Non-Invasive Diagnostic Approaches for Kidney Disease: The Role of Electronic Nose Systems
Abstract
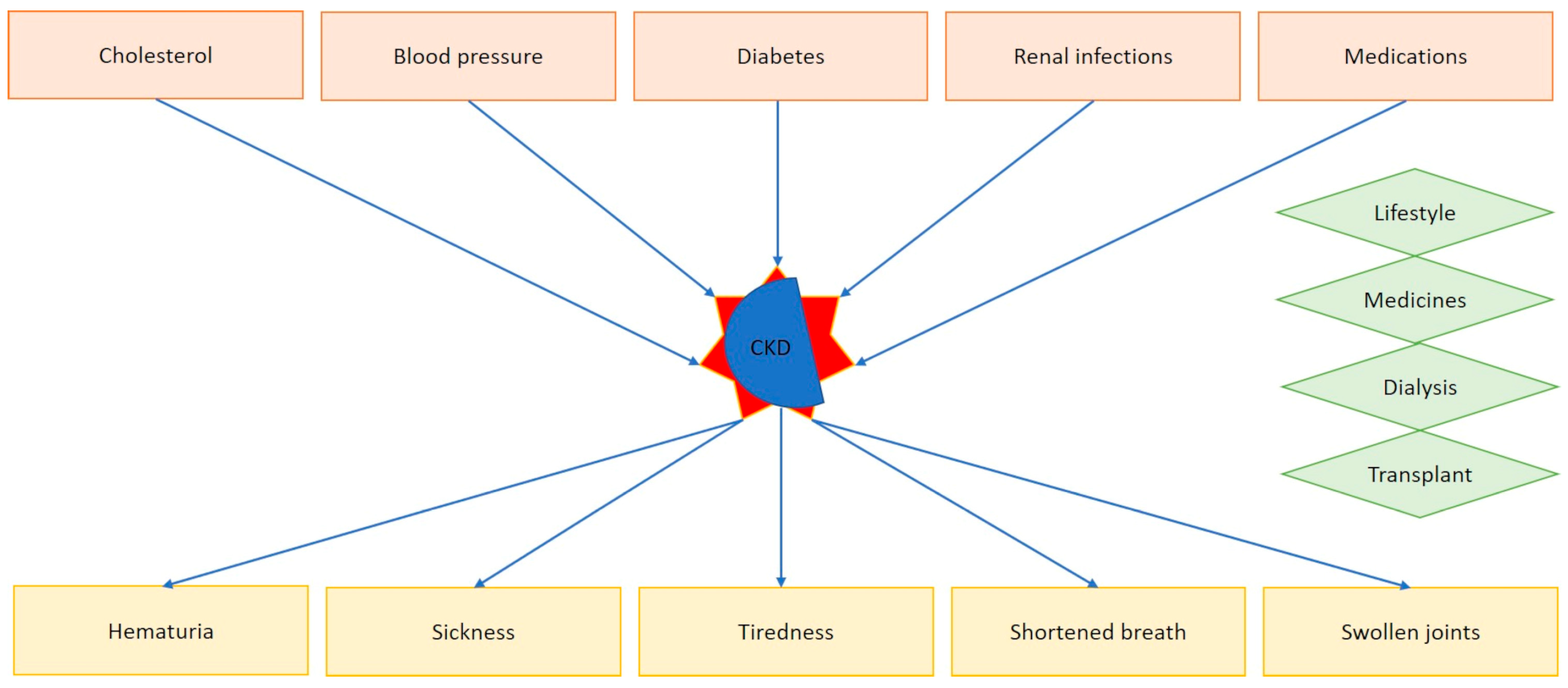
:1. Introduction
2. The Electronic Nose
2.1. The Historical Perspective: From the Ancient Age to the Modern Era
2.2. The e-Nose Sensing Part: Principle of Operation
Novel Sensing Devices Eventually Applied to e-Nose Systems
2.3. The e-Nose Intelligent Part: Most Popular Models and Their Main Characteristics
2.3.1. Principal Component Analysis
2.3.2. Support Vector Machine
2.3.3. Artificial Neural Networks
2.3.4. Linear Discriminant Analysis
2.3.5. k-Nearest Neighbors
2.3.6. Random Forest
2.3.7. Novel AI Models to Be Applied to e-Nose Systems
2.4. Validation: A Crucial Step for e-Nose Systems
3. Materials and Methods
4. Biomarkers of Chronic Kidney Disease
5. Electronic Nose Tools and Chronic Kidney Disease
6. Discussion
7. Conclusions and Future Perspectives
Author Contributions
Funding
Conflicts of Interest
References
- Pan American Health Organization, Chronic Kidney Disease. Available online: https://www.paho.org/en/topics/chronic-kidney-disease (accessed on 17 July 2024).
- Lv, J.C.; Zhang, L.X. Prevalence and Disease Burden of Chronic Kidney Disease. Adv. Exp. Med. Biol. 2019, 1165, 3–15. [Google Scholar] [CrossRef] [PubMed]
- NHS, Chronic Kidney Disease. Available online: https://www.nhs.uk/conditions/kidney-disease/ (accessed on 17 July 2024).
- Li, L.; Wang, J.; Feng, F.; Yan, J.; Zhao, B.; Li, X.; Zhong, Y. Breath volatile organic compounds for chronic kidney disease progression monitoring. Analyst 2024, 149, 1074–1080. [Google Scholar] [CrossRef] [PubMed]
- Wijaya, D.R.; Afianti, F.; Arifianto, A.; Rahmawati, D.; Kodogiannis, V.S. Ensemble machine learning approach for electronic nose signal processing. Sens. Bio-Sens. Res. 2022, 36, 100495. [Google Scholar] [CrossRef]
- Liu, T.; Guo, L.; Wang, M.; Su, C.; Wang, D.; Dong, H.; Chen, J.; Wu, W. Review on algorithm design in electronic noses: Challenges, status, and trends. Intell. Comput. 2023, 2, 0012. [Google Scholar] [CrossRef]
- Ziporyn, T. Taste and smell: The neglected senses. JAMA 1982, 247, 277–279, 282–285. [Google Scholar] [CrossRef]
- Hawkes, C. Olfaction in neurodegenerative disorder. Mov. Disord. 2003, 18, 364–372. [Google Scholar] [CrossRef]
- Persaud, K.; Dodd, G. Analysis of discrimination mechanisms in the mammalian olfactory system using a model nose. Nature 1982, 299, 352–355. [Google Scholar] [CrossRef]
- Gardner, J.W.; Bartlett, P.N. A brief history of electronic noses. Sens. Actuators B Chem. 1994, 18, 210–211. [Google Scholar] [CrossRef]
- Atanasio, M.; Sansone, F.; Conte, R.; Tonacci, A. Exploring Taste Sensation in the Metaverse: A Literature Review. In Proceedings of the 2024 IEEE Gaming, Entertainment, and Media Conference (GEM), Turin, Italy, 5–7 June 2024. [Google Scholar]
- Ward, R.J.; Rahman, S.; Wuerger, S.; Marshall, A. Predicting the crossmodal correspondences of odors using an electronic nose. Heliyon 2022, 8, e09284. [Google Scholar] [CrossRef]
- Tran, V.H.; Chan, H.P.; Thurston, M.; Jackson, P.; Lewis, C.; Yates, D.; Bell, G.; Thomas, P.S. Breath analysis of lung cancer patients using an electronic nose detection system. IEEE Sens. J. 2010, 10, 1514–1518. [Google Scholar] [CrossRef]
- Modesti, M.; Taglieri, I.; Bianchi, A.; Tonacci, A.; Sansone, F.; Bellincontro, A.; Venturi, F.; Sanmartin, C. E-nose and olfactory assessment: Teamwork or a challenge to the last data? The case of virgin olive oil stability and shelf life. Appl. Sci. 2021, 11, 8453. [Google Scholar] [CrossRef]
- Tonacci, A.; Corda, D.; Tartarisco, G.; Pioggia, G.; Domenici, C. A smart sensor system for detecting hydrocarbon volatile organic compounds in sea water. CLEAN–Soil Air Water 2015, 43, 147–152. [Google Scholar] [CrossRef]
- Arshak, K.I.; Cunniffe, C.; Moore, E.G.; Cavanagh, L.M. Custom electronic nose with potential homeland security applications. In Proceedings of the 2006 IEEE Sensors Applications Symposium, Houston, TX, USA, 7–9 February 2006. [Google Scholar]
- Furizal, F.; Ma’arif, A.; Firdaus, A.A.; Rahmaniar, W. Future potential of E-nose technology: A review. Int. J. Robot. Control. Syst. 2023, 3, 449–469. [Google Scholar] [CrossRef]
- Wijaya, D.R.; Sarno, R.; Zulaika, E.; Sabila, S.I. Development of mobile electronic nose for beef quality monitoring. Procedia Comput. Sci. 2017, 124, 728–735. [Google Scholar] [CrossRef]
- Freddi, S.; Marzuoli, C.; Pagliara, S.; Drera, G.; Sangaletti, L. Targeting biomarkers in the gas phase through a chemo-resistive electronic nose based on graphene functionalized with metal phthalocyanines. RSC Adv. 2022, 13, 251–263. [Google Scholar] [CrossRef]
- Gaggiotti, S.; Scroccarello, A.; Della Pelle, F.; Ferraro, G.; Del Carlo, M.; Mascini, M.; Cichelli, A.; Compagnone, D. An electronic nose based on 2D group VI transition metal dichalcogenides/organic compounds sensor array. Biosens. Bioelectron. 2022, 218, 114749. [Google Scholar] [CrossRef]
- Pineau, N.J.; Kompalla, J.F.; Güntner, A.T.; Pratsinis, S.E. Orthogonal gas sensor arrays by chemoresistive material design. Microchim. Acta 2018, 185, 563. [Google Scholar] [CrossRef]
- Chen, J.; Chen, Z.; Boussaid, F.; Zhang, D.; Pan, X.; Zhao, H.; Bermak, A.; Tsui, C.H.; Wang, X.; Fan, Z. Ultra-low-power smart electronic nose system based on three-dimensional tin oxide nanotube arrays. ACS Nano 2018, 12, 6079–6088. [Google Scholar] [CrossRef]
- Wang, J.; Ren, Y.; Liu, H.; Li, Z.; Liu, X.; Deng, Y.; Fang, X. Ultrathin 2D NbWO 6 perovskite semiconductor-based gas sensors with ultrahigh selectivity under low working temperature. Adv. Mater. 2022, 34, 2104958. [Google Scholar] [CrossRef]
- Kou, L.; Frauenheim, T.; Chen, C. Phosphorene as a superior gas sensor: Selective adsorption and distinct i- V response. J. Phys. Chem. Lett. 2014, 5, 2675–2681. [Google Scholar] [CrossRef]
- Yang, T.; Liu, Y.; Wang, H.; Duo, Y.; Zhang, B.; Ge, Y.; Zhang, H.; Chen, W. Recent advances in 0D nanostructure functionalized low-dimensional nanomaterials for chemiresistive gas sensors. J. Mater. Chem. C 2020, 8, 7272–7299. [Google Scholar] [CrossRef]
- Fu, X.; Yang, P.; Xiao, X.; Zhou, D.; Huang, R.; Zhang, X.; Cao, F.; Xiong, J.; Hu, Y.; Tu, Y.; et al. Ultra-fast and highly selective room-temperature formaldehyde gas sensing of Pt-decorated MoO3 nanobelts. J. Alloys Compd. 2019, 797, 666–675. [Google Scholar] [CrossRef]
- Li, T.; Yin, W.; Gao, S.; Sun, Y.; Xu, P.; Wu, S.; Kong, H.; Yang, G.; Wei, G. The Combination of Two-Dimensional Nanomaterials with Metal Oxide Nanoparticles for Gas Sensors: A Review. Nanomaterials 2022, 12, 982. [Google Scholar] [CrossRef]
- Zhou, T.; Zhang, T. Recent progress of nanostructured sensing materials from 0D to 3D: Overview of structure-property-application relationship for gas sensors. Small Methods 2021, 5, 2100515. [Google Scholar] [CrossRef] [PubMed]
- Nikolic, M.V.; Milovanovic, V.; Vasiljevic, Z.Z.; Stamenkovic, Z. Semiconductor gas sensors: Materials, technology, design, and application. Sensors 2020, 20, 6694. [Google Scholar] [CrossRef] [PubMed]
- Ren, P.; Qi, L.; You, K.; Shi, Q. Hydrothermal synthesis of hierarchical SnO2 nanostructures for improved formaldehyde gas sensing. Nanomaterials 2022, 12, 228. [Google Scholar] [CrossRef]
- Parichenko, A.; Huang, S.; Pang, J.; Ibarlucea, B.; Cuniberti, G. Recent advances in technologies toward the development of 2D materials-based electronic noses. TrAC Trends Anal. Chem. 2023, 166, 117185. [Google Scholar] [CrossRef]
- Borràs, E.; Ferré, J.; Boqué, R.; Mestres, M.; Aceña, L.; Busto, O. Data fusion methodologies for food and beverage authentication and quality assessment—A review. Anal. Chim. Acta 2015, 891, 1–14. [Google Scholar] [CrossRef]
- Śliwińska, M.; Wiśniewska, P.; Dymerski, T.; Namieśnik, J.; Wardencki, W. Food Analysis Using Artificial Senses. J. Agric. Food Chem. 2014, 62, 1423–1448. [Google Scholar] [CrossRef]
- Zou, Y.; Wan, H.; Zhang, X.; Ha, D.; Wang, P. Electronic Nose and Electronic Tongue. In Bioinspired Smell and Taste Sensors; Springer: Dordrecht, The Netherlands, 2015; pp. 19–44. [Google Scholar]
- Zakaria, A.; Shakaff, A.Y.; Masnan, M.J.; Saad, F.S.; Adom, A.H.; Ahmad, M.N.; Jaafar, M.N.; Abdullah, A.H.; Kam-arudin, L.M. Improved Maturity and Ripeness Classifications of Magnifera Indica cv. Harumanis Mangoes through Sensor Fusion of an Electronic Nose and Acoustic Sensor. Sensors 2012, 12, 6023–6048. [Google Scholar] [CrossRef]
- Kim, S.J.; Choi, S.J.; Jang, J.S.; Cho, H.J.; Kim, I.D. Innovative nanosensor for disease diagnosis. Acc. Chem. Res. 2017, 50, 1587–1596. [Google Scholar] [CrossRef] [PubMed]
- Palaparthy, V.S.; Doddapujar, S.N.; Surya, S.G.; Chandorkar, S.A.; Mukherji, S.; Baghini, M.S.; Rao, V.R. Hybrid pattern recognition for rapid explosive sensing with comprehensive analysis. IEEE Sens. J. 2020, 21, 8011–8019. [Google Scholar] [CrossRef]
- Chen, H.; Huo, D.; Zhang, J. Gas recognition in E-nose system: A review. IEEE Trans. Biomed. Circuits Syst. 2022, 16, 169–184. [Google Scholar] [CrossRef] [PubMed]
- Cortes, C.; Vapnik, V. Support-vector networks. Mach. Learn. 1995, 20, 273–297. [Google Scholar] [CrossRef]
- Tozlu, B.H.; Şimşek, C.; Aydemir, O.; Karavelioglu, Y. A High performance electronic nose system for the recognition of myocardial infarction and coronary artery diseases. Biomed. Signal Process. Control. 2021, 64, 102247. [Google Scholar] [CrossRef]
- Ding, X.; Zhang, Y.; Zhang, Y.; Ding, X.; Zhang, H.; Cao, T.; Qu, Z.; Ren, J.; Li, L.; Guo, Z.; et al. Modular assembly of MXene frameworks for noninvasive disease diagnosis via urinary volatiles. ACS Nano 2022, 16, 17376–17388. [Google Scholar] [CrossRef]
- Zhang, L.; Tian, F.; Nie, H.; Dang, L.; Li, G.; Ye, Q.; Kadri, C. Classification of multiple indoor air contaminants by an electronic nose and a hybrid support vector machine. Sens. Actuators B Chem. 2012, 174, 114–125. [Google Scholar] [CrossRef]
- Li, M.; Liu, H.; Chang, J.; Dai, T.; Nagashima, K.; Deng, Z.; Yanagida, T.; Fang, X.; Meng, G. Quantitatively discriminating alcohol molecules by thermally modulating NiO-based sensor arrays. Adv. Mater. Technol. 2022, 7, 2100762. [Google Scholar] [CrossRef]
- Yang, Y.; Wei, L. Application of E-nose technology combined with artificial neural network to predict total bacterial count in milk. J. Dairy Sci. 2021, 104, 10558–10565. [Google Scholar] [CrossRef]
- Fawaz, H.I.; Forestier, G.; Weber, J.; Idoumghar, L.; Müller, P.A. Deep learning for time series classification: A review. Data Min. Knowl. Discov. 2019, 33, 917–963. [Google Scholar] [CrossRef]
- Huang, G.B.; Zhu, Q.Y.; Siew, C.K. Extreme learning machine: A new learning scheme of feedforward neural networks. In Proceedings of the IEEE International Joint Conference on Neural Networks 2004, Budapest, Hungary, 25–29 July 2004. [Google Scholar]
- Ma, H.; Wang, T.; Li, B.; Cao, W.; Zeng, M.; Yang, J.; Su, Y.; Hu, N.; Zhou, Z.; Yang, Z. A low-cost and efficient electronic nose system for quantification of multiple indoor air contaminants utilizing HC and PLSR. Sens. Actuators B Chem. 2022, 350, 130768. [Google Scholar] [CrossRef]
- Faleh, R.; Gomri, S.; Aguir, K.; Kachouri, A. A new combined transient extraction method coupled with WO3 gas sensors for polluting gases classification. Sens. Rev. 2021, 41, 437–448. [Google Scholar] [CrossRef]
- Kang, M.; Cho, I.; Park, J.; Jeong, J.; Lee, K.; Lee, B.; Del Orbe Henriquez, D.; Yoon, K.; Park, I. High accuracy real-time multi-gas identification by a batch-uniform gas sensor array and deep learning algorithm. ACS Sens. 2022, 7, 430–440. [Google Scholar] [CrossRef] [PubMed]
- Wijaya, D.R.; Sarno, R.; Zulaika, E. DWTLSTM for electronic nose signal processing in beef quality monitoring. Sens. Actuators B Chem. 2021, 326, 128931. [Google Scholar] [CrossRef]
- Jiarpinijnun, A.; Osako, K.; Siripatrawan, U. Visualization of volatomic profiles for early detection of fungal in-fection on storage jasmine brown rice using electronic nose coupled with chemometrics. Measurement 2020, 157, 107561. [Google Scholar] [CrossRef]
- Teixeira, G.G.; Dias, L.G.; Rodrigues, N.; Marx, Í.M.; Veloso, A.C.; Pereira, J.A.; Peres, A.M. Application of a lab-made electronic nose for extra virgin olive oils commercial classification according to the perceived fruitiness intensity. Talanta 2021, 226, 122122. [Google Scholar] [CrossRef]
- Chen, Q.; Chen, Z.; Liu, D.; He, Z.; Wu, J. Constructing an E-nose using metal-ion-induced assembly of graphene oxide for diagnosis of lung cancer via exhaled breath. ACS Appl. Mater. Interfaces 2020, 12, 17713–17724. [Google Scholar] [CrossRef]
- Gamboa, J.C.R.; da Silva, A.J.; Araujo, I.C. Validation of the rapid detection approach for enhancing the electronic nose systems performance, using different deep learning models and support vector machines. Sens. Actuators B Chem. 2021, 327, 128921. [Google Scholar] [CrossRef]
- Yan, C.; Lu, A. A deep learning method combined with electronic nose to identify the rice origin. J. Instrum. 2022, 17, P08016. [Google Scholar] [CrossRef]
- Sun, H.; Hua, Z.; Yin, C.; Li, F.; Shi, Y. Geographical traceability of soybean: An electronic nose coupled with an effective deep learning method. Food Chem. 2024, 440, 138207. [Google Scholar] [CrossRef]
- Yang, Y.; Liu, H.; Gu, Y. A model transfer learning framework with back-propagation neural network for wine and Chinese liquor detection by electronic nose. IEEE Access 2020, 8, 105278–105285. [Google Scholar] [CrossRef]
- Bulucu, P.; Nakip, M.; Güzeliş, C. Multi-Sensor E-Nose Based on Online Transfer Learning Trend Predictive Neural Network. IEEE Access 2024, 12, 71442–71452. [Google Scholar] [CrossRef]
- Xiong, Y.; Li, Y.; Wang, C.; Shi, H.; Wang, S.; Yong, C.; Gong, Y.; Zhang, W.; Zou, X. Non-Destructive Detection of Chicken Freshness Based on Electronic Nose Technology and Transfer Learning. Agriculture 2023, 13, 496. [Google Scholar] [CrossRef]
- Li Voti, M.; Bax, C.; Marzocchi, M.; Sironi, S.; Capelli, L. Testing procedure for performance evaluation of electronic noses for environmental odour monitoring. Chem. Eng. Trans. 2018, 68, 277–282. [Google Scholar]
- Mirshahi, M.; Partovi Nia, V.; Adjengue, L. An online data validation algorithm for electronic nose. In Pattern Recognition Applications and Methods, Proceedings of the 5th International Conference, ICPRAM 2016, Rome, Italy, 24–26 February 2016; Revised Selected Papers 5; Springer International Publishing: Berlin/Heidelberg, Germany, 2016; pp. 104–120. [Google Scholar]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Buszewski, B.; Kesy, M.; Ligor, T.; Amann, A. Human exhaled air analytics: Biomarkers of diseases. Biomed. Chromatogr. 2007, 21, 553–566. [Google Scholar] [CrossRef]
- Chen, W.; Metsala, M.; Vaittinen, O.; Halonen, L. The origin of mouth-exhaled ammonia. J. Breath Res. 2014, 8, 036003. [Google Scholar] [CrossRef]
- Demirjian, S.; Paschke, K.M.; Wang, X.; Grove, D.; Heyka, R.J.; Dweik, R.A. Molecular breath analysis identifies the breathprint of renal failure. J. Breath Res. 2017, 11, 026009. [Google Scholar] [CrossRef] [PubMed]
- Romani, A.; Marrone, G.; Celotto, R.; Campo, M.; Vita, C.; Chiaramonte, C.; Carretta, A.; Di Daniele, N.; Noce, A. Utility of SIFT-MS to evaluate volatile organic compounds in nephropathic patients’ breath. Sci. Rep. 2022, 12, 10413. [Google Scholar] [CrossRef]
- Obermeier, J.; Trefz, P.; Happ, J.; Schubert, J.K.; Staude, H.; Fischer, D.C.; Miekisch, W. Exhaled volatile substances mirror clinical conditions in pediatric chronic kidney disease. PLoS ONE 2017, 12, e0178745. [Google Scholar] [CrossRef]
- Risby, T.H. Current status of clinical breath analysis. In Breath Analysis for Clinical Diagnosis and Therapeutic Monitoring; Amann, A., Smith, D., Eds.; World Scientific: Singapore, 2005; pp. 251–265. [Google Scholar]
- Pagonas, N.; Vautz, W.; Seifert, L.; Slodzinski, R.; Jankowski, J.; Zidek, W.; Westhoff, T.H. Volatile organic compounds in uremia. PLoS ONE 2012, 7, e46258. [Google Scholar] [CrossRef] [PubMed]
- Davies, S.; Španěl, P.; Smith, D. Quantitative analysis of ammonia on the breath of patients in end-stage renal failure. Kidney Int. 1997, 52, 223–228. [Google Scholar] [CrossRef] [PubMed]
- Neri, G.; Lacquaniti, A.; Rizzo, G.; Donato, N.; Latino, M.; Buemi, M. Real-time monitoring of breath ammonia during haemodialysis: Use of ion mobility spectrometry (IMS) and cavity ring-down spectroscopy (CRDS) techniques. Nephrol. Dial. Transplant. 2012, 27, 2945–2952. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, F.M.; Vaittinen, O.; Metsälä, M.; Lehto, M.; Forsblom, C.; Groop, P.H.; Halonen, L. Ammonia in breath and emitted from skin. J. Breath Res. 2013, 7, 017109. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Zhang, W.; Li, L.; Yu, Q. Breath ammonia detection based on tunable fiber laser photoacoustic spectroscopy. Appl. Phys. B 2011, 103, 263–269. [Google Scholar] [CrossRef]
- Oberg, B.P.; McMenamin, E.; Lucas, F.L.; McMonagle, E.; Morrow, J.; Ikizler, T.A.; Himmelfarb, J. Increased prevalence of oxidant stress and inflammation in patients with moderate to severe chronic kidney disease. Kidney Int. 2004, 65, 1009–1016. [Google Scholar] [CrossRef]
- Brien, J.F.; Loomis, C.W. Pharmacology of acetaldehyde. Can. J. Physiol. Pharmacol. 1983, 61, 1–22. [Google Scholar] [CrossRef]
- Himmelfarb, J.; Stenvinkel, P.; Ikizler, T.A.; Hakim, R.M. The elephant in uremia: Oxidant stress as a unifying concept of cardiovascular disease in uremia. Kidney Int. 2002, 62, 1524–1538. [Google Scholar] [CrossRef]
- Smith, D.; Wang, T.; Sulé-Suso, J.; Španěl, P.; El Haj, A. Quantification of acetaldehyde released by lung cancer cells in vitro using selected ion flow tube mass spectrometry. Rapid Commun. Mass Spectrom. 2003, 17, 845–850. [Google Scholar] [CrossRef]
- Ma, H.; Yu, L.; Byra, E.A.; Hu, N.; Kitagawa, K.; Nakayama, K.I.; Kawamoto, T.; Ren, J. Aldehyde dehydrogenase 2 knockout accentuates ethanol-induced cardiac depression: Role of protein phosphatases. J. Mol. Cell. Cardiol. 2010, 49, 322–329. [Google Scholar] [CrossRef]
- Mazzatenta, A.; Di Giulio, C.; Pokorski, M. Pathologies currently identified by exhaled biomarkers. Respir. Physiol. Neurobiol. 2013, 187, 128–134. [Google Scholar] [CrossRef] [PubMed]
- Ma, W.; Liu, X.; Pawliszyn, J. Analysis of human breath with micro extraction techniques and continuous monitoring of carbon dioxide concentration. Anal. Bioanal. Chem. 2006, 385, 1398–1408. [Google Scholar] [CrossRef] [PubMed]
- Kakoki, M.; Matsumoto, A.; Nagata, D.; Kobayakawa, N.; Kimura, K.; Momomura, S.; Hirata, Y. Analysis of nitric oxide in the exhaled air of patients with chronic glomerulonephritis. Clin. Nephrol. 1999, 52, 83–90. [Google Scholar] [PubMed]
- Di Francesco, F.; Fuoco, R.; Trivella, M.G.; Ceccarini, A. Breath analysis: Trends in techniques and clinical applications. Microchem. J. 2005, 79, 405–410. [Google Scholar] [CrossRef]
- Kwak, J.; Grigsby, C.C.; Smith, B.R.; Rizki, M.M.; Preti, G. Changes in volatile compounds of human urine as it ages: Their interaction with water. J. Chromatogr. B Analyt. Technol. Biomed. Life Sci. 2013, 941, 50–53. [Google Scholar] [CrossRef]
- Miekisch, W.; Schubert, J.K.; Noeldge-Schomburg, G.F. Diagnostic potential of breath analysis--focus on volatile organic compounds. Clin. Chim. Acta 2004, 347, 25–39. [Google Scholar] [CrossRef] [PubMed]
- Smith, D.; Wang, T.; Spanĕl, P. On-line, simultaneous quantification of ethanol, some metabolites and water vapour in breath following the ingestion of alcohol. Physiol. Meas. 2002, 23, 477–489. [Google Scholar] [CrossRef]
- Turner, C.; Spanĕl, P.; Smith, D. A longitudinal study of ethanol and acetaldehyde in the exhaled breath of healthy volunteers using selected-ion flow-tube mass spectrometry. Rapid Commun. Mass Spectrom. 2006, 20, 61–68. [Google Scholar] [CrossRef]
- Smith, D.; Pysanenko, A.; Spanĕl, P. Kinetics of ethanol decay in mouth- and nose-exhaled breath measured on-line by selected ion flow tube mass spectrometry following varying doses of alcohol. Rapid Commun. Mass Spectrom. 2010, 24, 1066–1074. [Google Scholar] [CrossRef]
- Cederbaum, A.I.; Lieber, C.S.; Rubin, E. Effect of acetaldehyde on fatty acid oxidation and ketogenesis by hepatic mitochondria. Arch. Biochem. Biophys. 1975, 169, 29–41. [Google Scholar] [CrossRef]
- Kesäniemi, Y.A.; Kervinen, K.; Miettinen, T.A. Acetaldehyde modification of low density lipoprotein accelerates its catabolism in man. Eur. J. Clin. Invest. 1987, 17, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Hanouneh, I.A.; Zein, N.N.; Cikach, F.; Dababneh, L.; Grove, D.; Alkhouri, N.; Lopez, R.; Dweik, R.A. The breathprints in patients with liver disease identify novel breath biomarkers in alcoholic hepatitis. Clin. Gastroenterol. Hepatol. 2014, 12, 516–523. [Google Scholar] [CrossRef] [PubMed]
- Phillips, M.; Altorki, N.; Austin, J.H.; Cameron, R.B.; Cataneo, R.N.; Kloss, R.; Maxfield, R.A.; Munawar, M.I.; Pass, H.I.; Rashid, A.; et al. Detection of lung cancer using weighted digital analysis of breath biomarkers. Clin. Chim. Acta 2008, 393, 76–84. [Google Scholar] [CrossRef] [PubMed]
- Montuschi, P.; Paris, D.; Melck, D.; Lucidi, V.; Ciabattoni, G.; Raia, V.; Calabrese, C.; Bush, A.; Barnes, P.J.; Motta, A. NMR spectroscopy metabolomic profiling of exhaled breath condensate in patients with stable and unstable cystic fibrosis. Thorax 2012, 67, 222–228. [Google Scholar] [CrossRef]
- de Laurentiis, G.; Paris, D.; Melck, D.; Montuschi, P.; Maniscalco, M.; Bianco, A.; Sofia, M.; Motta, A. Separating smoking-related diseases using NMR-based metabolomics of exhaled breath condensate. J. Proteome Res. 2013, 12, 1502–1511. [Google Scholar] [CrossRef]
- Longoni, B. Apoptosis and adaptive responses to oxidative stress in human endothelial cells exposed to cyclosporin A correlate with BCL-2 expression levels. FASEB J. 2001, 15, 731–740. [Google Scholar] [CrossRef]
- Weinstein, T. Haemolysis in haemodialysis patients: Evidence for impaired defence mechanisms against oxidative stress. Nephrol. Dial. Transplant. 2000, 15, 883–887. [Google Scholar] [CrossRef] [PubMed]
- Giustarini, D.; Dalle-Donne, I.; Tsikas, D.; Rossi, R. Oxidative stress and human diseases: Origin, link, measurement, mechanisms, and biomarkers. Crit. Rev. Clin. Lab. Sci. 2009, 46, 241–281. [Google Scholar] [CrossRef]
- Grabowska-Polanowska, B.; Skowron, M.; Miarka, P.; Pietrzycka, A.; Śliwka, I. The application of chromatographic breath analysis in the search of volatile biomarkers of chronic kidney disease and coexisting type 2 diabetes mellitus. J. Chromatogr. B Analyt. Technol. Biomed. Life Sci. 2017, 1060, 103–110. [Google Scholar] [CrossRef]
- Voss, A.; Baier, V.; Reisch, R.; von Roda, K.; Elsner, P.; Ahlers, H.; Stein, G. Smelling renal dysfunction via electronic nose. Ann. Biomed. Eng. 2005, 33, 656–660. [Google Scholar] [CrossRef]
- Guo, D.; Zhang, D.; Li, N.; Zhang, L.; Yang, J. A novel breath analysis system based on electronic olfaction. IEEE Trans. Biomed. Eng. 2010, 57, 2753–2763. [Google Scholar] [CrossRef]
- Marom, O.; Nakhoul, F.; Tisch, U.; Shiban, A.; Abassi, Z.; Haick, H. Gold nanoparticle sensors for detecting chronic kidney disease and disease progression. Nanomedicine 2012, 7, 639–650. [Google Scholar] [CrossRef]
- Assady, S.; Marom, O.; Hemli, M.; Ionescu, R.; Jeries, R.; Tisch, U.; Abassi, Z.; Haick, H. Impact of hemodialysis on exhaled volatile organic compounds in end-stage renal disease: A pilot study. Nanomedicine 2014, 9, 1035–1045. [Google Scholar] [CrossRef] [PubMed]
- Jayasree, T.; Bobby, M.; Muttan, S. Sensor data classification for renal dysfunction patients using support vector machine. J. Med. Biol. Eng. 2015, 35, 759–764. [Google Scholar] [CrossRef]
- Saidi, T.; Zaim, O.; Moufid, M.; El Bari, N.; Ionescu, R.; Bouchikhi, B. Exhaled breath analysis using electronic nose and gas chromatography–mass spectrometry for non-invasive diagnosis of chronic kidney disease, diabetes mellitus and healthy subjects. Sens. Actuators B Chem. 2018, 257, 178–188. [Google Scholar] [CrossRef]
- Le Maout, P.; Wojkiewicz, J.L.; Redon, N.; Lahuec, C.; Seguin, F.; Dupont, L.; Mikhailov, S.; Noskov, Y.; Ogurtsov, N.; Pud, A. Polyaniline nanocomposites based sensor array for breath ammonia analysis. Portable e-nose approach to non-invasive diagnosis of chronic kidney disease. Sens. Actuators B Chem. 2018, 274, 616–626. [Google Scholar] [CrossRef]
- Jokiniitty, E.; Hokkinen, L.; Kumpulainen, P.; Leskinen, Y.; Lehtimäki, T.; Oksala, N.; Roine, A. Urine headspace analysis with field asymmetric ion mobility spectrometry for detection of chronic kidney disease. Biomark. Med. 2020, 14, 629–638. [Google Scholar] [CrossRef]
- Chan, M.J.; Li, Y.J.; Wu, C.C.; Lee, Y.C.; Zan, H.W.; Meng, H.F.; Hsieh, M.H.; Lai, C.S.; Tian, Y.C. Breath Ammonia Is a Useful Biomarker Predicting Kidney Function in Chronic Kidney Disease Patients. Biomedicines 2020, 8, 468. [Google Scholar] [CrossRef]
- Kalidoss, R.; Umapathy, S.; Thirunavukkarasu, U.R. A breathalyzer for the assessment of chronic kidney disease patients’ breathprint: Breath flow dynamic simulation on the measurement chamber and experimental investigation. Biomed. Signal Process. Control. 2021, 70, 103060. [Google Scholar] [CrossRef]
- Costantini, M.; Filianoti, A.; Anceschi, U.; Bove, A.M.; Brassetti, A.; Ferriero, M.; Mastroianni, R.; Misuraca, L.; Tuderti, G.; Ciliberto, G.; et al. Human Urinary Volatilome Analysis in Renal Cancer by Electronic Nose. Biosensors 2023, 13, 427. [Google Scholar] [CrossRef]
- Li, X.; Zeng, W.; Zhuo, S.; Qian, B.; Chen, Q.; Luo, Q.; Qian, R. Highly Sensitive Room-Temperature Detection of Ammonia in the Breath of Kidney Disease Patients Using Fe2Mo3O8/MoO2@MoS2 Nanocomposite Gas Sensor. Adv. Sci. 2024, 11, e2405942. [Google Scholar] [CrossRef] [PubMed]
- Baldini, C.; Billeci, L.; Sansone, F.; Conte, R.; Domenici, C.; Tonacci, A. Electronic Nose as a Novel Method for Diagnosing Cancer: A Systematic Review. Biosensors 2020, 10, 84. [Google Scholar] [CrossRef] [PubMed]
- National Kidney Foundation. Available online: https://www.kidney.org/global-facts-about-kidney-disease (accessed on 22 August 2024).
- Francis, A.; Harhay, M.N.; Ong, A.C.M.; Tummalapalli, S.L.; Ortiz, A.; Fogo, A.B.; Fliser, D.; Roy-Chaudhury, P.; Fontana, M.; Nangaku, M.; et al. Chronic kidney disease and the global public health agenda: An international consensus. Nat. Rev. Nephrol. 2024, 20, 473–485. [Google Scholar] [CrossRef] [PubMed]
- Behera, B.; Joshi, R.; Anil Vishnu, G.K.; Bhalerao, S.; Pandya, H.J. Electronic nose: A non-invasive technology for breath analysis of diabetes and lung cancer patients. J. Breath Res. 2019, 13, 024001. [Google Scholar] [CrossRef]
- Witt, K.; Fischer, C.; Reulecke, S.; Kechagias, V.; Surber, R.; Figulla, H.R.; Voss, A. Electronic nose detects heart failure from exhaled breath. Biomed. Technol. 2013, 58. [Google Scholar] [CrossRef]
- Vadala, R.; Pattnaik, B.; Bangaru, S.; Rai, D.; Tak, J.; Kashyap, S.; Verma, U.; Yadav, G.; Dhaliwal, R.S.; Mittal, S.; et al. A review on electronic nose for diagnosis and monitoring treatment response in lung cancer. J. Breath Res. 2023, 17, 024002. [Google Scholar] [CrossRef]


| Technology | Pros | Cons |
|---|---|---|
| MOS | Low-cost, effectiveness, portability, reliability | Sensitivity to environmental conditions (temperature, humidity), baseline drifts, somewhat limited lifespan |
| MOSFET | High efficiency in power transform implementation, easy fabrication and integration, miniaturization | Heat generation, easy to be damaged |
| Optic fiber sensors | High sensitivity and accuracy, immunity to electromagnetic interference, small size and light weight, multiplexing capability | More expensive than alternatives, quite fragile, need maintenance |
| Solid electrolyte sensors | Safety, thermal stability, wide electrochemical window, good cycle performance | High interface impedance, air sensitivity |
| Conductive organic polymers | High conductivity, excellent electrical stimulus, biocompatibility and biodegradability | Suboptimal durability |
| Mass-sensitive sensors | Stable sensing materials, simple and affordable fabrication, rapidity of measurement | Sensitive to external disturbance, poor selectivity |
| Model (s) | Pros | Cons |
|---|---|---|
| PCA | Easy data visualization; multicollinearity and noise removal; reduced training time and model parameters | Significant run-times; limited features interpretability; significant loss of information during data processing; affected by outliers |
| SVM | Effective in high dimensional spaces; good memory efficiency; good versatility | Unable to provide direct probability estimates; tendency to overfit |
| ANN | Parallel operation; tolerance to noisy data; easily updated with new data; good performances in complex problems | Limited output interpretability; burden of computational process |
| LDA | Simple; portable; good performance | Normal features distribution required; not optimal with small dataset or few categories; tendency to overfit |
| kNN | Lack of training period: simple to implement | Not optimal with large dataset and with high dimensional data; sensitivity to noisy and missing data |
| RF | High accuracy; robustness to noise; handling missing values and numerical and categorical data; somewhat stable to overfitting | Poorly interpretable; high computational costs and memory usage |
| Clinical Condition (s) | Altered Biomarker (s) | Physiological Source (s) | Alteration Type | Reference (s) |
|---|---|---|---|---|
| Uremia, kidney impairment, CKD | Nitrogen-containing compounds (ammonia, dimethylamine, trimethylamine) | Protein metabolism [68] | Mostly increased | [63,66,67,69] |
| CKD, renal failure | Ammonia | Protein metabolism [65], blood urea [70,71,72,73] | Increased | [63,64,65] |
| Renal failure | 2-propanol | Acetone reduction [65] | Increased | [65] |
| Renal failure | Acetaldehyde | Oxidative stress, inflammatory processes [74,75,76,77,78] | Increased | [65] |
| CKD | Acetone | Decarboxylation of acetoacetate and acetyl-CoA [63], fatty acid metabolism [79] | Increased | [66,69] |
| CKD | Isoprene | Cholesterol metabolism [80] | Increased | [63,67] |
| Chronic glomerulonephritis | Nitric oxide | Metabolic processes | Increased | [81] |
| CKD (pediatric) | Pentanal, heptanal | Oxidative stress [67] | Increased | [67] |
| CKD (pediatric) | Ethanol | Non-specific, possibly environmental contamination [67] | Increased | [67] |
| Sample Population (Cases/Controls) | Disease Studied | e-Nose Technology/Device | Type of Sample (s) | Biomarker (s) | Performances | Reference (s) |
|---|---|---|---|---|---|---|
| 62 (42 ESKD, 20 CKD)/11 | ESKD, CKD | E-nose equipped with 3 MOS sensors | Body odor | Methane, butane, alcohols, ketones, carbon monoxide, nitrogen oxide, ammonia | ACC: 100% between patients and controls; ACC: 95.2% between ESKD and CKD | [98] |
| 110/335 (117 DM, 110 AIn, 108 HC) | Renal disease | Figaro MOS sensors | Dead-space breath air samples | H2, CO, VOCs, H2S, CO2, NH3, NO, NO2 | SE: 86.57%, SP: 83.47% | [99] |
| 46/20 | Different stages of CKD | GNP sensors | Breath samples | Isoprene, acetone, ethylene glycol, acetoin, methylated hydrocarbons, ketones | ACC: 79% between early-stage CKD and controls; ACC: 85% between stage 4 and stage 5 CKD; ACC: 76% between early and advanced CKD | [100] |
| 26/11 | ESKD | Nanomaterial-based sensors | Exhaled breath samples | Nonane, methylene chloride, isopropanol, styrene | ACC: 80% with DFA | [101] |
| 40/0 | CKD | Figaro TGS2444, MQ135, MQ137, TGS826 MOS sensors | Breath samples | Ammonia | ACC: 88% (for ammonia) | [102] |
| 16/28 (6 DM, 22 HC) | CKD | E-nose equipped with 6 chemical sensors: MQ-2, MQ-3, MQ9, MQ-135, MQ-137 and MQ-138 | Breath (and urine) samples | Different VOCs, including ammonia | Correct classification up to 100% with e-nose data analyzed by SVM | [103] |
| n.a. | Renal diseases (potentially) | E-nose based on PANI nanocomposites | Breath samples simulation | Ammonia | ACC: up to 85% with SVM | [104] |
| 95/n.a. | CKD | FAIMS | Urine headspace | VOC composition | 81.4% differentiation of kidney function extremes | [105] |
| 121/0 | CKD | V-OSC | Breath samples | Ammonia | ROC AUC = 0.835 (p < 0.0001) across CKD at 1st stage and at any stage at 974 ppb (SE: 69%; SP: 95%). ROC AUC = 0.831 (p < 0.0001) between patients with/without eGFR < 60 mL/min/1.73 m2 (at 1187 ppb: SE: 71%, SP: 78%; at 886 ppb: SE: 80%, SP: 69%) | [106] |
| 51/47 | CKD (under hemodialysis) | Figaro MQ135 MOS sensor | Breath samples | Ammonia | ACC: 85.7% | [107] |
| 110/142 | Renal cancer | Cyranose 320® | Urine sample | Combined VOCs | SP: 89.4%, SE: 71.8%, PPV: 84.04%, NPV: 80.37%; CVA: 81.7%, p < 0.001. ROC AUC: 0.85 | [108] |
| 6/3 | Early and late stage CKD | Fe2Mo3O8/MoO2@MoS2 nanocomposite gas sensor | Breath samples | Ammonia | R2 = 0.99 between ammonia concentrations and sensors’ outputs | [109] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sansone, F.; Tonacci, A. Non-Invasive Diagnostic Approaches for Kidney Disease: The Role of Electronic Nose Systems. Sensors 2024, 24, 6475. https://doi.org/10.3390/s24196475
Sansone F, Tonacci A. Non-Invasive Diagnostic Approaches for Kidney Disease: The Role of Electronic Nose Systems. Sensors. 2024; 24(19):6475. https://doi.org/10.3390/s24196475
Chicago/Turabian StyleSansone, Francesco, and Alessandro Tonacci. 2024. "Non-Invasive Diagnostic Approaches for Kidney Disease: The Role of Electronic Nose Systems" Sensors 24, no. 19: 6475. https://doi.org/10.3390/s24196475






