Sensors in Bone: Technologies, Applications, and Future Directions
Abstract
:1. Introduction
2. An Overview of the Available Bone Turnover Biomarkers and Existing Biosensors for Monitoring Bone Health
2.1. Biomarkers of Bone Formation
2.1.1. Alkaline Phosphatase (ALP)
2.1.2. Osteocalcin (OC)
2.1.3. Propeptides of Type I Procollagen (PICP and PINP)
2.2. Biomarkers of Bone Resorption
2.2.1. Hydroxyproline (OHP)
2.2.2. Hydroxylysine-Glycosides
2.2.3. Collagen Crosslink Molecules
2.2.4. Cross-Linked Telopeptides of Type I Collagen
2.2.5. Bone Sialoprotein (BSP)
2.2.6. Tartrate-Resistant Acid Phosphatase (TRAP)
2.2.7. Cathepsin K
2.3. Analytical Methods for the Measurement of Bone Turnover Markers
2.3.1. Enzyme-Linked Immunosorbent Assay (ELISA)
2.3.2. Electrochemiluminescence Immunoassay (ECLIA)
2.3.3. Radioimmunoassay (RIA)
2.3.4. High-Performance Liquid Chromatography (HPLC)
3. Biosensors for Bone Disorders
3.1. Electrochemical Biosensors
3.2. Colorimetric Biosensors
3.3. Fluorescence Biosensors
3.4. Multiplex Assays
3.5. Label-Free Biosensors
3.6. Biodegradable Biosensors
4. Bone Physical Sensors
4.1. Electrical Sensors
4.2. Optical Biosensors
4.3. Piezoelectric Sensors
5. Current Applications of Bone Sensors
6. Conclusions and Future Directions
Author Contributions
Funding
Conflicts of Interest
References
- Frost, H.M. Skeletal structural adaptations to mechanical usage (SATMU): 1. Redefining Wolff’s law: The bone modeling problem. Anat. Rec. 1990, 226, 403–413. [Google Scholar] [CrossRef] [PubMed]
- Crockett, J.C.; Rogers, M.J.; Coxon, F.P.; Hocking, L.J.; Helfrich, M.H. Bone remodelling at a glance. J. Cell Sci. 2011, 124, 991–998. [Google Scholar] [CrossRef] [PubMed]
- Feng, X.; McDonald, J.M. Disorders of bone remodeling. Annu. Rev. Pathol. Mech. Dis. 2011, 6, 121–145. [Google Scholar] [CrossRef] [PubMed]
- Lupsa, B.C.; Insogna, K. Bone health and osteoporosis. Endocrinol. Metab. Clin. 2015, 44, 517–530. [Google Scholar] [CrossRef]
- Claudon, A.l.; Vergnaud, P.; Valverde, C.c.; Mayr, A.; Klause, U.; Garnero, P. New automated multiplex assay for bone turnover markers in osteoporosis. Clin. Chem. 2008, 54, 1554–1563. [Google Scholar] [CrossRef]
- Parmar, B.J.; Longsine, W.; Sabonghy, E.P.; Han, A.; Tasciotti, E.; Weiner, B.K.; Ferrari, M.; Righetti, R. Characterization of controlled bone defects using 2D and 3D ultrasound imaging techniques. Phys. Med. Biol. 2010, 55, 4839. [Google Scholar] [CrossRef]
- Liu, L.; Webster, T.J. In situ sensor advancements for osteoporosis prevention, diagnosis, and treatment. Curr. Osteoporos. Rep. 2016, 14, 386–395. [Google Scholar] [CrossRef]
- Nash, K.E.; Ong, K.G.; Guldberg, R.E. Implantable biosensors for musculoskeletal health. Connect. Tissue Res. 2022, 63, 228–242. [Google Scholar] [CrossRef]
- Vasikaran, S.; Eastell, R.; Bruyère, O.; Foldes, A.J.; Garnero, P.; Griesmacher, A.; McClung, M.; Morris, H.A.; Silverman, S.; Trenti, T.; et al. Markers of bone turnover for the prediction of fracture risk and monitoring of osteoporosis treatment: A need for international reference standards. Osteoporos. Int. 2011, 22, 391–420. [Google Scholar] [CrossRef]
- Hart, S.M.; Eastell, R. Biochemical markers of bone turnover. Curr. Opin. Nephrol. Hypertens. 1999, 8, 421–427. [Google Scholar] [CrossRef]
- Magnusson, P.; Larsson, L.; Magnusson, M.; Davie, M.W.; Sharp, C.A. Isoforms of bone alkaline phosphatase: Characterization and origin in human trabecular and cortical bone. J. Bone Min. Res 1999, 14, 1926–1933. [Google Scholar] [CrossRef] [PubMed]
- Drechsler, C.; Verduijn, M.; Pilz, S.; Krediet, R.T.; Dekker, F.W.; Wanner, C.; Ketteler, M.; Boeschoten, E.W.; Brandenburg, V. Bone alkaline phosphatase and mortality in dialysis patients. Clin. J. Am. Soc. Nephrol. 2011, 6, 1752–1759. [Google Scholar] [CrossRef] [PubMed]
- Lowe, D.; Sanvictores, T.; Zubair, M.; John, S. Alkaline Phosphatase. In StatPearls; StatPearls Publishing LLC: Treasure Island, FL, USA, 2024. [Google Scholar]
- Gorman, L.; Statland, B.E. Clinical usefulness of alkaline phosphatase isoenzyme determinations. Clin. Biochem. 1977, 10, 171–174. [Google Scholar] [CrossRef] [PubMed]
- Farley, J.R.; Chesnut, C.H., 3rd; Baylink, D.J. Improved method for quantitative determination in serum of alkaline phosphatase of skeletal origin. Clin. Chem. 1981, 27, 2002–2007. [Google Scholar] [CrossRef]
- Abramowitz, M.; Muntner, P.; Coco, M.; Southern, W.; Lotwin, I.; Hostetter, T.H.; Melamed, M.L. Serum alkaline phosphatase and phosphate and risk of mortality and hospitalization. Clin. J. Am. Soc. Nephrol. 2010, 5, 1064–1071. [Google Scholar] [CrossRef]
- Khan, A.A.; Bilezikian, J.P.; Kung, A.; Dubois, S.J.; Standish, T.I.; Syed, Z.A. Alendronate therapy in men with primary hyperparathyroidism. Endocr. Pract. 2009, 15, 705–713. [Google Scholar] [CrossRef]
- Greenspan, S.L.; Emkey, R.D.; Bone III, H.G.; Weiss, S.R.; Bell, N.H.; Downs, R.W., Jr.; McKeever, C.; Miller, S.S.; Davidson, M.; Bolognese, M.A. Significant differential effects of alendronate, estrogen, or combination therapy on the rate of bone loss after discontinuation of treatment of postmenopausal osteoporosis: A randomized, double-blind, placebo-controlled trial. Ann. Intern. Med. 2002, 137, 875–883. [Google Scholar] [CrossRef]
- Meunier, P.J.; Roux, C.; Seeman, E.; Ortolani, S.; Badurski, J.E.; Spector, T.D.; Cannata, J.; Balogh, A.; Lemmel, E.-M.; Pors-Nielsen, S. The effects of strontium ranelate on the risk of vertebral fracture in women with postmenopausal osteoporosis. N. Engl. J. Med. 2004, 350, 459–468. [Google Scholar] [CrossRef]
- Hoang, Q.Q.; Sicheri, F.; Howard, A.J.; Yang, D.S. Bone recognition mechanism of porcine osteocalcin from crystal structure. Nature 2003, 425, 977–980. [Google Scholar] [CrossRef]
- Price, C.P.; Thompson, P.W. The role of biochemical tests in the screening and monitoring of osteoporosis. Ann. Clin. Biochem. 1995, 32, 244–260. [Google Scholar] [CrossRef]
- Brown, J.; Malaval, L.; Chapuy, M.; Delmas, P.; Edouard, C.; Meunier, P. Serum bone Gla-protein: A specific marker for bone formation in postmenopausal osteoporosis. Lancet 1984, 323, 1091–1093. [Google Scholar] [CrossRef] [PubMed]
- Ivaska, K.K.; Kakonen, S.-M.; Gerdhem, P.; Obrant, K.J.; Pettersson, K.; Vaananen, H.K. Urinary osteocalcin as a marker of bone metabolism. Clin. Chem. 2005, 51, 618–628. [Google Scholar] [CrossRef] [PubMed]
- Ivaska, K.K.; Hentunen, T.A.; Vääräniemi, J.; Ylipahkala, H.; Pettersson, K.; Väänänen, H.K. Release of intact and fragmented osteocalcin molecules from bone matrix during bone resorption in vitro. J. Biol. Chem. 2004, 279, 18361–18369. [Google Scholar] [CrossRef]
- Knapen, M.; Schurgers, L.; Vermeer, C. Vitamin K 2 supplementation improves hip bone geometry and bone strength indices in postmenopausal women. Osteoporos. Int. 2007, 18, 963–972. [Google Scholar] [CrossRef] [PubMed]
- Jukkola, A.; Tähtelä, R.; Thölix, E.; Vuorinen, K.; Blanco, G.; Risteli, L.; Risteli, J. Aggressive breast cancer leads to discrepant serum levels of the type I procollagen propeptides PINP and PICP. Cancer Res. 1997, 57, 5517–5520. [Google Scholar] [PubMed]
- Tromp, A.; Ooms, M.; Popp-Snijders, C.; Roos, J.; Lips, P. Predictors of fractures in elderly women. Osteoporos. Int. 2000, 11, 134–140. [Google Scholar] [CrossRef]
- Jagtap, V.R.; Ganu, J.V. Effect of antiresorptive therapy on urinary hydroxyproline in postmenopausal osteoporosis. Indian J. Clin. Biochem. 2012, 27, 90–93. [Google Scholar] [CrossRef]
- Calvo, M.S.; Eyre, D.R.; Gundberg, C.M. Molecular basis and clinical application of biological markers of bone turnover. Endocr. Rev. 1996, 17, 333–368. [Google Scholar]
- Swaminathan, R. Biochemical markers of bone turnover. Clin. Chim. Acta 2001, 313, 95–105. [Google Scholar] [CrossRef]
- Indumati, V.; Patil, V. Biochemical markers of bone remodeling in osteoporosis-current concepts. J. Clin. Diagn. Res. 2010, 4, 2089–2097. [Google Scholar]
- Yang, L.; Grey, V. Pediatric reference intervals for bone markers. Clin. Biochem. 2006, 39, 561–568. [Google Scholar] [CrossRef] [PubMed]
- Naidoo, U.; Goff, D.; Klibanski, A. Hyperprolactinemia and bone mineral density: The potential impact of antipsychotic agents. Psychoneuroendocrinology 2003, 28, 97–108. [Google Scholar] [CrossRef] [PubMed]
- Plebani, M.; Bernardi, D.; Meneghetti, M.F.; Ujka, F.; Zaninotto, M. Biological variability in assessing the clinical value of biochemical markers of bone turnover. Clin. Chim. Acta 2000, 299, 77–86. [Google Scholar] [CrossRef] [PubMed]
- Lane, J.M. Dynamics of Bone and Cartilage Metabolism. JBJS 2001, 83, 639. [Google Scholar] [CrossRef]
- Hlaing, T.T.; Compston, J.E. Biochemical markers of bone turnover—Uses and limitations. Ann. Clin. Biochem. 2014, 51, 189–202. [Google Scholar] [CrossRef]
- Viguet-Carrin, S.; Garnero, P.; Delmas, P. The role of collagen in bone strength. Osteoporos. Int. 2006, 17, 319–336. [Google Scholar] [CrossRef]
- Afsarimanesh, N.; Mukhopadhyay, S.; Kruger, M.; Marlena, K. Biosensors for the measurement of C-terminal telopeptide of type I Collagen (CTX-I). J. Osteoporos. Phys. Act. 2017, 5, 1000199. [Google Scholar] [CrossRef]
- Eastell, R. Bone Markers: Biochemical and Clinical Perspectives; CRC Press: Boca Raton, FL, USA, 2001. [Google Scholar]
- Herrmann, M.; Seibel, M. The amino-and carboxyterminal cross-linked telopeptides of collagen type I, NTX-I and CTX-I: A comparative review. Clin. Chim. Acta 2008, 393, 57–75. [Google Scholar] [CrossRef]
- Kyd, P.; De Vooght, K.; Kerkhoff, F.; Thomas, E.; Fairney, A. Clinical usefulness of biochemical resorption markers in osteoporosis. Ann. Clin. Biochem. 1999, 36, 483–491. [Google Scholar] [CrossRef]
- Nishizawa, Y.; Nakamura, T.; Ohta, H.; Kushida, K.; Gorai, I.; Shiraki, M.; Fukunaga, M.; Hosoi, T.; Miki, T.; Chaki, O. Guidelines for the use of biochemical markers of bone turnover in osteoporosis (2004). J. Bone Miner. Metab. 2005, 23, 97–104. [Google Scholar] [CrossRef]
- Zhang, J.-H.; Wang, J.; Tang, J.; Barnett, B.; Dickson, J.; Hahsimoto, N.; Williams, P.; Ma, W.; Zheng, W.; Yoneda, T. Bone sialoprotein promotes bone metastasis of a non-bone-seeking clone of human breast cancer cells. Anticancer Res. 2004, 24, 1361–1368. [Google Scholar] [PubMed]
- Ganss, B.; Kim, R.H.; Sodek, J. Bone sialoprotein. Crit. Rev. Oral Biol. Med. 1999, 10, 79–98. [Google Scholar] [CrossRef] [PubMed]
- Carlinfante, G.; Vassiliou, D.; Svensson, O.; Wendel, M.; Heinegård, D.; Andersson, G. Differential expression of osteopontin and bone sialoprotein in bone metastasis of breast and prostate carcinoma. Clin. Exp. Metastasis 2003, 20, 437–444. [Google Scholar] [CrossRef] [PubMed]
- Halleen, J.M.; Tiitinen, S.L.; Ylipahkala, H.; Fagerlund, K.M.; Vaananen, H.K. Tartrate-resistant acid phosphatase 5b (TRACP 5b) as a marker of bone resorption. Clin. Lab. 2006, 52, 499–510. [Google Scholar] [PubMed]
- Burtis, C.A.; Bruns, D.E. Tietz Fundamentals of Clinical Chemistry and Molecular Diagnostics-E-Book: Tietz Fundamentals of Clinical Chemistry and Molecular Diagnostics-E-Book; Elsevier Health Sciences: Amsterdam, The Netherlands, 2014. [Google Scholar]
- Delmas, P. Committee of Scientific Advisers of the International Osteoporosis Foundation. The use of biochemical markers of bone turnover in osteoporosis. Osteoporos. Int 2000, 11, S2–S17. [Google Scholar] [CrossRef]
- Nenonen, A.; Cheng, S.; Ivaska, K.K.; Alatalo, S.L.; Lehtimäki, T.; Schmidt-Gayk, H.; Uusi-Rasi, K.; Heinonen, A.; Kannus, P.; Sievänen, H. Serum TRACP 5b is a useful marker for monitoring alendronate treatment: Comparison with other markers of bone turnover. J. Bone Miner. Res. 2005, 20, 1804–1812. [Google Scholar] [CrossRef]
- Li, Z.; Yasuda, Y.; Li, W.; Bogyo, M.; Katz, N.; Gordon, R.E.; Fields, G.B.; Brömme, D. Regulation of collagenase activities of human cathepsins by glycosaminoglycans. J. Biol. Chem. 2004, 279, 5470–5479. [Google Scholar] [CrossRef]
- Leung, P.; Pickarski, M.; Zhuo, Y.; Masarachia, P.; Duong, L. The effects of the cathepsin K inhibitor odanacatib on osteoclastic bone resorption and vesicular trafficking. Bone 2011, 49, 623–635. [Google Scholar] [CrossRef]
- Pérez-Castrillón, J.L.; Pinacho, F.; De Luis, D.; Lopez-Menendez, M.; Dueñas Laita, A. Odanacatib, a new drug for the treatment of osteoporosis: Review of the results in postmenopausal women. J. Osteoporos. 2010, 2010, 401581. [Google Scholar] [CrossRef]
- Skoumal, M.; Haberhauer, G.; Kolarz, G.; Hawa, G.; Woloszczuk, W.; Klingler, A. Serum cathepsin K levels of patients with longstanding rheumatoid arthritis: Correlation with radiological destruction. Arthritis Res. Ther. 2004, 7, 1–6. [Google Scholar]
- Aydin, S. A short history, principles, and types of ELISA, and our laboratory experience with peptide/protein analyses using ELISA. Peptides 2015, 72, 4–15. [Google Scholar] [CrossRef] [PubMed]
- Lequin, R.M. Enzyme immunoassay (EIA)/enzyme-linked immunosorbent assay (ELISA). Clin. Chem. 2005, 51, 2415–2418. [Google Scholar] [CrossRef] [PubMed]
- Engvall, E. The ELISA, enzyme-linked immunosorbent assay. Clin. Chem. 2010, 56, 319–320. [Google Scholar] [CrossRef] [PubMed]
- Gan, S.D.; Patel, K.R. Enzyme immunoassay and enzyme-linked immunosorbent assay. J. Investig. Dermatol. 2013, 133, 1–3. [Google Scholar] [CrossRef]
- Schini, M.; Vilaca, T.; Gossiel, F.; Salam, S.; Eastell, R. Bone Turnover Markers: Basic Biology to Clinical Applications. Endocr. Rev. 2023, 44, 417–473. [Google Scholar] [CrossRef]
- Owen, J.A.; Punt, J.; Stranford, S.A. Kuby Immunology; WH Freeman: New York, NY, USA, 2013; Volume 27. [Google Scholar]
- Revoltella, R.P.; Laricchia Robbio, L.; Liedberg, B. Comparison of conventional immunoassays (RIA, ELISA) with surface plasmon resonance for pesticide detection and monitoring. Biotherapy 1998, 11, 135–145. [Google Scholar] [CrossRef]
- Graham, L.H.; Bolling, J.; Miller, G.; Pratt-Hawkes, N.; Joseph, S. Enzyme-Immunoassay for the Measurement of Luteinizing Hormone in the Serum of African Elephants (Loxodonta africana); Wiley Online Library: Hoboken, NJ, USA, 2002. [Google Scholar]
- Dziuba, J.; Nałęcz, D.; Minkiewicz, P.; Hanasiewicz, A. Application of ultraviolet spectroscopy to discriminate wheat α/β- and γ-gliadins separated with high-performance liquid chromatography—A short report. Pol. J. Food Nutr. Sci. 2007, 57, 191–193. [Google Scholar]
- Reuhs, B.L. High-performance liquid chromatography. In Food Analysis; Springer: Cham, Switzerland, 2017; pp. 213–226. [Google Scholar]
- Bhalla, P.; Singh, N. Generalized Drude scattering rate from the memory function formalism: An independent verification of the Sharapov-Carbotte result. Eur. Phys. J. B 2016, 89, 46. [Google Scholar] [CrossRef]
- Bhatia, D.; Paul, S.; Acharjee, T.; Ramachairy, S.S. Biosensors and their widespread impact on human health. Sens. Int. 2024, 5, 100257. [Google Scholar] [CrossRef]
- Kim, J.; Campbell, A.S.; de Ávila, B.E.-F.; Wang, J. Wearable biosensors for healthcare monitoring. Nat. Biotechnol. 2019, 37, 389–406. [Google Scholar] [CrossRef]
- German, N.; Popov, A.; Ramanaviciene, A. Reagentless Glucose Biosensor Based on Combination of Platinum Nanostructures and Polypyrrole Layer. Biosensors 2024, 14, 134. [Google Scholar] [CrossRef] [PubMed]
- Naresh, V.; Lee, N. A review on biosensors and recent development of nanostructured materials-enabled biosensors. Sensors 2021, 21, 1109. [Google Scholar] [CrossRef] [PubMed]
- Rani, S.; Bandyopadhyay-Ghosh, S.; Ghosh, S.B.; Liu, G. Advances in sensing technologies for monitoring of bone health. Biosensors 2020, 10, 42. [Google Scholar] [CrossRef] [PubMed]
- Park, R.; Jeon, S.; Jeong, J.; Park, S.-Y.; Han, D.-W.; Hong, S.W. Recent advances of point-of-care devices integrated with molecularly imprinted polymers-based biosensors: From biomolecule sensing design to intraoral fluid testing. Biosensors 2022, 12, 136. [Google Scholar] [CrossRef]
- Karunakaran, C.; Rajkumar, R.; Bhargava, K. Introduction to biosensors. In Biosensors and Bioelectronics; Elsevier: Amsterdam, The Netherlands, 2015; pp. 1–68. [Google Scholar]
- Malik, S.; Singh, J.; Goyat, R.; Saharan, Y.; Chaudhry, V.; Umar, A.; Ibrahim, A.A.; Akbar, S.; Ameen, S.; Baskoutas, S. Nanomaterials-based biosensor and their applications: A review. Heliyon 2023, 9, e19929. [Google Scholar] [CrossRef]
- Katey, B.; Voiculescu, I.; Penkova, A.N.; Untaroiu, A. A Review of Biosensors and Their Applications. ASME Open J. Eng. 2023, 2, 153–159. [Google Scholar] [CrossRef]
- Wang, J.; Chu, J.; Song, J.; Li, Z. The application of impantable sensors in the musculoskeletal system: A review. Front. Bioeng. Biotechnol. 2024, 12, 1270237. [Google Scholar] [CrossRef]
- Burny, F.; Donkerwolcke, M.; Moulart, F.; Bourgois, R.; Puers, R.; Van Schuylenbergh, K.; Barbosa, M.; Paiva, O.; Rodes, F.; Bégueret, J.B. Concept, design and fabrication of smart orthopedic implants. Med. Eng. Phys. 2000, 22, 469–479. [Google Scholar] [CrossRef]
- Wen, Y.-H.; Yang, G.Y.; Bailey, V.J.; Lin, G.; Tang, W.C.; Keyak, J.H. Mechanically robust micro-fabricated strain gauges for use on bones. In Proceedings of the 2005 3rd IEEE/EMBS Special Topic Conference on Microtechnology in Medicine and Biology, Oahu, HI, USA, 12–15 May 2005; pp. 302–304. [Google Scholar]
- Pang, C.; Lee, G.-Y.; Kim, T.-i.; Kim, S.M.; Kim, H.N.; Ahn, S.-H.; Suh, K.-Y. A flexible and highly sensitive strain-gauge sensor using reversible interlocking of nanofibres. Nat. Mater. 2012, 11, 795–801. [Google Scholar] [CrossRef]
- Dharap, P.; Li, Z.; Nagarajaiah, S.; Barrera, E. Nanotube film based on single-wall carbon nanotubes for strain sensing. Nanotechnology 2004, 15, 379. [Google Scholar] [CrossRef]
- Nogata, F.; Shimamoto, A.; Habu, T. Estimation of in vivo bone strength using ultrasound signals. Int. J. Mod. Phys. B 2003, 17, 1381–1387. [Google Scholar] [CrossRef]
- Umbrecht, F.; Wägli, P.; Dechand, S.; Gattiker, F.; Neuenschwander, J.; Sennhauser, U.; Hierold, C. Wireless implantable passive strain sensor: Design, fabrication and characterization. J. Micromech. Microeng. 2010, 20, 085005. [Google Scholar] [CrossRef]
- Bhalla, S.; Bajaj, S. Bone characterization using piezotransducers as biomedical sensors. Strain 2008, 44, 475–478. [Google Scholar] [CrossRef]
- Hsieh, M.; Fang, Y.-K.; Ju, M.; Ho, J.-J.; Ting, S. Development of a new contact-type piezoresistive micro-shear-stress sensor. In Proceedings of the Design, Test, Integration, and Packaging of MEMS/MOEMS, Montreux, Switzerland, 12–14 May 2002; pp. 285–295. [Google Scholar]
- Alfaro, F.; Weiss, L.; Campbell, P.; Miller, M.; Fedder, G.K. Design of a multi-axis implantable MEMS sensor for intraosseous bone stress monitoring. J. Micromech. Microeng. 2009, 19, 085016. [Google Scholar] [CrossRef]
- Alfaro, J.F.; Weiss, L.E.; Campbell, P.G.; Miller, M.C.; Heyward, C.; Doctor, J.S.; Fedder, G.K. Bioimplantable bone stress sensor. In Proceedings of the 2005 IEEE Engineering in Medicine and Biology 27th Annual Conference, Shanghai, China, 31 August–3 September 2005; pp. 518–521. [Google Scholar]
- Fresvig, T.; Ludvigsen, P.; Steen, H.; Reikerås, O. Fibre optic Bragg grating sensors: An alternative method to strain gauges for measuring deformation in bone. Med. Eng. Phys. 2008, 30, 104–108. [Google Scholar] [CrossRef]
- Mishra, V.; Singh, N.; Rai, D.; Tiwari, U.; Poddar, G.; Jain, S.; Mondal, S.; Kapur, P. Fiber Bragg grating sensor for monitoring bone decalcification. Orthop. Traumatol. Surg. Res. 2010, 96, 646–651. [Google Scholar] [CrossRef]
- Singh, P.; Shrivastava, A. Optical biosensor based on microbendings technique: An optimized mean to measure the bone strength. Adv. Opt. Technol. 2014, 2014, 853725. [Google Scholar] [CrossRef]
- Sirivisoot, S.; Yao, C.; Xiao, X.; Sheldon, B.W.; Webster, T.J. Developing biosensors for monitoring orthopedic tissue growth. In Materials Research Society Symposium Proceedings; Materials Research Society: Warrendale, PA, USA, 2007. [Google Scholar]
- Afsarimanesh, N.; Mukhopadhyay, S.C.; Kruger, M. Molecularly imprinted polymer-based electrochemical biosensor for bone loss detection. IEEE Trans. Biomed. Eng. 2017, 65, 1264–1271. [Google Scholar] [CrossRef]
- Ramanathan, M.; Patil, M.; Epur, R.; Yun, Y.; Shanov, V.; Schulz, M.; Heineman, W.R.; Datta, M.K.; Kumta, P.N. Gold-coated carbon nanotube electrode arrays: Immunosensors for impedimetric detection of bone biomarkers. Biosens. Bioelectron. 2016, 77, 580–588. [Google Scholar] [CrossRef]
- Yun, Y.-H.; Bhattacharya, A.; Watts, N.B.; Schulz, M.J. A label-free electronic biosensor for detection of bone turnover markers. Sensors 2009, 9, 7957–7969. [Google Scholar] [CrossRef]
- Inal Kabala, S.; Yagar, H.; Ozcan, H.M. A new biosensor for osteoporosis detection. Prep. Biochem. Biotechnol. 2019, 49, 511–520. [Google Scholar] [CrossRef] [PubMed]
- Sappia, L.; Felice, B.; Sanchez, M.A.; Martí, M.; Madrid, R.; Pividori, M.I. Electrochemical sensor for alkaline phosphatase as biomarker for clinical and in vitro applications. Sens. Actuators B Chem. 2019, 281, 221–228. [Google Scholar] [CrossRef]
- Koehne, J.E.; Cordeiro, M.J.S. Printed Electrochemical Sensor for Quantifying Bone Density Loss in Microgravity. In Proceedings of the 2021 Human Research Program Investigators’ Workshop, Virtual, 12–15 July 2021. [Google Scholar]
- Shaban, S.M.; Moon, B.-S.; Pyun, D.-G.; Kim, D.-H. A colorimetric alkaline phosphatase biosensor based on p-aminophenol-mediated growth of silver nanoparticles. Colloids Surf. B Biointerfaces 2021, 205, 111835. [Google Scholar] [CrossRef] [PubMed]
- Park, C.S.; Ha, T.H.; Kim, M.; Raja, N.; Yun, H.-s.; Sung, M.J.; Kwon, O.S.; Yoon, H.; Lee, C.-S. Fast and sensitive near-infrared fluorescent probes for ALP detection and 3d printed calcium phosphate scaffold imaging in vivo. Biosens. Bioelectron. 2018, 105, 151–158. [Google Scholar] [CrossRef]
- Hou, L.; Qin, Y.; Li, J.; Qin, S.; Huang, Y.; Lin, T.; Guo, L.; Ye, F.; Zhao, S. A ratiometric multicolor fluorescence biosensor for visual detection of alkaline phosphatase activity via a smartphone. Biosens. Bioelectron. 2019, 143, 111605. [Google Scholar] [CrossRef]
- Khashayar, P.; Amoabediny, G.; Larijani, B.; Hosseini, M.; Verplancke, R.; Schaubroeck, D.; Van Put, S.; Razi, F.; De Keersmaecker, M.; Adriaens, A. A multiplexed microfluidic platform for bone marker measurement: A proof-of-concept. Micromachines 2017, 8, 133. [Google Scholar] [CrossRef]
- Cho, I.-H.; Kim, D.H.; Park, S. Electrochemical biosensors: Perspective on functional nanomaterials for on-site analysis. Biomater. Res. 2020, 24, 6. [Google Scholar] [CrossRef]
- Li, H.; Liu, X.; Li, L.; Mu, X.; Genov, R.; Mason, A.J. CMOS electrochemical instrumentation for biosensor microsystems: A review. Sensors 2016, 17, 74. [Google Scholar] [CrossRef]
- Nabavi, N.; Khandani, A.; Camirand, A.; Harrison, R.E. Effects of microgravity on osteoclast bone resorption and osteoblast cytoskeletal organization and adhesion. Bone 2011, 49, 965–974. [Google Scholar] [CrossRef]
- Regard, J.B.; Zhong, Z.; Williams, B.O.; Yang, Y. Wnt signaling in bone development and disease: Making stronger bone with Wnts. Cold Spring Harb. Perspect. Biol. 2012, 4, a007997. [Google Scholar] [CrossRef]
- Bloomfield, S.A.; Martinez, D.A.; Boudreaux, R.D.; Mantri, A.V. Microgravity stress: Bone and connective tissue. Compr. Physiol 2016, 6, 645–686. [Google Scholar] [PubMed]
- Wignarajah, S.; Suaifan, G.A.; Bizzarro, S.; Bikker, F.J.; Kaman, W.E.; Zourob, M. Colorimetric assay for the detection of typical biomarkers for periodontitis using a magnetic nanoparticle biosensor. Anal. Chem. 2015, 87, 12161–12168. [Google Scholar] [CrossRef] [PubMed]
- Han, Y.; Chen, J.; Li, Z.; Chen, H.; Qiu, H. Recent progress and prospects of alkaline phosphatase biosensor based on fluorescence strategy. Biosens. Bioelectron. 2020, 148, 111811. [Google Scholar] [CrossRef]
- Samuel, V.R.; Rao, K.J. A review on label free biosensors. Biosens. Bioelectron. X 2022, 11, 100216. [Google Scholar] [CrossRef]
- Khashayar, P.; Amoabediny, G.; Larijani, B.; Vanfleteren, J. Bone biosensors: Knowing the present and predicting the future. J. Micromech. Microeng. 2016, 26, 023002. [Google Scholar] [CrossRef]
- Caglar, P.; Tuncel, S.; Malcik, N.; Landers, J.; Ferrance, J. A microchip sensor for calcium determination. Anal. Bioanal. Chem. 2006, 386, 1303–1312. [Google Scholar] [CrossRef]
- Malcik, N.; Ferrance, J.; Landers, J.; Caglar, P. The performance of a microchip-based fiber optic detection technique for the determination of Ca2+ ions in urine. Sens. Actuators B Chem. 2005, 107, 24–31. [Google Scholar] [CrossRef]
- Li, J. Fabrication and Characterization of Nano-FET Biosensors for Studying Osteocyte Mechanotransduction; University of Toronto: Toronto, ON, Canada, 2011. [Google Scholar]
- Singh, P.; Rai, H.; Singh, Z. Effect of neurons on the performance of microbend optical biosensor. Strain 2012, 1, 233–236. [Google Scholar]
- Afsarimanesh, N.; Mukhopadhyay, S.C.; Kruger, M. Sensing technologies for monitoring of bone-health: A review. Sens. Actuators A Phys. 2018, 274, 165–178. [Google Scholar] [CrossRef]
- Klosterhoff, B.S.; Ghee Ong, K.; Krishnan, L.; Hetzendorfer, K.M.; Chang, Y.-H.; Allen, M.G.; Guldberg, R.E.; Willett, N.J. Wireless implantable sensor for noninvasive, longitudinal quantification of axial strain across rodent long bone defects. J. Biomech. Eng. 2017, 139, 111004. [Google Scholar] [CrossRef]
- Luka, G.; Ahmadi, A.; Najjaran, H.; Alocilja, E.; DeRosa, M.; Wolthers, K.; Malki, A.; Aziz, H.; Althani, A.; Hoorfar, M. Microfluidics integrated biosensors: A leading technology towards lab-on-a-chip and sensing applications. Sensors 2015, 15, 30011–30031. [Google Scholar] [CrossRef] [PubMed]
- Arlett, J.; Myers, E.; Roukes, M. Comparative advantages of mechanical biosensors. Nat. Nanotechnol. 2011, 6, 203–215. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Liu, Y.; Li, Y.; Hao, Q. Development and application of resistance strain force sensors. Sensors 2020, 20, 5826. [Google Scholar] [CrossRef] [PubMed]
- Fukase, N.; Duke, V.R.; Lin, M.C.; Stake, I.K.; Huard, M.; Huard, J.; Marmor, M.T.; Maharbiz, M.M.; Ehrhart, N.P.; Bahney, C.S. Wireless measurements using electrical impedance spectroscopy to monitor fracture healing. Sensors 2022, 22, 6233. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Zhang, R.; Bi, R.; Olivo, M. Applications of Optical Fiber in Label-Free Biosensors and Bioimaging: A Review. Biosensors 2022, 13, 64. [Google Scholar] [CrossRef]
- Al-Fakih, E.; Osman, N.A.A.; Adikan, F.R.M. The use of fiber Bragg grating sensors in biomechanics and rehabilitation applications: The state-of-the-art and ongoing research topics. Sensors 2012, 12, 12890–12926. [Google Scholar] [CrossRef]
- Cole, C.P.; Navarro, R.R. eDisc: The first artificial spinal disc with integral force-Sensing microelectronics. Front. Biomed. Devices 2007, 42665, 49–50. [Google Scholar]
- Cushner, F.; Schiller, P.; Gross, J.; Mueller, J.; Hunter, W. A total knee arthroplasty prosthesis capable of remote patient monitoring. In Orthopaedic Proceedings; Bone & Joint: Singapore, 2021; p. 18. [Google Scholar]
- Graichen, F.; Bergmann, G.; Rohlmann, A. Hip endoprosthesis for in vivo measurement of joint force and temperature. J. Biomech. 1999, 32, 1113–1117. [Google Scholar] [CrossRef]
- D’Lima, D.D.; Townsend, C.P.; Arms, S.W.; Morris, B.A.; Colwell, C.W., Jr. An implantable telemetry device to measure intra-articular tibial forces. J. Biomech. 2005, 38, 299–304. [Google Scholar] [CrossRef]
- Song, S.J.; Lee, H.W.; Kim, K.I.; Park, C.H. Load imbalances existed as determined by a sensor after conventional gap balancing with a tensiometer in total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 2953–2961. [Google Scholar] [CrossRef]
- Ledet, E.H.; Tymeson, M.P.; DiRisio, D.J.; Cohen, B.; Uhl, R.L. Direct real-time measurement of in vivo forces in the lumbar spine. Spine J. 2005, 5, 85–94. [Google Scholar] [CrossRef] [PubMed]
- Glassman, S.D.; Carreon, L.Y.; Aruwajoye, O.; Benson, N.M.; Li, P.; Kurian, A.S. Local temperature elevation as a marker of spinal implant infection in an animal model. N. Am. Spine Soc. J. (NASSJ) 2021, 7, 100077. [Google Scholar] [CrossRef] [PubMed]
- McGilvray, K.C.; Unal, E.; Troyer, K.L.; Santoni, B.G.; Palmer, R.H.; Easley, J.T.; Demir, H.V.; Puttlitz, C.M. Implantable microelectromechanical sensors for diagnostic monitoring and post-surgical prediction of bone fracture healing. J. Orthop. Res. 2015, 33, 1439–1446. [Google Scholar] [CrossRef] [PubMed]
- Windolf, M.; Varjas, V.; Gehweiler, D.; Schwyn, R.; Arens, D.; Constant, C.; Zeiter, S.; Richards, R.G.; Ernst, M. Continuous Implant Load Monitoring to Assess Bone Healing Status—Evidence from Animal Testing. Medicina 2022, 58, 858. [Google Scholar] [CrossRef]
- Roriz, P.; Ferreira, J.M.; Potes, J.C.; Oliveira, M.T.; Frazão, O.; Santos, J.L.; Simões, J.A.d.O. In vivo measurement of the pressure signal in the intervertebral disc of an anesthetized sheep. J. Biomed. Opt. 2014, 19, 037006. [Google Scholar] [CrossRef]
| Marker | Secreted by/Source | Biological Sample | Analytical Method |
|---|---|---|---|
| Bone Formation Biomarker | |||
| Bone-specific alkaline phosphatase (BALP) | Osteoblasts | Serum | Colorimetric, ELISA, ECLIA, RIA |
| Osteocalcin (OC) | Osteoblasts, odontoblasts | Serum | ELISA |
| C-terminal propeptide of type I procollagen (PICP) | Osteoblasts | Serum | ELISA, RIA |
| N-terminal propeptide of type I procollagen (PINP) | Osteoblasts | Serum | ELISA, ECLIA, RIA |
| Bone Resorption Biomarker | |||
| Hydroxyproline (OHP) | Byproduct of collagen degradation | Urine | Colorimetric, HPLC |
| Hydroxylysine-glycosides (Hyl-glyc) | Byproduct of collagen degradation | Urine | HPLC, ELISA |
| Pyridinoline (PYD) | Formed during the extracellular maturation of collagen | Urine, Serum | HPLC, ELISA |
| Deoxypyridinoline (DPD) | Formed during the extracellular maturation of collagen | Urine, Serum | HPLC, ELISA |
| Amino-terminal cross-linked telopeptide of type I collagen (NTX-I) | Released by cathepsin K cleavage of bone collagen | Urine, Serum | ELISA, ECLIA, RIA |
| Carboxy-terminal cross-linked telopeptide of type I collagen (CTX-I) | Released by cathepsin K cleavage of bone collagen | Urine, Serum | ELISA, RIA |
| Bone sialoprotein (BSP) | Osteoblasts, osteoclasts, osteocytes, odontoblasts, and hypertrophic chondrocytes | Serum | ELISA, RIA |
| Tartrate-resistant acid phosphatase (TRAP) | Osteoclasts, neurons, and activated macrophages | Serum | Colorimetric, ELISA, RIA |
| Cathepsin K (Ctsk) | Osteoclasts | Serum | ELISA |
| Physical Sensors and Biomechanical Sensors | |||
|---|---|---|---|
| Sensor | Principle | Parameter Measured | References |
| MPACT 3500 Project | Resistance changes proportional to strain | Implant strain | [75] |
| Microfabricated Strain Gauge | Changes in electrical resistance due to strain | Surface strain on live bone | [76] |
| Flexible Strain-gauge Sensor | Changes in electrical resistance due to pressure, shear, and torsion | Pressure, shear, torsion | [77] |
| Nanotube Film Strain-sensing System | Voltage across film changes linearly with strain | Multidirectional strain sensing | [78] |
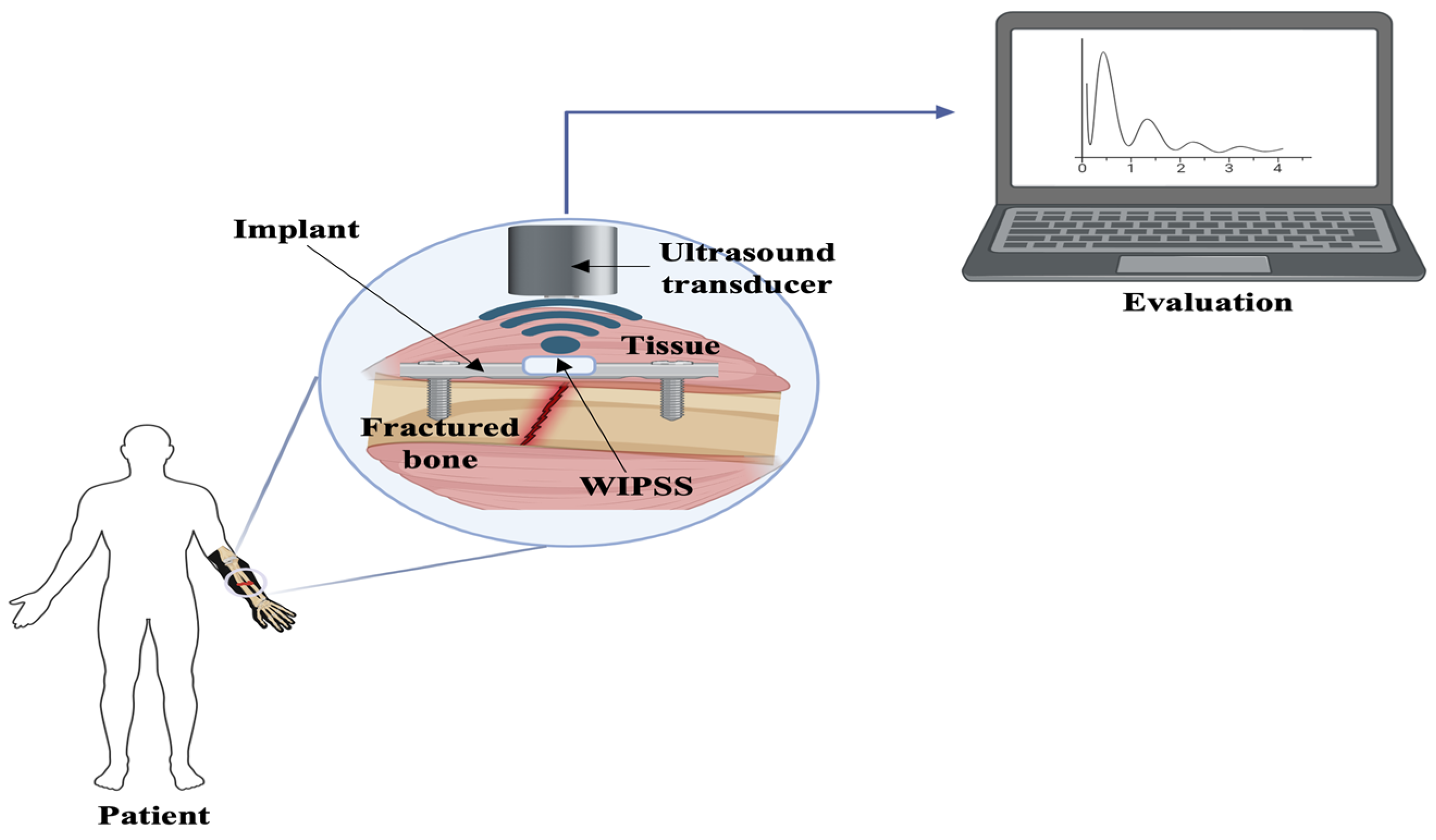
| Ultrasound-based Wireless Implantable Passive Strain Sensor (WIPSS) | Hydromechanical effects | Deformation of implants | [79,80] |
| Piezoelectric sensor | Changes in frequency-response function (FRF) | Mechanical parameters of bones | [81] |
| Piezoresistive Micro-shear-stress Sensor | Transformation of stress into voltage | Shear stress of knee prosthesis | [82] |
| Ultra-miniature Multiaxis Implantable Sensor | Changes in resistance | Bone stress at microscale level | [83,84] |
| Fiber Bragg Grating Sensors | Changes in Bragg wavelength due to strain | Strain measurement | [85,86] |
| Photometric sensor | Microbending technique to measure bone strength | Bone strength | [87] |
| Biodegradable sensor | Measures conductivity variations as new bone forms | Monitoring orthopedic tissue growth | [88] |
| Biosensors | |||
| Molecularly imprinted polymer biosensor for CTX-I | Selective binding of CTX-I molecules to synthesized antibodies | CTX-I | [89] |
| Carbon nanotube (CNT) electrodes coated with gold nanoparticles | Detection of CTX through antigen-antibody binding events on surface | CTX-I | [90] |
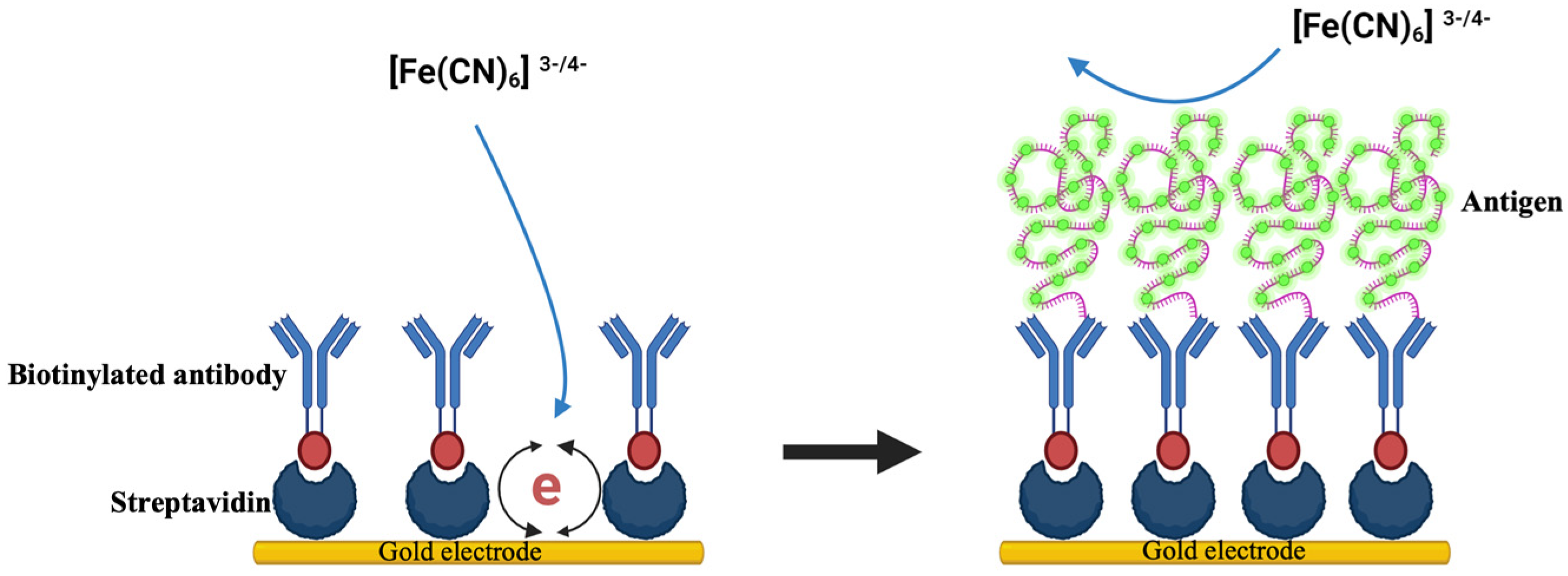
| Label-free immunosensor for C-terminal telopeptide bone turnover marker | Streptavidin immobilization, antibody binding, EIS for detection | CTX-I | [91] |
| Biosensor targeting osteocalcin | Covalent immobilization of antiosteocalcin antibody on gold electrode | Osteocalcin | [92] |
| Electrochemical biosensor for ALP determination | Disposable graphite screen-printed electrodes, SWV for quantification | ALP | [93] |
| Printed electrochemical biosensors for astronaut point-of-care testing | NTX antibodies are incorporated into the sensor’s electrode ink and read by handheld electronics for rapid measurements | NTX | [94] |
| Colorimetric sensor for alkaline phosphatase (ALP) | Detection of ALP activity through color change induced by AgNP growth | ALP | [95] |
| Novel NIR fluorescent probes for highly sensitive ALP detection | ALP cleaves the phosphate group in NIR probes, leading to a significant fluorescent signal increase | ALP | [96] |
| Selective, smartphone-based approach for visually detecting ALP using NH2-Cu-MOFs | Utilization of NH2-Cu-MOFs with oxidase mimicry and fluorescence capabilities for ALP detection | ALP | [97] |
| Automated multiplex immunoassay for bone turnover markers | Simultaneous measurement of CTX-I, PINP, OC, and PTH in 20 μL of serum | CTX-I, PINP, OC, PTH | [97] |
| Osteokit multiplex assay for bone marker assessment | Simultaneous measurement of OC and CTX-I in serum using a microfluidic platform | OC, CTX-I | [98] |
| Microchip-based sensor for determining calcium ion levels | Measurement of reflectance index of immobilized arsenazo III on polymer beads | Calcium ions | [97] |
| Sensor Type | Study | Implant | Remarks | Reference |
|---|---|---|---|---|
| Resistive sensors | Clinical studies | Hip | Sensors were integrated into a hip endoprosthesis to monitor joint contact forces and temperature distribution across the entirety of the titanium implant. | [122] |
| Knee | An electronic knee prosthesis was surgically implanted to assess tibial forces in vivo during daily activities following total knee arthroplasty (TKA). | [123] | ||
| Knee | To assess intercompartmental load intraoperatively following conventional gap balancing with a tensiometer during TKA. | [124] | ||
| Preclinical animal studies | Spine | In two baboons, interbody implants with instrumentation were surgically implanted into the disc space of a motion segment to monitor the in vivo loads in the lumbar spine. | [125] | |
| Spine | Temperature-sensing implants could consistently identify local temperature fluctuations linked to peri-implant wound infections. | [126] | ||
| Fracture | An implanted sensor system monitors implant load continuously to assess the status of bone healing. | [127] | ||
| Fracture | A wireless, biocompatible microelectromechanical system sensor was developed, evaluated, and implemented in a large animal model for monitoring purposes. | [128] | ||
| Optical sensors | Spine | Records the intradiscal pressure signal from a sedated sheep while it’s spontaneously breathing. | [129] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Anwar, A.; Kaur, T.; Chaugule, S.; Yang, Y.-S.; Mago, A.; Shim, J.-H.; John, A.A. Sensors in Bone: Technologies, Applications, and Future Directions. Sensors 2024, 24, 6172. https://doi.org/10.3390/s24196172
Anwar A, Kaur T, Chaugule S, Yang Y-S, Mago A, Shim J-H, John AA. Sensors in Bone: Technologies, Applications, and Future Directions. Sensors. 2024; 24(19):6172. https://doi.org/10.3390/s24196172
Chicago/Turabian StyleAnwar, Afreen, Taruneet Kaur, Sachin Chaugule, Yeon-Suk Yang, Aryan Mago, Jae-Hyuck Shim, and Aijaz Ahmad John. 2024. "Sensors in Bone: Technologies, Applications, and Future Directions" Sensors 24, no. 19: 6172. https://doi.org/10.3390/s24196172








