Experimental Validation of Realistic Measurement Setup for Quantitative UWB-Guided Hyperthermia Temperature Monitoring
Abstract
:1. Introduction
2. Materials and Methods
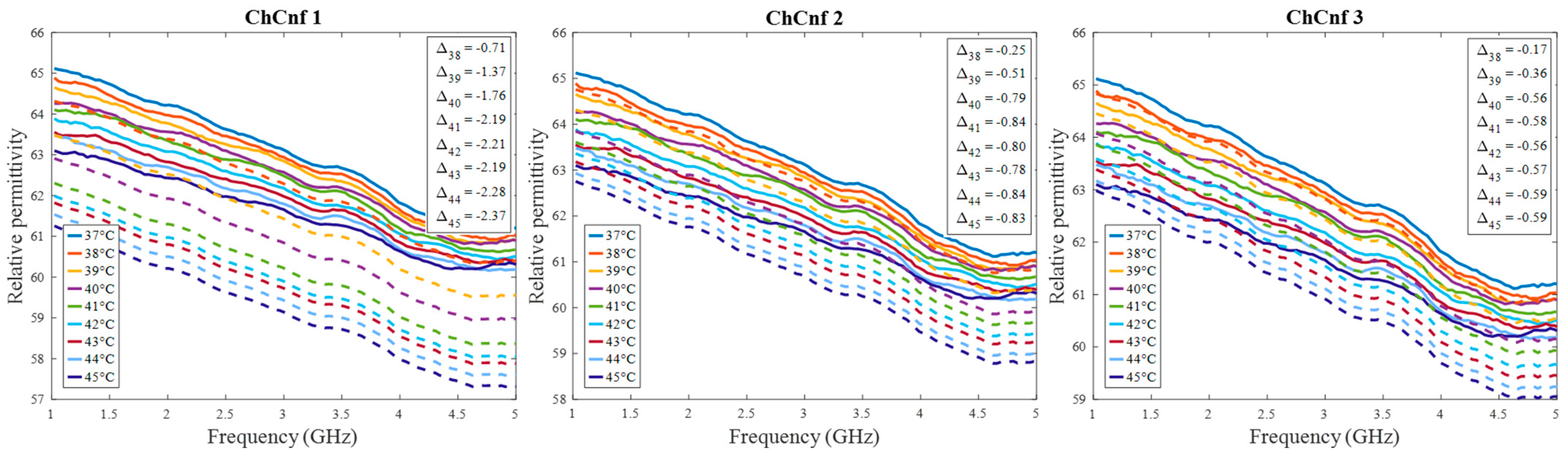
2.1. Frequency and Temperature Dependent Dielectric Properties
2.2. Methodology
2.3. Signal Processing
2.4. Microwave Imaging Algorithms
2.5. Tumor Temperature Estimation
2.6. Measurement Setup and Measurements
2.6.1. Ultra-Wideband Radar
2.6.2. Antennas and Antenna Arrangements
2.6.3. Phantom, Tissue Mimicking Materials, and Measurement Setup
3. Results
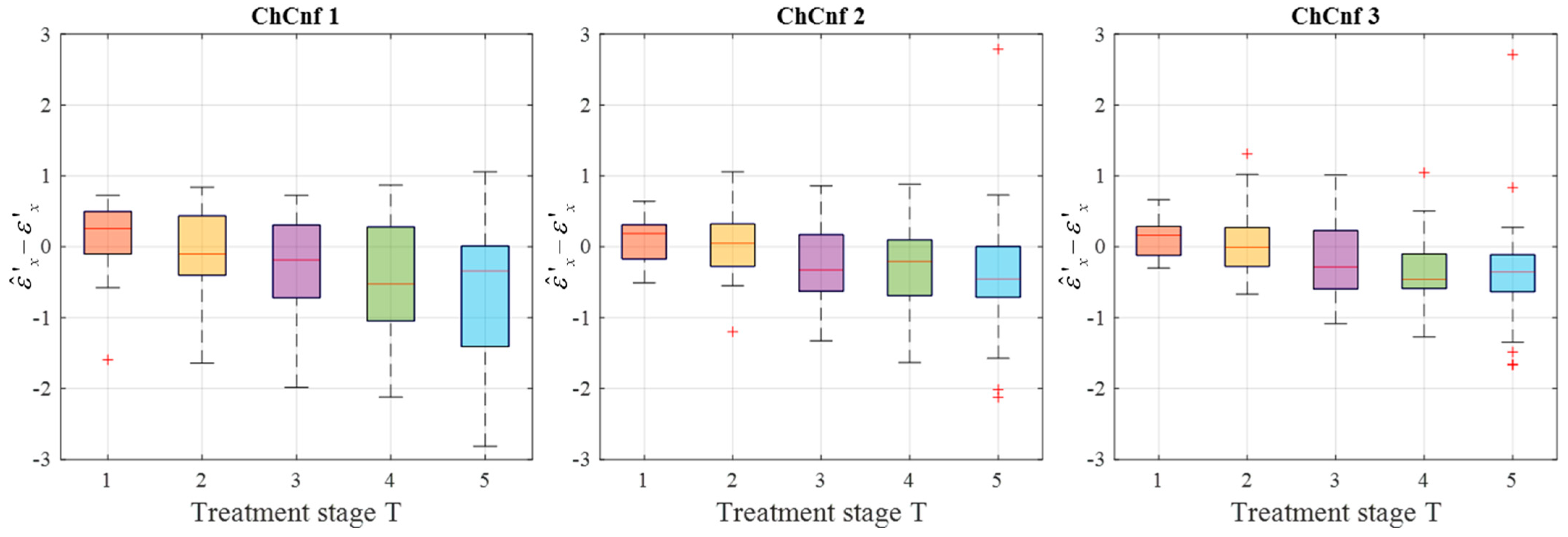
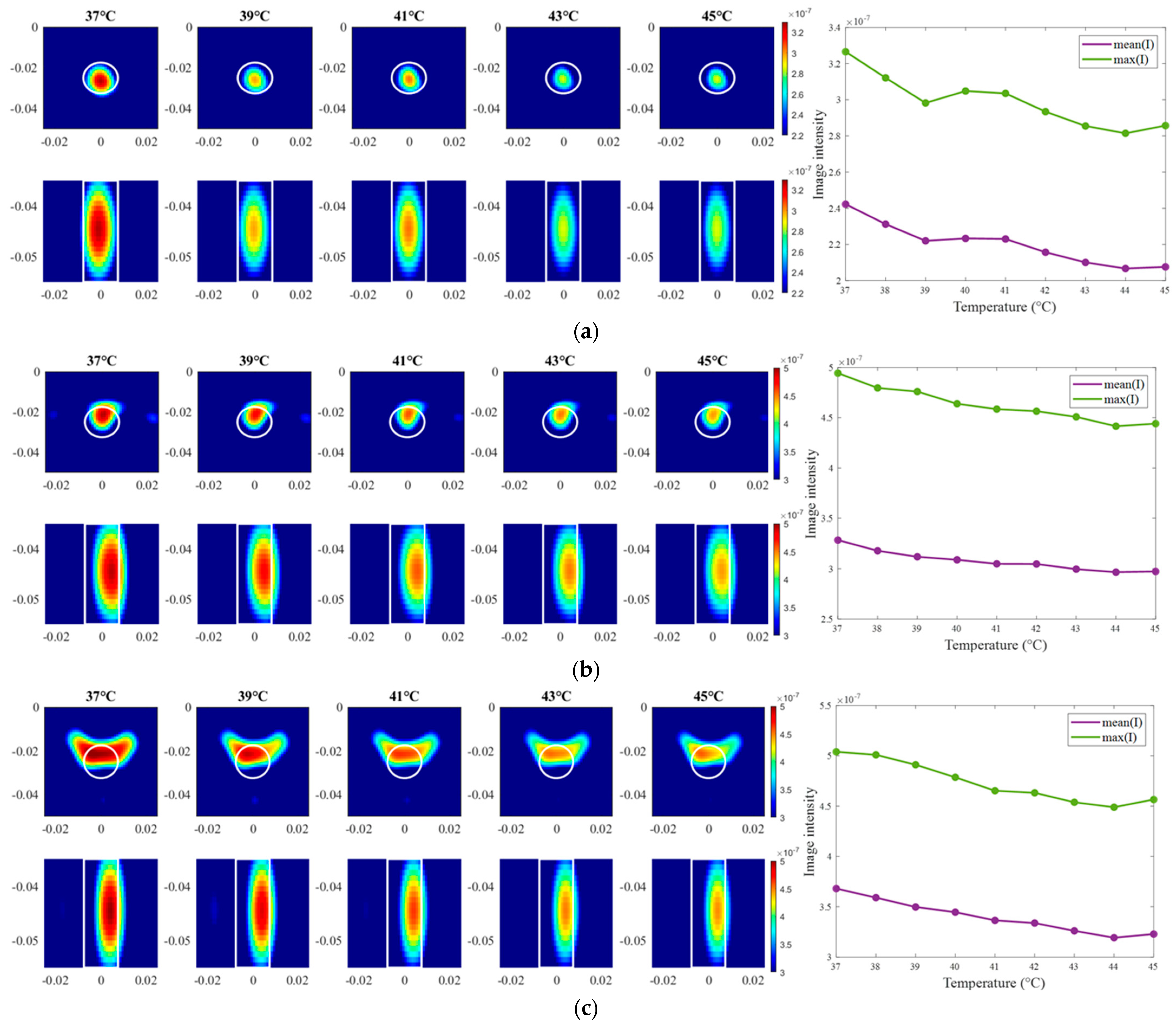
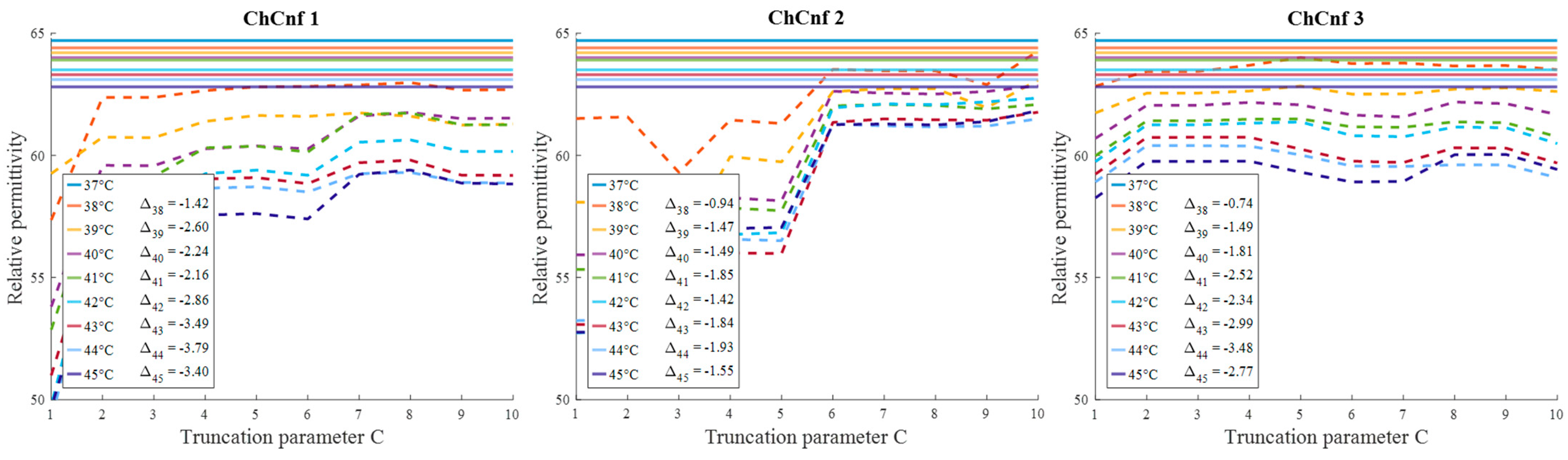
3.1. Imaging and Estimation of the Manually Changed Permittivity
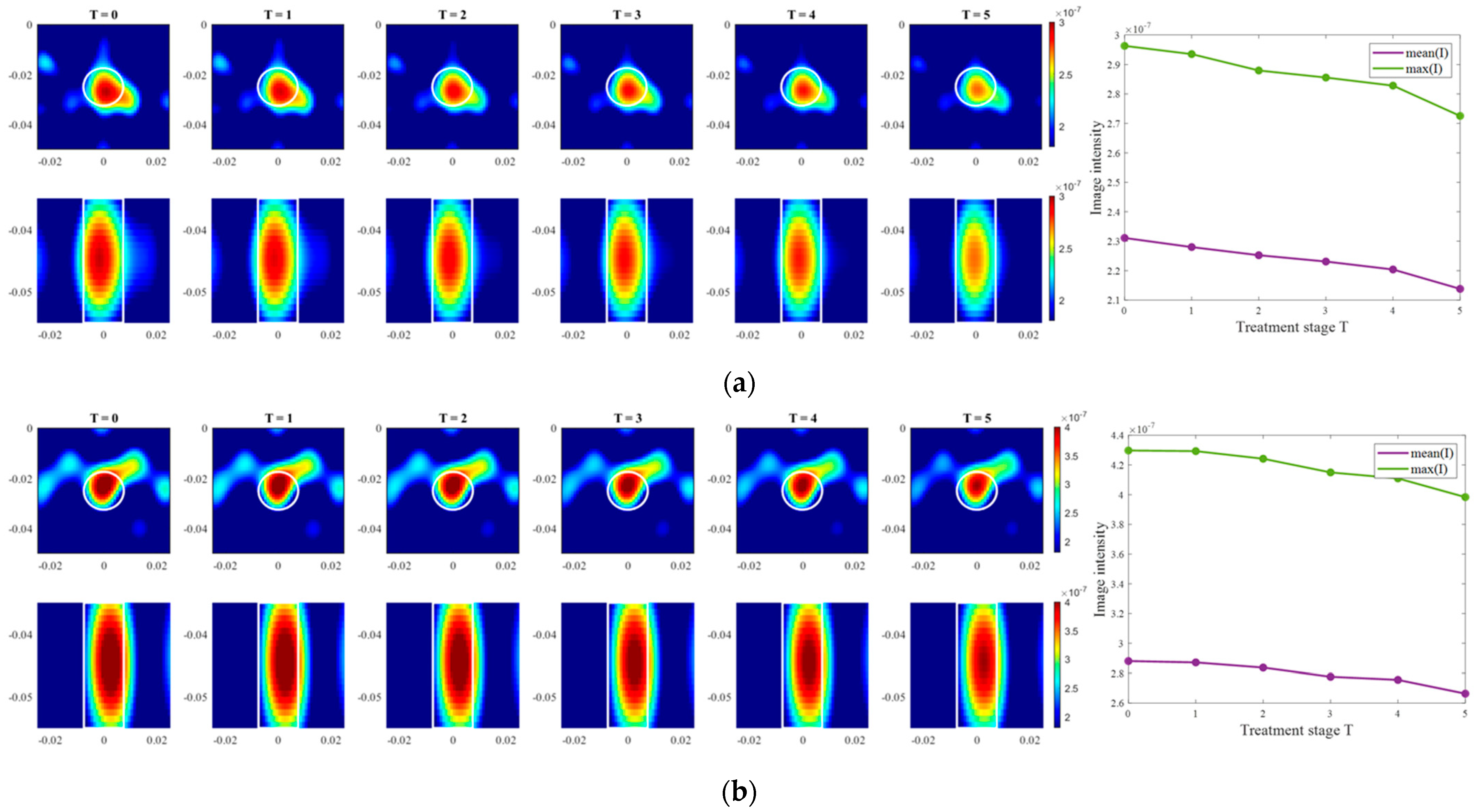
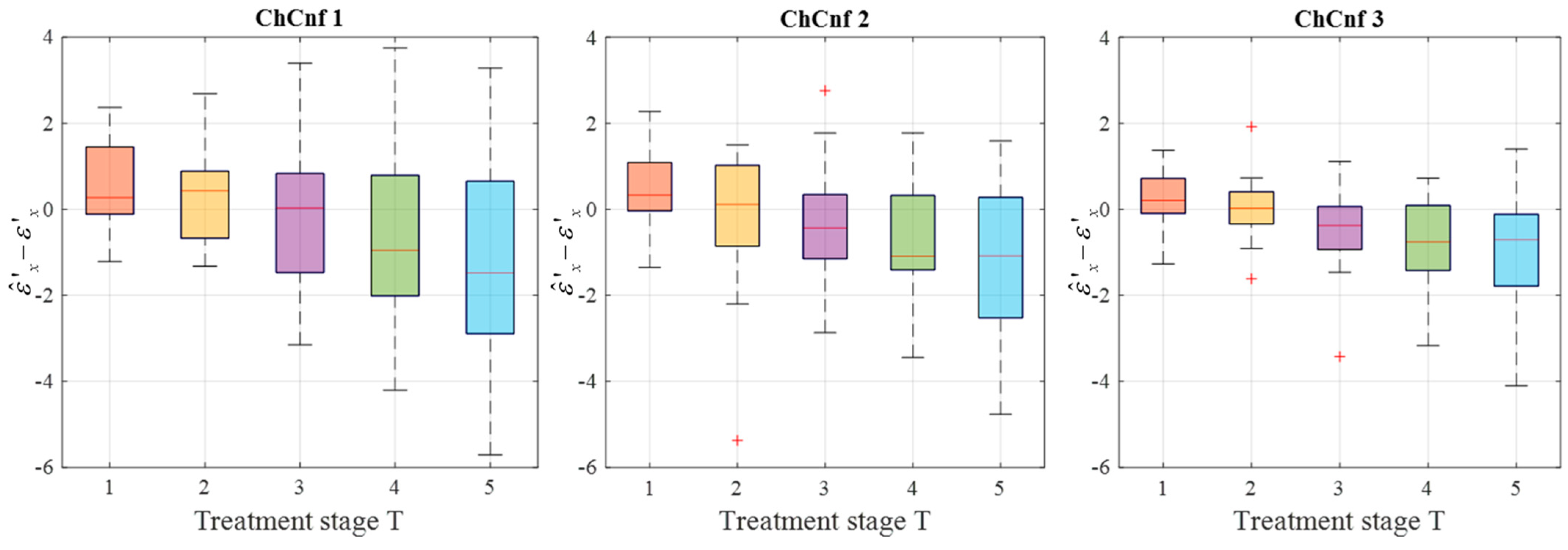
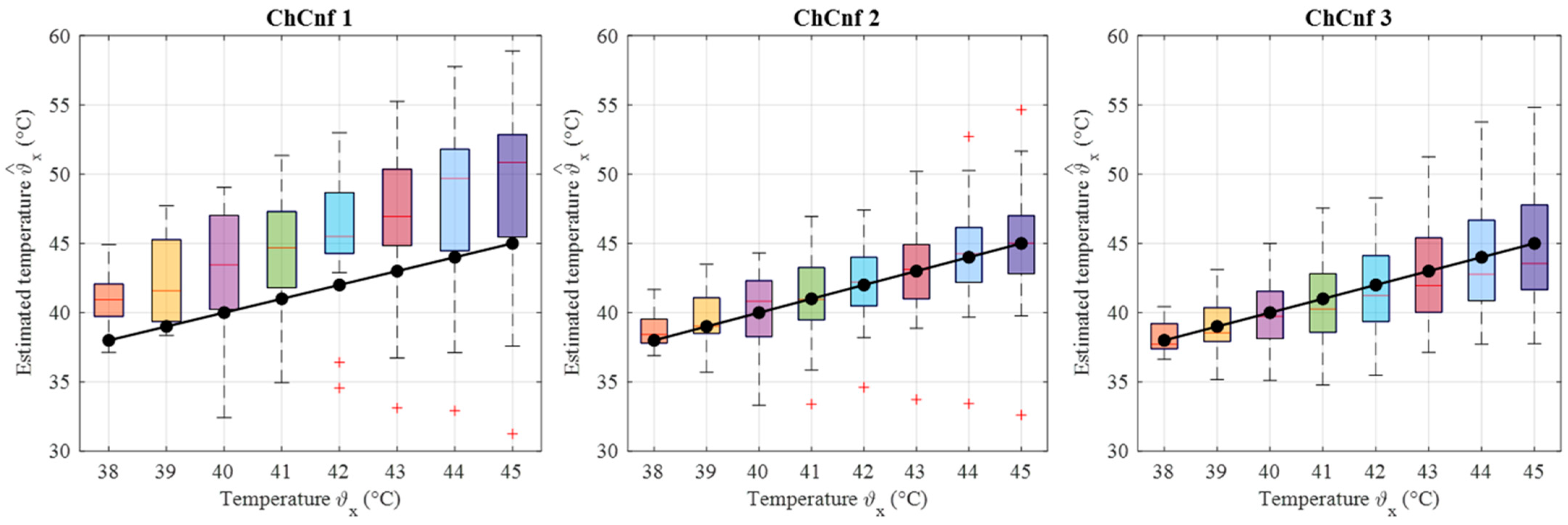
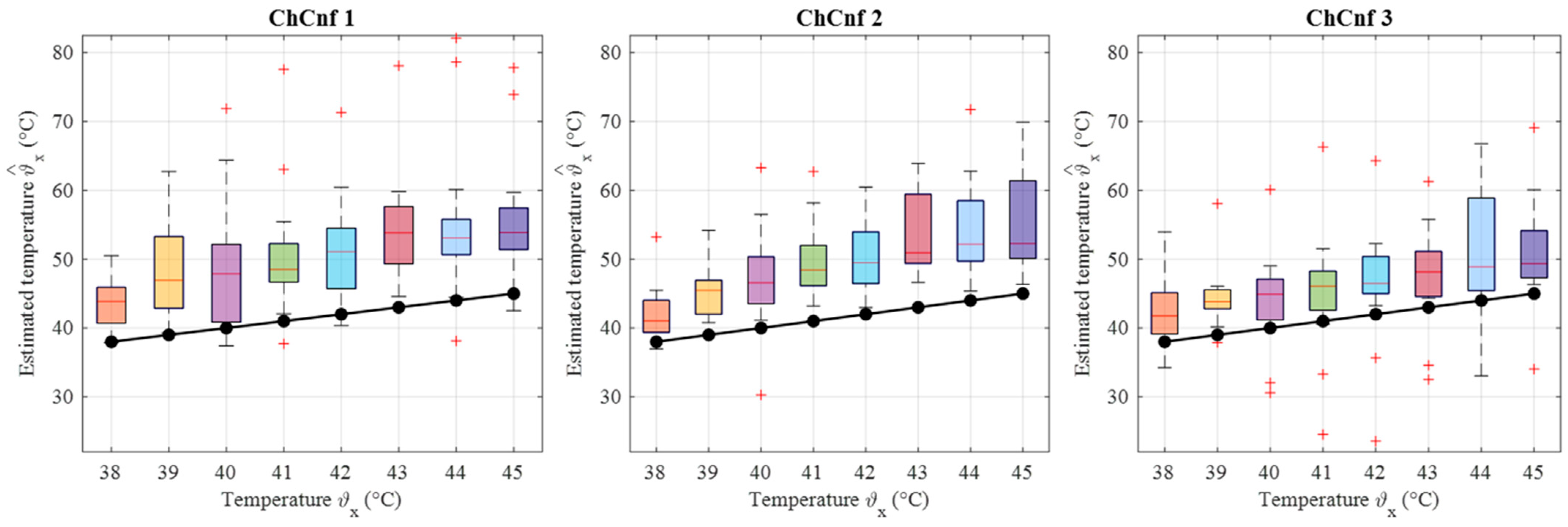
3.2. Imaging and Estimation of Temperature
4. Discussion
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- National Cancer Institute. Types of Cancer Treatment. Nih. 2015. Available online: https://www.cancer.gov/about-cancer/treatment/types (accessed on 10 June 2024).
- Datta, N.R.; Bose, A.K.; Kapoor, H.K.; Gupta, S. Head and neck cancers: Results of thermoradiotherapy versus radiotherapy. Int. J. Hyperth. 2009, 6, 479–486. [Google Scholar] [CrossRef] [PubMed]
- Datta, N.R.; Ordóñez, S.G.; Gaipl, U.S.; Paulides, M.M.; Crezee, H.; Gellermann, J.; Marder, D.; Puric, E.; Bodis, S. Local hyperthermia combined with radiotherapy and-/or chemotherapy: Recent advances and promises for the future. Cancer Treat. Rev. 2015, 41, 742–753. [Google Scholar] [CrossRef] [PubMed]
- IJff, M.; Crezee, J.; Oei, A.L.; Stalpers, L.J.A.; Westerveld, H. The role of hyperthermia in the treatment of locally advanced cervical cancer: A comprehensive review. Int. J. Gynecol. Cancer 2022, 32, 288–296. [Google Scholar] [CrossRef]
- Kok, H.P.; Cressman, E.N.K.; Ceelen, W.; Brace, C.L.; Ivkov, R.; Grüll, H.; ter Haar, G.; Wust, P.; Crezee, J. Heating technology for malignant tumors: A review. Int. J. Hyperth. 2020, 37, 711–741. [Google Scholar] [CrossRef]
- Valdagni, R.; Amichetti, M. Report of long-term follow-up in a randomized trial comparing radiation therapy and radiation therapy plus hyperthermia to metastatic lymphnodes in stage iv head and neck patients. Int. J. Radiat. Oncol. Biol. Phys. 1993, 28, 163–169. [Google Scholar] [CrossRef]
- Huilgol, N.G.; Gupta, S.; Sridhar, C.R. Hyperthermia with radiation in the treatment of locally advanced head and neck cancer: A report of randomized trial. J. Cancer Res. Ther. 2010, 6, 492–496. [Google Scholar] [CrossRef]
- Merten, R.; Ott, O.; Haderlein, M.; Bertz, S.; Hartmann, A.; Wullich, B.; Keck, B.; Kühn, R.; Rödel, C.M.; Weiss, C.; et al. Long-Term Experience of Chemoradiotherapy Combined with Deep Regional Hyperthermia for Organ Preservation in High-Risk Bladder Cancer (Ta, Tis, T1, T2). Oncologist 2019, 24, e1341–e1350. [Google Scholar] [CrossRef]
- Van Der Zee, J.; Peer-Valstar, J.N.; Rietveld, P.J.M.; De Graaf-Strukowska, L.; Van Rhoon, G.C. Practical limitations of interstitial thermometry during deep hyperthermia. Int. J. Radiat. Oncol. Biol. Phys. 1998, 40, 1205–1212. [Google Scholar] [CrossRef]
- Togni, P.; Rijnen, Z.; Numan, W.C.M.; Verhaart, R.F.; Bakker, J.F.; Van Rhoon, G.C.; Paulides, M.M. Electromagnetic redesign of the HYPERcollar applicator: Toward improved deep local head-and-neck hyperthermia. Phys. Med. Biol. 2013, 58, 5997–6009. [Google Scholar] [CrossRef]
- Adibzadeh, F.; Sumser, K.; Curto, S.; Yeo, D.T.B.; Shishegar, A.A.; Paulides, M.M. Systematic review of pre-clinical and clinical devices for magnetic resonance-guided radiofrequency hyperthermia. Int. J. Hyperth. 2020, 37, 15–27. [Google Scholar] [CrossRef] [PubMed]
- Fani, F.; Schena, E.; Saccomandi, P.; Silvestri, S. CT-based thermometry: An overview. Int. J. Hyperth. 2014, 30, 219–227. [Google Scholar] [CrossRef] [PubMed]
- Ebbini, E.S.; Simon, C.; Liu, D. Real-Time Ultrasound Thermography and Thermometry [Life Sciences]. IEEE Signal Process. Mag. 2018, 35, 166–174. [Google Scholar] [CrossRef]
- Poni, R.; Neufeld, E.; Capstick, M.; Bodis, S.; Samaras, T.; Kuster, N. Feasibility of temperature control by electrical impedance tomography in hyperthermia. Cancers 2021, 13, 3297. [Google Scholar] [CrossRef] [PubMed]
- Sun, G.; Ma, P.; Liu, J.; Shi, C.; Ma, J.; Peng, L. Design and implementation of a novel interferometric microwave radiometer for human body temperature measurement. Sensors 2021, 21, 1619. [Google Scholar] [CrossRef]
- Stec, B.; Dobrowolski, A.; Susek, W. Multifrequency Microwave Thermograph for Biomedical Applications. IEEE Trans. Biomed. Eng. 2004, 51, 548–551. [Google Scholar] [CrossRef] [PubMed]
- Grzegorczyk, T.M.; Meaney, P.M.; Kaufman, P.A.; DiFlorio-Alexander, R.M.; Paulsen, K.D. Fast 3-D Tomographic Microwave Imaging for Breast Cancer Detection. IEEE Trans. Med. Imaging 2012, 31, 1584–1592. [Google Scholar] [CrossRef]
- Chen, G.; Stang, J.; Haynes, M.; Leuthardt, E.; Moghaddam, M. Real-Time Three-Dimensional Microwave Monitoring of Interstitial Thermal Therapy. IEEE Trans. Biomed. Eng. 2018, 65, 528–538. [Google Scholar] [CrossRef]
- Kidera, S.; Neira, L.M.; Van Veen, B.D.; Hagness, S.C. TDOA-based microwave imaging algorithm for real-time microwave ablation monitoring. Int. J. Microw. Wirel. Technol. 2017, 10, 169–178. [Google Scholar] [CrossRef]
- Scapaticci, R.; Lopresto, V.; Pinto, R.; Cavagnaro, M.; Crocco, L. Monitoring Thermal Ablation via Microwave Tomography: An Ex Vivo Experimental Assessment. Diagnostics 2018, 8, 81. [Google Scholar] [CrossRef]
- Dogu, S.; Onal, H.; Yilmaz, T.; Akduman, I.; Akinci, M.N. Continuous Monitoring of Hyperthermia Treatment of Breast Tumors with Singular Sources Method. IEEE Access 2023, 11, 6584–6593. [Google Scholar] [CrossRef]
- Onal, H.; Yilmaz, T.; Akinci, M.N. A BIM-Based Algorithm for Quantitative Monitoring of Temperature Distribution during Breast Hyperthermia Treatments. IEEE Access 2023, 11, 38680–38695. [Google Scholar] [CrossRef]
- Tesarik, J.; Vrba, J.; Trefna, H.D. Non-invasive Thermometry during Hyperthermia Using Differential Microwave Imaging Approach. In Proceedings of the 15th European Conference on Antennas and Propagation, EuCAP 2021, Dusseldorf, Germany, 22–26 March 2021. [Google Scholar]
- Sachs, J. Handbook of Ultra-Wideband Short-Range Sensing: Theory, Sensors, Applications; Wiley-VCH: Hoboken, NJ, USA, 2012; ISBN 978-3-527-40853-5. [Google Scholar]
- Prokhorova, A.; Ley, S.; Helbig, M. Quantitative interpretation of uwb radar images for non-invasive tissue temperature estimation during hyperthermia. Diagnostics 2021, 11, 818. [Google Scholar] [CrossRef] [PubMed]
- Helbig, M.; Faenger, B.; Ley, S.; Hilger, I. Multistatic M-sequence UWB Radar System for Microwave Breast Imaging. In Proceedings of the 2021 IEEE Conference on Antenna Measurements and Applications, CAMA 2021, Antibes Juan-les-Pins, France, 15–17 November 2021; pp. 540–545. [Google Scholar]
- Prokhorova, A.; Ley, S.; Ruiz, A.Y.; Scapaticci, R.; Crocco, L.; Helbig, M. Preliminary Investigations of Microwave Imaging Algorithms for Tissue Temperature Estimation during Hyperthermia Treatment. In Proceedings of the 2021 International Conference on Electromagnetics in Advanced Applications, ICEAA 2021, Honolulu, HI, USA, 9–13 August 2021; pp. 79–84. [Google Scholar]
- Prokhorova, A.; Fiser, O.; Vrba, J.; Helbig, M. Experimental Study of Optimal Antenna Array Configuration for Non-invasive UWB Microwave Temperature Monitoring during Hyperthermia. In Proceedings of the 2021 IEEE Conference on Antenna Measurements and Applications, CAMA 2021, Antibes Juan-les-Pins, France, 15–17 November 2021; pp. 529–534. [Google Scholar]
- Prokhorova, A.; Fiser, O.; Vrba, J.; Helbig, M. Microwave Ultra-Wideband Imaging for Non-invasive Temperature Monitoring during Hyperthermia Treatment. In Electromagnetic Imaging for a Novel Generation of Medical Devices; Lecture Notes in Bioengineering; Vipiana, F., Crocco, L., Eds.; Springer International Publishing: Cham, Switzerland, 2023; Volume Part F809, pp. 293–330. ISBN 978-3-031-28666-7. [Google Scholar]
- Pollacco, D.A.; Farina, L.; Wismayer, P.S.; Farrugia, L.; Sammut, C.V. Characterization of the dielectric properties of biological tissues and their correlation to tissue hydration. IEEE Trans. Dielectr. Electr. Insul. 2018, 25, 2191–2197. [Google Scholar] [CrossRef]
- Maniakova, E.; Faktorova, D. Measuring the Dielectric Properties of Tumor and Breast Phantoms Used in the Microwave Frequency Range. In Proceedings of the CBU International Conference Proceedings, Prague, Czech Republic, 23–25 March 2016; Volume 4, pp. 647–651. [Google Scholar]
- Lazebnik, M.; Popovic, D.; McCartney, L.; Watkins, C.B.; Lindstrom, M.J.; Harter, J.; Sewall, S.; Ogilvie, T.; Magliocco, A.; Breslin, T.M.; et al. A large-scale study of the ultrawideband microwave dielectric properties of normal, benign and malignant breast tissues obtained from cancer surgeries. Phys. Med. Biol. 2007, 52, 6093–6115. [Google Scholar] [CrossRef]
- O’Rourke, A.P.; Lazebnik, M.; Bertram, J.M.; Converse, M.C.; Hagness, S.C.; Webster, J.G.; Mahvi, D.M. Dielectric properties of human normal, malignant and cirrhotic liver tissue: In vivo and ex vivo measurements from 0.5 to 20 GHz using a precision open-ended coaxial probe. Phys. Med. Biol. 2007, 52, 4707–4719. [Google Scholar] [CrossRef]
- Martellosio, A.; Pasian, M.; Bozzi, M.; Perregrini, L.; Mazzanti, A.; Svelto, F.; Summers, P.E.; Renne, G.; Preda, L.; Bellomi, M. Dielectric properties characterization from 0.5 to 50 GHz of breast cancer tissues. IEEE Trans. Microw. Theory Tech. 2017, 65, 998–1011. [Google Scholar] [CrossRef]
- Ley, S.; Schilling, S.; Fiser, O.; Vrba, J.; Sachs, J.; Helbig, M. Ultra-wideband temperature dependent dielectric spectroscopy of porcine tissue and blood in the microwave frequency range. Sensors 2019, 19, 1707. [Google Scholar] [CrossRef]
- Salahuddin, S.; La Gioia, A.; Elahi, M.A.; Porter, E.; O’Halloran, M.; Shahzad, A. Comparison of in-vivo and ex-vivo dielectric properties of biological tissues. In Proceedings of the 2017 19th International Conference on Electromagnetics in Advanced Applications, ICEAA 2017, Verona, Italy, 11–15 September 2017; pp. 582–585. [Google Scholar]
- Rossmann, C.; Haemmerich, D. Review of temperature dependence of thermal properties, dielectric properties, and perfusion of biological tissues at hyperthermic and ablation temperatures. Crit. Rev. Biomed. Eng. 2014, 42, 467–492. [Google Scholar] [CrossRef]
- Slanina, T.; Nguyen, D.H.; Moll, J.; Krozer, V. Temperature dependence studies of tissue-mimicking phantoms for ultra-wideband microwave breast tumor detection. Biomed. Phys. Eng. Express 2022, 8, 055017. [Google Scholar] [CrossRef]
- Lopresto, V.; Pinto, R.; Lovisolo, G.A.; Cavagnaro, M. Changes in the dielectric properties of ex vivo bovine liver during microwave thermal ablation at 2.45 GHz. Phys. Med. Biol. 2012, 57, 2309–2327. [Google Scholar] [CrossRef] [PubMed]
- Prokhorova, A.; Ley, S.; Fiser, O.; Vrba, J.; Sachs, J.; Helbig, M. Temperature Dependent Dielectric Properties of Tissue Mimicking Phantom Material in the Microwave Frequency Range. In Proceedings of the 14th European Conference on Antennas and Propagation, EuCAP 2020, Copenhagen, Denmark, 15–20 March 2020. [Google Scholar]
- Helbig, M.; Koch, J.H.; Ley, S.; Herrmann, R.; Kmec, M.; Schilling, K.; Sachs, J. Development and test of a massive MIMO system for fast medical UWB imaging. In Proceedings of the 2017 19th International Conference on Electromagnetics in Advanced Applications, ICEAA 2017, Verona, Italy, 11–15 September 2017; pp. 1331–1334. [Google Scholar]
- Fiser, O.; Merunka, I.; Vrba, J. Waveguide applicator system for head and neck hyperthermia treatment. J. Electr. Eng. Technol. 2016, 11, 1744–1753. [Google Scholar] [CrossRef]
- Whittle, A.T.; Marshall, I.; Mortimore, I.L.; Wraith, P.K.; Sellar, R.J.; Douglas, N.J. Neck soft tissue and fat distribution: Comparison between normal men and women by magnetic resonance imaging. Thorax 1999, 54, 323–328. [Google Scholar] [CrossRef] [PubMed]
- Buono, R.; Sabatino, L.; Greco, F. Neck fat volume as a potential indicator of difficult intubation: A pilot study. Saudi J. Anaesth. 2018, 12, 67–71. [Google Scholar] [CrossRef] [PubMed]
- Joachimowicz, N.; Conessa, C.; Henriksson, T.; Duchêne, B. Breast phantoms for microwave imaging. IEEE Antennas Wirel. Propag. Lett. 2014, 13, 1333–1336. [Google Scholar] [CrossRef]
- Relva, M.; Devesa, S. Dielectric Stability of Triton X-100-Based Tissue-Mimicking Materials for Microwave Imaging. Spectrosc. J. 2023, 1, 72–85. [Google Scholar] [CrossRef]
- Fiber Optic Temperature Sensors-Weidmann Optocon. Available online: https://weidmann-optocon.com/products/fiber-optic-temperature-sensors/ (accessed on 5 July 2024).
- Scapaticci, R.; Bellizzi, G.G.; Cavagnaro, M.; Lopresto, V.; Crocco, L. Exploiting Microwave Imaging Methods for Real-Time Monitoring of Thermal Ablation. Int. J. Antennas Propag. 2017, 2017, 5231065. [Google Scholar] [CrossRef]
- Vasquez, J.A.T.; Scapaticci, R.; Turvani, G.; Bellizzi, G.; Rodriguez-Duarte, D.O.; Joachimowicz, N.; Duchêne, B.; Tedeschi, E.; Casu, M.R.; Crocco, L.; et al. A prototype microwave system for 3D brain stroke imaging. Sensors 2020, 20, 2607. [Google Scholar] [CrossRef]
- Mozumi, M.; Nagaoka, R.; Hasegawa, H. Utilization of singular value decomposition in high-frame-rate cardiac blood flow imaging. Jpn. J. Appl. Phys. 2019, 58, SGGE02. [Google Scholar] [CrossRef]
- Tobon Vasquez, J.A.; Scapaticci, R.; Turvani, G.; Ricci, M.; Farina, L.; Litman, A.; Casu, M.R.; Crocco, L.; Vipiana, F. Noninvasive Inline Food Inspection via Microwave Imaging Technology: An Application Example in the Food Industry. IEEE Antennas Propag. Mag. 2020, 62, 18–32. [Google Scholar] [CrossRef]
- Rodriguez-Duarte, D.O.; Origlia, C.; Vasquez, J.A.T.; Scapaticci, R.; Crocco, L.; Vipiana, F. Experimental Assessment of Real-Time Brain Stroke Monitoring via a Microwave Imaging Scanner. IEEE Open J. Antennas Propag. 2022, 3, 824–835. [Google Scholar] [CrossRef]














Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Prokhorova, A.; Helbig, M. Experimental Validation of Realistic Measurement Setup for Quantitative UWB-Guided Hyperthermia Temperature Monitoring. Sensors 2024, 24, 5902. https://doi.org/10.3390/s24185902
Prokhorova A, Helbig M. Experimental Validation of Realistic Measurement Setup for Quantitative UWB-Guided Hyperthermia Temperature Monitoring. Sensors. 2024; 24(18):5902. https://doi.org/10.3390/s24185902
Chicago/Turabian StyleProkhorova, Alexandra, and Marko Helbig. 2024. "Experimental Validation of Realistic Measurement Setup for Quantitative UWB-Guided Hyperthermia Temperature Monitoring" Sensors 24, no. 18: 5902. https://doi.org/10.3390/s24185902




