A Clustering-Based Approach to Functional and Biomechanical Parameters Recorded with a Pair of Smart Eyeglasses in Older Adults in Order to Determine Physical Performance Groups
Abstract
:1. Introduction
2. Materials and Methods
2.1. Particpants
2.2. Experimental Design
2.3. Apparatus, Data Collection
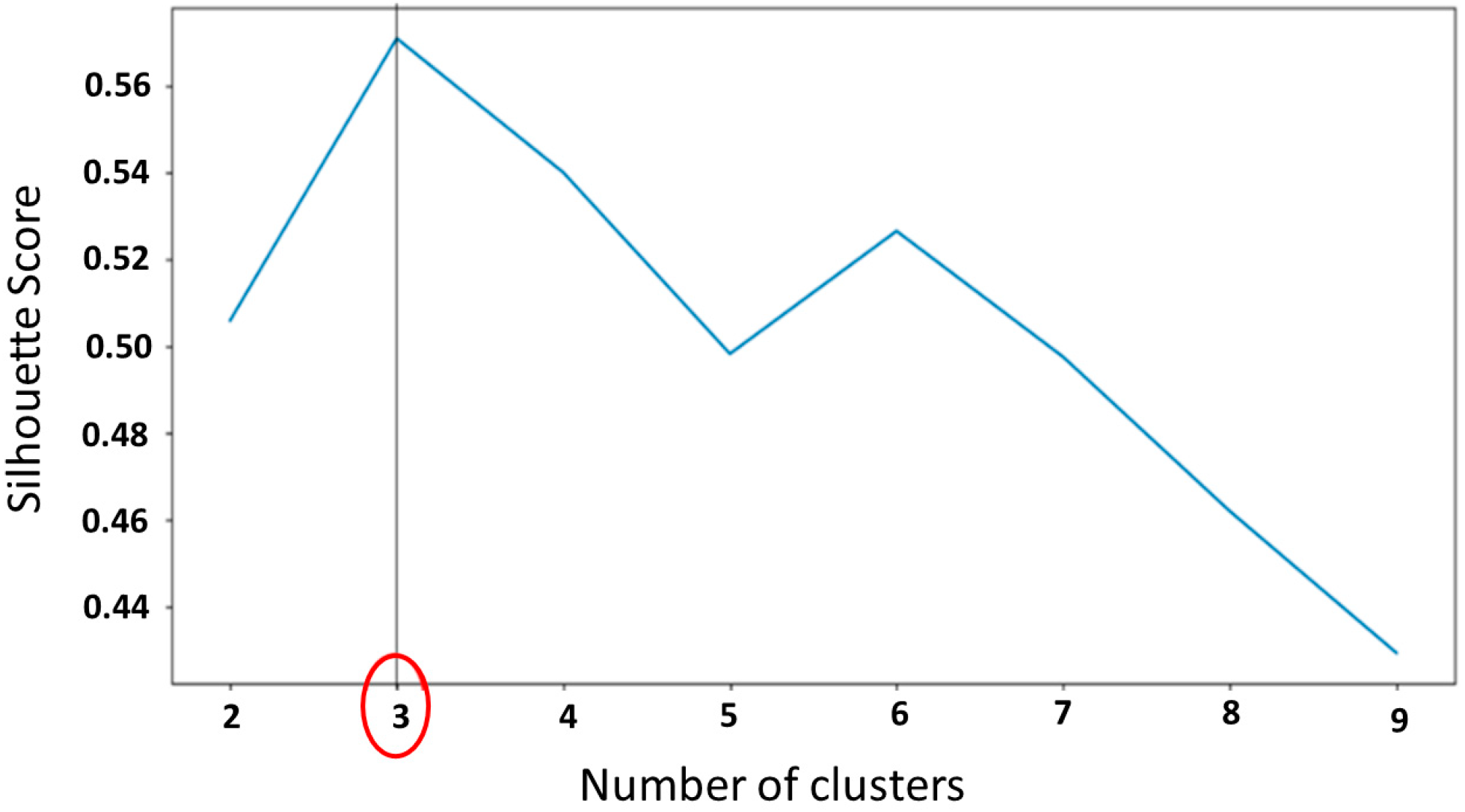
2.4. Statistical Analysis
3. Results
3.1. Fall History Groups
3.2. Frailty Phenotype Groups
3.3. Physical Performance Groups
3.3.1. Characteristics of the Three Performance Groups
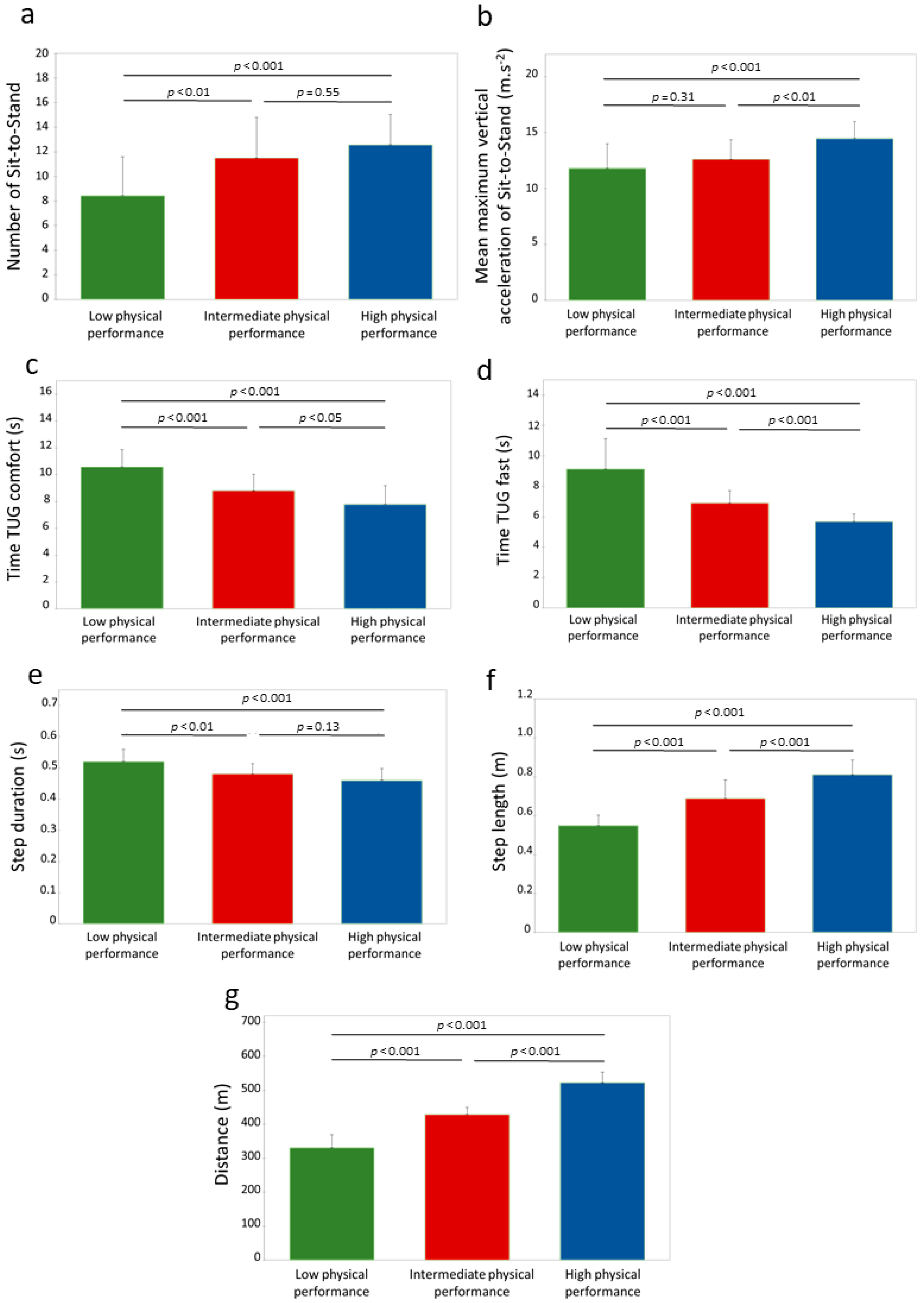
3.3.2. Physical Capacities of the Three Performance Groups
3.3.3. Physical Performance Equation Obtained from the Functional and Biomechanical Parameters Measured
× 0.009 + step length × (−0.098) + step duration × 0.051 + TUG time fast × 0.002 + TUG time comfort ×
(−0.045) −2.265
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fried, L.P. Risk Factors for 5-Year Mortality in Older Adults: The Cardiovascular Health Study. JAMA 1998, 279, 585–592. [Google Scholar] [CrossRef]
- O’Caoimh, R.; Galluzzo, L.; Rodríguez-Laso, Á.; Van der Heyden, J.; Ranhoff, A.H.; Lamprini-Koula, M.; Ciutan, M.; López-Samaniego, L.; Carcaillon-Bentata, L.; Kennelly, S.; et al. Prevalence of frailty at population level in European ADVANTAGE Joint Action Member States: A systematic review and meta-analysis. Ann. Ist. Super. Sanita 2018, 54, 226–238. [Google Scholar] [CrossRef]
- Organisation Mondiale de la Santé. Falls. Available online: https://www.who.int/news-room/fact-sheets/detail/falls (accessed on 5 September 2022).
- Buatois, S.; Bénétos, A. Mise en place d’une échelle clinique simple pour évaluer le risque de chutes répétées chez les seniors. Kinésithérapie Rev. 2011, 11, 45–48. [Google Scholar] [CrossRef]
- Campbell, A.J.; Borrie, M.J.; Spears, G.F.; Jackson, S.L.; Brown, J.S.; Fitzgerald, J.L. Circumstances and Consequences of Falls Experienced by a Community Population 70 Years and over during a Prospective Study. Age Ageing 1990, 19, 136–141. [Google Scholar] [CrossRef]
- Beauchet, O.; Eynard-Valhorgues, F.; Blanchon, M.A.; Terrat, C.; Gonthier, R. Factors contributing to falls in elderly subjects leading to acute-care hospitalization. Presse Med. 2000, 29, 1544–1548. [Google Scholar]
- Boulgarides, L.K.; McGinty, S.M.; Willett, J.A.; Barnes, C.W. Use of Clinical and Impairment-Based Tests to Predict Falls by Community-Dwelling Older Adults. Phys. Ther. 2003, 83, 328–339. [Google Scholar] [CrossRef] [PubMed]
- Kado, D.M.; Huang, M.-H.; Barrett-Connor, E.; Greendale, G.A. Hyperkyphotic Posture and Poor Physical Functional Ability in Older Community-Dwelling Men and Women: The Rancho Bernardo Study. J. Gerontol. A Biol. Sci. Med. Sci. 2005, 60, 633–637. [Google Scholar] [CrossRef]
- Tinetti, M.E.; Williams, C.S. Falls, Injuries Due to Falls, and the Risk of Admission to a Nursing Home. N. Engl. J. Med. 1997, 337, 1279–1284. [Google Scholar] [CrossRef] [PubMed]
- Fried, L.P.; Ferrucci, L.; Darer, J.; Williamson, J.D.; Anderson, G. Untangling the Concepts of Disability, Frailty, and Comorbidity: Implications for Improved Targeting and Care. J. Gerontol. A Biol. Sci. Med. Sci. 2004, 59, M255–M263. [Google Scholar] [CrossRef]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in Older Adults: Evidence for a Phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M146–M157. [Google Scholar] [CrossRef]
- Sternberg, S.A.; Schwartz, A.W.; Karunananthan, S.; Bergman, H.; Mark Clarfield, A. The Identification of Frailty: A Systematic Literature Review. J. Am. Geriatr. Soc. 2011, 59, 2129–2138. [Google Scholar] [CrossRef] [PubMed]
- Wolf, E.J.; Harrington, K.M.; Clark, S.L.; Miller, M.W. Sample Size Requirements for Structural Equation Models: An Evaluation of Power, Bias, and Solution Propriety. Educ. Psychol. Meas. 2013, 73, 913–934. [Google Scholar] [CrossRef]
- Cheng, M.-H.; Chang, S.-F. Frailty as a Risk Factor for Falls Among Community Dwelling People: Evidence From a Meta-Analysis: Falls With Frailty. J. Nurs. Scholarsh. 2017, 49, 529–536. [Google Scholar] [CrossRef] [PubMed]
- Fhon, J.R.S.; Rodrigues, R.A.P.; Neira, W.F.; Huayta, V.M.R.; Robazzi, M.L. Fall and its association with the frailty syndrome in the elderly: Systematic review with meta-analysis. Rev. Esc. Enferm. USP 2016, 50, 1005–1013. [Google Scholar] [CrossRef] [PubMed]
- Brodie, M.A.; Lord, S.R.; Coppens, M.J.; Annegarn, J.; Delbaere, K. Eight-week remote monitoring using a freely worn device reveals unstable gait patterns in older fallers. IEEE Trans. Biomed. Eng. 2015, 62, 2588–2594. [Google Scholar] [CrossRef] [PubMed]
- Wu, L.C.; Laksari, K.; Kuo, C.; Luck, J.F.; Kleiven, S.; ‘Dale’ Bass, C.R.; Camarillo, D.B. Bandwidth and sample rate requirements for wearable head impact sensors. J. Biomech. 2016, 49, 2918–2924. [Google Scholar] [CrossRef] [PubMed]
- Hars, M.; Trombetti, A. Evaluation de la marche, de l’équilibre et du muscle chez le sujet âgé. Rev. Med. Suisse 2013, 9, 1265–1271. [Google Scholar] [PubMed]
- Podsiadlo, D.; Richardson, S. The Timed “Up & Go”: A Test of Basic Functional Mobility for Frail Elderly Persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar] [CrossRef]
- Buisseret, F.; Catinus, L.; Grenard, R.; Jojczyk, L.; Fievez, D.; Barvaux, V.; Dierick, F. Timed Up and Go and Six-Minute Walking Tests with Wearable Inertial Sensor: One Step Further for the Prediction of the Risk of Fall in Elderly Nursing Home People. Sensors 2020, 20, 3207. [Google Scholar] [CrossRef]
- Lee, J.; Geller, A.I.; Strasser, D.C. Analytical Review: Focus on Fall Screening Assessments. PM&R 2013, 5, 609–621. [Google Scholar] [CrossRef]
- Lusardi, M.M.; Fritz, S.; Middleton, A.; Allison, L.; Wingood, M.; Phillips, E.; Criss, M.; Verma, S.; Osborne, J.; Chui, K.K. Determining Risk of Falls in Community Dwelling Older Adults: A Systematic Review and Meta-analysis Using Posttest Probability. J. Geriatr. Phys. Ther. 2017, 40, 1–36. [Google Scholar] [CrossRef]
- Schoene, D.; Smith, S.T.; Davies, T.A.; Delbaere, K.; Lord, S.R. A Stroop Stepping Test (SST) using low-cost computer game technology discriminates between older fallers and non-fallers. Age Ageing 2014, 43, 285–289. [Google Scholar] [CrossRef] [PubMed]
- Beck Jepsen, D.; Robinson, K.; Ogliari, G.; Montero-Odasso, M.; Kamkar, N.; Ryg, J.; Freiberger, E.; Tahir, M. Predicting falls in older adults: An umbrella review of instruments assessing gait, balance, and functional mobility. BMC Geriatr. 2022, 22, 615. [Google Scholar] [CrossRef]
- Gates, S.; Fisher, J.D.; Cooke, M.W.; Carter, Y.H.; Lamb, S.E. Multifactorial assessment and targeted intervention for preventing falls and injuries among older people in community and emergency care settings: Systematic review and meta-analysis. BMJ 2008, 336, 130–133. [Google Scholar] [CrossRef]
- Babič, F.; Trtica Majnarić, L.; Bekić, S.; Holzinger, A. Machine Learning for Family Doctors: A Case of Cluster Analysis for Studying Aging Associated Comorbidities and Frailty. In Machine Learning and Knowledge Extraction, Proceedings of the Third IFIP TC 5, TC 12, WG 8.4, WG 8.9, WG 12.9 International Cross-Domain Conference, CD-MAKE 2019, Canterbury, UK, 26–29 August 2019; Holzinger, A., Kieseberg, P., Tjoa, A.M., Weippl, E., Eds.; Springer: Berlin/Heidelberg, Germany, 2019; Volume 11713, pp. 178–194. [Google Scholar] [CrossRef]
- Goh, C.-H.; Wong, K.K.; Tan, M.P.; Ng, S.-C.; Chuah, Y.D.; Kwan, B.-H. Development of an effective clustering algorithm for older fallers. PLoS ONE 2022, 17, e0277966. [Google Scholar] [CrossRef] [PubMed]
- Majumder, S.; Mondal, T.; Deen, M. Wearable Sensors for Remote Health Monitoring. Sensors 2017, 17, 130. [Google Scholar] [CrossRef] [PubMed]
- Ren, L.; Peng, Y. Research of Fall Detection and Fall Prevention Technologies: A Systematic Review. IEEE Access 2019, 7, 77702–77722. [Google Scholar] [CrossRef]
- Cohen, C.; Kampel, T.; Verloo, H. Acceptability of an intelligent wireless sensor system for the rapid detection of health issues: Findings among home-dwelling older adults and their informal caregivers. Patient Prefer. Adherence 2016, 10, 1687–1695. [Google Scholar] [CrossRef]
- Rantz, M.; Skubic, M.; Abbott, C.; Galambos, C.; Popescu, M.; Keller, J.; Stone, E.; Back, J.; Miller, S.J.; Petroski, G.F. Automated In-Home Fall Risk Assessment and Detection Sensor System for Elders. Gerontologist 2015, 55, S78–S87. [Google Scholar] [CrossRef]
- Subramaniam, S.; Faisal, A.I.; Deen, M.J. Wearable Sensor Systems for Fall Risk Assessment: A Review. Front. Digit. Health 2022, 4, 921506. [Google Scholar] [CrossRef]
- Özdemir, A. An Analysis on Sensor Locations of the Human Body for Wearable Fall Detection Devices: Principles and Practice. Sensors 2016, 16, 1161. [Google Scholar] [CrossRef]
- Lindemann, U.; Hock, A.; Stuber, M.; Keck, W.; Becker, C. Evaluation of a fall detector based on accelerometers: A pilot study. Med. Biol. Eng. Comput. 2005, 43, 548–551. [Google Scholar] [CrossRef]
- Hellec, J.; Chorin, F.; Castagnetti, A.; Colson, S.S. Sit-To-Stand Movement Evaluated Using an Inertial Measurement Unit Embedded in Smart Glasses—A Validation Study. Sensors 2020, 20, 5019. [Google Scholar] [CrossRef]
- Hellec, J.; Chorin, F.; Castagnetti, A.; Guérin, O.; Colson, S.S. Smart Eyeglasses: A Valid and Reliable Device to Assess Spatiotemporal Parameters during Gait. Sensors 2022, 22, 1196. [Google Scholar] [CrossRef] [PubMed]
- Hellec, J.; Hayotte, M.; Chorin, F.; Colson, S.S.; d’Arripe-Longueville, F. Acceptability of smart eyeglasses to detect and prevent falls among the elderly: Applying the UTAUT2 model and examining associations with fall-related functional physical capacities. J. Med. Internet Res. 2023, 25, e41220. [Google Scholar] [CrossRef]
- Silva, J.; Madureira, J.; Tonelo, C.; Baltazar, D.; Silva, C.; Martins, A.; Alcobia, C.; Sousa, I. Comparing Machine Learning Approaches for Fall Risk Assessment. In Proceedings of the 10th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2017), Porto, Portugal, 21–23 February 2017; SciTePress: Setubal, Portugal, 2017; pp. 223–230. [Google Scholar] [CrossRef]
- Ogbuabor, G.; Ugwoke, F.N. Clustering Algorithm for a Healthcare Dataset Using Silhouette Score Value. Int. J. Comput. Sci. Inf. Technol. 2018, 10, 27–37. [Google Scholar] [CrossRef]
- Kwon, M.-S.; Kwon, Y.-R.; Park, Y.-S.; Kim, J.-W. Comparison of gait patterns in elderly fallers and non-fallers. Technol. Health Care 2018, 26, 427–436. [Google Scholar] [CrossRef] [PubMed]
- Mortaza, N.; Abu Osman, N.A.; Mehdikhani, N. Are the spatio-temporal parameters of gait capable of distinguishing a faller from a non-faller elderly? Eur. J. Phys. Rehabil. Med. 2014, 50, 677–691. [Google Scholar]
- Pophal da Silva, L.; Boneti Moreira, N.; Barbosa de Freitas, P.; Pereira, G.; Rodacki, A.L.F. Gait Parameters of Older Adults according to Their Fall History and Functional Capacity While Walking at Different Speeds. Gerontology 2021, 67, 532–543. [Google Scholar] [CrossRef] [PubMed]
- Delbaere, K.; Close, J.C.T.; Heim, J.; Sachdev, P.S.; Brodaty, H.; Slavin, M.J.; Kochan, N.A.; Lord, S.R. A Multifactorial Approach to Understanding Fall Risk in Older People. J. Am. Geriatr. Soc. 2010, 58, 1679–1685. [Google Scholar] [CrossRef]
- Montesinos, L.; Castaldo, R.; Pecchia, L. Wearable inertial sensors for fall risk assessment and prediction in older adults: A systematic review and meta-analysis. IEEE Trans. Neural Syst. Rehabil. Eng. 2018, 26, 573–582. [Google Scholar] [CrossRef]
- Ruiz-Ruiz, L.; Jimenez, A.R.; Garcia-Villamil, G.; Seco, F. Detecting Fall Risk and Frailty in Elders with Inertial Motion Sensors: A Survey of Significant Gait Parameters. Sensors 2021, 21, 6918. [Google Scholar] [CrossRef]
- Schwenk, M.; Howe, C.; Saleh, A.; Mohler, J.; Grewal, G.; Armstrong, D.; Najafi, B. Frailty and Technology: A Systematic Review of Gait Analysis in Those with Frailty. Gerontology 2014, 60, 79–89. [Google Scholar] [CrossRef] [PubMed]
- Boreskie, K.F.; Rose, A.V.; Hay, J.L.; Kehler, D.S.; Costa, E.C.; Moffatt, T.L.; Arora, R.C.; Duhamel, T.A. Frailty status and cardiovascular disease risk profile in middle-aged and older females. Exp. Gerontol. 2020, 140, 111061. [Google Scholar] [CrossRef] [PubMed]
- Millor, N.; Lecumberri, P.; Gómez, M.; Martínez-Ramírez, A.; Izquierdo, M. An evaluation of the 30-s chair stand test in older adults: Frailty detection based on kinematic parameters from a single inertial unit. J. Neuroeng. Rehabil. 2013, 10, 86. [Google Scholar] [CrossRef]
- Ansai, J.H.; Farche, A.C.S.; Rossi, P.G.; de Andrade, L.P.; Nakagawa, T.H.; de Medeiros Takahashi, A.C. Performance of Different Timed Up and Go Subtasks in Frailty Syndrome. J. Geriatr. Phys. Ther. 2019, 42, 287–293. [Google Scholar] [CrossRef] [PubMed]
- Greene, B.R.; Doheny, E.P.; O’Halloran, A.; Kenny, R.A. Frailty status can be accurately assessed using inertial sensors and the TUG test. Age Ageing 2014, 43, 406–411. [Google Scholar] [CrossRef]
- Vergara, I.; Mateo-Abad, M.; Saucedo-Figueredo, M.C.; Machón, M.; Montiel-Luque, A.; Vrotsou, K.; Nava del Val, M.A.; Díez-Ruiz, A.; Güell, C.; Matheu, A.; et al. Description of frail older people profiles according to four screening tools applied in primary care settings: A cross sectional analysis. BMC Geriatr. 2019, 19, 342. [Google Scholar] [CrossRef]
- Dapp, U.; Vinyard, D.; Golgert, S.; Krumpoch, S.; Freiberger, E. Reference values of gait characteristics in community-dwelling older persons with different physical functional levels. BMC Geriatr. 2022, 22, 713. [Google Scholar] [CrossRef]
- World Health Organization. World Report on Ageing and Health. Available online: https://apps.who.int/iris/handle/10665/186463 (accessed on 17 June 2020).
- DREES. Troubles de la Vision: Sept Adultes Sur Dix Portent des Lunettes. Available online: https://drees.solidarites-sante.gouv.fr/sites/default/files/2020-10/er881.pdf (accessed on 17 June 2020).
- Novac, P.-E.; Pegatoquet, A.; Miramond, B.; Caquineau, C. UCA-EHAR: A Dataset for Human Activity Recognition with Embedded AI on Smart Glasses. Appl. Sci. 2022, 12, 3849. [Google Scholar] [CrossRef]
- Bargiotas, I.; Wang, D.; Mantilla, J.; Quijoux, F.; Moreau, A.; Vidal, C.; Barrois, R.; Nicolai, A.; Audiffren, J.; Labourdette, C.; et al. Preventing falls: The use of machine learning for the prediction of future falls in individuals without history of fall. J. Neurol. 2023, 720, 618–631. [Google Scholar] [CrossRef] [PubMed]


| Faller Group n = 34 | Non-Faller Group n = 50 | p Value | |
|---|---|---|---|
| STS: Number in 30 s | 10.82 ± 3.42 | 11.10 ± 3.44 | 0.72 |
| STS: Average maximal vertical acceleration (m·s−2) | 13.02 ± 2.15 | 12.84 ± 2.04 | 0.69 |
| 6MWT: Distance covered (m) | 410.36 ± 80.69 | 441.35 ± 70.93 | 0.07 |
| 6MWT: Average step duration (s) | 0.48 ± 0.04 | 0.48 ± 0.05 | 0.56 |
| 6MWT: Average step length (m) | 0.65 ± 0.12 | 0.71 ± 0.12 | 0.04 |
| TUG: Time comfort (s) | 8.87 ± 1.54 | 9.08 ± 1.73 | 0.55 |
| TUG: Time fast (s) | 7.27 ± 1.74 | 7.06 ± 1.77 | 0.54 |
| Robust Group n = 24 | Pre-Frail Group n = 45 | Frail Group n = 15 | |
|---|---|---|---|
| STS: Number in 30 s | 12.79 ± 3.12 ** | 10.82 ± 2.79 | 8.60 ± 4.12 |
| STS: Average maximal vertical acceleration (m·s−2) | 13.95 ± 1.27 ** | 12.82 ± 2.13 | 11.53 ± 2.17 |
| 6MWT: Distance covered (m) | 452.76 ± 73.39 ** | 434.21 ± 64.04 | 374.25 ± 91.33 |
| 6MWT: Average step duration (s) | 0.48 ± 0.05 | 0.48 ± 0.04 | 0.50 ± 0.04 |
| 6MWT: Average step length (m) | 0.72 ± 0.10 * | 0.69 ± 0.12 | 0.62 ± 0.15 |
| TUG: Time comfort (s) | 8.39 ± 1.36 | 9.14 ± 1.81 | 9.54 ± 1.34 |
| TUG: Time fast (s) | 6.64 ± 1.44 * | 7.11 ± 1.74 | 8.09 ± 1.95 |
| LPP | IPP | HPP | |
|---|---|---|---|
| n | 22 | 39 | 23 |
| Sex (% females) | 68% | 72% | 65% |
| Age (years) | 77.45 ± 4.39 *** | 75.12 ± 5.61 *** | 69.43 ± 4.29 |
| Height (cm) | 164.73 ± 8.15 | 164.54 ± 7.83 | 168.61 ± 8.57 |
| Body mass (kg) | 68.52 ± 14.76 | 69.16 ± 13.52 | 68.94 ± 12.97 |
| Fallers (%) | 45.45 | 41.03 | 34.78 |
| Robust (%) | 18.18 | 25.64 | 43.48 |
| Pre-frail (%) | 40.91 | 64.10 | 47.82 |
| Frail (%) | 40.91 | 10.26 ££ | 8.70 ££ |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hellec, J.; Colson, S.S.; Jaafar, A.; Guérin, O.; Chorin, F. A Clustering-Based Approach to Functional and Biomechanical Parameters Recorded with a Pair of Smart Eyeglasses in Older Adults in Order to Determine Physical Performance Groups. Sensors 2024, 24, 1427. https://doi.org/10.3390/s24051427
Hellec J, Colson SS, Jaafar A, Guérin O, Chorin F. A Clustering-Based Approach to Functional and Biomechanical Parameters Recorded with a Pair of Smart Eyeglasses in Older Adults in Order to Determine Physical Performance Groups. Sensors. 2024; 24(5):1427. https://doi.org/10.3390/s24051427
Chicago/Turabian StyleHellec, Justine, Serge S. Colson, Amyn Jaafar, Olivier Guérin, and Frédéric Chorin. 2024. "A Clustering-Based Approach to Functional and Biomechanical Parameters Recorded with a Pair of Smart Eyeglasses in Older Adults in Order to Determine Physical Performance Groups" Sensors 24, no. 5: 1427. https://doi.org/10.3390/s24051427
APA StyleHellec, J., Colson, S. S., Jaafar, A., Guérin, O., & Chorin, F. (2024). A Clustering-Based Approach to Functional and Biomechanical Parameters Recorded with a Pair of Smart Eyeglasses in Older Adults in Order to Determine Physical Performance Groups. Sensors, 24(5), 1427. https://doi.org/10.3390/s24051427






