Inertial Measuring System to Evaluate Gait Parameters and Dynamic Alignments for Lower-Limb Amputation Subjects
Abstract
1. Introduction
2. Material and Methods
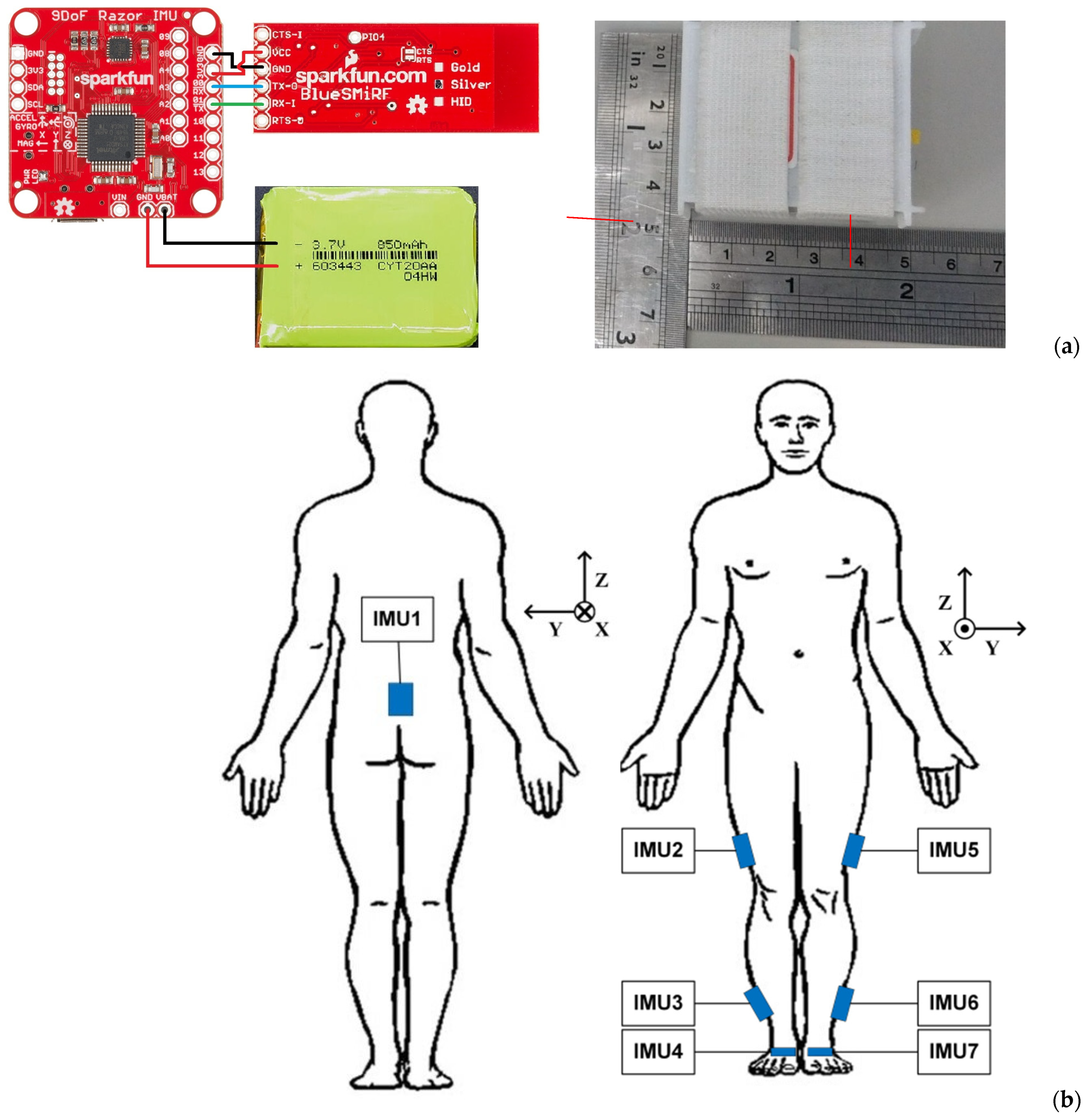
2.1. Wireless Inertial Measuring System
2.2. Computation Algorithms
2.2.1. Rotation and Coordinate Transformation of Orientation
2.2.2. Madgwick Filtering for Quaternion Correction
2.2.3. ZUPT for Gait Phase Detection
2.3. Kinematic Parameters and Gait Visualization
Gait Visualization
3. System Validation
- (1)
- ABB® IRB 120 robotics
- (2)
- Qualisys® Motion System
4. Clinical Application on Amputee Subjects
5. Discussion
6. Concluding Remarks
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pillet, H.; Sapin-de Brosses, E.; Fode, P.; Lavaste, F. Three-Dimensional Motions of Trunk and Pelvis during Transfemoral Amputee Gait. Arch. Phys. Med. Rehabil. 2008, 89, 87–94. [Google Scholar] [CrossRef] [PubMed]
- Esquenazi, A. Gait analysis in lower-limb amputation and prosthetic rehabilitation. Phys. Med. Rehabil. Clin. N. Am. 2014, 25, 153–167. [Google Scholar] [CrossRef]
- Pinhey, S.R.; Murata, H.; Hisano, G.; Ichimura, D.; Hobara, H.; Major, M.J. Effects of walking speed and prosthetic knee control type on external mechanical work in transfemoral prosthesis users. J. Biomech. 2022, 134, 110984. [Google Scholar] [CrossRef]
- Brandt, A.; Huang, H.H. Effects of extended stance time on a powered knee prosthesis and gait symmetry on the lateral control of balance during walking in individuals with unilateral amputation. J. Neuroeng. Rehabil. 2019, 16, 151. [Google Scholar] [CrossRef]
- Clemens, S.; Kim, K.J.; Gailey, R.; Kirk-Sanchez, N.; Kristal, A.; Gaunaurd, I. Inertial sensor-based measures of gait symmetry and repeatability in people with unilateral lower limb amputation. Clin. Biomech. 2020, 72, 102–107. [Google Scholar] [CrossRef]
- Wasser, J.G.; Acasio, J.C.; Miller, R.H.; Hendershot, B.D. Lumbopelvic coordination while walking in service members with unilateral lower limb loss: Comparing variabilities derived from vector coding and continuous relative phase. Gait Posture 2022, 92, 284–289. [Google Scholar] [CrossRef]
- Chang, Y.; Kang, J.; Kim, G.; Shin, H.; Park, S. Intramuscular Properties of Resting Lumbar Muscles in Patients with Unilateral Lower Limb Amputation. Appl. Sci. 2021, 11, 9122. [Google Scholar] [CrossRef]
- Dillingham, T.R.; Pezzin, L.E.; MacKenzie, E.J.; Burgess, A.R. Use and satisfaction with prosthetic devices among persons with trauma-related amputations: A long-term outcome study. Am. J. Phys. Med. Rehabil. 2001, 80, 563–571. [Google Scholar] [CrossRef]
- Persine, S.; Leteneur, S.; Gillet, C.; Bassement, J.; Charlate, F.; Simoneau-Buessinger, E. Walking abilities improvements are associated with pelvis and trunk kinematic adaptations in transfemoral amputees after rehabilitation. Clin. Biomech. 2022, 94, 105619. [Google Scholar] [CrossRef] [PubMed]
- Zidarov, D.; Swaine, B.; Gauthier-Gagnon, C. Quality of life of persons with lower-limb amputation during rehabilitation and at 3-month follow-up. Arch. Phys. Med. Rehabil. 2009, 90, 634–645. [Google Scholar] [CrossRef] [PubMed]
- Won, N.Y.; Paul, A.; Garibaldi, M.; Baumgartner, R.E.; Kaufman, K.R.; Reider, L.; Wrigley, J.; Morshed, S. Scoping review to evaluate existing measurement parameters and clinical outcomes of transtibial prosthetic alignment and socket fit. Prosthet. Orthot. Int. 2022, 46, 95–107. [Google Scholar] [CrossRef] [PubMed]
- Zahedi, M.; Spence, W.; Solomonidis, S.; Paul, J. Alignment of l owe-limb prostheses. J. Rehabil. Res. Dev. 1986, 23, 2–19. [Google Scholar] [PubMed]
- Cardenas, A.M.; Uribe, J.; Font-Llagunes, J.M.; Hernandez, A.M.; Plata, J.A. The effect of prosthetic alignment on the stump temperature and ground reaction forces during gait in transfemoral amputees. Gait Posture 2022, 95, 76–83. [Google Scholar] [CrossRef] [PubMed]
- Ásgeirsdóttir, Þ. A Methodology to Quantify Alignment of Transtibial and Transfemoral Prostheses Using Optical Motion Capture System. Master’s Thesis, KTH Royal Institute of Technology, Stockholm, Sweden, 2022. [Google Scholar]
- Zhou, L.; Fischer, E.; Tunca, C.; Brahms, C.M.; Ersoy, C.; Granacher, U.; Arnrich, B. How We Found Our IMU: Guidelines to IMU Selection and a Comparison of Seven IMUs for Pervasive Healthcare Applications. Sensors 2020, 20, 4090. [Google Scholar] [CrossRef] [PubMed]
- Mueller, J.K.P.; Evans, B.M.; Ericson, M.N.; Farquhar, E.; Lind, R.; Kelley, K.; Pusch, M.; von Marcard, T.; Wilken, J.M. A mobile motion analysis system using inertial sensors for analysis of lower limb prosthetics. In Proceedings of the 2011 Future of Instrumentation International Workshop (FIIW) Proceedings, Oak Ridge, TN, USA, 7–8 November 2011; pp. 59–62. [Google Scholar]
- Ledoux, E.D. Inertial Sensing for Gait Event Detection and Transfemoral Prosthesis Control Strategy. IEEE Trans. Biomed. Eng. 2018, 65, 2704–2712. [Google Scholar] [CrossRef]
- Bastas, G.; Fleck, J.J.; Peters, R.A.; Zelik, K.E. IMU-based gait analysis in lower limb prosthesis users: Comparison of step demarcation algorithms. Gait Posture 2018, 64, 30–37. [Google Scholar] [CrossRef]
- Robinson, J.L.; Smidt, G.L.; Arora, J.S. Accelerographic, temporal, and distance gait factors in below-knee amputees. Phys. Ther. 1977, 57, 898–904. [Google Scholar] [CrossRef]
- Wentink, E.C.; Schut, V.G.; Prinsen, E.C.; Rietman, J.S.; Veltink, P.H. Detection of the onset of gait initiation using kinematic sensors and EMG in transfemoral amputees. Gait Posture 2014, 39, 391–396. [Google Scholar] [CrossRef]
- Simonetti, E.; Bergamini, E.; Vannozzi, G.; Bascou, J.; Pillet, H. Estimation of 3d body center of mass acceleration and instantaneous velocity from a wearable inertial sensor network in transfemoral amputee gait: A case study. Sensors 2021, 21, 3129. [Google Scholar] [CrossRef]
- Demeco, A.; Frizziero, A.; Nuresi, C.; Buccino, G.; Pisani, F.; Martini, C.; Foresti, R.; Costantino, C. Gait Alteration in Individual with Limb Loss: The Role of Inertial Sensors. Sensors 2023, 23, 1880. [Google Scholar] [CrossRef] [PubMed]
- Nolan, L.; Wit, A.; Dudziñski, K.; Lees, A.; Lake, M.; Wychowañski, M. Adjustments in gait symmetry with walking speed in trans-femoral and trans-tibial amputees. Gait Posture 2003, 17, 142–151. [Google Scholar] [CrossRef]
- Vu, H.T.T.; Dong, D.; Cao, H.L.; Verstraten, T.; Lefeber, D.; Vanderborght, B.; Geeroms, J. A Review of Gait Phase Detection Algorithms for Lower Limb Prostheses. Sensors 2020, 20, 3972. [Google Scholar] [CrossRef]
- Vu, H.T.T.; Gomez, F.; Cherelle, P.; Lefeber, D.; Nowe, A.; Vanderborght, B. ED-FNN: A New Deep Learning Algorithm to Detect Percentage of the Gait Cycle for Powered Prostheses. Sensors 2018, 18, 2389. [Google Scholar] [CrossRef]
- Kobayashi, T.; Orendurff, M.S.; Boone, D.A. Dynamic alignment of transtibial prostheses through visualization of socket reaction moments. Prosthet. Orthot. Int. 2015, 39, 512–516. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, H.; Kobayashi, T.; Gao, F.; Kataoka, M. A proper sequence of dynamic alignment in transtibial prosthesis: Insight through socket reaction moments. Sci. Rep. 2023, 13, 458. [Google Scholar] [CrossRef] [PubMed]
- Kibria, Z.; Kotamraju, B.P.; Commuri, S. An Intelligent Control Approach for Reduction of Gait Asymmetry in Transfemoral Amputees. In Proceedings of the 2023 International Symposium on Medical Robotics (ISMR), Atlanta, GA, USA, 19–21 April 2023; pp. 1–8. [Google Scholar] [CrossRef]
- Di Paolo, S.; Barone, G.; Alesi, D.; Mirulla, A.I.; Gruppioni, E.; Zaffagnini, S.; Bragonzoni, L. Longitudinal Gait Analysis of a Transfemoral Amputee Patient: Single-Case Report from Socket-Type to Osseointegrated Prosthesis. Sensors 2023, 23, 4037. [Google Scholar] [CrossRef] [PubMed]
- Ng, G.; Andrysek, J. Classifying changes in amputee gait following physiotherapy using machine learning and continuous inertial sensor signals. Sensors 2023, 23, 1412. [Google Scholar] [CrossRef]
- Manz, S.; Seifert, D.; Altenburg, B.; Schmalz, T.; Dosen, S.; Gonzalez-Vargas, J. Using embedded prosthesis sensors for clinical gait analyses in people with lower limb amputation: A feasibility study. Clin. Biomech. 2023, 106, 105988. [Google Scholar] [CrossRef]
- Kuipers, J.B. Quaternions and Rotation Sequences. In Proceedings of the International Conference on Geometry, Integrability and Quantization, Varna, Bulgaria, 1–10 September 1999; pp. 127–143. [Google Scholar]
- Madgwick, S.O.; Harrison, A.J.; Vaidyanathan, R. Estimation of IMU and MARG orientation using a gradient descent algorithm. In Proceedings of the 2011 IEEE International Conference on Rehabilitation Robotics, Zurich, Switzerland, 29 June–1 July 2011; pp. 1–7. [Google Scholar]
- Skog, I.; Handel, P.; Nilsson, J.-O.; Rantakokko, J. Zero-velocity detection—An algorithm evaluation. IEEE Trans. Biomed. Eng. 2010, 57, 2657–2666. [Google Scholar] [CrossRef] [PubMed]
- Qiu, S.; Wang, Z.; Zhao, H.; Liu, L.; Jiang, Y. Using Body-Worn Sensors for Preliminary Rehabilitation Assessment in Stroke Victims with Gait Impairment. IEEE Access 2018, 6, 31249–31258. [Google Scholar] [CrossRef]
- Masugi, Y.; Kawai, H.; Ejiri, M.; Hirano, H.; Fujiwara, Y.; Tanaka, T.; Iijima, K.; Inomata, T.; Obuchi, S.P. Early strong predictors of decline in instrumental activities of daily living in community-dwelling older Japanese people. PLoS ONE 2022, 17, e0266614. [Google Scholar] [CrossRef]
- Craig, J. Introduction to Robotics—Mechanics and Control, 3rd ed.; Pearson Education: Harlow, UK, 2005; p. 66. [Google Scholar]
- Akarsu, S.; Tekin, L.; Safaz, I.; Göktepe, A.S.; Yazıcıoğlu, K. Quality of life and functionality after lower limb amputations: Comparison between uni- vs. Bilateral amputee patients. Prosthet. Orthot. Int. 2013, 37, 9–13. [Google Scholar] [CrossRef] [PubMed]
- Köse, A.; Cereatti, A.; Della Croce, U. Bilateral step length estimation using a single inertial measurement unit attached to the pelvis. J. Neuroeng. Rehabil. 2012, 9, 9. [Google Scholar] [CrossRef] [PubMed]
- Shema-Shiratzky, S.; Beer, Y.; Mor, A.; Elbaz, A. Smartphone-based inertial sensors technology—Validation of a new application to measure spatiotemporal gait metrics. Gait Posture 2022, 93, 102–106. [Google Scholar] [CrossRef]
- Denavit, J.; Hartenberg, R.S. A kinematic notation for lower-pair mechanisms based on matrices. J. Appl. Mech. 1955, 22, 215–221. [Google Scholar] [CrossRef]
- Cai, M.-L. Gait Analysis and Walk Trajectory Reconstruction Based on Multiple Wireless Inertial Sensors. Master’s Thesis, National Central University, Taoyuan City, Taiwan, 2021. [Google Scholar]
- Kaveny, K.J.; Simon, A.M.; Lenzi, T.; Finucane, S.B.; Seyforth, E.A.; Finco, G.; Culler, K.L.; Hargrove, L.J. Initial results of a variable speed knee controller for walking with a powered knee and ankle prosthesis. In Proceedings of the 2018 7th IEEE International Conference on Biomedical Robotics and Biomechatronics (Biorob), Enschede, The Netherlands, 26–29 August 2018; IEEE: Piscataway, NJ, USA, 2018; pp. 764–769. [Google Scholar]
- Vanicek, N.; Strike, S.; McNaughton, L.; Polman, R. Gait patterns in transtibial amputee fallers vs. non-fallers: Biomechanical differences during level walking. Gait Posture 2009, 29, 415–420. [Google Scholar] [CrossRef]
- Tian, J.; Yuan, L.; Xiao, W.; Ran, T.; Zhang, J.; He, L. Constrained control methods for lower extremity rehabilitation exoskeleton robot considering unknown perturbations. Nonlinear Dyn. 2022, 108, 1395–1408.47. [Google Scholar] [CrossRef]
- Roerdink, M.; Roeles, S.; van der Pas, S.C.; Bosboom, O.; Beek, P.J. Evaluating asymmetry in prosthetic gait with step-length asymmetry alone is flawed. Gait Posture 2012, 35, 446–451. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.K.; Vandervort, E.E.; Moran, K.M.; Adler, C.M.; Chihuri, S.T.; Youdan, G.A. Walking asymmetry and its relation to patient-reported and performance-based outcome measures in individuals with unilateral lower limb loss. Int. Biomech. 2022, 9, 33–41. [Google Scholar] [CrossRef]
- Batten, H.R.; McPhail, S.M.; Mandrusiak, A.M.; Varghese, P.N.; Kuys, S.S. Gait speed as an indicator of prosthetic walking potential following lower limb amputation. Prosthet. Orthot. Int. 2019, 43, 196–203. [Google Scholar] [CrossRef]
- Mattes, S.J.; Martin, P.E.; Royer, T.D. Walking symmetry and energy cost in persons with unilateral transtibial amputations: Matching prosthetic and intact limb inertial properties. Arch. Phys. Med. Rehabil. 2000, 81, 561–568. [Google Scholar] [CrossRef] [PubMed]
- Middleton, A.; Fulk, G.D.; Beets, M.W.; Herter, T.M.; Fritz, S.L. Self-Selected Walking Speed is Predictive of Daily Ambulatory Activity in Older Adults. J. Aging Phys. Act. 2016, 24, 214–222. [Google Scholar] [CrossRef] [PubMed]















| Motion Tasks | RMSE (mm) | EP (%) | Designated Path Length (mm) |
|---|---|---|---|
| 2D (Right) | 5.94 ± 1.31 | 0.92 ± 0.2 | 5209 |
| 2D (Left) | 4.51 ± 0.64 | 0.7 ± 0.1 | |
| 3D (Right) | 13.49 ± 1.83 | 1.65 ± 0.22 | 8307.3 |
| 3D (Left) | 14.56 ± 1.12 | 1.78 ± 0.14 |
| Hip | Knee | Ankle | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Left | Right | Left | Right | Left | Right | |||||||
| RMSE (mm) (°) * | 6.4 ± 0.62 | 6 ± 0.86 | 6.74 ± 1.71 | 6.16 ± 1.62 | 7.31 ± 1.54 | 8.22 ± 1.37 | ||||||
| CC | 0.96 ± 0.01 | 0.96 ± 0.02 | 0.98 ± 0.01 | 0.98 ± 0.01 | 0.89 ± 0.04 | 0.81 ± 0.08 | ||||||
| EP (%) | 20 ± 3.80 | 21 ± 5.30 | 12 ± 1.70 | 15 ± 8.10 | 37 ± 13.20 | 33 ± 12.10 | ||||||
| Swing | Stance | Swing | Stance | Swing | Stance | Swing | Stance | Swing | Stance | Swing | Stance | |
| RMSE (°) | 7.21 | 6.46 | 8.2 | 6.74 | 7.45 | 5.4 | 8.42 | 6.06 | 8.88 | 4.26 | 8.99 | 6.17 |
| CC | 0.91 | 0.93 | 0.88 | 0.91 | 0.97 | 0.83 | 0.93 | 0.9 | 0.87 | 0.94 | 0.79 | 0.83 |
| Subject # | Gender | Age (yr) | Weight (kg) | Height (cm) | Affected Side | Level of Amputation | Duration of Prosthesis Usage | Prosthesis |
|---|---|---|---|---|---|---|---|---|
| 1 | F | 53 | 53 | 157 | R | T/F | More than 20 years | Knee: Total Knee® 2000 |
| Foot: FEEDOM Seirra® | ||||||||
| 2 | M | 43 | 75 | 178 | L | T/F | More than 25 years | Knee: Total Knee® 2000 |
| Foot: ottobock-1D35 | ||||||||
| 3 | M | 26 | 60 | 172 | R | T/T | More than 8 years | Foot: Pro-Flex® XC |
| 4 | M | 53 | 72 | 170 | L | T/T | More than 40 years | Foot: Pro-Flex® XC |
| 5 | M | 45 | 95 | 178 | L | T/T | More than 20 years | Foot: Pro-Flex® XC |
| # | Speed (m/min) | Cadence (Step/min) | Stride (m) | Low Back Motion (°) * | ROMs of Healthy Legs (°) | ROMs of Prosthetic Legs (°) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| C | S | T | Hip | Knee | Ankle | Hip | Knee | Ankle | ||||
| 1 | 73.9 ± 1.8 | 123.2 ± 3 | 1.2± 0 | 3.3 ± 0.4 | 7.9 ± 0.4 | 5.8 ± 1.5 | 45.1 ± 1.7 | 30.7 ± 1.6 | 39.7 ± 7.9 | 43.3 ± 1.1 | 66.2 ± 1.9 | 27.7 ± 2.6 |
| 2 | 67.6 ± 1.1 | 90.1 ± 1.5 | 1.5± 0 | 10.5 ± 0.4 | 13.4 ± 0.8 | 11.9 ± 0.5 | 42.3 ± 1.8 | 46.3 ± 3.3 | 23.8 ± 1.9 | 40.9 ± 1.1 | 65.4 ± 1.0 | 21.9 ± 4.2 |
| 3 | 70.6 ± 6.5 | 117.7 ± 10.9 | 1.2 ± 0 | 2.5 ± 0.8 | 3.9 ± 0.6 | 3.7 ± 0.6 | 33.1 ± 1.7 | 37.8 ± 6.5 | 21.4 ± 1.6 | 30.3 ± 2.8 | 44.5 ± 3.8 | 20.8 ± 2.6 |
| 4 | 78.1 ± 5.7 | 104.1 ± 7.6 | 1.5 ± 0 | 2.8 ± 0.3 | 3.8 ± 0.7 | 2.3 ± 2 | 38.1 ± 6.6 | 38.8 ± 4.5 | 29.7 ± 2.8 | 48.3 ± 2.8 | 52.1 ± 3.8 | 29.8 ± 7.3 |
| 5 | 78.3 ± 4.9 | 112.4 ± 5.8 | 1.4 ± 0.1 | 5.4 ± 0.6 | 11.8 ± 1.3 | 10 ± 1.3 | 35.9 ± 3.5 | 46.2 ± 3.4 | 32.3 ± 6.5 | 41.3 ± 0.8 | 41.8 ± 7.0 | 17.6 ± 2.9 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Han, S.-L.; Cai, M.-L.; Pan, M.-C. Inertial Measuring System to Evaluate Gait Parameters and Dynamic Alignments for Lower-Limb Amputation Subjects. Sensors 2024, 24, 1519. https://doi.org/10.3390/s24051519
Han S-L, Cai M-L, Pan M-C. Inertial Measuring System to Evaluate Gait Parameters and Dynamic Alignments for Lower-Limb Amputation Subjects. Sensors. 2024; 24(5):1519. https://doi.org/10.3390/s24051519
Chicago/Turabian StyleHan, Shao-Li, Meng-Lin Cai, and Min-Chun Pan. 2024. "Inertial Measuring System to Evaluate Gait Parameters and Dynamic Alignments for Lower-Limb Amputation Subjects" Sensors 24, no. 5: 1519. https://doi.org/10.3390/s24051519
APA StyleHan, S.-L., Cai, M.-L., & Pan, M.-C. (2024). Inertial Measuring System to Evaluate Gait Parameters and Dynamic Alignments for Lower-Limb Amputation Subjects. Sensors, 24(5), 1519. https://doi.org/10.3390/s24051519






