Breathing Monitoring in Soccer: Part I—Validity of Commercial Wearable Sensors
Abstract
:1. Introduction
2. Materials and Methods
2.1. Experimental Set-Up and Protocol
- A paced-breathing test of 5 min. This phase was included to systematically test the performance of the three commercial devices at different values. Participants were asked to run at a moderate self-paced speed while pacing their according to a metronome track beeping from 15 bpm to 75 bpm (the inspiratory and expiratory phases had two different tones to facilitate the execution of the task). Participants received the output of the digital metronome through in-ear headphones connected to a smartphone attached to their upper arm.
- A warm-up with the ball of 5 min. This phase was included to test the performance of the three commercial devices during classical movements made by soccer players when passing the ball and running with it.
- A shuttle run intermittent test of 9 min. This test reproduced the protocol performed in a previous study composed of 15 s of work and 30 s of passive recovery [17]. The test consisted of 12 shuttle runs performed according to a maximal session effort prescription. This test was chosen to verify whether the three commercial devices are suitable for describing the fast response of to the alternation of work and rest commonly observed during this test [17].
- A cool-down of 5 min. This test phase was included to evaluate the performance of the three commercial devices during a slow recovery run.
2.2. Wearable Devices and Related Respiratory Signals
2.2.1. Reference System
2.2.2. ComfTech® Vest
2.2.3. Tyme WearTM Vest
2.2.4. BioharnessTM 3.0 Strap
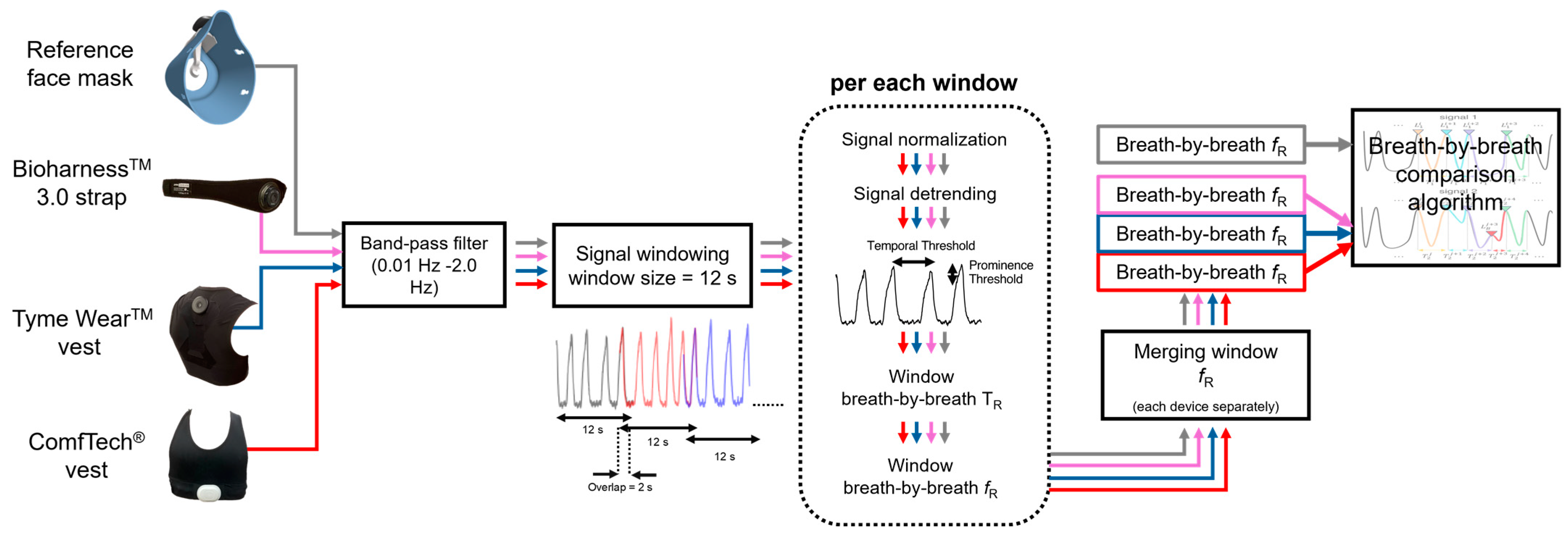
2.3. Signal Pre-Processing
2.4. Data Analysis and Respiratory Rate Estimation
2.5. Breath-by-Breath Comparison
- True positives: for any , the nearest was considered a true positive if it fell within . In such cases, the values were computed as the ratio between 60 and or .
- False positives: (i) the nearest of any was counted as a false positive if it did not fall within ; (ii) any that was not the nearest of any reference was also counted as a false positive.
- False negatives: finally, when did not have any nearest falling within , a false negative was counted.
2.6. Identification of the Prominence Percentage for Each Commercial Device
2.7. Comparison Based on Second-by-Second Values and Different Window Lengths
3. Results
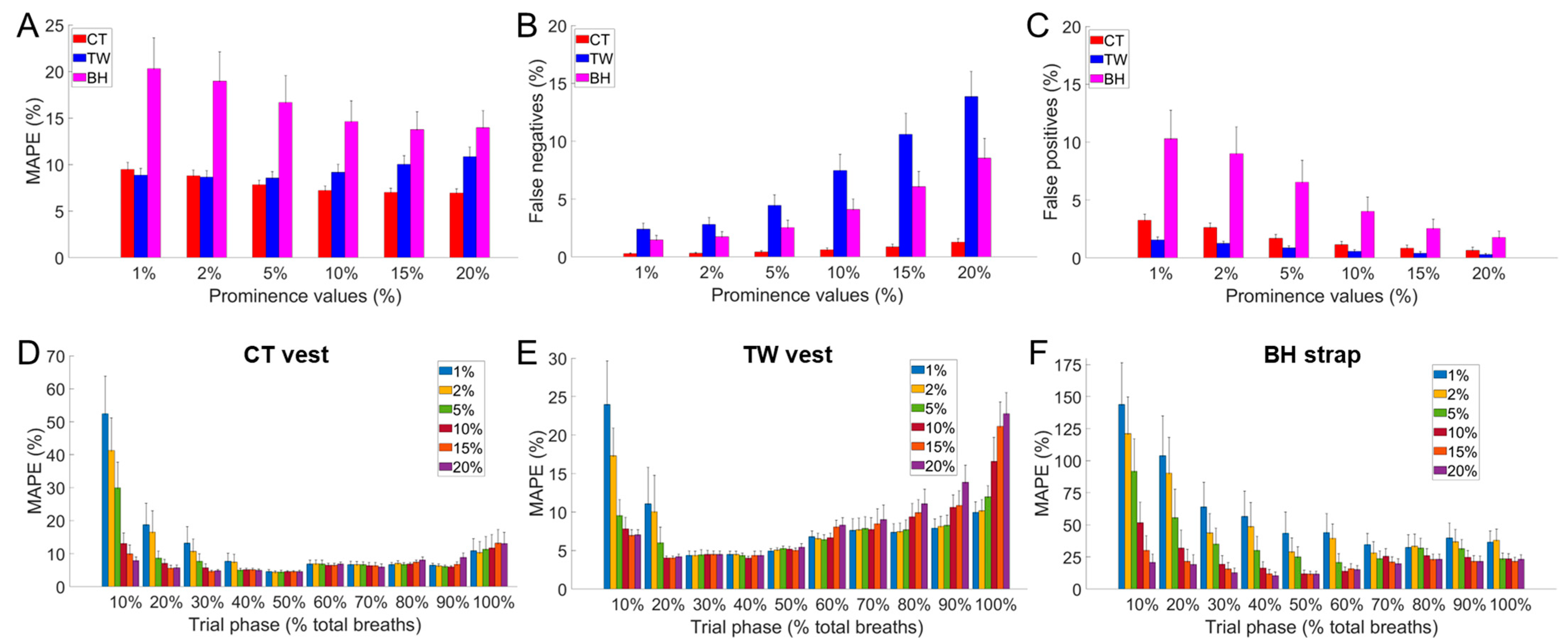
3.1. Identification of the Prominence Threshold for Each Commercial Device
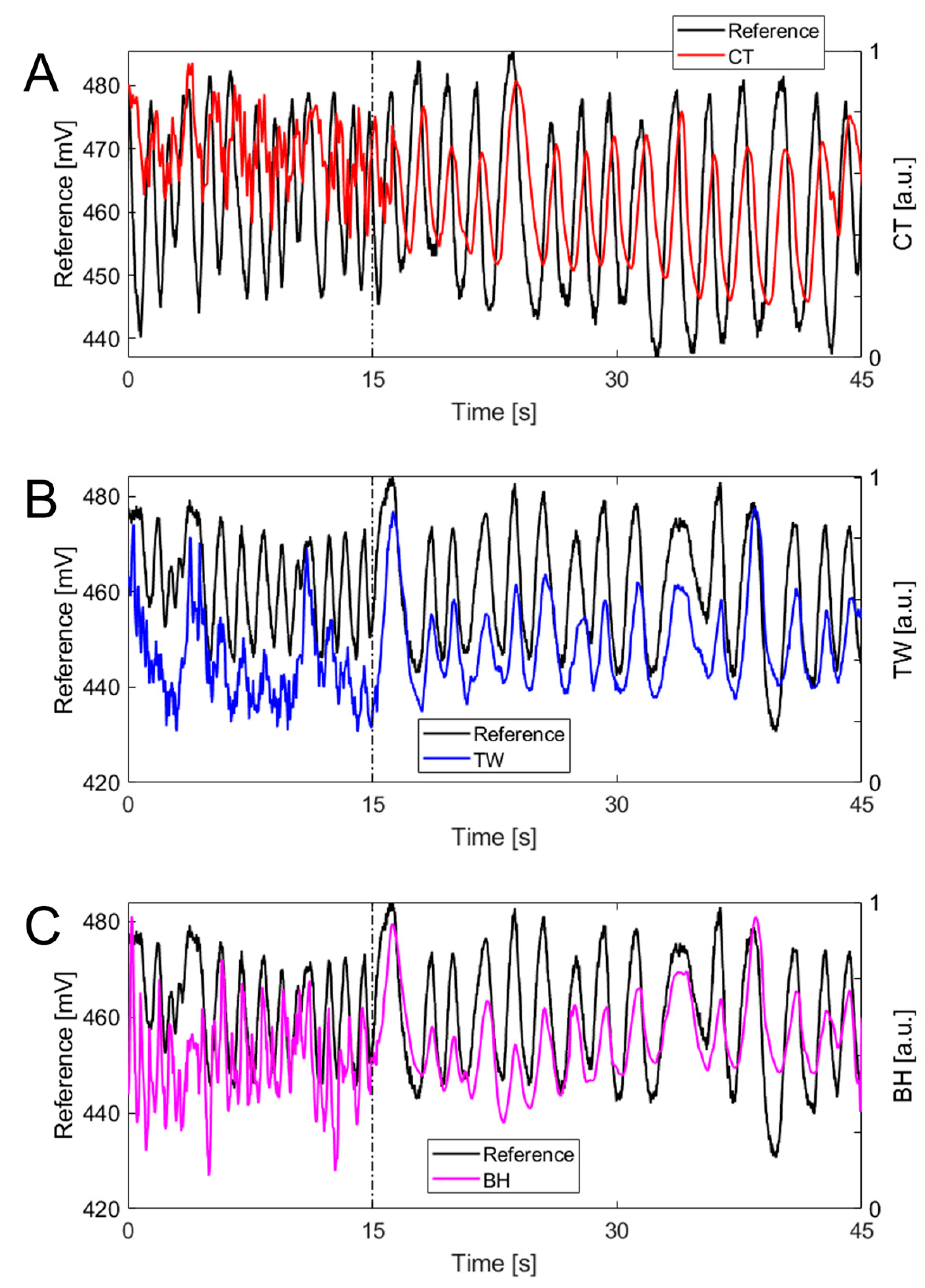
3.2. Respiratory Frequency Time Course
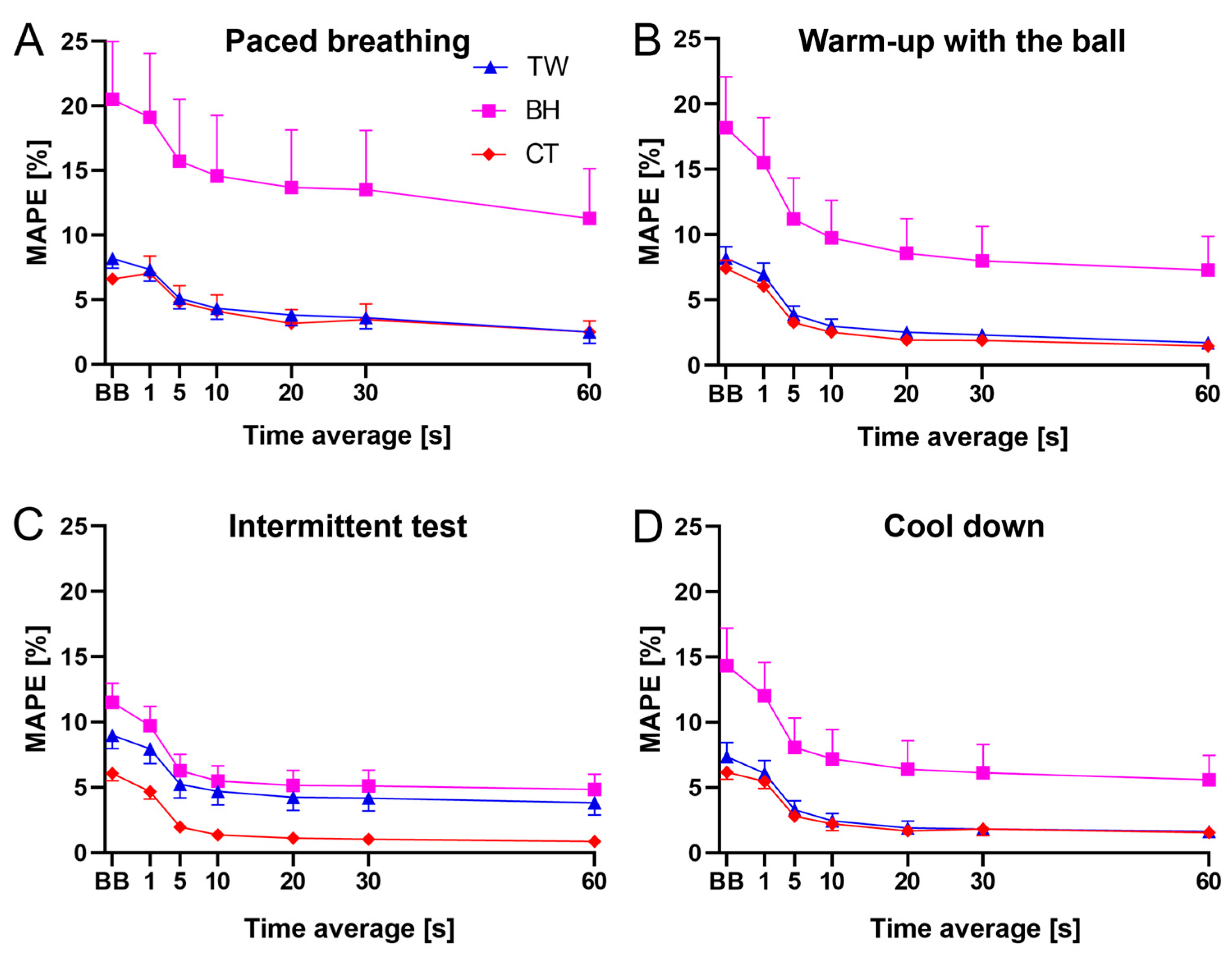
3.3. MAPE Values across Phases and Window Lengths
3.4. Individual Values of Precision and Accuracy
4. Discussion
4.1. ComfTech® Vest
4.2. Tyme WearTM Vest
4.3. BioharnessTM 3.0 Strap
4.4. Validation Methodology
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mandorino, M.; Tessitore, A.; Lacome, M. Loading or Unloading? This Is the Question! A Multi-Season Study in Professional Football Players. Sports 2024, 12, 148. [Google Scholar] [CrossRef] [PubMed]
- Mandorino, M.; Clubb, J.; Lacome, M. Predicting Soccer Players’ Fitness Status Through a Machine-Learning Approach. Int. J. Sports Physiol. Perform. 2024, 19, 443–453. [Google Scholar] [CrossRef] [PubMed]
- Seshadri, D.R.; Thom, M.L.; Harlow, E.R.; Gabbett, T.J.; Geletka, B.J.; Hsu, J.J.; Drummond, C.K.; Phelan, D.M.; Voos, J.E. Wearable Technology and Analytics as a Complementary Toolkit to Optimize Workload and to Reduce Injury Burden. Front. Sport. Act. Living 2021, 2, 630576. [Google Scholar] [CrossRef] [PubMed]
- Akenhead, R.; Nassis, G.P. Training Load and Player Monitoring in High-Level Football: Current Practice and Perceptions. Int. J. Sports Physiol. Perform. 2016, 11, 587–593. [Google Scholar] [CrossRef] [PubMed]
- Ravé, G.; Granacher, U.; Boullosa, D.; Hackney, A.C.; Zouhal, H. How to Use Global Positioning Systems (GPS) Data to Monitor Training Load in the “Real World” of Elite Soccer. Front. Physiol. 2020, 11, 560581. [Google Scholar] [CrossRef] [PubMed]
- Osgnach, C.; di Prampero, P.E.; Zamparo, P.; Morin, J.B.; Pavei, G. Mechanical and Metabolic Power in Accelerated Running–Part II: Team Sports. Eur. J. Appl. Physiol. 2024, 124, 417–431. [Google Scholar] [CrossRef] [PubMed]
- Clavel, P.; Leduc, C.; Morin, J.B.; Buchheit, M.; Lacome, M. Reliability of Individual Acceleration-Speed Profile in-Situ in Elite Youth Soccer Players. J. Biomech. 2023, 153, 111602. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, P.; Tavares, F.; Loureiro, N.; Ferreira, R.; Araújo, J.P.; Reis, J.; Vaz, J.R. In-Situ Acceleration-Speed Profile of an Elite Soccer Academy: A Cross-Sectional Study. J. Sports Sci. 2023, 41, 1868–1874. [Google Scholar] [CrossRef] [PubMed]
- Beato, M.; Devereux, G.; Stiff, A. Validity and Reliability of Global Positioning System Units (STATSports Viper) for Measuring Distance and Peak Speed in Sports. J. Strength Cond. Res. 2018, 32, 2831–2837. [Google Scholar] [CrossRef]
- Impellizzeri, F.M.; Shrier, I.; McLaren, S.J.; Coutts, A.J.; McCall, A.; Slattery, K.; Jeffries, A.C.; Kalkhoven, J.T. Understanding Training Load as Exposure and Dose. Sports Med. 2023, 53, 1667–1679. [Google Scholar] [CrossRef]
- Jeffries, A.C.; Marcora, S.M.; Coutts, A.J.; Wallace, L.; McCall, A.; Impellizzeri, F.M. Development of a Revised Conceptual Framework of Physical Training for Use in Research and Practice. Sports Med. 2022, 52, 709–724. [Google Scholar] [CrossRef] [PubMed]
- Foster, C.; Rodriguez-Marroyo, J.A.; De Koning, J.J. Monitoring Training Loads: The Past, the Present, and the Future. Int. J. Sports Physiol. Perform. 2017, 12, 2–8. [Google Scholar] [CrossRef] [PubMed]
- Halson, S.L. Monitoring Training Load to Understand Fatigue in Athletes. Sports Med. 2014, 44 (Suppl. S2), 139–147. [Google Scholar] [CrossRef] [PubMed]
- Martin, M.; Rampinini, E.; Bosio, A.; Azzalin, A.; McCall, A.; Ward, P. Relationships Between Internal and External Load Measures and Fitness Level Changes in Professional Soccer Players. Res. Q. Exerc. Sport 2023, 94, 760–772. [Google Scholar] [CrossRef] [PubMed]
- Impellizzeri, F.M.; Rampinini, E.; Marcora, S.M. Physiological Assessment of Aerobic Training in Soccer. J. Sports Sci. 2005, 23, 583–592. [Google Scholar] [CrossRef] [PubMed]
- Alexandre, D.; Da Silva, C.D.; Hill-Haas, S.; Wong, D.P.; Natali, A.J.; De Lima, J.R.P.; Filho, M.G.B.B.; Marins, J.J.C.B.; Garcia, E.S.; Karim, C. Heart Rate Monitoring in Soccer: Interest and Limits during Competitive Match Play and Training, Practical Application. J. Strength Cond. Res. 2012, 26, 2890–2906. [Google Scholar] [CrossRef] [PubMed]
- Nicolò, A.; Montini, M.; Girardi, M.; Felici, F.; Bazzucchi, I.; Sacchetti, M. Respiratory Frequency as a Marker of Physical Effort during High-Intensity Interval Training in Soccer Players. Int. J. Sports Physiol. Perform. 2020, 15, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Coutts, A.J.; Rampinini, E.; Marcora, S.M.; Castagna, C.; Impellizzeri, F.M. Heart Rate and Blood Lactate Correlates of Perceived Exertion during Small-Sided Soccer Games. J. Sci. Med. Sport 2009, 12, 79–84. [Google Scholar] [CrossRef] [PubMed]
- Drust, B.; Atkinson, G.; Reilly, T. Future Perspectives in the Evaluation of the Physiological Demands of Soccer. Sports Med. 2007, 37, 783–805. [Google Scholar] [CrossRef]
- Nicolò, A.; Marcora, S.M.; Bazzucchi, I.; Sacchetti, M. Differential Control of Respiratory Frequency and Tidal Volume during High-Intensity Interval Training. Exp. Physiol. 2017, 102, 934–949. [Google Scholar] [CrossRef]
- Nicolò, A.; Massaroni, C.; Passfield, L. Respiratory Frequency during Exercise: The Neglected Physiological Measure. Front. Physiol. 2017, 8. [Google Scholar] [CrossRef] [PubMed]
- Romano, C.; Nicolò, A.; Innocenti, L.; Sacchetti, M.; Schena, E.; Massaroni, C. Design and Testing of a Smart Facemask for Respiratory Monitoring during Cycling Exercise. Biosensors 2023, 13, 369. [Google Scholar] [CrossRef]
- Nicolò, A.; Massaroni, C.; Schena, E.; Sacchetti, M. The Importance of Respiratory Rate Monitoring: From Healthcare to Sport and Exercise. Sensors 2020, 20, 6396. [Google Scholar] [CrossRef] [PubMed]
- Massaroni, C.; Nicolò, A.; Lo Presti, D.; Sacchetti, M.; Silvestri, S.; Schena, E. Contact-Based Methods for Measuring Respiratory Rate. Sensors 2019, 19, 908. [Google Scholar] [CrossRef] [PubMed]
- Vanegas, E.; Igual, R.; Plaza, I. Sensing Systems for Respiration Monitoring: A Technical Systematic Review. Sensors 2020, 20, 5446. [Google Scholar] [CrossRef] [PubMed]
- Aliverti, A. Wearable Technology: Role in Respiratory Health and Disease. Breathe 2017, 13, e27–e36. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Allen, J.; Zheng, D.; Chen, F. Recent Development of Respiratory Rate Measurement Technologies. Physiol. Meas. 2019, 40, 07TR01. [Google Scholar] [CrossRef] [PubMed]
- Chu, M.; Nguyen, T.; Pandey, V.; Zhou, Y.; Pham, H.N.; Bar-Yoseph, R.; Radom-Aizik, S.; Jain, R.; Cooper, D.M.; Khine, M. Respiration Rate and Volume Measurements Using Wearable Strain Sensors. npj Digit. Med. 2019, 2, 8. [Google Scholar] [CrossRef] [PubMed]
- Dinh, T.; Nguyen, T.; Phan, H.P.; Nguyen, N.T.; Dao, D.V.; Bell, J. Stretchable Respiration Sensors: Advanced Designs and Multifunctional Platforms for Wearable Physiological Monitoring. Biosens. Bioelectron. 2020, 166, 112460. [Google Scholar] [CrossRef]
- Shen, S.; Zhou, Q.; Chen, G.; Fang, Y.; Kurilova, O.; Liu, Z.; Li, S.; Chen, J. Advances in Wearable Respiration Sensors. Mater. Today 2024, 72, 140–162. [Google Scholar] [CrossRef]
- Kim, D.; Lee, J.; Park, M.K.; Ko, S.H. Recent Developments in Wearable Breath Sensors for Healthcare Monitoring. Commun. Mater. 2024, 5, 41. [Google Scholar] [CrossRef]
- Vitazkova, D.; Foltan, E.; Kosnacova, H.; Micjan, M.; Donoval, M.; Kuzma, A.; Kopani, M.; Vavrinsky, E. Advances in Respiratory Monitoring: A Comprehensive Review of Wearable and Remote Technologies. Biosensors 2024, 14, 90. [Google Scholar] [CrossRef] [PubMed]
- Hailstone, J.; Kilding, A.E. Reliability and Validity of the ZephyrTM BioHarnessTM to Measure Respiratory Responses to Exercise. Meas. Phys. Educ. Exerc. Sci. 2011, 15, 293–300. [Google Scholar] [CrossRef]
- Kim, J.H.; Roberge, R.; Powell, J.B.; Shafer, A.B.; Jon Williams, W. Measurement Accuracy of Heart Rate and Respiratory Rate during Graded Exercise and Sustained Exercise in the Heat Using the Zephyr BioHarness TM. Int. J. Sports Med. 2013, 34, 497–501. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Zhu, S.H.; Wang, G.H.; Ye, F.; Li, P.Z. Validity and Reliability of Multiparameter Physiological Measurements Recorded by the Equivital LifeMonitor during Activities of Various Intensities. J. Occup. Environ. Hyg. 2013, 10, 78–85. [Google Scholar] [CrossRef] [PubMed]
- Villar, R.; Beltrame, T.; Hughson, R.L. Validation of the Hexoskin Wearable Vest during Lying, Sitting, Standing, and Walking Activities. Appl. Physiol. Nutr. Metab. 2015, 40, 1019–1024. [Google Scholar] [CrossRef] [PubMed]
- Elliot, C.A.; Hamlin, M.J.; Lizamore, C.A. Validity and Reliability of the Hexoskin Wearable Biometric Vest during Maximal Aerobic Power Testing in Elite Cyclists. J. Strength Cond. Res. 2019, 33, 1437–1444. [Google Scholar] [CrossRef] [PubMed]
- Harbour, E.; Lasshofer, M.; Genitrini, M.; Schwameder, H. Enhanced Breathing Pattern Detection during Running Using Wearable Sensors. Sensors 2021, 21, 5606. [Google Scholar] [CrossRef] [PubMed]
- Massaroni, C.; Sacchetti, M.; Romano, C.; Schena, E.; Innocenti, L.; Nicolò, A. The Effects of Different Algorithms on the Performance of a Strain-Based Wearable Device Estimating Respiratory Rate during Cycling Exercise. In Proceedings of the 2023 IEEE International Workshop on Metrology for Industry 4.0 & IoT (MetroInd4.0&IoT), Brescia, Italy, 6–8 June 2023; pp. 142–147. [Google Scholar] [CrossRef]
- Romano, C.; Innocenti, L.; Schena, E.; Sacchetti, M.; Nicolò, A.; Massaroni, C. A Signal Quality Index for Improving the Estimation of Breath-by-Breath Respiratory Rate During Sport and Exercise. IEEE Sens. J. 2023, 23, 31250–31258. [Google Scholar] [CrossRef]
- Massaroni, C.; Nicolò, A.; Girardi, M.; La Camera, A.; Schena, E.; Sacchetti, M.; Silvestri, S.; Taffoni, F. Validation of a Wearable Device and an Algorithm for Respiratory Monitoring during Exercise. IEEE Sens. J. 2019, 19, 4652–4659. [Google Scholar] [CrossRef]
- Antonelli, A.; Guilizzoni, D.; Angelucci, A.; Melloni, G.; Mazza, F.; Stanzi, A.; Venturino, M.; Kuller, D.; Aliverti, A. Comparison between the AirgoTM Device and a Metabolic Cart during Rest and Exercise. Sensors 2020, 20, 3943. [Google Scholar] [CrossRef] [PubMed]
- Gouw, A.H.; Van Guilder, G.P.; Cullen, G.G.; Dalleck, L.C. Is the Tyme Wear Smart Shirt Reliable and Valid at Detecting Personalized Ventilatory Thresholds in Recreationally Active Individuals? Int. J. Environ. Res. Public Health 2022, 19, 1147. [Google Scholar] [CrossRef] [PubMed]



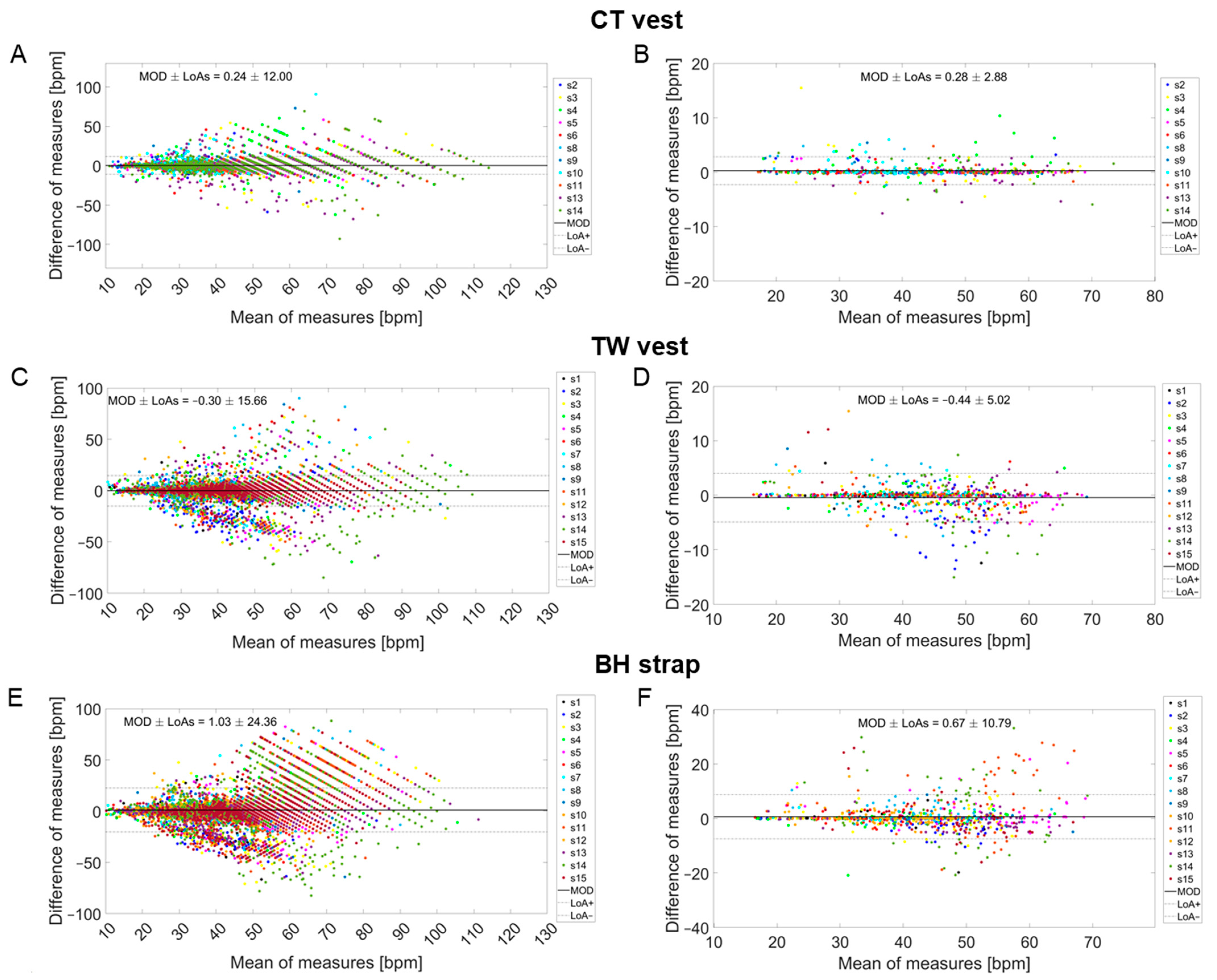
| Breath-by-Breath Analysis | Analysis Based on 30 s Windows | |||||
|---|---|---|---|---|---|---|
| Soccer Player | MOD ± LoAs [bpm] | MAE [bpm] | MAPE [%] | MOD ± LoAs [bpm] | MAE [bpm] | MAPE [%] |
| 1 | −0.11 ± 8.14 | 1.88 | 5.16 | −0.24 ± 3.82 | 0.56 | 1.44 |
| 2 | −1.75 ± 19.32 | 5.67 | 11.81 | −2.62 ± 7.75 | 3.17 | 6.39 |
| 3 | −0.43 ± 17.91 | 4.28 | 9.36 | −0.53 ± 3.82 | 1.25 | 2.98 |
| 4 | 0.19 ± 13.42 | 3.33 | 7.85 | 0.10 ± 3.03 | 1.01 | 2.76 |
| 5 | −0.52 ± 13.12 | 3.37 | 6.14 | −0.69 ± 2.89 | 0.86 | 1.57 |
| 6 | 0.18 ± 11.07 | 2.68 | 7.13 | 0.07 ± 2.79 | 0.66 | 1.66 |
| 7 | 0.08 ± 9.83 | 2.55 | 6.05 | 0.01 ± 2.26 | 0.55 | 1.42 |
| 8 | −0.12 ± 18.25 | 4.66 | 11.95 | 0.05 ± 5.73 | 2.11 | 5.58 |
| 9 | 0.08 ± 10.37 | 2.82 | 6.37 | 0.07 ± 2.63 | 0.51 | 1.70 |
| 11 | −0.44 ± 15.89 | 4.29 | 8.40 | −0.69 ± 3.78 | 1.30 | 3.07 |
| 12 | 0.11 ± 11.10 | 2.78 | 7.51 | 0.13 ± 5.31 | 1.21 | 3.68 |
| 13 | −0.43 ± 19.34 | 5.47 | 10.89 | −0.53 ± 4.83 | 1.74 | 3.28 |
| 14 | −0.94 ± 24.67 | 6.68 | 13.26 | −1.28 ± 8.59 | 3.01 | 6.19 |
| 15 | 0.03 ± 15.48 | 4.00 | 9.16 | 0.01 ± 5.56 | 1.35 | 4.09 |
| Overall | −0.30 ± 15.66 | 3.89 | 8.65 | −0.44 ± 5.02 | 1.38 | 3.27 |
| Breath-by-Breath Analysis | Analysis Based on 30 s Windows | |||||
|---|---|---|---|---|---|---|
| Soccer Player | MOD ± LoAs [bpm] | MAE [bpm] | MAPE [%] | MOD ± LoAs [bpm] | MAE [bpm] | MAPE [%] |
| 2 | 0.20 ± 7.37 | 1.94 | 4.81 | 0.27 ± 1.55 | 0.36 | 1.16 |
| 3 | 0.08 ± 12.97 | 3.75 | 7.32 | 0.28 ± 4.90 | 1.02 | 3.72 |
| 4 | 1.15 ± 17.04 | 4.49 | 10.17 | 1.10 ± 4.30 | 1.35 | 3.23 |
| 5 | 0.23 ± 9.66 | 3.22 | 6.18 | 0.24 ± 1.40 | 0.36 | 1.07 |
| 6 | 0.21 ± 8.62 | 2.39 | 6.35 | 0.10 ± 1.27 | 0.29 | 0.89 |
| 8 | 0.28 ± 8.03 | 2.42 | 6.36 | 0.43 ± 2.26 | 0.64 | 2.24 |
| 9 | 0.16 ± 7.44 | 2.18 | 5.28 | 0.23 ± 1.63 | 0.31 | 1.01 |
| 10 | 0.37 ± 10.02 | 2.83 | 8.06 | 0.53 ± 2.50 | 0.59 | 1.79 |
| 11 | 0.22 ± 10.43 | 3.16 | 6.10 | 0.20 ± 1.75 | 0.47 | 1.01 |
| 13 | −0.31 ± 15.39 | 4.12 | 8.17 | −0.37 ± 3.39 | 1.00 | 2.15 |
| 14 | 0.28 ± 16.51 | 4.36 | 8.54 | 0.16 ± 3.16 | 0.92 | 2.12 |
| Overall | 0.24 ± 12.00 | 3.17 | 7.03 | 0.28 ± 2.88 | 0.66 | 1.85 |
| Breath-by-Breath Analysis | Analysis Based on 30 s Windows | |||||
|---|---|---|---|---|---|---|
| Soccer Player | MOD ± LoAs [bpm] | MAE [bpm] | MAPE [%] | MOD ± LoAs [bpm] | MAE [bpm] | MAPE [%] |
| 1 | −0.05 ± 12.11 | 2.64 | 6.98 | −0.21 ± 5.91 | 0.90 | 2.02 |
| 2 | −1.93 ± 18.16 | 5.23 | 10.47 | −2.44 ± 5.14 | 2.49 | 5.05 |
| 3 | 0.25 ± 28.54 | 8.49 | 17.57 | −0.12 ± 8.28 | 3.01 | 7.42 |
| 4 | 0.13 ± 12.11 | 3.53 | 8.07 | −0.26 ± 6.00 | 1.25 | 3.07 |
| 5 | 2.38 ± 25.97 | 8.19 | 15.74 | 2.15 ± 10.12 | 3.21 | 7.62 |
| 6 | 0.17 ± 17.02 | 4.36 | 10.78 | 0.05 ± 3.51 | 1.25 | 3.68 |
| 7 | 0.19 ± 8.14 | 2.53 | 6.05 | 0.12 ± 1.32 | 0.32 | 0.95 |
| 8 | 2.03 ± 23.37 | 6.76 | 16.81 | 2.26 ± 6.08 | 2.75 | 7.70 |
| 9 | 0.16 ± 13.04 | 3.45 | 7.44 | 0.13 ± 3.71 | 0.87 | 1.94 |
| 10 | 0.31 ± 12.68 | 3.15 | 8.83 | 0.35 ± 2.97 | 0.89 | 2.86 |
| 11 | 7.84 ± 43.16 | 16.98 | 34.30 | 5.53 ± 22.44 | 10.04 | 21.5 |
| 12 | 0.40 ± 13.47 | 3.81 | 9.69 | 0.45 ± 5.07 | 1.30 | 4.01 |
| 13 | −0.62 ± 20.86 | 6.31 | 12.43 | −1.24 ± 4.84 | 2.12 | 4.43 |
| 14 | 2.91 ± 40.73 | 13.62 | 30.78 | 2.93 ± 22.49 | 9.28 | 23.89 |
| 15 | 0.92 ± 32.01 | 9.77 | 23.03 | 0.36 ± 13.94 | 4.54 | 13.4 |
| Overall | 1.03 ± 24.36 | 6.59 | 14.60 | 0.67 ± 10.79 | 2.95 | 7.30 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Innocenti, L.; Romano, C.; Greco, G.; Nuccio, S.; Bellini, A.; Mari, F.; Silvestri, S.; Schena, E.; Sacchetti, M.; Massaroni, C.; et al. Breathing Monitoring in Soccer: Part I—Validity of Commercial Wearable Sensors. Sensors 2024, 24, 4571. https://doi.org/10.3390/s24144571
Innocenti L, Romano C, Greco G, Nuccio S, Bellini A, Mari F, Silvestri S, Schena E, Sacchetti M, Massaroni C, et al. Breathing Monitoring in Soccer: Part I—Validity of Commercial Wearable Sensors. Sensors. 2024; 24(14):4571. https://doi.org/10.3390/s24144571
Chicago/Turabian StyleInnocenti, Lorenzo, Chiara Romano, Giuseppe Greco, Stefano Nuccio, Alessio Bellini, Federico Mari, Sergio Silvestri, Emiliano Schena, Massimo Sacchetti, Carlo Massaroni, and et al. 2024. "Breathing Monitoring in Soccer: Part I—Validity of Commercial Wearable Sensors" Sensors 24, no. 14: 4571. https://doi.org/10.3390/s24144571
APA StyleInnocenti, L., Romano, C., Greco, G., Nuccio, S., Bellini, A., Mari, F., Silvestri, S., Schena, E., Sacchetti, M., Massaroni, C., & Nicolò, A. (2024). Breathing Monitoring in Soccer: Part I—Validity of Commercial Wearable Sensors. Sensors, 24(14), 4571. https://doi.org/10.3390/s24144571











