Effect of Unanticipated Tasks on Side-Cutting Stability of Lower Extremity with Patellofemoral Pain Syndrome
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Sensors
2.3. Procedures
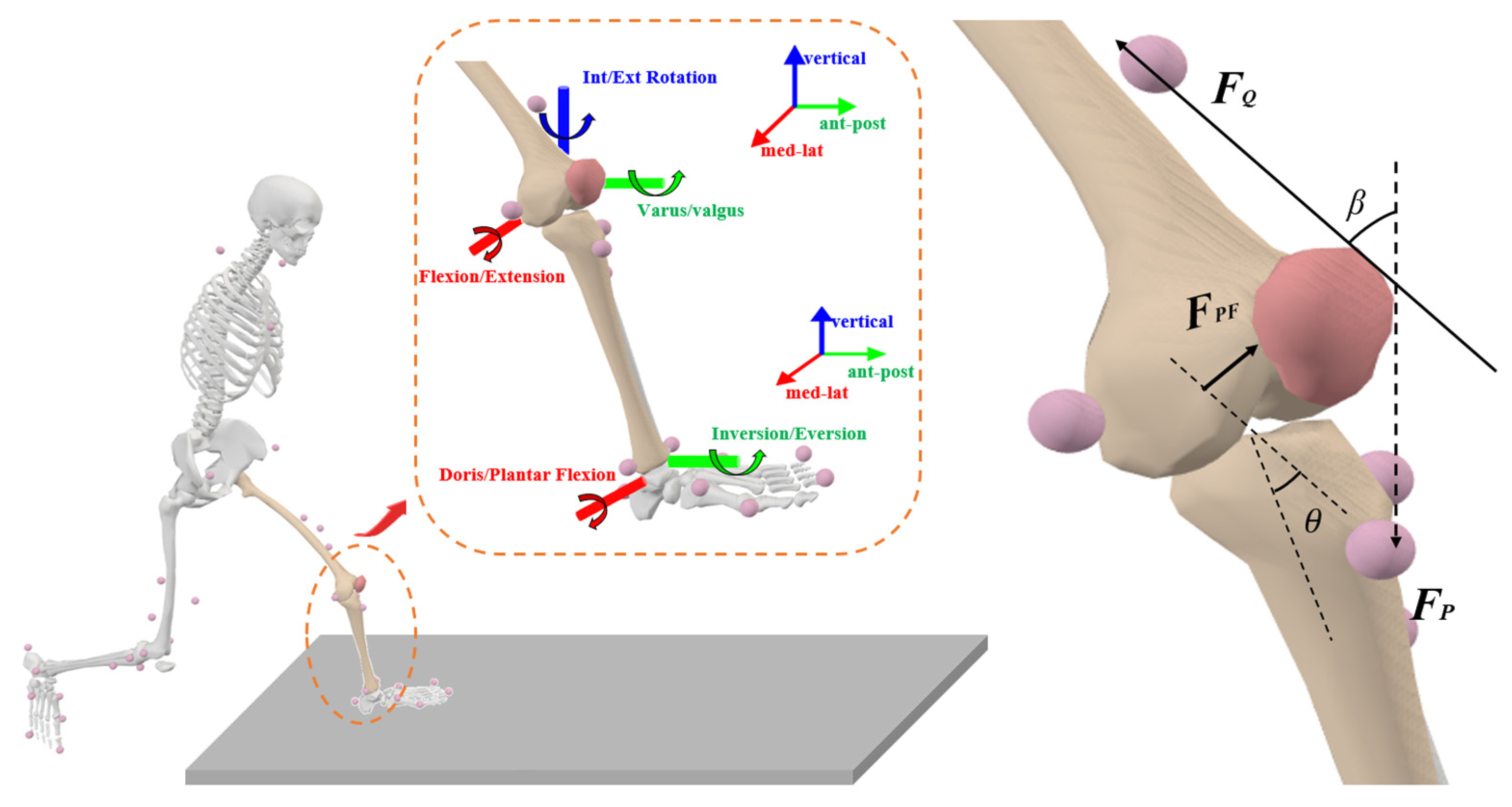
2.4. Data Processing
2.5. Statistical Analysis
3. Results
3.1. Joint Kinematics
3.2. Joint Kinetics
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Senter, C.; Hame, S.L. Biomechanical analysis of tibial torque and knee flexion angle: Implications for understanding knee injury. Sports Med. 2006, 36, 635–641. [Google Scholar] [CrossRef] [PubMed]
- Nakagawa, T.H.; Moriya, É.T.; Maciel, C.D.; Serrao, A. Frontal plane biomechanics in males and females with and without patellofemoral pain. Med. Sci. Sports Exerc. 2012, 44, 1747–1755. [Google Scholar] [CrossRef] [PubMed]
- Davis, I.S.; Powers, C. Patellofemoral pain syndrome: Proximal, distal, and local factors—International research retreat, April 30–May 2, 2009, Baltimore, Maryland. J. Orthop. Sports Phys. Ther. 2010, 40, A1–A48. [Google Scholar] [CrossRef]
- Post, W.R. Current concepts clinical evaluation of patients with patellofemoral disorders. Arthrosc. J. Arthrosc. Relat. Surg. 1999, 15, 841–851. [Google Scholar] [CrossRef] [PubMed]
- Halabchi, F.; Mazaheri, R.; Seif-Barghi, T. Patellofemoral pain syndrome and modifiable intrinsic risk factors; how to assess and address? Asian J. Sports Med. 2013, 4, 85. [Google Scholar] [CrossRef]
- Lankhorst, N.; van Middelkoop, M.; Crossley, K.; Bierma-Zeinstra, S.; Oei, E.; Vicenzino, B.; Collins, N. Factors that predict a poor outcome 5–8 years after the diagnosis of patellofemoral pain: A multicentre observational analysis. Br. J. Sports Med. 2016, 50, 881–886. [Google Scholar] [CrossRef]
- Utting, M.; Davies, G.; Newman, J. Is anterior knee pain a predisposing factor to patellofemoral osteoarthritis? Knee 2005, 12, 362–365. [Google Scholar] [CrossRef]
- Neal, B.S.; Lack, S.D.; Lankhorst, N.E.; Raye, A.; Morrissey, D.; Van Middelkoop, M. Risk factors for patellofemoral pain: A systematic review and meta-analysis. Br. J. Sports Med. 2019, 53, 270–281. [Google Scholar] [CrossRef]
- San Jose, A.J.; Maniar, N.; Whiteley, R.; Opar, D.A.; Timmins, R.G.; Kotsifaki, R. Lower Patellofemoral Joint Contact Force During Side-Step Cutting after Return-to-Sports Clearance Following Anterior Cruciate Ligament Reconstruction. Am. J. Sports Med. 2023, 51, 1777–1784. [Google Scholar] [CrossRef]
- Kong, L.; Wu, P.; Zhang, X.; Meng, L.; Kong, L.; Zhang, Q.; Shen, J. Effects of mental fatigue on biomechanical characteristics of lower extremities in patients with functional ankle instability during unanticipated side-step cutting. Front. Physiol. 2023, 14, 1123201. [Google Scholar] [CrossRef]
- Hase, K.; Stein, R. Turning strategies during human walking. J. Neurophysiol. 1999, 81, 2914–2922. [Google Scholar] [CrossRef] [PubMed]
- Leppänen, M.; Pasanen, K.; Kujala, U.M.; Vasankari, T.; Kannus, P.; Äyrämö, S.; Krosshaug, T.; Bahr, R.; Avela, J.; Perttunen, J. Stiff landings are associated with increased ACL injury risk in young female basketball and floorball players. Am. J. Sports Med. 2017, 45, 386–393. [Google Scholar] [CrossRef] [PubMed]
- Olsen, O.-E.; Myklebust, G.; Engebretsen, L.; Bahr, R. Injury mechanisms for anterior cruciate ligament injuries in team handball: A systematic video analysis. Am. J. Sports Med. 2004, 32, 1002–1012. [Google Scholar] [CrossRef] [PubMed]
- Beaulieu, M.L.; Lamontagne, M.; Xu, L. Lower limb muscle activity and kinematics of an unanticipated cutting manoeuvre: A gender comparison. Knee Surg. Sports Traumatol. Arthrosc. 2009, 17, 968–976. [Google Scholar] [CrossRef]
- Ford, K.R.; Myer, G.D.; Toms, H.E.; Hewett, T.E. Gender differences in the kinematics of unanticipated cutting in young athletes. Med. Sci. Sports Exerc. 2005, 37, 124–129. [Google Scholar] [CrossRef]
- Zebis, M.K.; Bencke, J.; Andersen, L.L.; Døssing, S.; Alkjær, T.; Magnusson, S.P.; Kjær, M.; Aagaard, P. The effects of neuromuscular training on knee joint motor control during sidecutting in female elite soccer and handball players. Clin. J. Sport Med. 2008, 18, 329–337. [Google Scholar] [CrossRef]
- Kim, J.H.; Lee, K.-K.; Kong, S.J.; An, K.O.; Jeong, J.H.; Lee, Y.S. Effect of anticipation on lower extremity biomechanics during side-and cross-cutting maneuvers in young soccer players. Am. J. Sports Med. 2014, 42, 1985–1992. [Google Scholar] [CrossRef]
- Besier, T.F.; Lloyd, D.G.; Ackland, T.R.; Cochrane, J.L. Anticipatory effects on knee joint loading during running and cutting maneuvers. Med. Sci. Sports Exerc. 2001, 33, 1176–1181. [Google Scholar] [CrossRef]
- Weinhandl, J.T.; Earl-Boehm, J.E.; Ebersole, K.T.; Huddleston, W.E.; Armstrong, B.S.; O’Connor, K.M. Anticipatory effects on anterior cruciate ligament loading during sidestep cutting. Clin. Biomech. 2013, 28, 655–663. [Google Scholar] [CrossRef]
- Houck, J.R.; Duncan, A.; Kenneth, E. Comparison of frontal plane trunk kinematics and hip and knee moments during anticipated and unanticipated walking and side step cutting tasks. Gait Posture 2006, 24, 314–322. [Google Scholar] [CrossRef]
- Powers, C.M.; Witvrouw, E.; Davis, I.S.; Crossley, K.M. Evidence-based framework for a pathomechanical model of patellofemoral pain: 2017 patellofemoral pain consensus statement from the 4th International Patellofemoral Pain Research Retreat, Manchester, UK: Part 3. Br. J. Sports Med. 2017, 51, 1713–1723. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.-X.; Liu, H.-B.; Zhao, Z.-N.; Wang, Y.-B.; Luan, Z.-L. Effects of movement direction and limb dominance on ankle muscular force in sidestep cutting. Med. Eng. Phys. 2022, 110, 103914. [Google Scholar] [CrossRef] [PubMed]
- Havens, K.L.; Sigward, S.M. Cutting mechanics: Relation to performance and anterior cruciate ligament injury risk. Med. Sci. Sports Exerc. 2015, 47, 818–824. [Google Scholar] [CrossRef] [PubMed]
- Dutton, R.A.; Khadavi, M.J.; Fredericson, M. Patellofemoral pain. Phys. Med. Rehabil. Clin. 2016, 27, 31–52. [Google Scholar] [CrossRef] [PubMed]
- Suda, E.Y.; Hirata, R.P.; Palsson, T.; Vuillerme, N.; Sacco, I.C.; Graven-Nielsen, T. Experimental knee-related pain enhances attentional interference on postural control. Eur. J. Appl. Physiol. 2019, 119, 2053–2064. [Google Scholar] [CrossRef]
- Maniar, N.; Schache, A.G.; Cole, M.H.; Opar, D.A. Lower-limb muscle function during sidestep cutting. J. Biomech. 2019, 82, 186–192. [Google Scholar] [CrossRef]
- Dierks, T.A.; Manal, K.T.; Hamill, J.; Davis, I. Lower extremity kinematics in runners with patellofemoral pain during a prolonged run. Med. Sci. Sports Exerc. 2011, 43, 693–700. [Google Scholar] [CrossRef]
- Freddolini, M.; Placella, G.; Gervasi, G.; Morello, S.; Cerulli, G. Quadriceps muscles activity during gait: Comparison between PFPS subjects and healthy control. Musculoskelet. Surg. 2017, 101, 181–187. [Google Scholar] [CrossRef]
- Kuriki, H.U.; de Azevedo, F.M.; de Faria Negrão Filho, R.; Alves, N. Comparison of different analysis techniques for the determination of muscle onset in individuals with patellofemoral pain syndrome. J. Electromyogr. Kinesiol. 2011, 21, 982–987. [Google Scholar] [CrossRef]
- Willy, R.W.; Manal, K.T.; Witvrouw, E.E.; Davis, I.S. Are mechanics different between male and female runners with patellofemoral pain? Med. Sci. Sports Exerc. 2012, 44, 2165. [Google Scholar] [CrossRef]
- Brown, S.R.; Brughelli, M.; Hume, P.A. Knee mechanics during planned and unplanned sidestepping: A systematic review and meta-analysis. Sports Med. 2014, 44, 1573–1588. [Google Scholar] [CrossRef] [PubMed]
- Doyle, E. Appraisal of clinical practice guideline: Patellofemoral pain: Clinical practice guidelines linked to the international classification of functioning, disability and health from the academy of orthopaedic physical therapy of the American physical therapy association. J. Physiother. 2020, 66, 134. [Google Scholar] [CrossRef] [PubMed]
- Yu, P.; Fernandez, J. Alterations in Lower Limb Biomechanical Characteristics during the Cutting Manoeuvre in Chronic Ankle Instability Population and Copers. Phys. Act. Health 2024, 8, 148–156. [Google Scholar] [CrossRef]
- Quan, W.; Gao, L.; Xu, D.; Zhou, H.; Korim, T.; Shao, S.; Baker, J.S.; Gu, Y. Simulation of lower limb muscle activation using running shoes with different heel-to-toe drops using opensim. Healthcare 2023, 11, 1243. [Google Scholar] [CrossRef] [PubMed]
- Whyte, E.F.; Richter, C.; O’Connor, S.; Moran, K.A. The effect of high intensity exercise and anticipation on trunk and lower limb biomechanics during a crossover cutting manoeuvre. J. Sports Sci. 2018, 36, 889–900. [Google Scholar] [CrossRef]
- Quan, W.; Ren, F.; Xu, D.; Gusztav, F.; Baker, J.S.; Gu, Y. Effects of fatigue running on joint mechanics in female runners: A prediction study based on a partial least squares algorithm. Front. Bioeng. Biotechnol. 2021, 9, 746761. [Google Scholar] [CrossRef]
- Yu, L.; Wang, Y.; Fernandez, J.; Mei, Q.; Zhao, J.; Yang, F.; Gu, Y. Dose–response effect of incremental lateral-wedge hardness on the lower limb Biomechanics during typical badminton footwork. J. Sports Sci. 2023, 41, 972–989. [Google Scholar] [CrossRef]
- Liew, B.X.; Sullivan, L.; Morris, S.; Netto, K. Lower-limb stiffness mediates speed but not turning angle during unplanned side-step cutting. J. Biomech. 2021, 115, 110132. [Google Scholar] [CrossRef]
- Kim, H.; Son, S.; Seeley, M.; Hopkins, J. Functional fatigue alters lower-extremity neuromechanics during a forward-side jump. Int. J. Sports Med. 2015, 36, 1192–1200. [Google Scholar] [CrossRef]
- Trinler, U.; Schwameder, H.; Baker, R.; Alexander, N. Muscle force estimation in clinical gait analysis using AnyBody and OpenSim. J. Biomech. 2019, 86, 55–63. [Google Scholar] [CrossRef]
- Mei, Q.; Gu, Y.; Xiang, L.; Baker, J.S.; Fernandez, J. Foot pronation contributes to altered lower extremity loading after long distance running. Front. Physiol. 2019, 10, 573. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Mei, Q.; Peng, H.-T.; Li, J.; Wei, C.; Gu, Y. A comparative study on loadings of the lower extremity during deep squat in Asian and Caucasian individuals via OpenSim musculoskeletal modelling. BioMed Res. Int. 2020, 2020, 7531719. [Google Scholar] [CrossRef]
- Hall, M.; Diamond, L.E.; Lenton, G.K.; Pizzolato, C.; Saxby, D.J. Immediate effects of valgus knee bracing on tibiofemoral contact forces and knee muscle forces. Gait Posture 2019, 68, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Hamill, J.; Gruber, A.H.; Derrick, T.R. Lower extremity joint stiffness characteristics during running with different footfall patterns. Eur. J. Sport Sci. 2014, 14, 130–136. [Google Scholar] [CrossRef] [PubMed]
- Bonacci, J.; Vicenzino, B.; Spratford, W.; Collins, P. Take your shoes off to reduce patellofemoral joint stress during running. Br. J. Sports Med. 2014, 48, 425–428. [Google Scholar] [CrossRef]
- Nunes, G.S.; de Oliveira Silva, D.; Pizzari, T.; Serrão, F.V.; Crossley, K.M.; Barton, C.J. Clinically measured hip muscle capacity deficits in people with patellofemoral pain. Phys. Ther. Sport 2019, 35, 69–74. [Google Scholar] [CrossRef]
- Patla, A.E.; Adkin, A.; Ballard, T. Online steering: Coordination and control of body center of mass, head and body reorientation. Exp. Brain Res. 1999, 129, 629–634. [Google Scholar] [CrossRef]
- McLean, S.G.; Neal, R.J.; Myers, P.T.; Walters, M.R. Knee joint kinematics during the sidestep cutting maneuver: Potential for injury in women. Med. Sci. Sports Exerc. 1999, 31, 959–968. [Google Scholar] [CrossRef]
- Sigward, S.M.; Powers, C.M. The influence of gender on knee kinematics, kinetics and muscle activation patterns during side-step cutting. Clin. Biomech. 2006, 21, 41–48. [Google Scholar] [CrossRef]
- Park, E.-J.; Lee, J.-H.; Ryue, J.-J.; Sohn, J.-H.; Lee, K.-K. Influence of anticipation on landing patterns during side-cutting maneuver in female collegiate soccer players. Korean J. Sport Biomech. 2011, 21, 391–395. [Google Scholar] [CrossRef]
- Cortes, N.; Blount, E.; Ringleb, S.; Onate, J.A. Soccer-specific video simulation for improving movement assessment. Sports Biomech. 2011, 10, 22–34. [Google Scholar] [CrossRef] [PubMed]
- Borotikar, B.S.; Newcomer, R.; Koppes, R.; McLean, S.G. Combined effects of fatigue and decision making on female lower limb landing postures: Central and peripheral contributions to ACL injury risk. Clin. Biomech. 2008, 23, 81–92. [Google Scholar] [CrossRef] [PubMed]
- Shultz, S.J.; Carcia, C.R.; Gansneder, B.M.; Perrin, D.H. The independent and interactive effects of navicular drop and quadriceps angle on neuromuscular responses to a weight-bearing perturbation. J. Athl. Train. 2006, 41, 251. [Google Scholar] [PubMed]
- Ford, K.R.; Myer, G.D.; Hewett, T.E. Valgus knee motion during landing in high school female and male basketball players. Med. Sci. Sports Exerc. 2003, 35, 1745–1750. [Google Scholar] [CrossRef] [PubMed]
- Collins, J.D.; Almonroeder, T.G.; Ebersole, K.T.; O’Connor, K.M. The effects of fatigue and anticipation on the mechanics of the knee during cutting in female athletes. Clin. Biomech. 2016, 35, 62–67. [Google Scholar] [CrossRef]
- Havens, K.L.; Sigward, S.M. Joint and segmental mechanics differ between cutting maneuvers in skilled athletes. Gait Posture 2015, 41, 33–38. [Google Scholar] [CrossRef]
- Giesche, F.; Stief, F.; Groneberg, D.A.; Wilke, J. Effect of unplanned athletic movement on knee mechanics: A systematic review with multilevel meta-analysis. Br. J. Sports Med. 2021, 55, 1366–1378. [Google Scholar] [CrossRef]
- Li, G.; DeFrate, L.; Zayontz, S.; Park, S.; Gill, T. The effect of tibiofemoral joint kinematics on patellofemoral contact pressures under simulated muscle loads. J. Orthop. Res. 2004, 22, 801–806. [Google Scholar] [CrossRef]
- Besier, T.F.; Lloyd, D.G.; Cochrane, J.L.; Ackland, T.R. External loading of the knee joint during running and cutting maneuvers. Med. Sci. Sports Exerc. 2001, 33, 1168–1175. [Google Scholar] [CrossRef]
- Pandy, M.G.; Lin, Y.-C.; Kim, H.J. Muscle coordination of mediolateral balance in normal walking. J. Biomech. 2010, 43, 2055–2064. [Google Scholar] [CrossRef]
- Neptune, R.; Zajac, F.; Kautz, S. Muscle force redistributes segmental power for body progression during walking. Gait Posture 2004, 19, 194–205. [Google Scholar] [CrossRef] [PubMed]
- Zajac, F.E.; Gordon, M.E. Determining muscle’s force and action in multi-articular movement. Exerc. Sport Sci. Rev. 1989, 17, 187–230. [Google Scholar] [CrossRef] [PubMed]
- Li, G.; Rudy, T.; Sakane, M.; Kanamori, A.; Ma, C.; Woo, S.-Y. The importance of quadriceps and hamstring muscle loading on knee kinematics and in-situ forces in the ACL. J. Biomech. 1999, 32, 395–400. [Google Scholar] [CrossRef] [PubMed]






| Variables (°) | Anticipated | Unanticipated | p-Value | t | |
|---|---|---|---|---|---|
| Peak ankle angle | Dorsiflexion | 23.67 ± 5.10 | 25.28 ± 4.00 | 0.036 * | −2.141 |
| Plantarflexion | −25.59 ± 6.20 | −32.02 ± 6.57 | <0.001 * | 5.633 | |
| Inversion | −6.89 ± 4.76 | −4.10 ± 5.09 | 0.003 * | −3.089 | |
| Eversion | −22.51 ± 7.70 | −17.41 ± 4.28 | <0.001 * | −4.766 | |
| Internal rotation | 5.27 ± 2.52 | 5.37 ± 2.28 | 0.769 | −0.295 | |
| External rotation | −8.43 ± 3.81 | −7.89 ± 2.82 | 0.386 | −0.873 | |
| Peak knee angle | Flexion | −57.49 ± 6.37 | −58.37 ± 5.40 | 0.349 | −0.943 |
| Adduction | −5.50 ± 2.72 | 3.47 ± 1.86 | <0.001 * | −4.812 | |
| Abduction | −1.37 ± 3.35 | −3.70 ± 2.77 | <0.001 * | −6.200 | |
| Internal rotation | 7.14 ± 5.87 | 9.44 ± 5.27 | 0.003 * | 3.094 | |
| External rotation | −8.69 ± 4.19 | −7.28 ± 4.06 | 0.052 | 1.984 | |
| Peak hip angle | Flexion | −14.63 ± 7.31 | −15.75 ± 7.85 | 0.275 | 4.897 |
| Adduction | 18.15 ± 4.52 | 15.70 ± 3.81 | <0.001 * | 3.619 | |
| Abduction | −0.59 ± 4.01 | −2.69 ± 3.04 | 0.005 * | 2.911 | |
| Internal rotation | 6.93 ± 6.37 | 5.42 ± 3.21 | 0.073 | 1.823 | |
| External rotation | −8.78 ± 5.09 | −9.04 ± 3.03 | 0.686 | 0.406 | |
| Variables (°) | Anticipated | Unanticipated | p-Value | t | |
|---|---|---|---|---|---|
| ROM of ankle | Sagittal plane | 49.26 ± 8.17 | 57.30 ± 7.24 | <0.001 * | −5.470 |
| Frontal plane | 15.62 ± 5.70 | 13.31 ± 3.89 | 0.008 * | 2.743 | |
| Transverse plane | 13.70 ± 3.65 | 13.26 ± 2.96 | 0.481 | 0.708 | |
| ROM of knee | Sagittal plane | 43.68 ± 5.60 | 45.43 ± 6.68 | 0.112 | 1.161 |
| Frontal plane | 6.86 ± 1.84 | 7.44 ± 2.32 | 0.069 | 1.851 | |
| Transverse plane | 15.82 ± 4.28 | 16.72 ± 3.65 | 0.126 | 1.553 | |
| ROM of hip | Sagittal plane | 62.16 ± 8.33 | 59.23 ± 10.30 | 0.023 * | 2.337 |
| Frontal plane | 18.74 ± 5.04 | 18.39 ± 5.08 | 0.591 | 0.540 | |
| Transverse plane | 15.17 ± 5.42 | 14.46 ± 3.67 | 0.144 | 1.481 | |
| Variables | Anticipated | Unanticipated | p-Value | t | |
|---|---|---|---|---|---|
| Ankle | Dorsiflexion/Plantarflexion (°) | 7.47 ± 4.89 | 7.57 ± 3.85 | 0.914 | −0.109 |
| Inversion/Eversion (°) | −9.06 ± 5.74 | −6.53 ± 5.11 | 0.011 * | −2.612 | |
| Internal/External rotation (°) | −0.29 ± 3.05 | −0.34 ± 3.02 | 0.921 | 0.100 | |
| Knee | Flexion/Extension (°) | −24.80 ± 6.93 | −27.15 ± 6.76 | 0.094 | −1.700 |
| Adduction/Abduction (°) | −0.75 ± 3.10 | −2.19 ± 2.36 | <0.001 * | −3.816 | |
| Internal/External rotation (°) | 4.29 ± 6.06 | 6.00 ± 4.09 | 0.041 | 2.089 | |
| Hip | Flexion/Extension (°) | 47.53 ± 5.47 | 43.01 ± 4.63 | <0.001 * | 3.593 |
| Adduction/Abduction (°) | 2.74 ± 4.10 | −0.34 ± 3.46 | <0.001 * | 5.013 | |
| Internal/External rotation (°) | 3.39 ± 4.78 | −4.31 ± 4.30 | 0.134 | 1.518 | |
| Variables | Anticipated | Unanticipated | p-Value | t | |
|---|---|---|---|---|---|
| Peak ankle moment | Dorsiflexion (Nm/BW) | 0.43 ± 0.42 | 0.43 ± 0.39 | 0.883 | 0.148 |
| Plantarflexion (Nm/BW) | −2.76 ± 0.53 | −2.72 ± 0.55 | 0.557 | 0.590 | |
| Inversion (Nm/BW) | 0.31 ± 0.22 | 0.61 ± 0.39 | <0.001 * | 6.412 | |
| Eversion (Nm/BW) | −0.25 ± 0.23 | −0.14 ± 0.21 | <0.001 * | 3.559 | |
| Internal rotation (Nm/BW) | 0.48 ± 0.27 | 0.66 ± 0.33 | <0.001 * | 3.799 | |
| External rotation (Nm/BW) | −0.12 ± 0.09 | −0.10 ± 0.09 | 0.360 | 0.923 | |
| Peak knee moment | Extension (Nm/BW) | 3.66 ± 0.63 | 4.17 ± 0.54 | <0.001 * | 4.383 |
| Flexion (Nm/BW) | −0.67 ± 0.33 | −0.50 ± 0.23 | 0.002 * | 3.266 | |
| Adduction (Nm/BW) | 0.53 ± 0.30 | 0.86 ± 0.48 | <0.001 * | 4.963 | |
| Abduction (Nm/BW) | −0.57 ± 0.35 | −0.59 ± 0.46 | 0.707 | −0.377 | |
| Internal rotation (Nm/BW) | 0.31 ± 0.22 | 0.31 ± 0.38 | 0.946 | −0.068 | |
| External rotation (Nm/BW) | −0.47 ± 0.26 | −0.91 ± 0.33 | 0.001 * | −3.376 | |
| Peak. hip moment | Extension (Nm/BW) | 1.28 ± 0.64 | 1.46 ± 0.76 | 0.160 | −1.424 |
| Flexion (Nm/BW) | −4.49 ± 0.88 | −4.90 ± 0.98 | 0.026 * | 2.276 | |
| Adduction (Nm/BW) | 1.53 ± 0.77 | 1.46 ± 0.62 | 0.543 | 0.612 | |
| Abduction (Nm/BW) | −1.24 ± 1.10 | −1.01 ± 0.62 | 0.087 | −1.743 | |
| Internal rotation (Nm/BW) | 1.66 ± 0.60 | 1.73 ± 0.63 | 0.563 | −0.592 | |
| External rotation (Nm/BW) | −0.47 ± 0.25 | −0.59 ± 0.42 | 0.028 * | 2.259 | |
| Parameters | Anticipated | Unanticipated | p-Value |
|---|---|---|---|
| Peak PTF (N) | 5.25 ± 1.41 | 6.10 ± 2.12 | 0.022 * |
| Peak PFCA (cm2) | 4.25 ± 0.46 | 4.00 ± 0.50 | 0.013 * |
| Peak PP (MPa) | 12.83 ± 4.52 | 15.93 ± 7.20 | 0.011 * |
| Ankle stiffness (Nm·(°)−1·kg−1) | 0.06 ± 0.01 | 0.07 ± 0.01 | <0.001 * |
| Knee stiffness (Nm·(°)−1·kg−1) | 0.10 ± 0.02 | 0.11 ± 0.02 | 0.214 |
| Hip stiffness (Nm·(°)−1·kg−1) | 0.11 ± 0.03 | 0.09 ± 0.02 | 0.002 * |
| Parameters | Anticipated | Unanticipated | p-Value |
|---|---|---|---|
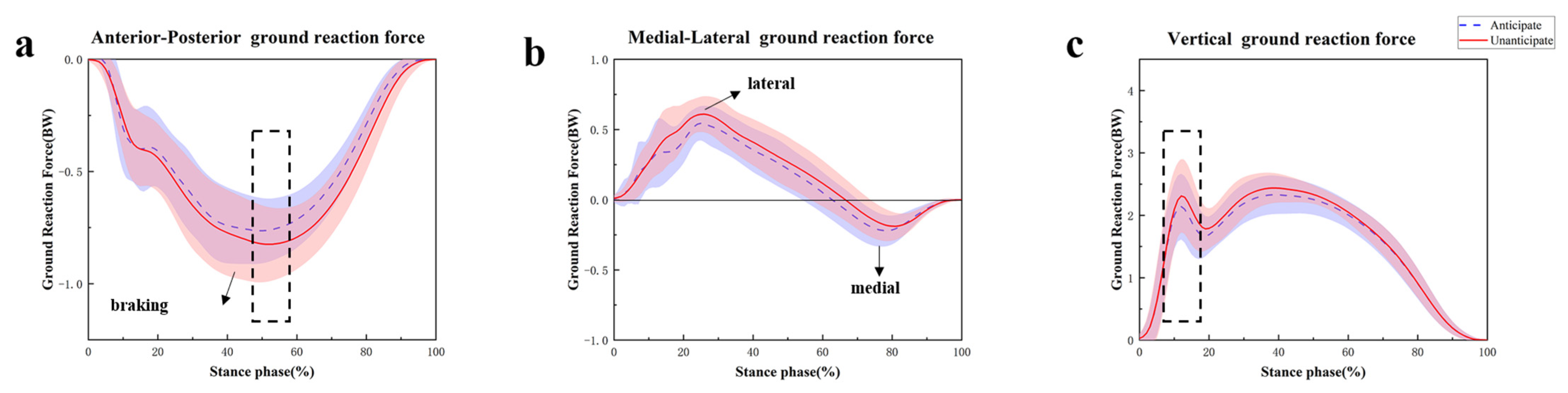
| Peak Breaking Force (BW) | −0.79 ± 0.14 | −0.84 ± 0.16 | 0.034 * |
| Peak Lateral Force (BW) | 0.64 ± 0.21 | 0.68 ± 0.13 | 0.173 |
| Peak Medial Force (BW) | −0.23 ± 0.10 | −0.20 ± 0.09 | 0.073 |
| Peak Vertical Force (BW) | 2.59 ± 0.30 | 2.72 ± 0.38 | 0.011 * |
| Parameters | Anticipated | Unanticipated | p-Value |
|---|---|---|---|
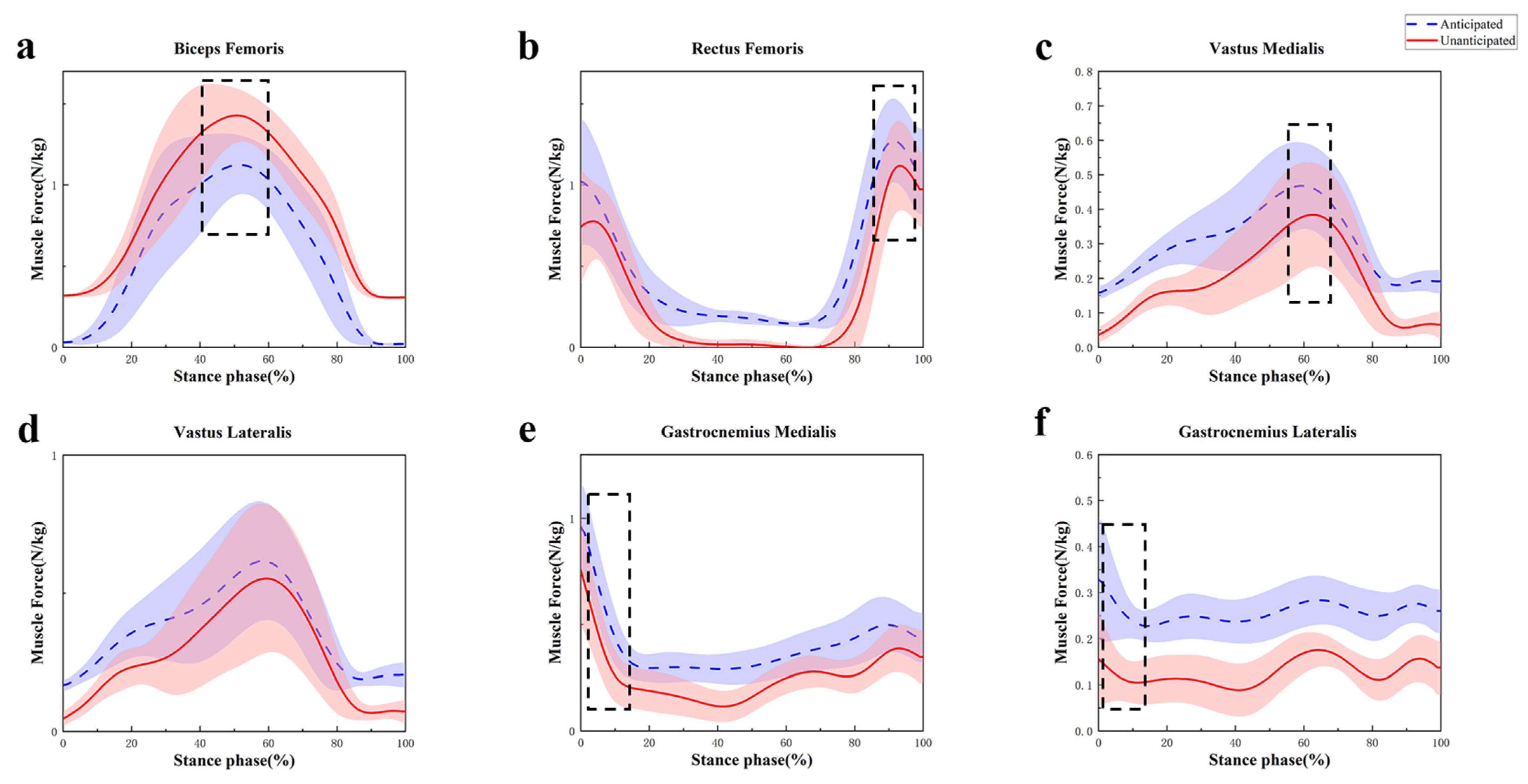
| Biceps femoris (BF) | 1.19 ± 0.22 | 1.49 ± 0.18 | <0.001 * |
| Rectus femoris (RF) | 1.36 ± 0.26 | 1.17 ± 0.26 | <0.001 * |
| Vastus medialis (VM) | 0.50 ± 0.14 | 0.42 ± 0.15 | <0.001 * |
| Vastus lateralis (VL) | 0.67 ± 0.24 | 0.63 ± 0.25 | 0.075 |
| Gastrocnemius medialis (GM) | 0.96 ± 0.21 | 0.76 ± 0.24 | <0.001 * |
| Gastrocnemius lateralis (GL) | 0.38 ± 0.08 | 0.24 ± 0.05 | <0.001 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ma, Y.; Quan, W.; Wang, X.; Baker, J.S.; Gao, Z.; Gu, Y. Effect of Unanticipated Tasks on Side-Cutting Stability of Lower Extremity with Patellofemoral Pain Syndrome. Sensors 2024, 24, 6427. https://doi.org/10.3390/s24196427
Ma Y, Quan W, Wang X, Baker JS, Gao Z, Gu Y. Effect of Unanticipated Tasks on Side-Cutting Stability of Lower Extremity with Patellofemoral Pain Syndrome. Sensors. 2024; 24(19):6427. https://doi.org/10.3390/s24196427
Chicago/Turabian StyleMa, Yiwen, Wenjing Quan, Xuting Wang, Julien S. Baker, Zixiang Gao, and Yaodong Gu. 2024. "Effect of Unanticipated Tasks on Side-Cutting Stability of Lower Extremity with Patellofemoral Pain Syndrome" Sensors 24, no. 19: 6427. https://doi.org/10.3390/s24196427








