An Intelligent Hand-Assisted Diagnosis System Based on Information Fusion
Abstract
:1. Introduction
- 1.
- Collected and integrated medical data related to hand function diagnosis to construct a knowledge graph-based hand disease Q&A system. Additionally, the integration of speech recognition technology enhances the system’s applicability in various scenarios, catering to the diverse needs of patients and doctors.
- 2.
- Developed a high-precision and robust hand activity recognition algorithm that meets clinical application standards. This algorithm can accurately assess the functional status of patients’ hands, providing critical support for doctors in diagnosis and treatment.
- 3.
- Constructed an intelligent hand-assisted diagnosis system that integrates the aforementioned Q&A and activity recognition technologies. This system offers intelligent and precise diagnostic support for healthcare professionals.
2. Related Work
2.1. Wearable Sensors
2.2. Visual Diagnostic Assistance
2.3. Medical Question Answering System
3. Methods
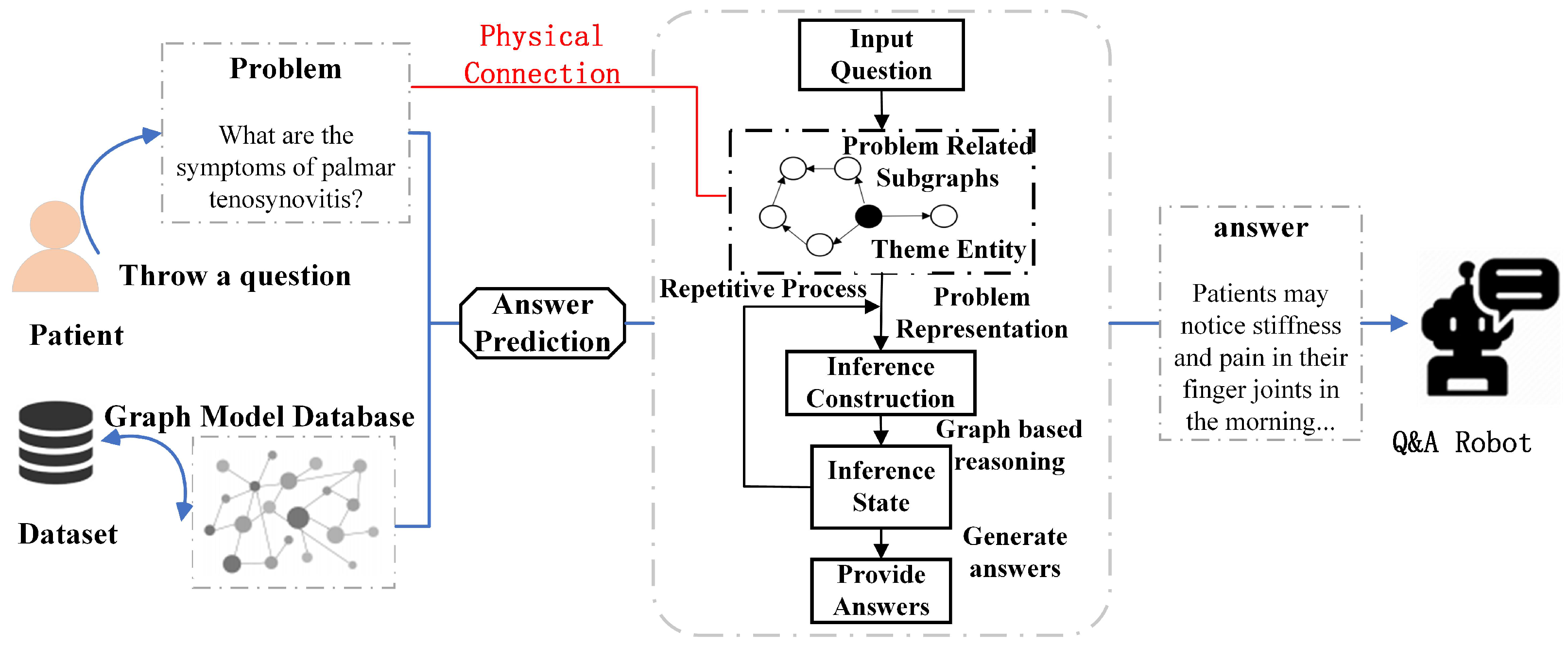
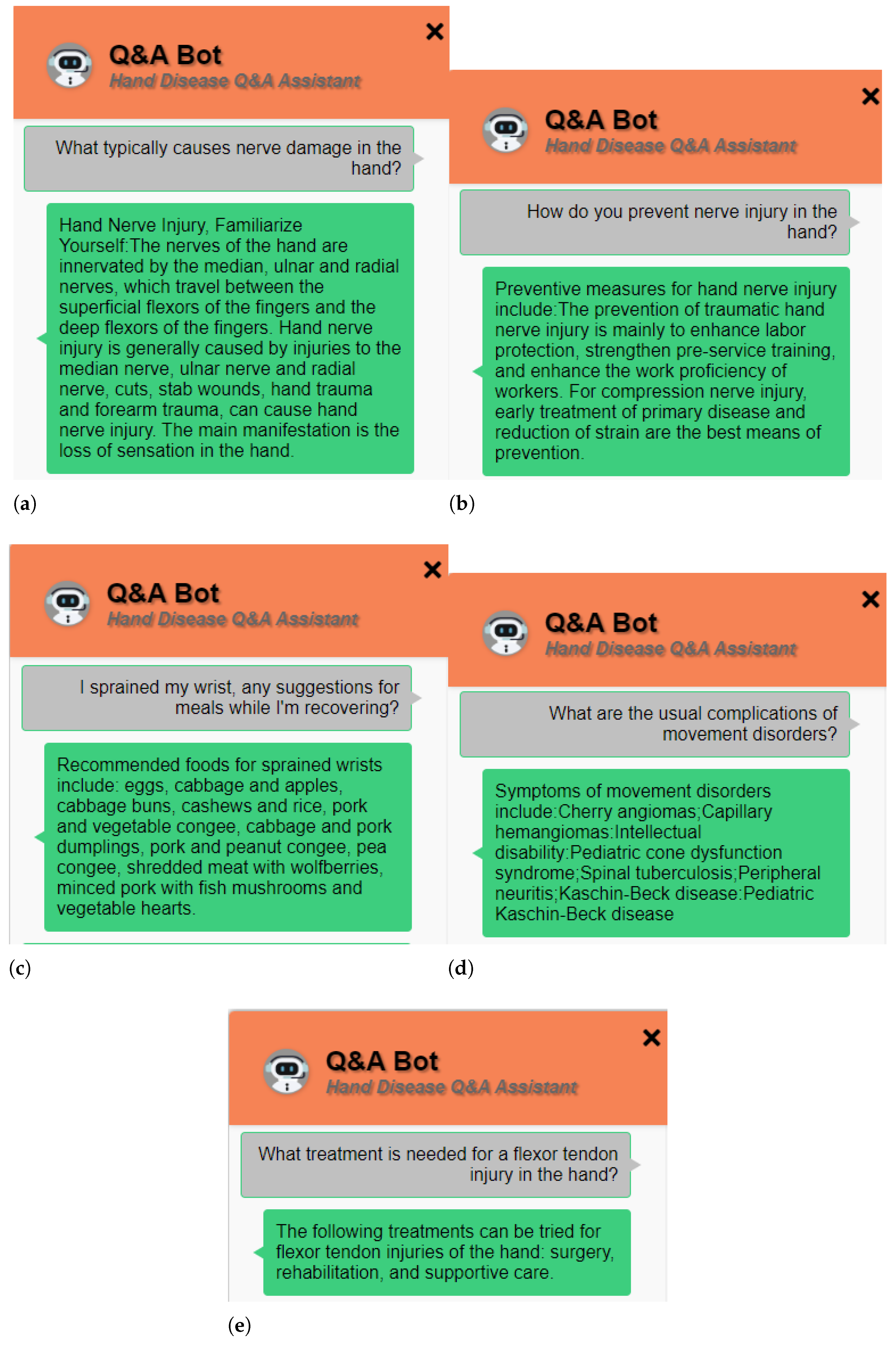
3.1. Establishing a Question-Answering System
Question-Answering Knowledge Base from Information Retrieval
3.2. Knowledge Graph Construction for Question-Answering System
3.2.1. Data Collection and Graph Construction
3.2.2. Question Classification
3.2.3. Knowledge Graph Matching and Resulting Feedback
3.2.4. Interactive UI Development
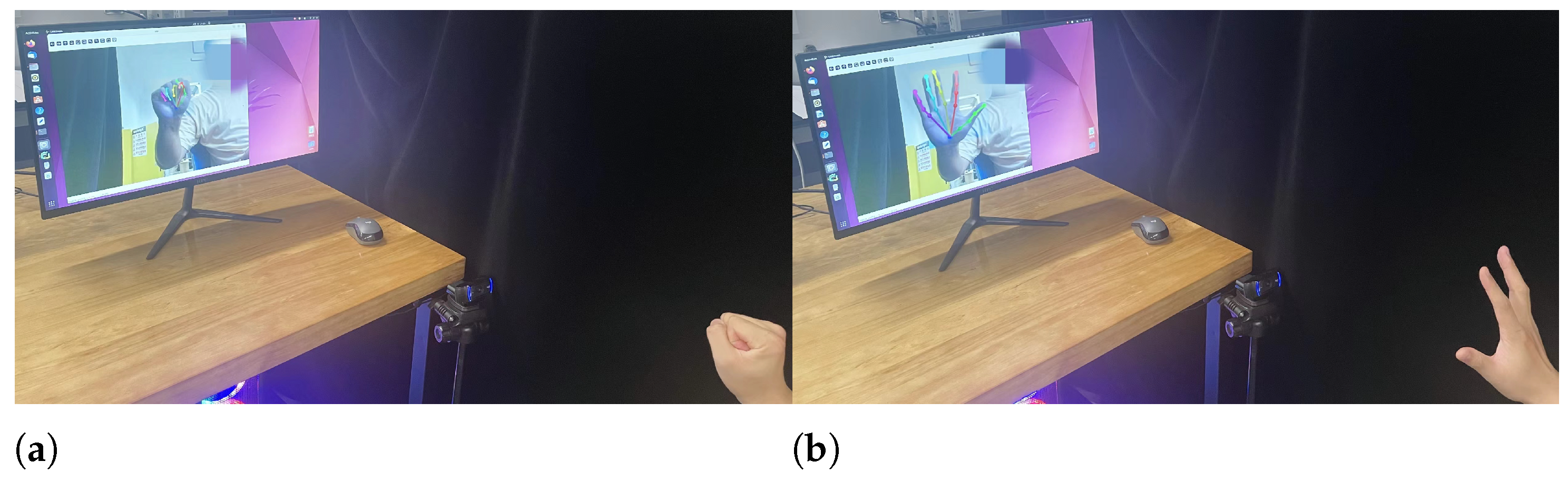
3.3. Establishing a Visual System
3.3.1. Algorithm Optimization
3.3.2. Algorithm Extension
4. Hand Mobility Test
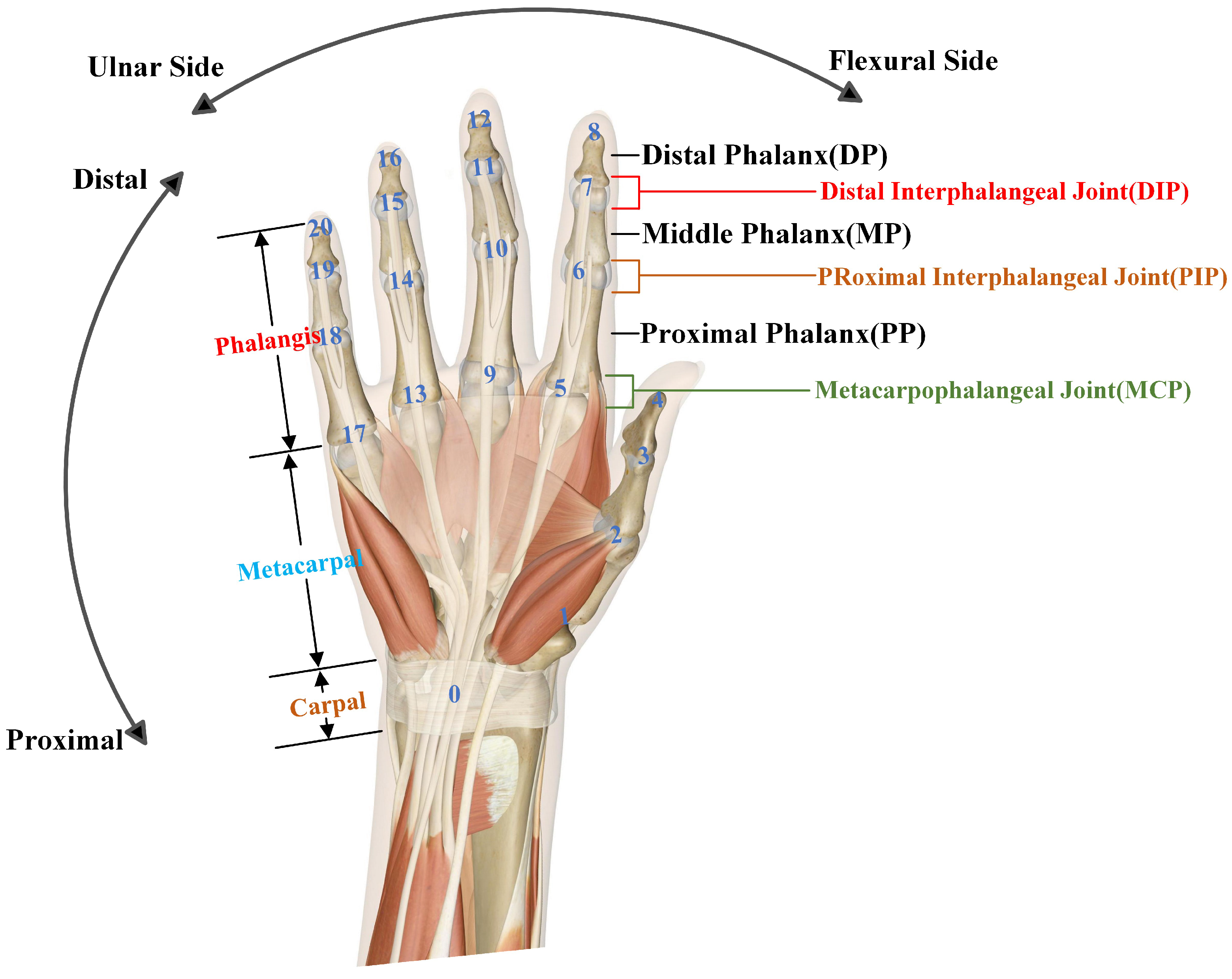
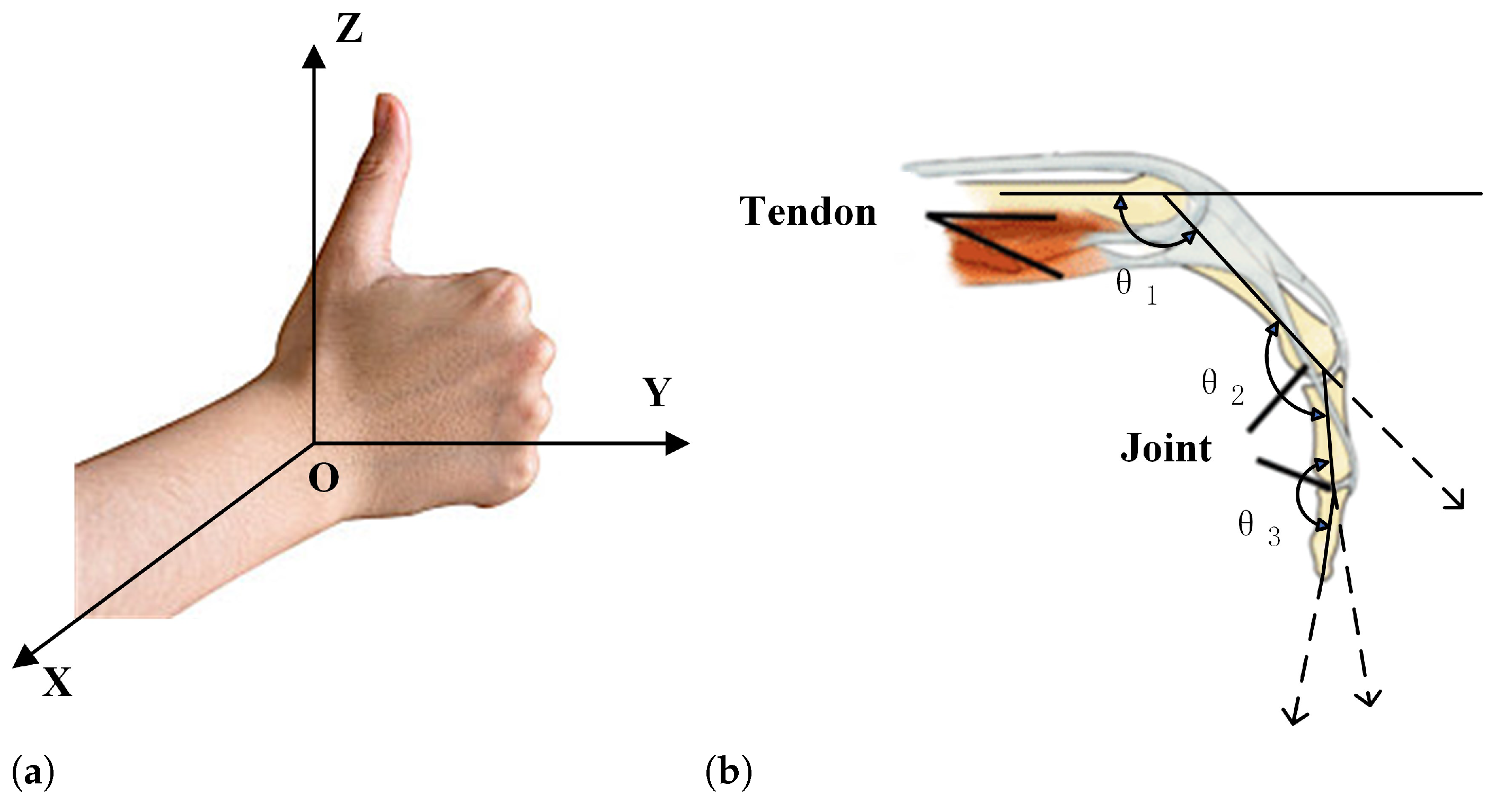
4.1. Hand Kinematics Analysis
4.2. Standard Evaluation of Hand Movements
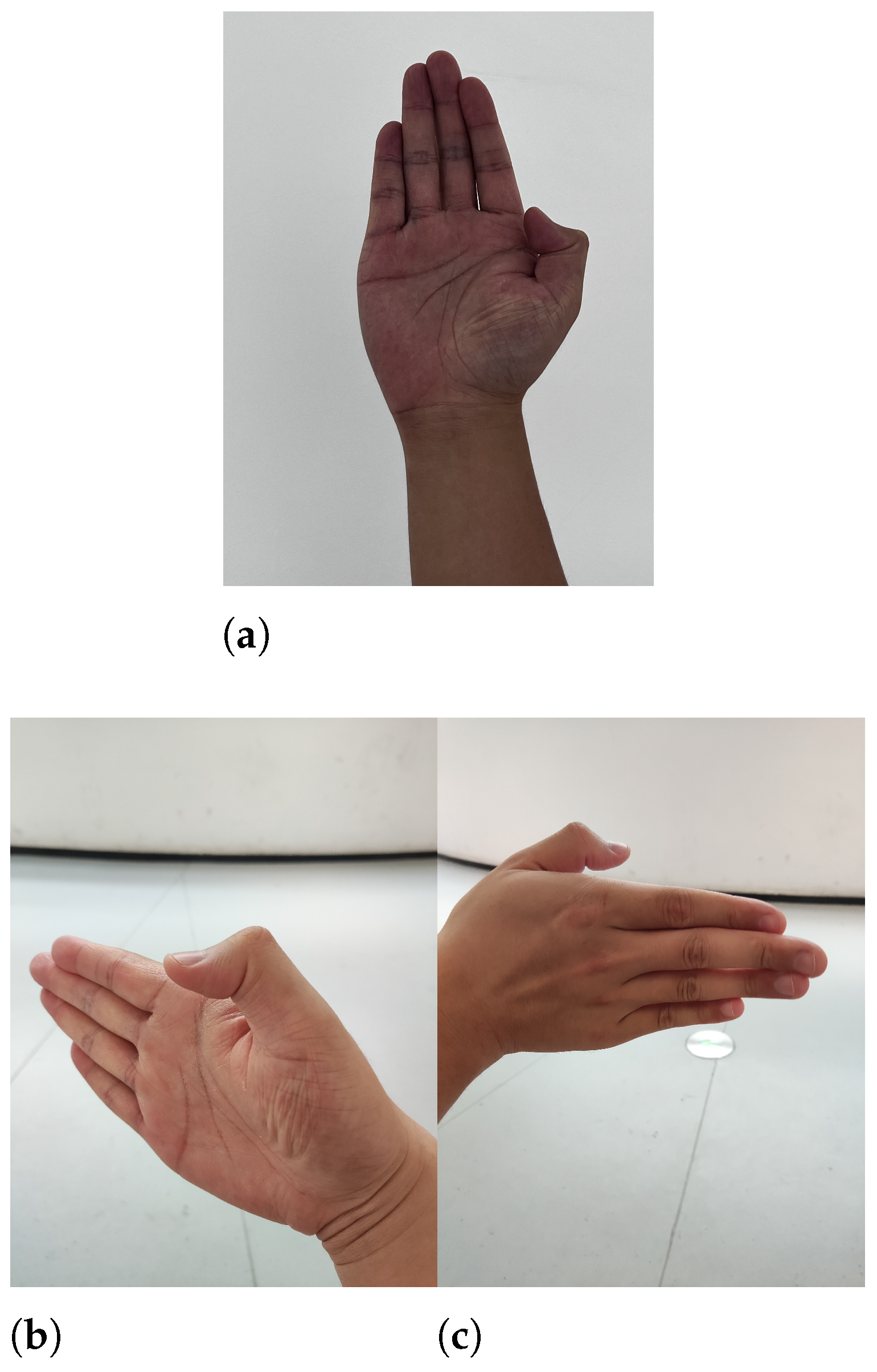
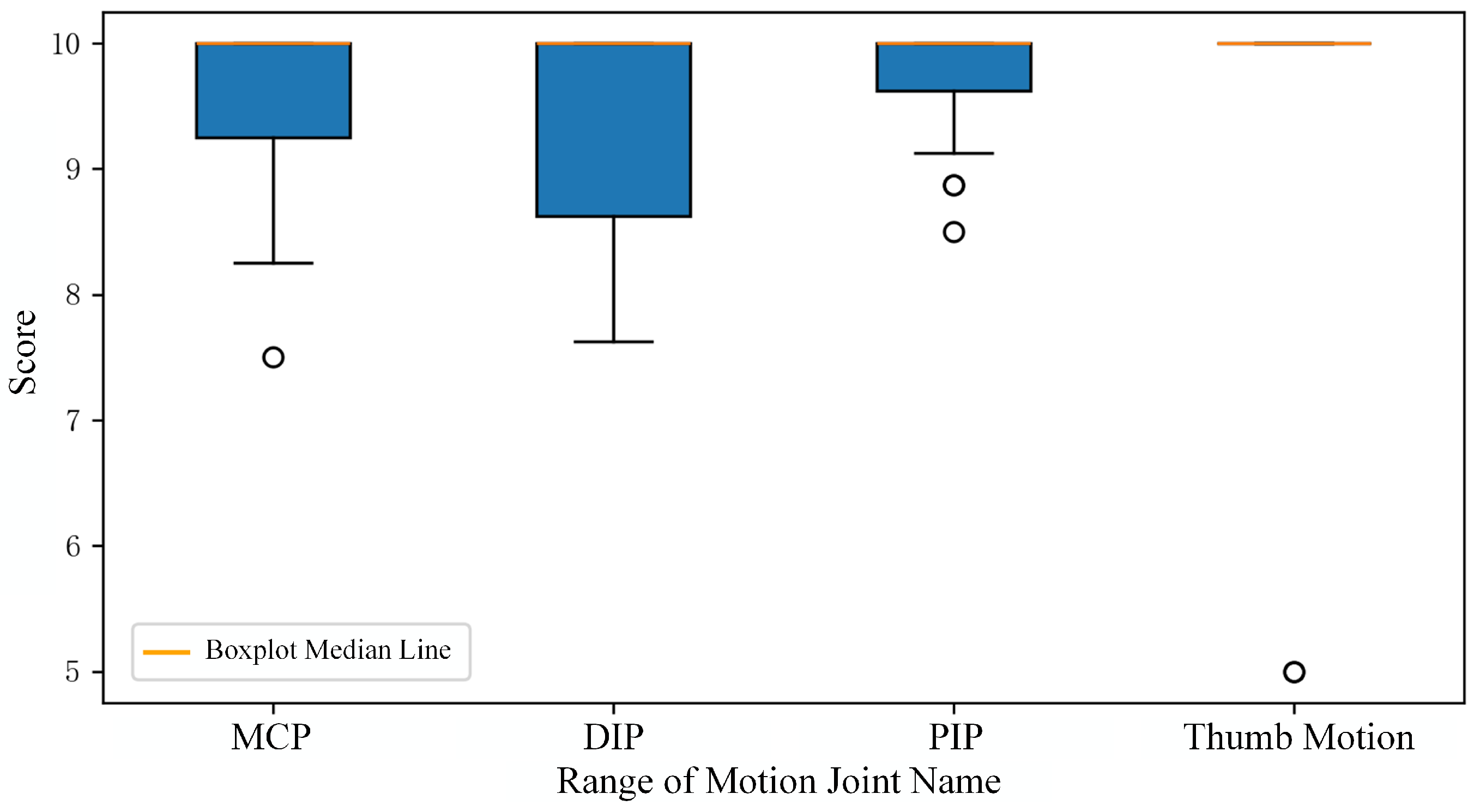
4.3. Single-Frame Image Hand Movement Reliability Test
- Occlusion and Complexity: In complex scenarios involving occlusion, the algorithm may rely heavily on prior models for thumb localization, introducing a degree of arbitrariness and uncertainty.
- Unique Thumb Biomechanics: The thumb possesses a wider range of motion and a distinct joint structure compared to other fingers. Its movement trajectory and posture variations differ significantly, potentially hindering the algorithm’s ability to fully learn and comprehend its unique motion characteristics.
4.4. Sequential Frame Acquisition Hand Movement Reliability Test
4.5. Reliability Testing of Interactive Question-Answering System
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ma, Q.; Li, R.; Wang, L.; Yin, P.; Wang, Y.; Yan, C.; Ren, Y.; Qian, Z.; Vaughn, M.G.; McMillin, S.E.; et al. Temporal trend and attributable risk factors of stroke burden in China, 1990–2019: An analysis for the Global Burden of Disease Study 2019. Lancet Public Health 2021, 6, e897–e906. [Google Scholar] [CrossRef]
- Langhorne, P.; Bernhardt, J.; Kwakkel, G. Stroke rehabilitation. Lancet 2011, 377, 1693–1702. [Google Scholar] [CrossRef]
- Zheng, Y.; Peng, Y.; Wang, G.; Liu, X.; Dong, X.; Wang, J. Development and evaluation of a sensor glove for hand function assessment and preliminary attempts at assessing hand coordination. Measurement 2016, 93, 1–12. [Google Scholar] [CrossRef]
- Lee, Y.; Park, H.S. Design Optimization of a Soft Robotic Rehabilitation Glove Based on Finger Workspace Analysis. Biomimetics 2024, 9, 172. [Google Scholar] [CrossRef]
- Rieger, C.; Desai, J. A Preliminary Study to Design and Evaluate Pneumatically Controlled Soft Robotic Actuators for a Repetitive Hand Rehabilitation Task. Biomimetics 2022, 7, 139. [Google Scholar] [CrossRef]
- Li, F.; Chen, J.; Ye, G.; Dong, S.; Gao, Z.; Zhou, Y. Soft robotic glove with sensing and force feedback for rehabilitation in virtual reality. Biomimetics 2023, 8, 83. [Google Scholar] [CrossRef]
- Li, F.; Chen, J.; Zhou, Z.; Xie, J.; Gao, Z.; Xiao, Y.; Dai, P.; Xu, C.; Wang, X.; Zhou, Y. Lightweight soft robotic glove with whole-hand finger motion tracking for hand rehabilitation in virtual reality. Biomimetics 2023, 8, 425. [Google Scholar] [CrossRef]
- Fleischer, C.; Wege, A.; Kondak, K.; Hommel, G. Application of EMG signals for controlling exoskeleton robots: Biomedizinische Technik. Biomed. Tech. 2006, 51, 314–319. [Google Scholar] [CrossRef]
- Tigrini, A.; Ranaldi, S.; Verdini, F.; Mobarak, R.; Scattolini, M.; Conforto, S.; Schmid, M.; Burattini, L.; Gambi, E.; Fioretti, S.; et al. Intelligent Human–Computer Interaction: Combined Wrist and Forearm Myoelectric Signals for Handwriting Recognition. Bioengineering 2024, 11, 458. [Google Scholar] [CrossRef]
- Tigrini, A.; Verdini, F.; Scattolini, M.; Barbarossa, F.; Burattini, L.; Morettini, M.; Fioretti, S.; Mengarelli, A. Handwritten digits recognition from sEMG: Electrodes location and feature selection. IEEE Access 2023, 11, 58006–58015. [Google Scholar] [CrossRef]
- Schabowsky, C.N.; Godfrey, S.B.; Holley, R.J.; Lum, P.S. Development and pilot testing of HEXORR: Hand EXOskeleton Rehabilitation Robot. J. NeuroEng. Rehabil. 2010, 7, 36. [Google Scholar] [CrossRef]
- Chiri, A.; Vitiello, N.; Giovacchini, F.; Roccella, S.; Vecchi, F.; Carrozza, M.C. Mechatronic Design and Characterization of the Index Finger Module of a Hand Exoskeleton for Post-Stroke Rehabilitation. IEEE/ASME Trans. Mechatron. 2012, 17, 884–894. [Google Scholar] [CrossRef]
- Cheng, L.; Chen, M.; Li, Z. Design and Control of a Wearable Hand Rehabilitation Robot. IEEE Access 2018, 6, 74039–74050. [Google Scholar] [CrossRef]
- Fu, Y.; Zhang, Q.; Zhang, F.; Gan, Z. Design and development of a hand rehabilitation robot for patient-cooperative therapy following stroke. In Proceedings of the 2011 IEEE International Conference on Mechatronics and Automation, Beijing, China, 7–10 August 2011; pp. 112–117. [Google Scholar]
- Guo, K.; Lu, J.; Liu, C.; Yang, H. Development, Research, Optimization and Experiment of Exoskeleton Robot for Hand Rehabilitation Training. Appl. Sci. 2022, 12, 10580. [Google Scholar] [CrossRef]
- Gu, X.; Zhang, Y.; Sun, W.; Bian, Y.; Kristensson, P.O. Dexmo: An Inexpensive and Lightweight Mechanical Exoskeleton for Motion Capture and Force Feedback in VR. In Proceedings of the CHI’16: CHI Conference on Human Factors in Computing Systems, San Jose, CA, USA, 7–12 May 2016; ACM: New York, NY, USA, 2016. [Google Scholar]
- Polygerinos, P.; Galloway, K.C.; Savage, E.; Herman, M.; O’Donnell, K.; Walsh, C.J. Soft robotic glove for hand rehabilitation and task specific training. In Proceedings of the 2015 IEEE International Conference on Robotics and Automation (ICRA), Seattle, WA, USA, 26–30 May 2015; pp. 2913–2919. [Google Scholar]
- Yap, H.K.; Kamaldin, N.; Lim, J.H.; Nasrallah, F.A.; Goh, J.C.H.; Yeow, C. A Magnetic Resonance Compatible Soft Wearable Robotic Glove for Hand Rehabilitation and Brain Imaging. IEEE Trans. Neural Syst. Rehabil. Eng. 2017, 25, 782–793. [Google Scholar] [CrossRef]
- Bützer, T.L.; Lambercy, O.; Arata, J.; Gassert, R. Fully Wearable Actuated Soft Exoskeleton for Grasping Assistance in Everyday Activities. Soft Robot. 2020, 8, 128–143. [Google Scholar] [CrossRef]
- Kang, B.B.; Choi, H.; Lee, H.; Cho, K.J. Exo-Glove Poly II: A Polymer-Based Soft Wearable Robot for the Hand with a Tendon-Driven Actuation System. Soft Robot. 2019, 6, 214–227. [Google Scholar] [CrossRef]
- Kim, D.H.; Lee, Y.; Park, H. Bioinspired High-Degrees of Freedom Soft Robotic Glove for Restoring Versatile and Comfortable Manipulation. Soft Robot. 2021, 9, 734–744. [Google Scholar] [CrossRef]
- Lai, J.; Song, A.; Shi, K.; Ji, Q.; Lu, Y.; Li, H. Design and Evaluation of a Bidirectional Soft Glove for Hand Rehabilitation-Assistance Tasks. IEEE Trans. Med. Robot. Bionics 2023, 5, 730–740. [Google Scholar]
- Chen, X.; Gong, L.; Wei, L.; Yeh, S.C.; Xu, L.D.; Zheng, L.; Zou, Z. A Wearable Hand Rehabilitation System with Soft Gloves. IEEE Trans. Ind. Inform. 2021, 17, 943–952. [Google Scholar] [CrossRef]
- Deng, L.; Shen, Y.; Hong, Y.; Dong, Y.; He, X.; Yuan, Y.; Li, Z.; Ding, H. Sen-Glove: A Lightweight Wearable Glove for Hand Assistance with Soft Joint Sensing. In Proceedings of the 2022 International Conference on Robotics and Automation (ICRA), Philadelphia, PA, USA, 23–27 May 2022; pp. 5170–5175. [Google Scholar]
- Potter, L.E.; Araullo, J.; Carter, L. The Leap Motion controller: A view on sign language. In Proceedings of the Australasian Computer-Human Interaction Conference, Adelaide, Australia, 25–29 November 2013. [Google Scholar]
- Keselman, L.; Woodfill, J.I.; Grunnet-Jepsen, A.; Bhowmik, A. Intel RealSense Stereoscopic Depth Cameras. arXiv 2017, arXiv:1705.05548. [Google Scholar]
- Zhang, F.; Bazarevsky, V.; Vakunov, A.; Tkachenka, A.; Sung, G.; Chang, C.L.; Grundmann, M. MediaPipe Hands: On-device Real-time Hand Tracking. arXiv 2020, arXiv:2006.10214. [Google Scholar]
- Metcalf, C.D.; Robinson, R.; Malpass, A.J.; Bogle, T.P.; Dell, T.A.; Harris, C.; Demain, S.H. Markerless Motion Capture and Measurement of Hand Kinematics: Validation and Application to Home-Based Upper Limb Rehabilitation. IEEE Trans. Biomed. Eng. 2013, 60, 2184–2192. [Google Scholar] [CrossRef]
- Zestas, O.N.; Soumis, D.N.; Kyriakou, K.I.D.; Seklou, K.; Tselikas, N.D. A computer-vision based hand rehabilitation assessment suite. AEU Int. J. Electron. Commun. 2023, 169, 154762. [Google Scholar] [CrossRef]
- Sucar, L.E.; Luis, R.; Leder, R.S.; Hernández, J.; Sánchez, I. Gesture therapy: A vision-based system for upper extremity stroke rehabilitation. In Proceedings of the 2010 Annual International Conference of the IEEE Engineering in Medicine and Biology, Buenos Aires, Argentina, 31 August–4 September 2010; pp. 3690–3693. [Google Scholar]
- Zariffa, J.; Steeves, J.D. Computer vision-based classification of hand grip variations in neurorehabilitation. In Proceedings of the 2011 IEEE International Conference on Rehabilitation Robotics, Zurich, Switzerland, 29 June–1 July 2011; pp. 1–4. [Google Scholar]
- Huang, X.; Zhang, J.; Li, D.; Li, P. Knowledge Graph Embedding Based Question Answering. In Proceedings of the Twelfth ACM International Conference on Web Search and Data Mining, Melbourne, VIC, Australia, 11–15 February 2019. [Google Scholar]
- Luo, K.; Lin, F.; Luo, X.; Zhu, K. Knowledge Base Question Answering via Encoding of Complex Query Graphs. In Proceedings of the 2018 Conference on Empirical Methods in Natural Language Processing, Brussels, Belgium, 31 October–4 November 2018. [Google Scholar]
- Available online: https://www.xywy.com/ (accessed on 1 June 2024).
- Li, H.; Chen, P.P.K.; Zhou, Y. 3D Hand Mesh Recovery from Monocular RGB in Camera Space. arXiv 2024, arXiv:2405.07167. [Google Scholar]
- Zimmermann, C.; Ceylan, D.; Yang, J.; Russell, B.C.; Argus, M.; Brox, T. FreiHAND: A Dataset for Markerless Capture of Hand Pose and Shape From Single RGB Images. In Proceedings of the 2019 IEEE/CVF International Conference on Computer Vision (ICCV), Seoul, Republic of Korea, 27 October–2 November 2019; pp. 813–822. [Google Scholar]
- Reis, D.; Kupec, J.; Hong, J.; Daoudi, A. Real-Time Flying Object Detection with YOLOv8. arXiv 2023, arXiv:2305.09972. [Google Scholar]
- Emerson, E.T.; Krizek, T.J.; Greenwald, D.P. Anatomy, physiology, and functional restoration of the thumb. Ann. Plast. Surg. 1996, 36, 180–191. [Google Scholar] [CrossRef]
- Pan, D.; Gu, Y.; Shi, D.; Shou, K. Trial Standards for Upper Limb Function Evaluation by the Chinese Association of Hand Surgery. Chin. J. Hand Surg. 2000, 16, 130–135. [Google Scholar]
- Gladstone, D.J.; Danells, C.; Black, S.E. The Fugl-Meyer Assessment of Motor Recovery after Stroke: A Critical Review of Its Measurement Properties. Neurorehabilit. Neural Repair 2002, 16, 232–240. [Google Scholar] [CrossRef]
- Cave, E.F.; Roberts, S.M. A method for measuring and recording joint function. J. Bone Joint Surg. 1936, 18, 455–465. [Google Scholar]
- Lü, L.; Yang, J.; Gu, F.; Fan, J.; Wang, C.; Zhu, Q.; Liu, X. Accuracy of key point matrix technology based contactless automatic measurement for joint motion of hand. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi Zhongguo Xiufu Chongjian Waike Zazhi Chin. J. Reparative Reconstr. Surg. 2022, 36, 540–547. [Google Scholar]
- Houston, A.; Walters, V.; Corbett, T.; Coppack, R. Evaluation of a multi-sensor Leap Motion setup for biomechanical motion capture of the hand. J. Biomech. 2021, 127, 110713. [Google Scholar] [CrossRef] [PubMed]




| Method | Advantages | Limitations |
|---|---|---|
| Wearable Sensors | Precise measurement of joint angles and positions | Not suitable for patients with severe hand impairments; fixed pattern, unable to adapt to multiple situations |
| Visual Diagnostic Assistance | Low-cost, stable, no restriction on hand flexibility, no data drift | Lack of targeted design for clinical scenarios; self-occlusion and other issues may lead to a decrease in accuracy |
| Medical Question-Answering System | More precise in answering professional medical questions than search engines; aids subjective understanding of patient symptoms and living impairments | Currently limited coverage for hand diseases |
| Entity Type | Meaning | Example |
|---|---|---|
| name | Disease Name | Tendon sheath cyst |
| desc | Disease Introduction | Tendon sheath cyst refers to an internal adhesive that occurs near ... |
| cause | Disease Etiology | The disease is more common in the back of the wrist and foot ... |
| prevention | Preventive Measures | Tendon sheath cysts pay attention to rest in the affected area ... |
| cure_lasttime | Treatment Cycle | 1–3 weeks |
| cure_way | Treatment Methods | Surgical therapy, rehabilitation therapy, supportive therapy |
| cured_probe | Cure Probability | 80% |
| easy_get | Susceptible Population | More common in young and middle-aged people |
| Entity Type | Entity Quantity | Example |
|---|---|---|
| Department | 51 | Rehabilitation department; dermatology |
| Disease | 1805 | Compression of the dorsal scapular nerve; tendon sheath cyst |
| Drug | 10 | Da Yue Jing Wan; dexamethasone sodium phosphate injection |
| Food | 2606 | Stewed lamb with persimmons; tofu and seafood soup |
| Producer | 22 | Cephalosporin; levofloxacin tablets |
| Total | 4494 | Approximately 45,000 entity level |
| Entity Type | Entity Quantity | Example |
|---|---|---|
| acompany_with | 1063 | <tenosynovitis, comorbidities, purulent dactylitis> |
| belongs_to | 1840 | <Renault’s disease, belongs to, rheumatic immune disease> |
| do_eat | 4686 | <Hand flexor tendon injury, recommended to eat, cashew> |
| drugs_of | 22 | <Renqing Mangjue, on sale, Ganlu Renqing Mangjue> |
| no_eat | 4692 | <Achilles tendinitis, avoid eating, chicken wings> |
| recommand_drug | 10 | <Thallium poisoning, recommended medication, renqingmangjue> |
| recommand_eat | 22 | <Recommended recipe for distal fracture of torso bone, fried eggplant with egg> |
| Total | 20,828 | Approximately 21,000 entity level |
| Activity Name | Activity Standard | Score |
|---|---|---|
| MCP Flexion and Extension | °–° | 7.5~10 |
| °–° | 5~7.5 | |
| °–° | 2.5~5 | |
| <° | 0~2.5 | |
| PIP Flexion and Extension | °–° | |
| °–° | ||
| °–° | ||
| <° | ||
| DIP Flexion and Extension | °–° | 7.5~10 |
| °–° | 5~7.5 | |
| °–° | 2.5~5 | |
| <° | 0~2.5 | |
| Thumb Opposition | can | 10 |
| hard | 5 | |
| can’t | 0 | |
| Thumb Active Range of Motion (AROM) | >° | 10 |
| <° | 5 | |
| Stiffness | 0 |
| Activity State | Thumb DIP | Thumb MCP | Index DIP | Index PIP | Index MCP |
|---|---|---|---|---|---|
| Extension | 5.3 | 3.7 | 2.8 | 3.3 | 4.1 |
| Flexion | 29.7 | 4.8 | 7.8 | 6.8 | 8.0 |
| Activity State | Middle DIP | Middle PIP | Middle MCP | Ring DIP | Ring PIP |
| Extension | 3.8 | 4.8 | 5.2 | 5.1 | 3.6 |
| Flexion | 7.0 | 7.8 | 7.5 | 5.9 | 5.6 |
| Activity State | Ring MCP | Little DIP | Little PIP | Little MCP | |
| Extension | 3.9 | 2.7 | 4.0 | 3.3 | |
| Flexion | 11.0 | 6.3 | 10.6 | 6.9 |
| Viewpoint Positions | Angular Error |
|---|---|
| Main Experiment Viewpoint | |
| Comparative Viewpoint 1 | |
| Comparative Viewpoint 2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, H.; Zhou, Y. An Intelligent Hand-Assisted Diagnosis System Based on Information Fusion. Sensors 2024, 24, 4745. https://doi.org/10.3390/s24144745
Li H, Zhou Y. An Intelligent Hand-Assisted Diagnosis System Based on Information Fusion. Sensors. 2024; 24(14):4745. https://doi.org/10.3390/s24144745
Chicago/Turabian StyleLi, Haonan, and Yitong Zhou. 2024. "An Intelligent Hand-Assisted Diagnosis System Based on Information Fusion" Sensors 24, no. 14: 4745. https://doi.org/10.3390/s24144745






