross, D.; Karas, M.; Migueles, J.H.; Khan, S.; et al. Quantification of acceleration as activity counts in ActiGraph wearables. Sci. Rep. 2022, 12, 11958. [Google Scholar] [CrossRef] [PubMed]
- Brønd, J.C.; Andersen, L.B.; Arvidsson, D. Generating ActiGraph counts from raw acceleration recorded by an alternative monitor. Med. Sci. Sports Exerc. 2017, 49, 2351–2360. [Google Scholar] [CrossRef] [PubMed]
- Doherty, A.; Jackson, D.; Hammerla, N.; Plötz, T.; Olivier, P.; Granat, M.H.; White, T.; Van Hees, V.T.; Trenell, M.I.; Owen, C.G.; et al. Large scale population assessment of physical activity using wrist worn accelerometers: The UK biobank study. PLoS ONE 2017, 12, e0169649. [Google Scholar] [CrossRef] [PubMed]
- Snyder, R.G.; Schneider, L.W.; Owings, C.L.; Reynolds, H.M.; Golomb, D.H.; Schork, M.A. Anthropometry of Infants, Children, and Youths to Age 18 for Product Safety Design; Highway Safety Research Institute: Ann Arbor, MI, USA, 1977. [Google Scholar]
- Zhou, J.; Schaefer, S.Y.; Smith, B.A. Quantifying caregiver movement when measuring infant movement across a full day: A case report. Sensors 2019, 19, 2886. [Google Scholar] [CrossRef] [PubMed]

| Measure | Type | Advantages | Limitations |
|---|---|---|---|
| Doubly labeled water (DLW) | direct | highly valid and reliable for estimating energy expenditure, unobtrusive, non-invasive | excessive cost, inability to capture duration of activity, participant burden, difficult logistics of multiple urine collections, multiple visits [4] |
| Maximal oxygen consumption (VO2MAX) | direct | highly valid, real-time or recorded data | expensive, difficult to carry, cumbersome to operate, potential safety issues for the very young [6] |
| Heart rate (HR) monitoring | direct | real-time or recorded data for long periods, unobtrusive, modest cost, relatively low participant burden | accuracy affected by emotional state, ambient temperature, fitness level, [4] muscle mass, [7] age, [4] can remain elevated after movement has stopped, i.e., lag [8] |
| Observational rating (video coding) | direct | flexible, provides contextual information, provides details on activities | high cost of time and energy, [9] potential for reactivity, [7] exists for children but not infants [3,5] |
| Wearable accelerometer | direct | real-time or recorded data for long periods, unobtrusive, small size, relatively modest cost, [4] relatively low participant burden | sensitivity of thresholds to age group and activity type, [10] potential for reactivity |
| Self-reported diaries | indirect | low cost, low participant burden | limited reliability [11,12] |
| Participant Code | Group | Age (Days) | Body Length (cm) | Thigh + Shank Length (cm) | Aligned Session Length (min) |
|---|---|---|---|---|---|
| 1 | TD | 31 | 53 | 18.5 | 5.96 |
| 2 | TD | 297 | 75.5 | 27.3 | 6.42 |
| 3 | TD | 65 | 61.5 | 23.6 | 8.45 |
| 4 | TD | 129 | 68.7 | 21.7 | 6.64 |
| 5 | TD | 47 | 59.8 | 25.7 | 4.69 |
| 6 | TD | 44 | 56 | 26 | 2.71 |
| 7 | AR | 137 * | 59.5 | 27 | 5.76 |
| 8 | AR | 333 * | 68.5 | 27.6 | 5.56 |
| 9 | AR | 202 * | 67 | 32 | 6.11 |
| 10 | AR | 433 * | 70 | 32 | 4.98 |
| Accelerometer | |||||
| Sedentary | Active | ||||
| Primary optimization step | Gold standard (observational rating) | Sedentary | SEDSED | SEDACTIVE | |
| Active | ACTIVESED | ACTIVEACTIVE | |||
| Accelerometer | |||||
| Sedentary | Light | MV | |||
| Secondary optimization step | Gold standard (observational rating) | Sedentary | SEDSED | SEDLIGHT | SEDMV |
| Light | LIGHTSED | LIGHTLIGHT | LIGHTMV | ||
| MV | MVSED | MVLIGHT | MVMV | ||
| Primary optimization step | Definitions: SEDSED: Sedentary, correctly predicted as sedentary SEDACTIVE: Sedentary, incorrectly predicted as active ACTIVESED: Active, incorrectly predicted as sedentary ACTIVEACTIVE: Active, correctly predicted as active | ||||
| Secondary optimization step | Definitions: SEDSED: Sedentary, correctly predicted as sedentary SEDLIGHT: Sedentary, incorrectly predicted as light SEDMV: Sedentary, incorrectly predicted as MV LIGHTSED: Light, incorrectly predicted as sedentary LIGHTLIGHT: Light, correctly predicted as light LIGHTMV: Light, incorrectly predicted as MV MVSED: MV, incorrectly predicted as sedentary MVLIGHT: MV, incorrectly predicted as light MVMV: MV, correctly predicted as MV | ||||
| Threshold value | Threshold Name | Jerk, TP (m/s2) | Jerk, PAP (m/s2) | Acceleration, TP (m/s) | Acceleration, PAP (m/s) | |
| Primary optimization | Sedentary/active | 27.0 | 18.0 | 1.30 | 1.0 | |
| Secondary optimization | Light/MV | 41.0 | 56.0 | 1.80 | 2.6 | |
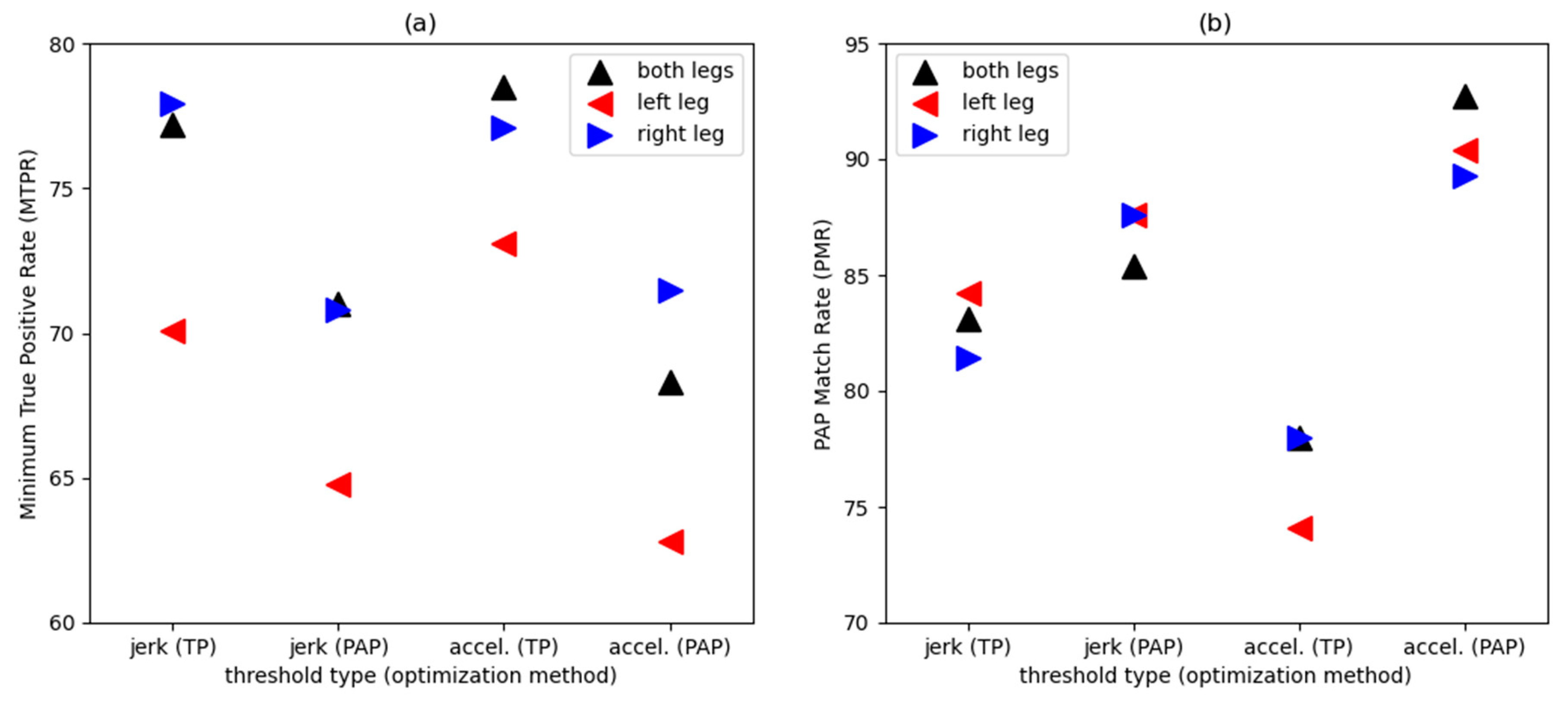
| Overall rating, each threshold | Evaluation metric | Jerk, TP | Jerk, PAP | Acceleration, TP | Acceleration, PAP | |
| Primary optimization | MTPR | 78.4 | 71.5 | 78.5 | 76.4 | |
| PMR | 97.2 | 85.4 | 97.7 | 92.7 | ||
| Secondary optimization | MTPR | 77.2 | 71.0 | 78.5 | 68.3 | |
| PMR | 83.1 | 85.4 | 78.0 | 92.7 |
| Threshold value | Threshold Name | Jerk, TP (m/s2) | Jerk, PAP (m/s2) | Acceleration, TP (m/s) | Acceleration, PAP (m/s) | |
| Primary optimization | Sedentary/active | 10.0 | 8.00 | 0.600 | 0.50 | |
| Secondary optimization | Light/MV | 16.0 | 27.0 | 0.800 | 1.30 | |
| Overall rating, each threshold | Evaluation metric | Jerk, TP | Jerk, PAP | Acceleration, TP | Acceleration, PAP | |
| Primary optimization | MTPR | 70.1 | 65.3 | 67.8 | 70.8 | |
| PMR | 96.1 | 91.5 | 80.8 | 90.4 | ||
| Secondary optimization | MTPR | 70.1 | 64.8 | 73.1 | 62.8 | |
| PMR | 84.2 | 87.6 | 74.1 | 90.4 |
| Threshold value | Threshold Name | Jerk, TP (m/s2) | Jerk, PAP (m/s2) | Acceleration, TP (m/s) | Acceleration, PAP (m/s) | |
| Primary optimization | Sedentary/active | 11.0 | 7.00 | 0.400 | 0.300 | |
| Secondary optimization | Light/MV | 17.0 | 24.0 | 0.800 | 1.00 | |
| Overall rating, each threshold | Evaluation metric | Jerk, TP | Jerk, PAP | Acceleration, TP | Acceleration, PAP | |
| Primary optimization | MTPR | 78.5 | 70.8 | 77.1 | 71.5 | |
| PMR | 97.7 | 87.6 | 97.7 | 89.3 | ||
| Secondary optimization | MTPR | 77.9 | 70.8 | 77.1 | 71.5 | |
| PMR | 81.4 | 87.6 | 78.0 | 89.3 |
| Gold Standard | Jerk, TP | Jerk, PAP | Acceleration, TP | Acceleration, PAP | |||
|---|---|---|---|---|---|---|---|
| Primary optimization step | True positive rate (%) | Sedentary | 100 | 78.5 | 71.5 | 78.5 | 76.4 |
| Active | 100 | 82.9 | 92.9 | 83.4 | 90.0 | ||
| True negative rate (%) | Sedentary | 100 | 82.9 | 92.9 | 83.4 | 90.0 | |
| Active | 100 | 78.5 | 71.5 | 78.5 | 76.4 | ||
| Predicted activity proportion (%) | Sedentary Active | 40.6 | 42.0 | 33.2 | 41.7 | 36.9 | |
| 59.4 | 58.0 | 66.8 | 58.3 | 63.1 | |||
| Secondary optimization step | True positive rate (%) | Sedentary | 100 | 78.5 | 71.5 | 78.5 | 76.4 |
| Light | 100 | 25.8 | 54.5 | 18.2 | 51.5 | ||
| MV | 100 | 77.2 | 71.0 | 80.0 | 68.3 | ||
| True negative rate (%) | Sedentary | 100 | 82.9 | 92.9 | 83.4 | 90.0 | |
| Light | 100 | 93.4 | 83.0 | 94.8 | 84.4 | ||
| MV | 100 | 72.4 | 76.7 | 69.5 | 78.1 | ||
| Predicted activity proportion (%) | Sedentary | 40.6 | 42.0 | 33.2 | 41.7 | 36.9 | |
| Light | 18.6 | 10.1 | 23.9 | 7.61 | 22.3 | ||
| MV | 40.8 | 47.9 | 42.8 | 50.7 | 40.8 |
| Gold Standard | Jerk, TP | Jerk, PAP | Acceleration, TP | Acceleration, PAP | |||
|---|---|---|---|---|---|---|---|
| Primary optimization step | True positive rate (%) | Sedentary | 100 | 70.1 | 65.3 | 76.4 | 70.8 |
| Active | 100 | 76.3 | 83.4 | 67.8 | 72.0 | ||
| True negative rate (%) | Sedentary | 100 | 76.3 | 83.4 | 67.8 | 72.0 | |
| Active | 100 | 70.1 | 65.3 | 76.4 | 70.8 | ||
| Predicted activity proportion (%) | Sedentary Active | 40.6 | 42.5 | 36.3 | 50.1 | 45.4 | |
| 59.4 | 57.5 | 63.7 | 49.9 | 54.6 | |||
| Secondary optimization step | True positive rate (%) | Sedentary | 100 | 70.1 | 65.3 | 95.2 | 70.8 |
| Light | 100 | 18.2 | 45.5 | 9.09 | 18.2 | ||
| MV | 100 | 76.6 | 64.8 | 73.1 | 62.8 | ||
| True negative rate (%) | Sedentary | 100 | 76.3 | 83.4 | 67.8 | 72.0 | |
| Light | 100 | 91.0 | 79.9 | 95.2 | 82.4 | ||
| MV | 100 | 73.8 | 79.0 | 75.7 | 81.0 | ||
| Predicted activity proportion (%) | Sedentary | 40.6 | 42.5 | 36.3 | 50.1 | 45.4 | |
| Light | 18.6 | 10.7 | 24.8 | 5.63 | 17.7 | ||
| MV | 40.8 | 46.8 | 38.9 | 44.2 | 36.9 |
| Gold Standard | Jerk, TP | Jerk, PAP | Acceleration, TP | Acceleration, PAP | |||
|---|---|---|---|---|---|---|---|
| Primary optimization step | True positive rate (%) | Sedentary | 100 | 78.5 | 70.8 | 77.1 | 71.5 |
| Active | 100 | 83.4 | 90.5 | 86.3 | 89.6 | ||
| True negative rate (%) | Sedentary | 100 | 83.4 | 90.5 | 86.3 | 89.6 | |
| Active | 100 | 78.5 | 70.8 | 77.1 | 71.5 | ||
| Predicted activity proportion (%) | Sedentary Active | 40.6 | 41.7 | 34.4 | 39.4 | 35.2 | |
| 59.4 | 58.3 | 65.6 | 60.6 | 64.8 | |||
| Secondary optimization step | True positive rate (%) | Sedentary | 100 | 78.5 | 70.8 | 77.1 | 71.5 |
| Light | 100 | 13.6 | 37.9 | 10.6 | 31.8 | ||
| MV | 100 | 77.9 | 71.7 | 80.0 | 73.8 | ||
| True negative rate (%) | Sedentary | 100 | 83.4 | 90.5 | 86.3 | 89.6 | |
| Light | 100 | 91.7 | 82.0 | 91.7 | 83.7 | ||
| MV | 100 | 71.0 | 75.2 | 67.6 | 73.8 | ||
| Predicted activity proportion (%) | Sedentary | 40.6 | 41.7 | 34.4 | 39.4 | 35.2 | |
| Light | 18.6 | 9.30 | 21.7 | 8.73 | 19.2 | ||
| MV | 40.8 | 49.0 | 43.9 | 51.8 | 45.6 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ghazi, M.A.; Zhou, J.; Havens, K.L.; Smith, B.A. Accelerometer Thresholds for Estimating Physical Activity Intensity Levels in Infants: A Preliminary Study. Sensors 2024, 24, 4436. https://doi.org/10.3390/s24144436
Ghazi MA, Zhou J, Havens KL, Smith BA. Accelerometer Thresholds for Estimating Physical Activity Intensity Levels in Infants: A Preliminary Study. Sensors. 2024; 24(14):4436. https://doi.org/10.3390/s24144436
Chicago/Turabian StyleGhazi, Mustafa A., Judy Zhou, Kathryn L. Havens, and Beth A. Smith. 2024. "Accelerometer Thresholds for Estimating Physical Activity Intensity Levels in Infants: A Preliminary Study" Sensors 24, no. 14: 4436. https://doi.org/10.3390/s24144436





